Unit 5 - PSL 310 - Flashcards
1/55
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
56 Terms
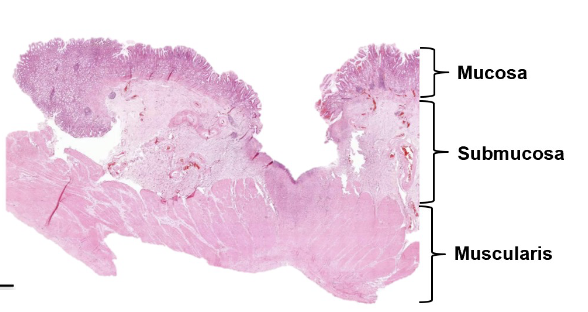
Gastrointestinal Layers - Stomach
and
Secretion vs. Excretion
Mucosa - most visceral
mucous epithelium
lamina propria
musclaris mucosae
Sub Mucosa
Submucosal Plexus(Meissner’s): ENS Gland Secretion
big blood vessels inside
Muscilaris
Circular Muscle
Myenteric Plexus(Auerbach’s): ENS Smooth Muscle
Longitudinal Muscle
Seroa
Connective Tissue Layer
Peritoneum
Secretion = move something onto the surface of an epithelial lining
Excretion = removal from the body, i.e., sweat, feces, urine
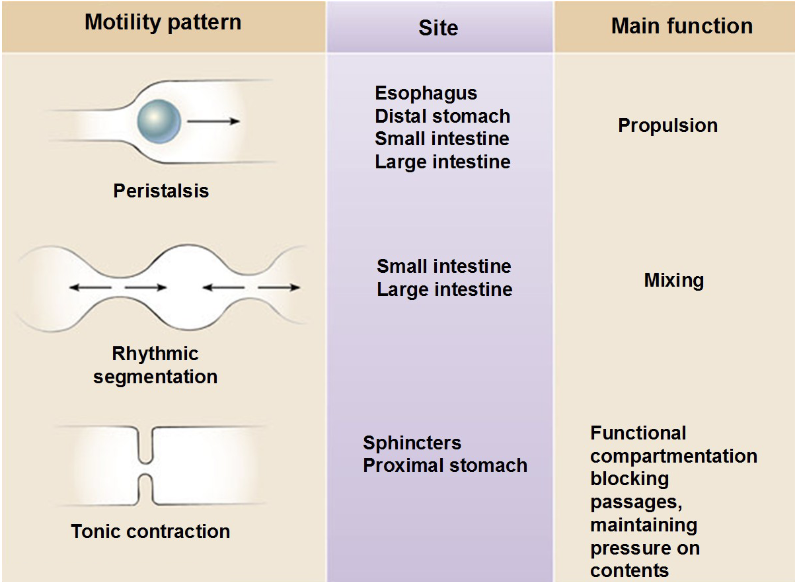
Molility Patters, Functions and Locations
Peristalis - (propulsion) - everywhere
Rhythmic segmentation - (mixing) - Small and Large Intestine
Tonic contraction - (Functional compartmentation, blocking passages, maintaining pressure on contents) - Spincters and Proximal Stomach
GI Tract Activity - Autonomic, Enteric, and Diffuse Neuroendocrine System (DNES)
Autonomic -
PNS Stimulates the GI tract
SNS Inhibits the GI tract
Enteric - “little brain in the gut”, Feedforward and enteric receptors
submucosal (Meissner’s) - glandular secretion
myenteric (Auerbach’s) - motility
- contains interoceptors (mechanical & chemical)

DNES - “single cell endocrine glands” —> secretes the hormones into the blood, but still has effects on the SI and stomach
gastroendocrine (stomach) and enteroendocrine (SI) cells
secrete endocrine hormones that modulate GI tract activity
Salivary Glands
Parotid - cheek
Submandibular - beneath the mandible
Sublingual - beneath the tongue
All have ducts that open up into the oral cavity, innervated by PNS, through the feed-forward and visceral receptors
*Sialorrhea: excessive drooling, largely due to cognitive disorders, but also a problem swallowing.
*Treatment: Can be treated with an AChe inhibitor (PNS Inhibator)
Oral Cavity - Digestion - Mechanical, Chemical
Mechanical - chewing and smashing food against the hard palate with the tongue increases its surface area. Deglutition = Swallowing
Chemical - paired salivary glands secrete the constituents of saliva (water, mucus, ions, buffers, antimicrobics (IgA, lysozyme), enzymes (lingual lipase, salivary amylase(starch)))
*pH in the oral cavity is ≈ 7 (salivary amylase) —> Carbohydrates
*pH optimum of lingual lipase is ≈ 5, doesn’t work to break down lipids, cruises down to the stomach where the pH is 5
Esophagus - anatomy and cells
The esophagus is 20 cell layers of non-keratinized stratified squamous epithelium —> lubricated with mucus
Upper Esophageal Sphincter = prevents air from entering the stomach
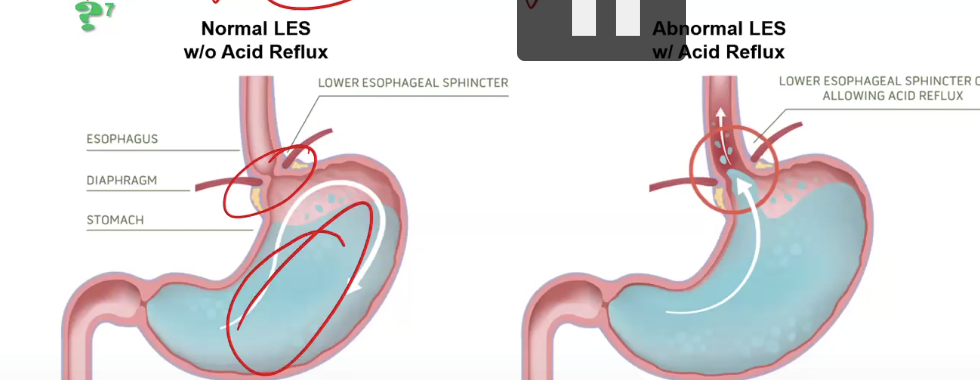
Lower Esophageal Sphincter (cardiac sphincter) - prevents stomach contents from entering the esophagus. If not good, GERD (heartburn).
