Cartilage & Bone: Overview (Lecture Notes)
1/48
Earn XP
Description and Tags
Question-and-answer flashcards covering cartilage and bone concepts from the lecture notes.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
49 Terms
What are the functions of cartilage?
Surround and protect organs, muscles, blood vessels and nerves (bone, connective tissue proper)
Carry and store nutrients (blood)
Support (bone, cartilage, connective tissue proper)
Immunity (blood cells, loose areolar)
Insulate (adipose)
Name the three types of cartilage.
Hyaline cartilage, elastic cartilage, and fibrocartilage.
Hyaline cartilage, the most common type, is found in:
Articular Cartilage: Covers bone ends in synovial joints, providing smooth movement (lacks perichondrium here).
Respiratory Tract: Nose, trachea, larynx (maintains open airways).
Costal Cartilage: Connects ribs to sternum (allows breathing flexibility).
Embryonic Skeleton: Temporary template for most developing bones.
Where is elastic cartilage located?
known for its flexibility, is found in:
Ear (Auricle/Pinna): Shapes the external ear.
Epiglottis: Flap preventing food entry to trachea during swallowing.
Eustachian (Auditory) Tubes: Helps equalize middle ear pressure.
Laryngeal Cartilages: Provides support and elasticity to parts of the larynx.
Where is fibrocartilage located?
known for high tensile strength and compression resistance, is found in:
Intervertebral Discs: Shock absorbers between vertebrae.
Pubic Symphysis: Connects pelvic halves (stability & flexibility).
Knee Menisci: C-shaped pads stabilizing the knee joint.
Articular Discs: Found in some joints (e.g., TMJ) for congruence and shock absorption.
What are chondroblasts?
Immature cartilage cells located under the perichondrium. They secrete the extracellular matrix and are vital for cartilage growth and repair. As they become embedded, they mature into chondrocytes.
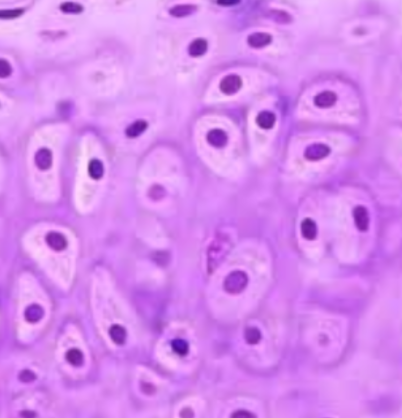
What are chondrocytes?
Mature cartilage cells residing in small spaces called lacunae within the cartilage matrix. They maintain the matrix and respond to mechanical stress, ensuring cartilage integrity.
What is the perichondrium?
A dense, irregular connective tissue layer surrounding most hyaline and all elastic cartilage (absent on articular cartilage and fibrocartilage). It has two layers:
- Outer Fibrous Layer: For protection and mechanical support (collagen fibers, fibroblasts).
- Inner Chondrogenic Layer: Contains chondroblasts for appositional growth (width) and repair.
What is the extracellular matrix of cartilage composed of?
The cartilage ECM provides its unique properties, mainly:
- Collagen Fibers: Primarily Type II (hyaline, elastic) or Type I (fibrocartilage), offering tensile strength.
- Ground Substance: A hydrated, gel-like material rich in proteoglycans, GAGs (e.g., chondroitin sulfate), and water (up to 80%). This allows resistance to compression and nutrient diffusion.
Why doesn’t cartilage regenerate well?
has limited repair capacity due to:
Avascularity: No direct blood supply; slow and inefficient nutrient diffusion from perichondrium or synovial fluid.
Lack of Innervation: No nerves, so injury often goes unnoticed until severe.
Low Metabolic Rate: Chondrocytes are metabolically sluggish, limiting rapid matrix production.
Limited Cell Mobility: Chondrocytes are trapped in lacunae, restricting movement to injury sites.
What are the features of hyaline cartilage?
- Most Common Type: Prevalent throughout the body.
- Appearance: Glassy and translucent in fresh tissue.
- Fiber Composition: Fine, invisible network of mostly Type II collagen fibers.
- Locations: Articular surfaces, respiratory tract, costal cartilages, embryonic skeleton.
- Perichondrium: Present, except at articular surfaces (for easier movement).