Esophageal Pathology - GERD
largely results from acid reflux due to gastroesophageal reflux disease (GERD), caused by abnormal/weakened/relaxes LES or increased intra-abdominal pressure from pregnancy, obesity, hiatal hernia, gastroparesisor
Treatment: Gerd can be treated with antacids (TUMS), H2RAs (Pepcid, Zantax [blocks histamine-2 receptors in the stomach, thus reducing the amount of acid the stomach produces]), PPIs (Prilosec, Nexium, Protonix), and surgery
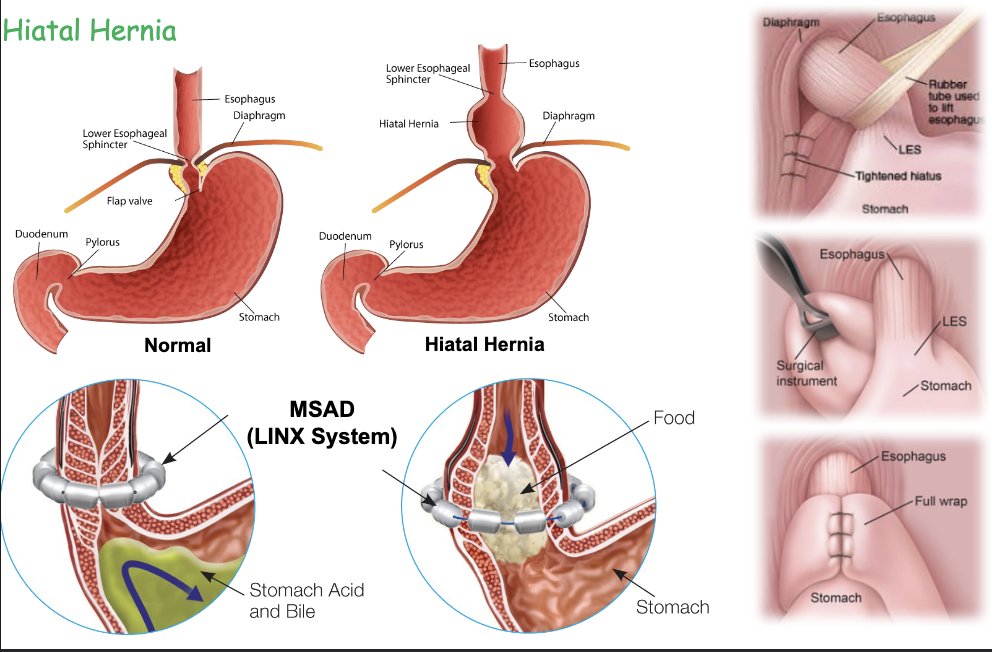
Hiatal Hernia
Caused by obesity or pregnancy, it can be treated with MSAD (Linux System) and Nissen fundoplication (surgery)
Esophagitis + Barrett’s esophagus + Esophageal Cancer
Esophagitis - inflammation of the esophageal lining, caused by GERD, infections, or NSAIDs.
“pill induced” - stuck pill in throat
Barrett’s is caused by chronic GERD, which transforms stratified squamous cells of the lower one-third of the esophageal lining to a simple columnar epithelium with goblet cells. “Survival of the fit”
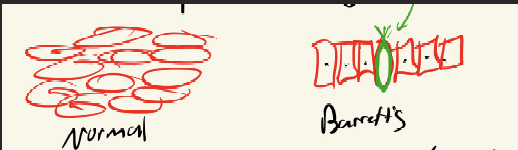
Barrett’s esophagus cells can become dysplastic (precancerous), which can cause Esophageal Cancer ( caused by GERD, smoking, alcohol, obesity, and tobacco)
Stomach Anatomy
Fundus - upper “pouch”
Cardia - near the esophagus
Body / Corpus - main body
Pylorus - the bottom, end of the stomach, has the Pyloric Sphincter
Ruggae - permanent folds in the mucosa and submucosa —> increases surface area of stomach
3 muscle layers - (OUTER) Longitudinal, Circular, and Oblique (INNER) —> allows the stomach to mix and turn due to having 3 muscle layers
*The stomach growling sound is due to chyme squirting into the Duodenum through the pyloric Sphincter
Stomach - Digesion - Chemical, Mechanical
Mechanical - peristaltic wave contractions mix the bolus with digestive juices and periodically “squirt” chyme into the duodenum
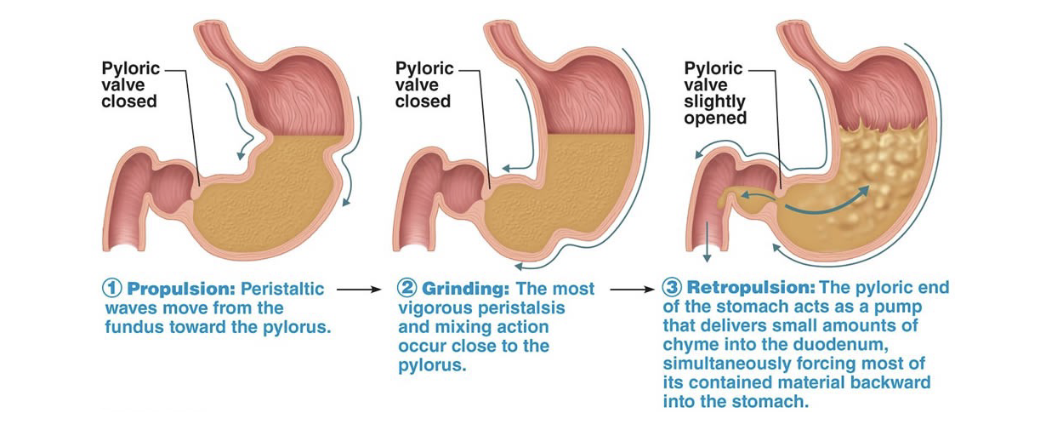
Chemical - gastric glands produce digestive enzymes and gastroendocrine hormones, which are found in gastric folds (folds on the rugae)
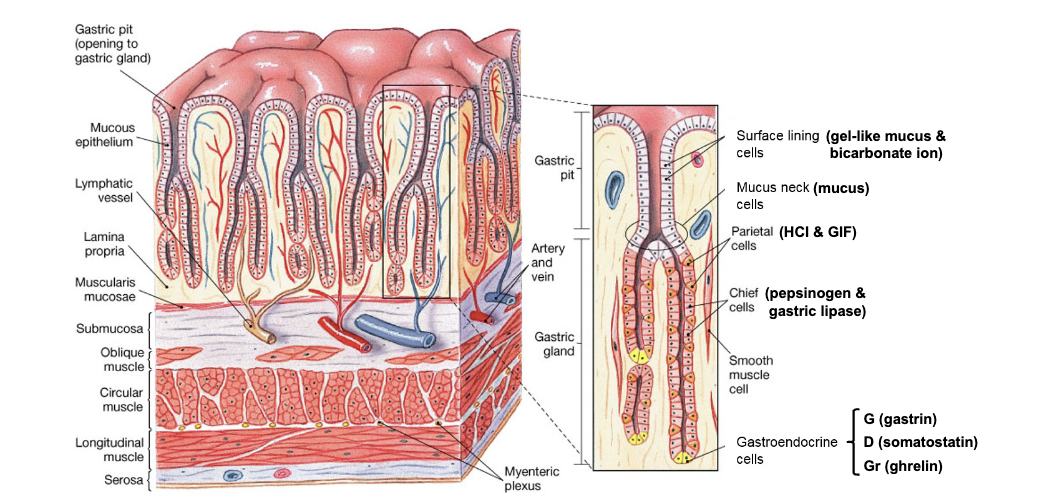
Gastric Pit - Pit —> Neck (isthamus) —> Base (where glands secrete stuff) [lamina propria]
Surface Lining Cells secrete an INSOLUBLE gel-like mucus & bicarb. which makes up the gastric mucosal barrier
Mucus Neck Cells release normal mucus, which becomes part of the chyme
Base
Parietal Cell: Secretes H+ (pumps into Lumen of stomach) and GIF (absorption of vitamin B12)
Chief Cell: Secretes pepsinogen (inactive protein enzyme), gets cleaved into pepsin. Secretes gastric lipase (lipids)
Gastroendocrine cells: Gastrin —> tells stomach to digest more. Somatostatin —> inhibits production of HCL (parietal cells). Ghrelin → Grr hormone stimulates one to be hungry (only in interdigestive state)
*released into the blood, not the stomach
When stomach is empty Gastrin and Somatostain is still released.
Gastric Mucosal Barrier + Stomach Acidity
Stomach acidity kills microbes, denatures protein, and “activates” pepsinogen (technically at a pH of 2, it reaches around and cuts off its amino acids, making it active pepsin
Parietal Cells release H+, which binds with Cl-, making the stomach acidic, pH of 2 (interdigestive state) and, pH of 5 (digestive state). Carbonic anhydrase also releases GIF (B12 absorption) —> the GIF and B12 combination goes down to the Small intestine to be absorbed.
Surface Lining Cells release mucus and Bicarb. making a “barrier”.
Neck Cells: release mucus into the Lumen
*H. pylori: bacteria secrete ammonia, which repels H+ ions so they can get to the barrier. Once at the barrier, they burrow down to the surface, damaging lining cells, causing them not to release mucus and bicarbonate. This causes gastric ulcers, gastritis, and inflammation of the stomach
Treatment: 1) antibiotics, 2) PPIs (inhibit Parietal Cell), 3) Probiotics (good bacteria outcompete the bad)
Stomach - Parietal Cell + Regulation
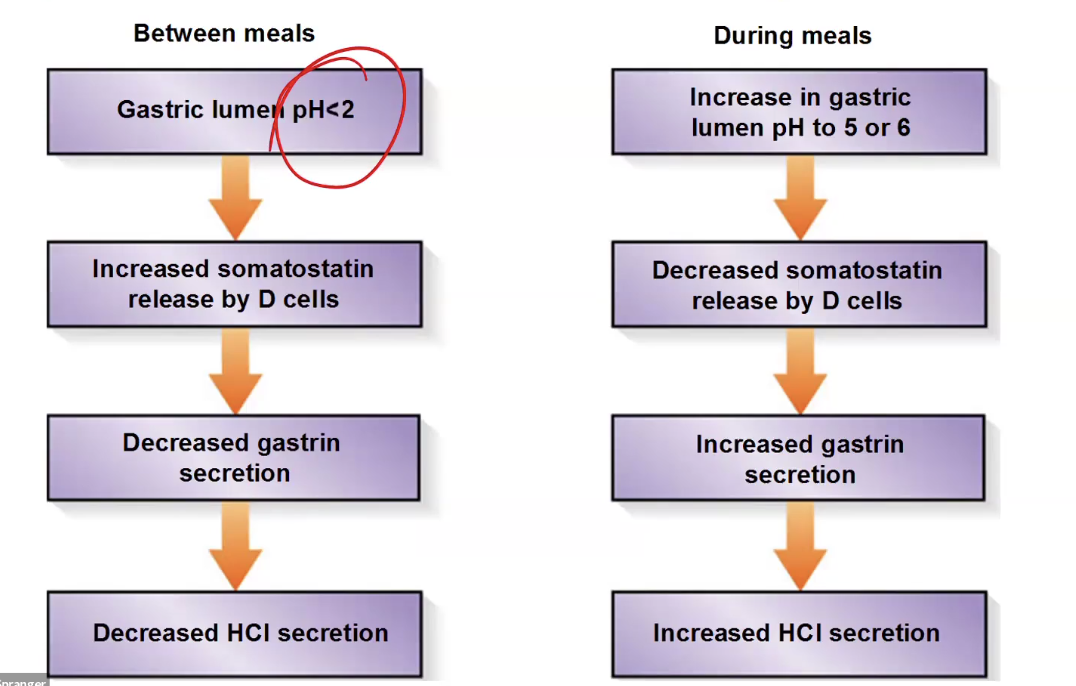
Parietal Cell is under a tonic break by the D Cell (Somatostatin Secretion) when the pH is < 2, “self-check” for making sure stomach pH doesn’t get too low
Increased ENS would directly increase Parietal Cell Stimulation (acid secretion) using ACh.