What are the features of elastic cartilage?
- High Flexibility: Bends easily and returns to original shape due to its elasticity.
- Fiber Composition: Rich in elastic fibers (elastin) intertwined with Type II collagen.
- Appearance: Appears yellowish due to elastic fibers.
- Locations: External ear, epiglottis, Eustachian tubes, some larynx cartilages.
- Perichondrium: Always covered by a perichondrium.
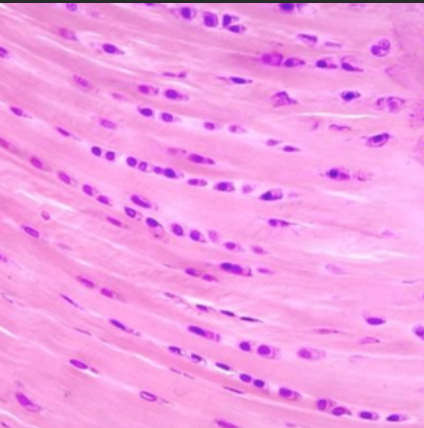
What are the features of fibrocartilage?
- High Tensile Strength: Excellent resistance to pulling forces and compression.
- Fiber Composition: Dense, parallel bundles of thick, visible Type I collagen fibers.
- Cell Arrangement: Chondrocytes often arranged in rows between collagen bundles.
- Locations: Areas of high stress (intervertebral discs, pubic symphysis, knee menisci).
- Perichondrium: Lacks a perichondrium (distinguishing feature).
What are the major functions of bone?
- Support & Protection: Provides a rigid framework and protects vital organs (e.g., skull, rib cage).
- Enable Movement: Attachment points for muscles, acting as levers for movement.
- Mineral Storage: Reservoir for Ca^{2+} and PO_4^{3-}, released as needed for homeostasis.
- Hematopoiesis: Red bone marrow produces blood cells.
- Energy Storage: Yellow bone marrow (medullary cavity) stores fat as an energy reserve.
- Energy Metabolism: Osteocytes secrete osteocalcin, regulating blood sugar and fat deposition.
What is osteoid?
The organic, unmineralized component of bone matrix secreted by osteoblasts. It's mainly Type I collagen (90%) and ground substance, providing bone's tensile strength and flexibility before mineralization.
What minerals give bone rigidity?
The primary mineral is hydroxyapatite (Ca{10}(PO4)6(OH)2), a crystalline calcium phosphate. It accounts for 65-70% of bone mass and provides its hardness and compression resistance.
How is bone both flexible and rigid?
unique composition balances these properties:
Flexibility: Achieved by the organic component (Type I collagen fibers), which provides tensile strength and resistance to stretching/twisting.
Rigidity: Provided by the inorganic mineral (hydroxyapatite crystals), offering hardness, compression resistance, and weight-bearing capacity.
Who are osteoblasts?
Bone-forming cells (immature) that synthesize and secrete osteoid (organic bone matrix). They are found on bone surfaces (periosteum and endosteum) and differentiate into osteocytes when trapped in mineralized matrix.
Who are osteoclasts?
Large, multinucleated cells responsible for bone resorption (breaking down bone tissue). Derived from monocytes, they create an acidic environment and release enzymes to dissolve bone, releasing minerals for remodeling and homeostasis.
Who are osteocytes?
The most abundant, mature bone cells (derived from osteoblasts) housed in lacunae within the mineralized matrix. They maintain the bone matrix and sense mechanical stress, signaling for bone remodeling.
What is the difference between osteoblasts and osteocytes?
Key differences in activity and location:
- Osteoblasts: Build bone by actively synthesizing and secreting osteoid on bone surfaces.
- Osteocytes: Maintain bone and sense mechanical strain. They are mature osteoblasts trapped within mineralized bone matrix in lacunae.
What is the periosteum?
A tough, vascularized, dense irregular connective tissue membrane covering the external surface of most bones (except articular cartilage). It has two layers:
- Outer Fibrous Layer: Protection; anchoring for tendons/ligaments.
- Inner Cellular (Cambium) Layer: Contains osteoblasts and osteoprogenitor cells for diametrical bone growth (appositional) and fracture repair.
What is the endosteum?