ENS would also stimulate G Cell (Gastrin Secretion) (tell the stomach to increase digestion), stimulate parietal cells directly, and stimulate ECL Cells (Histamine), which also activate parietal cells
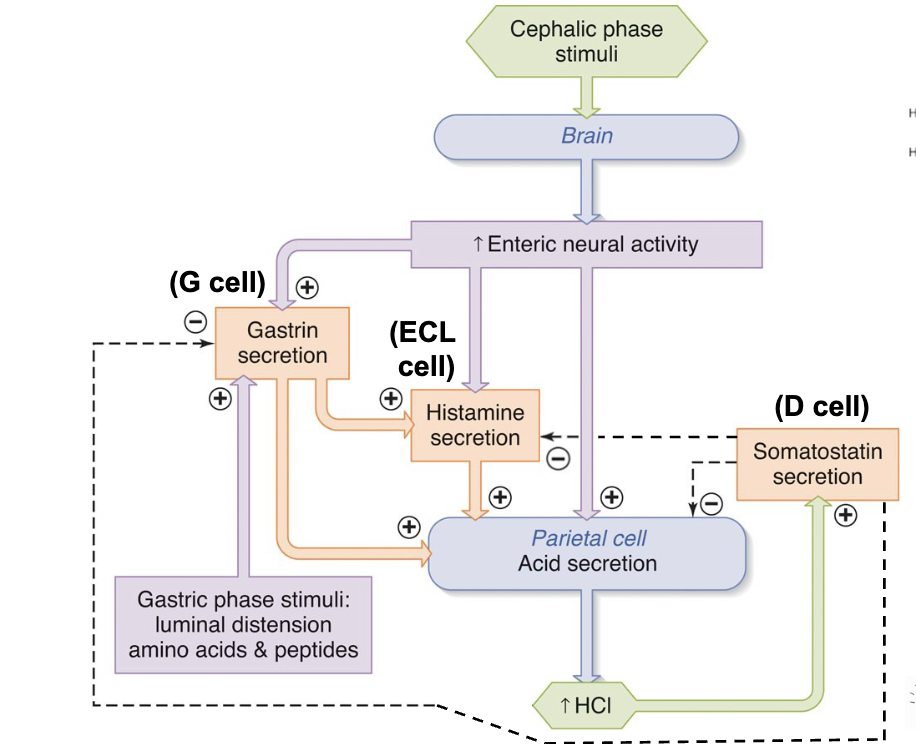
Presence of food + Stretch stimulates Gastrin + Histamine → Increase Parietal Cell stimulation
Stomach - Gastroendocrine Cells
RELEASED INTO THE BLOOD
G Cell (gastrin)
Increased gastric activity (mechanical and chemical)
induced by Amino Acids, stretch, and FeedForward
D Cell (somatostatin) - tonically secreted interdigestive state
Inhibits parietal cells
induced by low pH (tonic break of parietal cells to keep pH no lower than 2)
Gr Cell (ghrelin) - tonically secreted interdigestive state
increases neuroopeptide Y (NPY) in the hypothalamus, stimulating appetite (making you feel full)
Stomach - Chief Cell
Secretes pepsinogen (pH 2 → pepsin) and gastric lipase (pH 5 → works well)
*The hormone leptin decreases appetite ( ⬇ NPY)
*Pepsinogen autocleaves to pepsin (peptidase enzyme)
Neuroendocrine Control of the Stomach - 3 phases
Brain: controls the stomach by feedforward (Cephalic Phase), Vagus nerve, through the Submucosal and Myenteric plexus stimulates Mucous cells, Chief cells, Parietal Cells, and G Cells → Gastrin (Positive Feedback).
Stomach: controls the stomach by the presence of food, pH, and positive feedback (Gastric Phase). Stretch and Chemoreceptors stimulate through the Submucosal and Myenteric plexus, stimulating Mucous cells, Chief cells, Parietal Cells, and G Cells → Gastrin (Positive Feedback).
Small Intestine: controls the stomach by short, enterogastric reflexes and negative feedback (Intestinal Phase) - Through Enteroendocrine Cells (SMILK), they inhibit Myenteric & Submucosal plexus and shut down the stomach ( shut down peristalsis, Myenteric & Submucosal plexus, Chief & Parietal Cells) GIP, CCK, GLP-1, Secretin
Gastritis + Peptic Ulcer Disease (PUD)
Gastritis is inflammation of the stomach lining caused by NSAIDS and H. Pylori infection
Treated by antacids, antibiotics (amoxicillin and clarithromycin), H2RAs → (inhibits parietal cells), and PPIs → (inhibits stomach acid pump)
“Triple Therapy” → PPI + Amoxicillin + Clarithromycin
Peptic Ulcer Disease (PUD) is a degradation of the gastric mucosa down to, or beyond, the submucosa, caused by chronic pepsin & HCl corrosion, NSAID, and H. pylori can exacerbate it
Treated the same as Gastritis,
Small Intenstine - Anatomy
Duodenum - 10 inches, right after the stomach
Jejunum - 8 feet, right after Duodenum, “90% of absorption of nutrients”
Ileaum - 11 feet, right after Jejunum, (opens into the Cecum, a pouch-like structure that is the beginning of the colon, where the appendix is found)
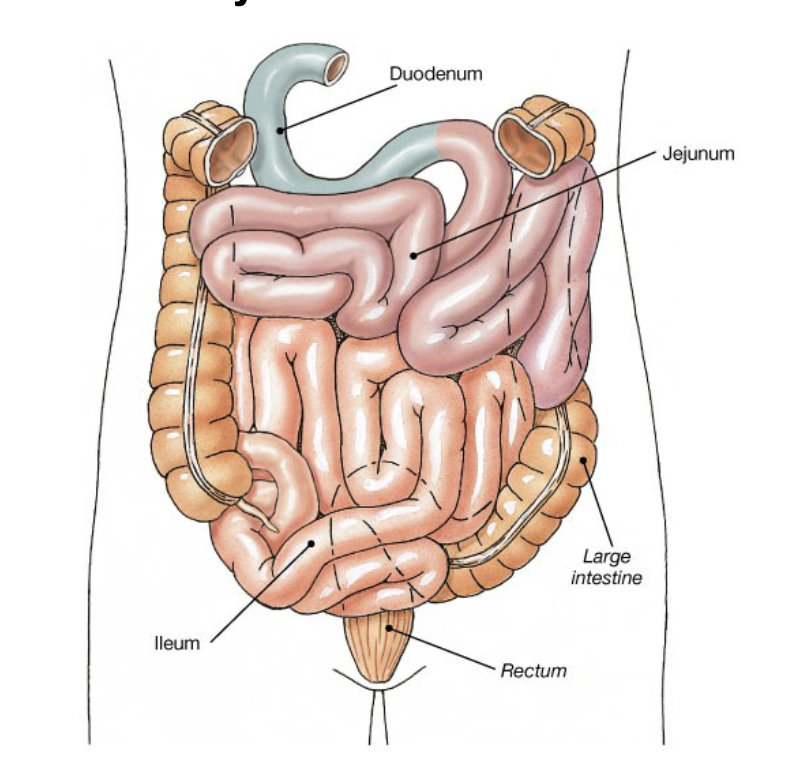
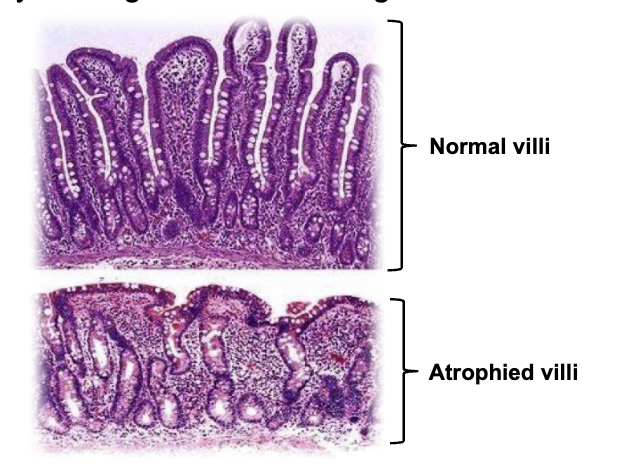
Inside the SI, they have large circular folds called Plica (mucosa and submucosa). These plica have smaller folds on them called Intestinal Villi (mucosa), these Villi have microvilli on the individual simple columnar epithelium.
*only 2 layers of muscle (inner circular, outer longitudinal)
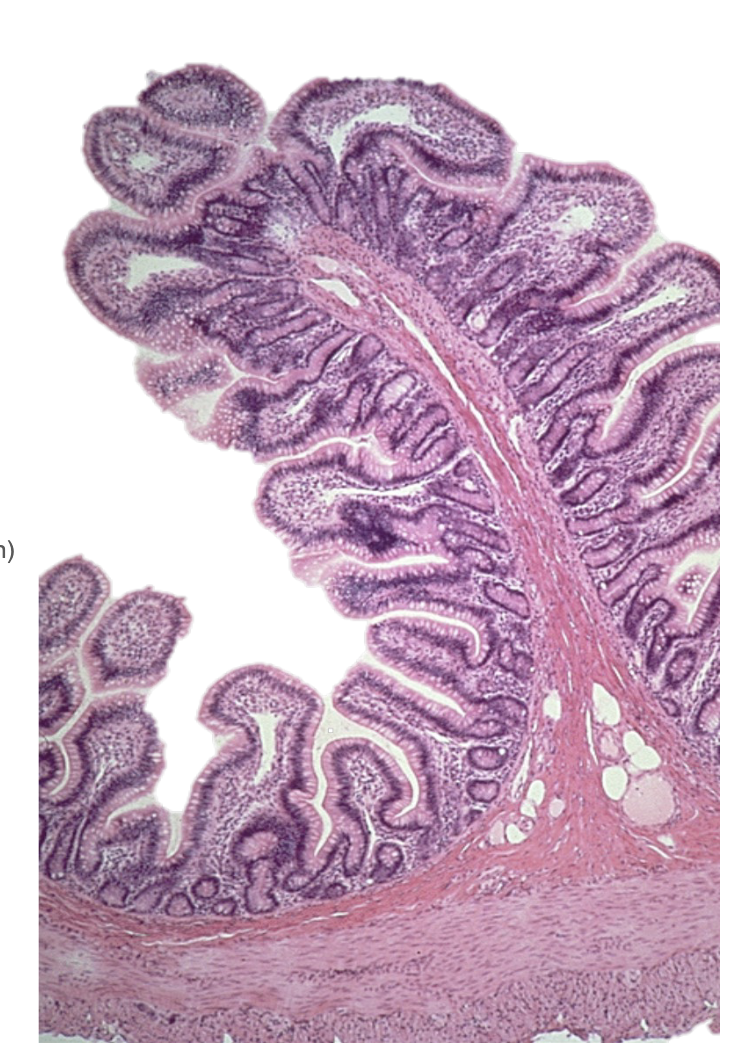
Inbetwen each Villi, there are invaginations (dips in mucosa) where the intestinal glands are found called Crypts of Lieberkühn
Small Intestinal Glands - Crypts of Lieberkühn
*90% of all digestion happens in the SI (specifically the Jejunum)
Golbet Cell = (mucus)
Enteroendocrine Cell = (SMILK)→ shuts the stomach down through negative feedback
S - secretin (induced by low pH) simulates Centroacinar Cells, Biliary, and Brunner’s glands to secrete bicarb. Also inhibits parietal cells.
M - motilin (induced by pH 5) stimulates interdigestive migrating contractions (IMCs) which sweep bacteria, aka cleanse itself.
I - cholecystokinin (CCK) (induced by food) stimulates pancreatic acinar cell secretion, bile production/excretion, relaxes the Sphincter of Oddi, ⬇ NPY indirectly, and inhibits gastric activity.
⬇ - (stimulate beta cells to produce insulin before glucose enters the blood, “feedforward”)
L - GLP-1 (glucagon-like peptide) (induced by glucose) stimulates insulin release, ⬇ NPY *GLP-1 agonists are Ozempic (weight loss + type 2 diabetes) = gastroparesis (delayed emptying)
K - GIP (glucose-dependent insulinotropic polypeptide) (induced by glucose), same as GLP-1 essentially.
Paneth Cell = (antimicrobics)
Accessory Glands ( Gallbladder, Pancrease and Liver)
Bile = breaks down lipids
pH of the Small Intestine is ≈ 8. Gets buffered by bicarb. released from Brunner’s Glands and Biliary Ductular Cells.