A thin, delicate connective tissue membrane that lines all internal surfaces of bone. (e.g., medullary cavity, central canals, trabeculae). It contains osteoblasts and osteoclasts, making it a key site for bone remodeling, growth, and repair.
What is the function of the medullary cavity?
The hollow, central space within the diaphysis (shaft) of long bones. Its primary function is to house bone marrow:
- Adults: Primarily yellow bone marrow (fat storage).
- Children: Contains red bone marrow (hematopoiesis/blood cell production).
What is the epiphyseal line?
A thin, distinct line of compact bone in adult long bones, representing the remnant of the epiphyseal plate (growth plate). It signifies that longitudinal (length) bone growth has ceased and the epiphysis and diaphysis have fused.
What is the periosteum vs endosteum difference?
The main differences are location and function:
- Periosteum: Covers the exterior of bone; responsible for appositional growth, repair, and nutrient supply.
- Endosteum: Lines the interior of bone (medullary cavity, central canals, trabeculae); crucial for bone remodeling due to osteoblast/osteoclast presence.
What is compact bone?
Dense, hard outer layer of most bones (e.g., diaphysis of long bones). It's solid, strong, and resists bending/twisting. Microscopically, it's characterized by tightly packed osteons.
What is spongy bone?
Lighter, less dense bone tissue found inside bones (e.g., epiphyses of long bones, flat bones). It consists of a lattice-like network of bony spines called trabeculae, which provide strength while minimizing weight. Spaces between trabeculae are filled with red bone marrow.
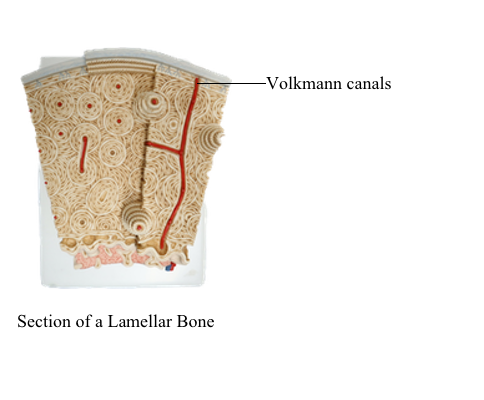
What is the microstructure of compact bone called?
Compact bone is organized into repeating cylindrical units called osteons (Haversian systems). Each osteon includes:
Central (Haversian) Canal: Longitudinal (HEIGHT/VERTICAL) canal with blood vessels and nerves.
Lamellae: Concentric rings of mineralized matrix around the central canal.
Lacunae: Small cavities housing osteocytes, located between lamellae.
Canaliculi: Tiny channels connecting lacunae to each other and to the central canal, for nutrient/waste exchange.
Volkmann’s (Perforating) Canals: Perpendicular (HORZINTIAL)canals connecting adjacent osteons and periosteum to central canals (blood supply).
What are lacunae?
Small, oval-shaped cavities or spaces within the solid bone (or cartilage) matrix. In bone, they house osteocytes, protecting them while allowing matrix maintenance.
What are lamellae?
Thin, concentric layers or rings of mineralized bone matrix. In compact bone, they are arranged around the central Haversian canal within osteons, providing strength.
What are canaliculi?
Microscopic, hair-like channels radiating from lacunae through lamellae. They connect adjacent lacunae to each other and to the central canals, facilitating nutrient and waste diffusion to osteocytes.
What is a Volkmann’s canal?
>acts like the pipes connectin the central canals in bone. They help facilitate communication and nutrient exchange between osteons.
Also called a perforating canal, it's a horizontal or oblique canal that runs perpendicular to central (Haversian) canals. These canals allow blood vessels and nerves to connect different osteons and the periosteum.
How does spongy bone differ microscopically from compact bone?
Key microscopic differences:
- No Osteons: Spongy bone lacks the organized osteon units seen in compact bone.
- Trabeculae: Instead, it features an irregular lattice-work of thin bony plates called trabeculae.
- Nutrient Diffusion: Osteocytes in spongy bone receive nutrients via canaliculi that open directly onto trabecular surfaces, allowing diffusion from the surrounding bone marrow spaces (no central canals).
Where is spongy bone located?
Spongy bone is primarily found in:
- Epiphyses of Long Bones: Fills the ends of long bones (e.g., femur, humerus).
- Interior of Flat, Short, and Irregular Bones: Forms the inner bulk of bones like vertebrae, hip bones, sternum, and cranial bones, usually sandwiched between compact bone layers.
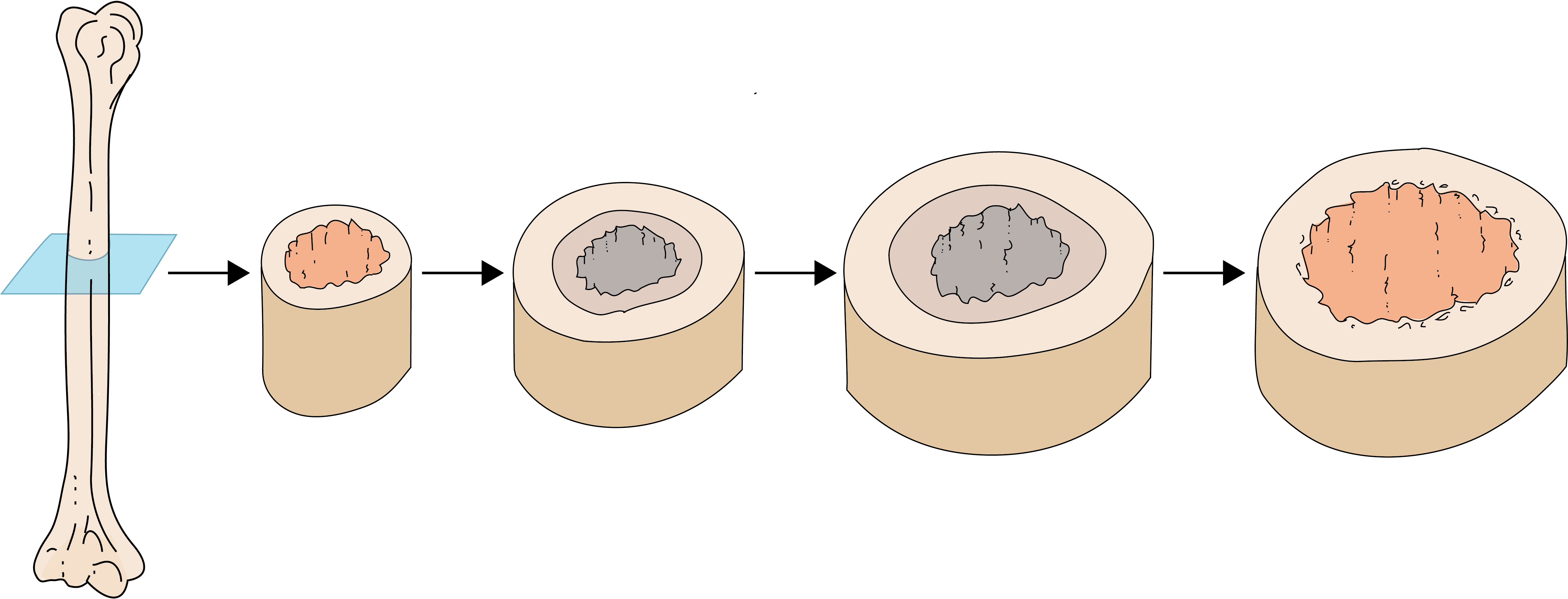
What are the two types of bone growth?
Bone primarily grows through two mechanisms:
- Interstitial Growth (Growth in Length): Occurs at epiphyseal plates, leading to the lengthening of long bones.
- Appositional Growth (Growth in Diameter/Thickness): Deposition of new bone on the outer surface, increasing bone width.
Where does interstitial bone growth occur?
increase in length or internal size of a tissue due to the division of cells within it and the secretion of new matrix between existing cells.
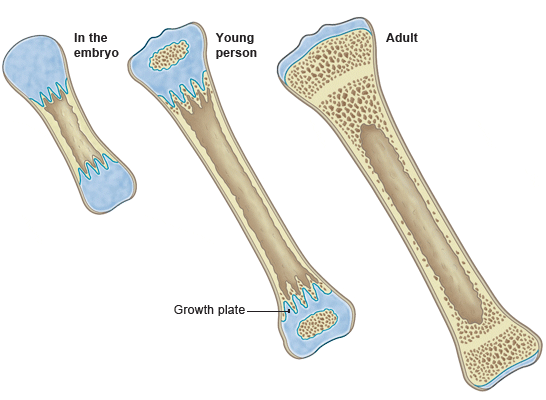
What is appositional bone growth?