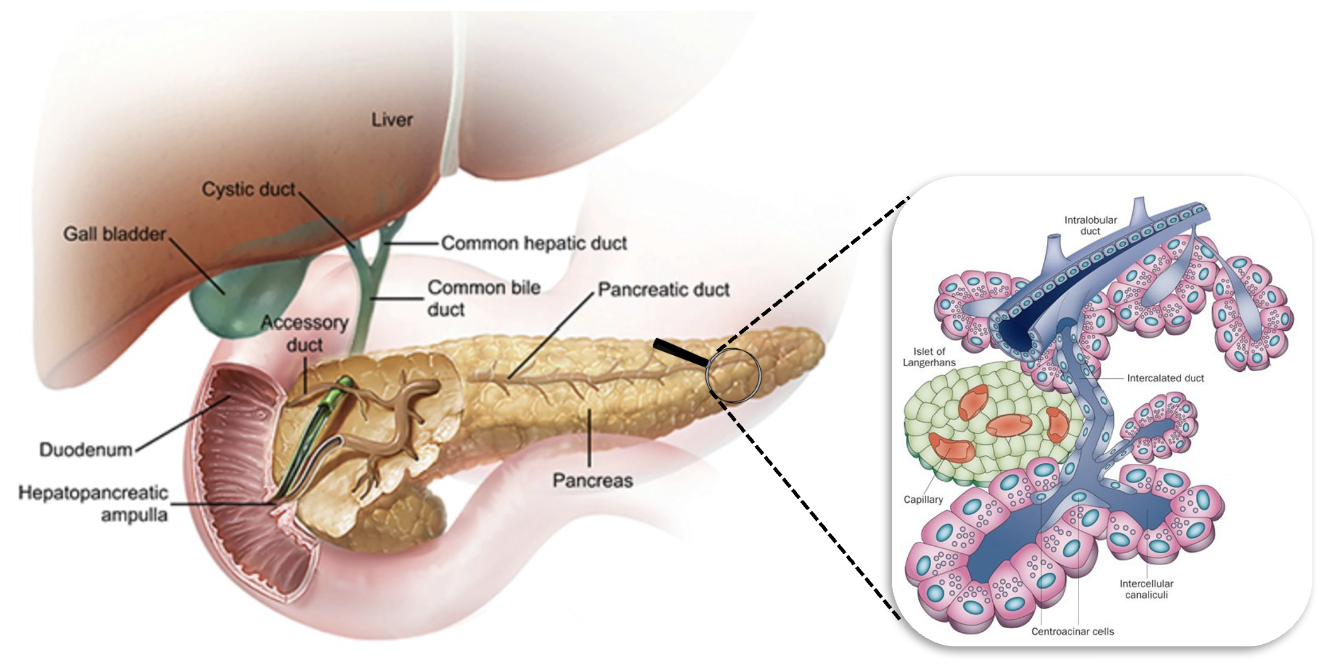
Sphincter of Oddi - Regulates bile secretion into the Duodenum.
Liver - creates the bile
Pancreas - 99% exocrine - releases digestive enzymes, acini release all the digestive enzymes in inactive forms, they become active in the SI. The Centroacinar cells release bicarbonate, aiding in the buffer.
Gallbladder - the muscular sack that concentrates and pushes bile through the Sphincter of Oddi
*type 1 diabetes, sometimes take digestive pills bc of a faulty pancreas
Small Intestine - Mechanical and Chemical Digestion
Mechanical - peristaltic wave contractions to propel wastes toward the colon
Chemical - from exocrine acini in pancreas: Trypsinogen, Chymotrypsinogen, Procarboxypeptidase A&B, Pancreatic Amylase, Pancreatic Lipase, Colipase, Ribonuclease; pH optima ≈ 8.
PANCREASE JUICE 👆 👆👆 👆👆 👆👆 👆
*Small Intestine Brush Borders: brush border enzymes (dextrinases, disaccharidases, and peptidases) perform terminal digestion, and enterokinase activates trypsinogen
Hepatic Portal System
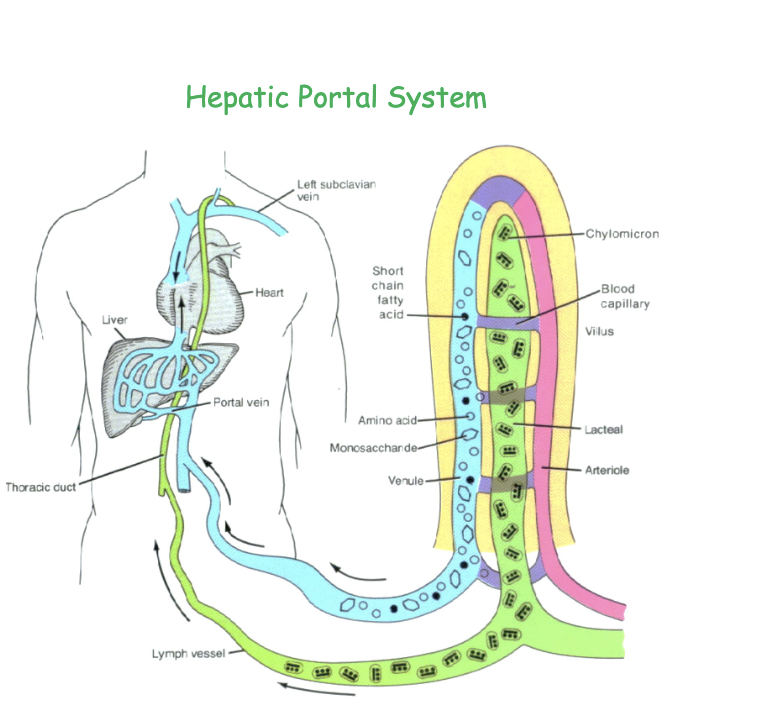
All nutrients absorbed go through the liver first, then the heart.
Lipids bypass the pathway, going straight to the subclavian (lymph vessels) as they are too big.
Celiac disease
Genetic condition: nausea, vomiting, diarrhea, abdominal pain, malnutrition, and anemia,
Gluten essentially gets into the wall of the intestine, where it doesn’t belong, and causes an immune reaction. Causes a bunch of damage to the epithelial lining.
Apendix
feces gets into appendiz and causes:
Appendicitis (inflamed) → Peritonitis (bacteria from burst appendix in peritoneum) → Sepsis (bacteria in blood)
Large Intestine + Inflammatoru Bowel Diseases
Large Intestine reabsorbs water, and ions electrolytes, B12. It compacts feces, and adds tons of mucus making it sticky.
Haustra (sac-like colon) → due to the 3 straps of muscle, taenia coli. This creates better storage and faciliate segmentation. facilitates
IBD - chronic inflammation and ulceration of the bowel
Crohn’s disease - mostly SI - diffuse disease (patches of irritation)
Ulcerative Colitis - mostly LI - irritation throughout the colon
Treated with anti-inflammatory drugs (5-ASAs, corticosteroids, immunosuppressants)
Diverticulitis + Colon Cancer
If feces/bacteria get into the colon out-pouching called (diverticula), it is (diverticulosis), but if it gets inflamed, it is (diverticulitis). This will cause rectal bleeding, scar tissue, and abdominal pain.
Treatment: (mild) antibiotics and surgical resection (severe)
Colon cancer affects individuals with IBDs, family history, smokers, and diet. Usually begins with small (benign) polyps. Rectal bleeding and rapid weight loss are signals. 91% 5-year SR if localized.