Appositional growth is how bones increase in diameter or thickness through a coordinated process:
- Deposition: Osteoblasts in the periosteum deposit new bone matrix on the external surface.
- Resorption: Simultaneously, osteoclasts on the endosteal surface resorb bone from the inner surface, enlarging the medullary cavity without making the bone too heavy.
What is remodeling in bone?
Bone remodeling is a continuous process of old bone removal and new bone formation throughout life. It involves:
- Osteoclasts: Resorb (break down) old/damaged bone.
- Osteoblasts: Deposit (form) new bone.
This maintains mineral homeostasis and adapts bone structure to mechanical stress.
What are the renewal rates for bone types?
Bone remodeling rates differ significantly:
- Compact Bone: Renewed approximately every 10 years (slower turnover).
- Spongy Bone: Renewed about every 3–4 years (much faster turnover, making it more metabolically active and susceptible to conditions like osteoporosis).
What is osteoporosis?
>A chronic disease characterized by low bone mass and microscopic deterioration of bone architecture, leading to increased fragility and fracture risk.
>Here, resorption by osteoclasts exceeds deposition by osteoblasts. Common in vertebrae and femoral neck, especially with aging and postmenopausal estrogen deficiency.
osteoclasts>osteoblasts
What would be the opposite of osteoporosis?
The opposite of osteoporosis (low bone density, fragility) would be a condition of increased bone density or higher bone mass. Examples include:
- Osteopetrosis: A rare genetic disorder with abnormally dense, yet paradoxically brittle, bones due to defective osteoclast function (failure to resorb bone).
- More generally, osteosclerosis: Hardening or thickening of bone due to increased formation or decreased resorption, without necessarily leading to brittleness.
What are sesamoid bones?
Small, independent bones embedded within tendons, typically where a tendon crosses a joint. They act as pulleys to modify muscle pull, reduce friction, and improve mechanical advantage. The prime example is the patella (kneecap) in the quadriceps tendon.
Name the five classes of bone.
Bones are categorized by shape into five major classes:
- Long bones: Longer than wide (e.g., femur, humerus).
- Short bones: Roughly cube-shaped (e.g., carpals, tarsals).
- Flat bones: Thin, flattened, often curved (e.g., sternum, skull bones, scapulae).
- Irregular bones: Complex shapes not fitting other categories (e.g., vertebrae, hip bones).
- Sesamoid bones: Small bones embedded in tendons (e.g., patella).
What are the features of a long bone?
A typical long bone has:
- Diaphysis (Shaft): Main cylindrical body of compact bone, surrounding a medullary cavity.
- Epiphyses (Ends): Proximal and distal ends; wider than diaphysis, composed of spongy bone covered by compact bone.
- Articular Cartilage: Smooth hyaline cartilage covering the epiphyses at joints, for reduced friction.
- Periosteum: Dense connective tissue covering the outer bone surface (except articular cartilage).
- Medullary Cavity: Hollow space in diaphysis; contains yellow bone marrow in adults.
- Endosteum: Thin membrane lining inner bone surfaces.
What covers the ends of long bones with articular cartilage?
The ends of long bones that form articulating joints, specifically the epiphyses, are covered by a layer of articular (hyaline) cartilage.
What covers the outside of the bone?
The external surface of most bones (excluding articular cartilage) is covered by the periosteum. This fibrous membrane is crucial for growth, repair, and nutrient supply.
What lines the inside of bone and medullary cavity?
The internal surfaces of bone, including the medullary (marrow) cavity, central canals of osteons, and spongy bone trabeculae, are lined by the endosteum. It contains active osteoblasts and osteoclasts.
What role do bone cells play in energy metabolism?
Bone cells, especially osteocytes, function as endocrine cells by secreting osteocalcin. When activated, osteocalcin:
- Regulates Blood Sugar: Increases pancreatic insulin secretion and improves tissue insulin sensitivity, lowering blood glucose.
- Influences Fat Storage: Affects adipocytes, influencing fat deposition and overall energy balance.
This shows bone's role beyond just structure.