Treatment: chemotherapy, radiation, bowel reconstruction, surgical resection
Importance of Dietary Fiber
Essentially pushes against walls of Large Intestine, making it flex. Which makes feces more voluminous. If not, can super easily cause diverticulosis.
Male Repro. Anatomy
Scrotum: an outpouching of the Abdominal Cavity
Tunica Vaginalis: outpouching of the Peritoneal Cavity
S- Seminiferous Tubules
E- Epididymus
V- Vas defrons
E- Ejaculatory Duct
N- nothing
U- Urethra
P- Penis
*regulates heat using Pampiniform Plexus (countercurrent heat exchange) & using the Dartos smooth muscle (wrinkly) + Cremaster Muscle (testes ↑ and ↓)
Seminiforus Tubulers
highly confulated tubules lined by a seminiferous epithelium (400m long)
contains spermatogenic cells (developing sperm) and Sertoli Cells (Nurse Cells)
surrouned by loose CT containg vasculature and interstiail cells of Leydig (testosterone)
Sertoli Cells
transverse the entire wall of the seminiferous tubule, creating tight junctions between the basal and adluminal compartments. This allows for the blood-testis barrier, which allows basal cells to create clones without the immune system attacking the “foreign” clone.
secrete luminal fluid (semen)
produce ABP (holds testosterone in high concentration)
produce (AMH/MIS) —> makes sure Mullerian Ducts (female) don’t develop, only Wolffian Ducts (male)
produce Inhibin (negative feedback)
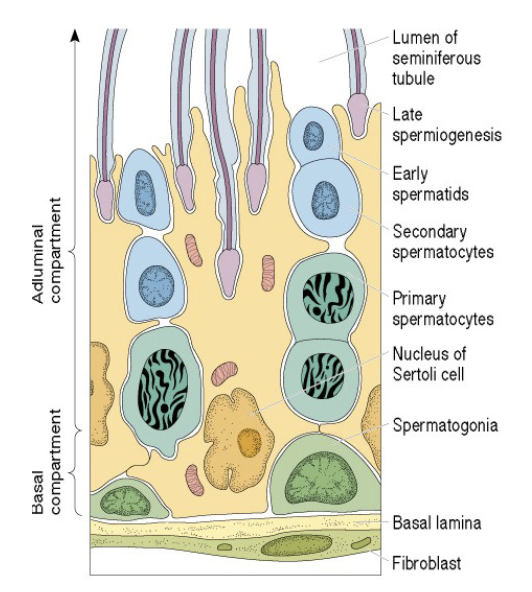
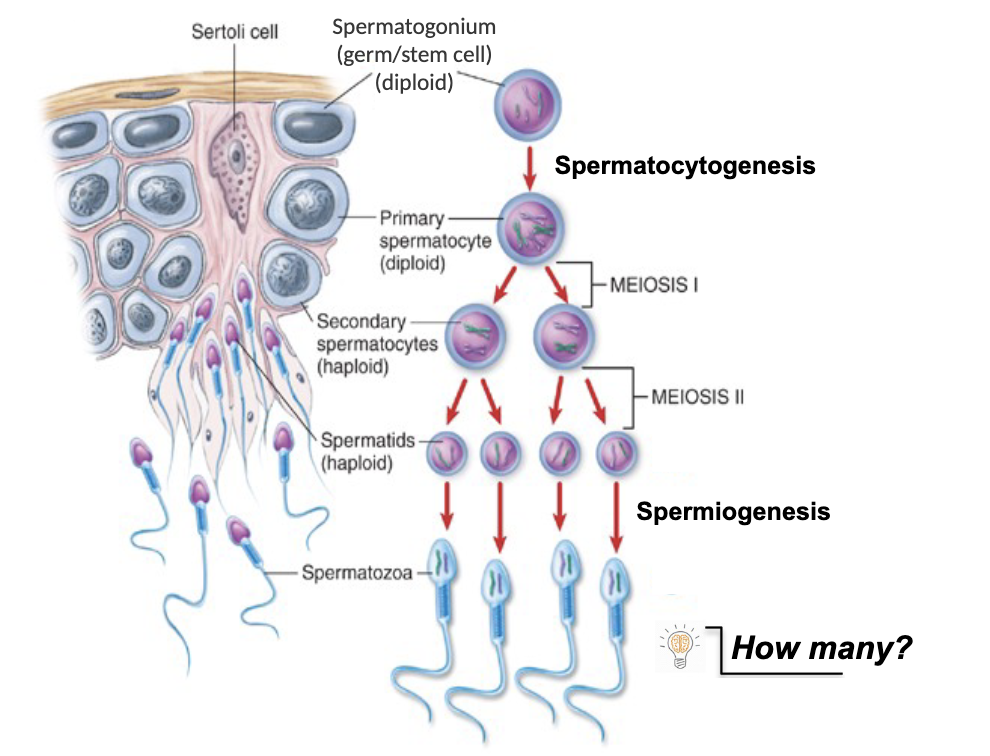
Spermatogenic cells + Order of Division
1) Spermatogonia 2) Primary Spermatocytes 3) Secondary Spermatocytes 4) Spermatids 5) Spermatozoa
-born with diploid Spermatogonium
Spermatocytogenesis = the process of Spermatogonia (diploid) becoming primary Spermatocytes (diploid)
Spermiogenesis = the process of spermatids (haploid) becoming mature sperm
≈ 10 million sperm are made each day
Gential Ducts - Testes
Seminiferous tubules open up to the tubuli recti → transport sperm to the rete testis
Rete testis (collects + transports) sperm to efferent ducts that reabsorb Sertoli Cell secretion and (concentrate + compact) sperm
Efferent ducts send sperm to the epididymus (reach motility but are incapacitated by glycerophosphocholine)
Epididymus → vas defereons → ejaculatory ducts
Male Repro. - Glands
Seminal Vesicles - join the vas deferens just about the prostate, create fructose-rich seminal fluid and semenogelins (sticky), ≈ 70% of the total semen volume
Prostate - produces alkaline-rich buffer seminal fluid and prostate-specific antigen (PSA), which liquefies semen in female repro. tract, ≈ 30% of the total semen volume *elivate PSA is a sign of Prostate Cancer
Bulbourethral (Cowper’s) gland - produces pre-ejaculate, cleanses and lubricates the urethra. (not part of semen technically)
Penis Anatomy + Erection
contains three columns of erectile tissue: two dorsal columns (corpora cavernosa) and one ventral column (corpus spongiosum), urethra is found here
These are vascular spaces that can easily fill with blood
During the flaccid state, increased SNS activity decreased blood flow to penis, blood is shunted away from penis via ateriovenous (AV) shunt
During the erect state, decreased SNS activity, increased PNS activity and increase blood flow to penis (NO mediated), more blood goes to penis (not the shunt) → Swells and blocks of the drain (allows for a sustained erection)
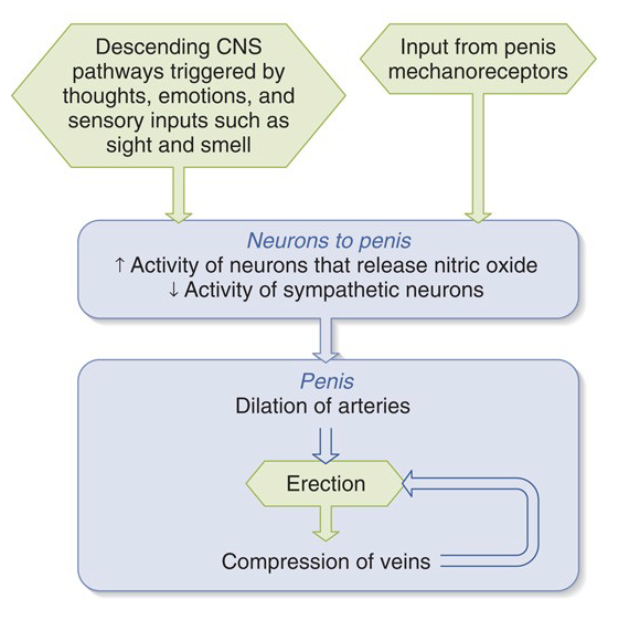
PNS Innervation of the Penis + Erectile Dysfunction
Ach binds to M3 Receptors which activates Ca2+/calmodulin which activates NO synthase → diffuses to smooth muscle cells, stimulates Guanlyate cyclase (GTP → cGMP), cGMP inhibits myosin light chain kinase therefore relaxes blood vessel, increase blood flow.
Viagra/Cialis inhibit PDE (degrades cGMP) so long erection occurs
Ejaculation (spinal reflex) is mainly due to the bulbospongiosis muscle
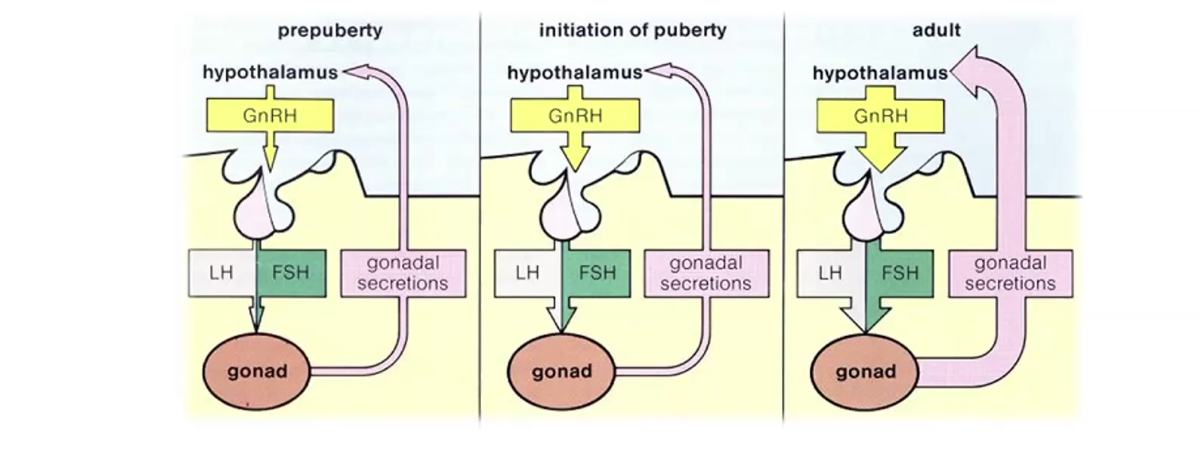
Male Repro. Endocrinology + Testosterone
LH stimulates testosterone production
FSH stimulates spermatogenesis
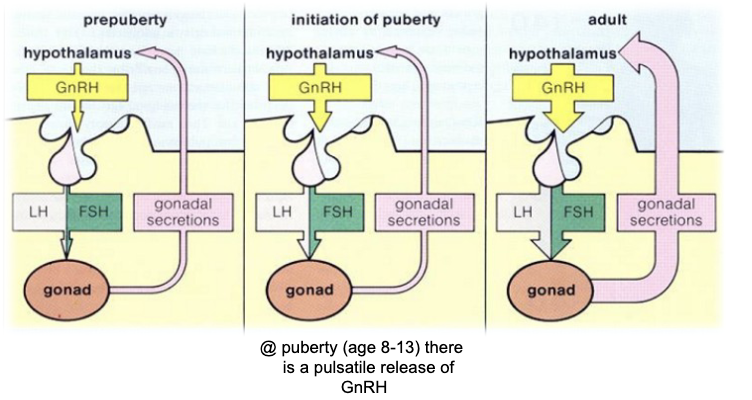
Prepuberty, GnRH release, which causes the release of LH and FSH (no negative feedback)
During Puberty, there are bursts of GnRH which cause larger secretions of LH and FSH, sensitive negative feedback that stabilizes the hormones.
Adults, even more GnRH and extremely sensitive negative feedback.
Sertoli cells release inhibin, which inhibits FSH
Leydig cells release Testosterone, which inhibits LH
Testosterone is converted to dihydrotestosterone (DHT), a more potent form of testosterone, in the prostate via the enzyme 5 ⍺-reductase.
A male with a 5 ⍺-reductase deficiency will have normal reproductive tract development, but abnormal development of external genitalia (ambiguous genitalia).
Too much test. can cause test. to be converted to estradiol (estrogen) in Sertoli cells via the aromatase enzyme.
*Adrenal hormones (DHEA, androstenedione) help create secondary sex characteristics prior to the maturation of the hypothalamus
Renal - Kidney Anatomy
Cortex - contains Bowman’s Capsule / Gloomerules, DCTs and PCTs
Medulla - contains Loops of Henley, and Collecting Ducts
Renal Papilla → Minor / Major calyx drain into Renal pelvis which drains to Ureter
Cortical / Juxtamedulary Nephrons
Nephrons contain renal corpuscle (Bowman’s + glomerulus), which is the site of blood filtration. Vasular Pole (where the afferent arteriole enters) and Urinary Pole (where PCT starts).
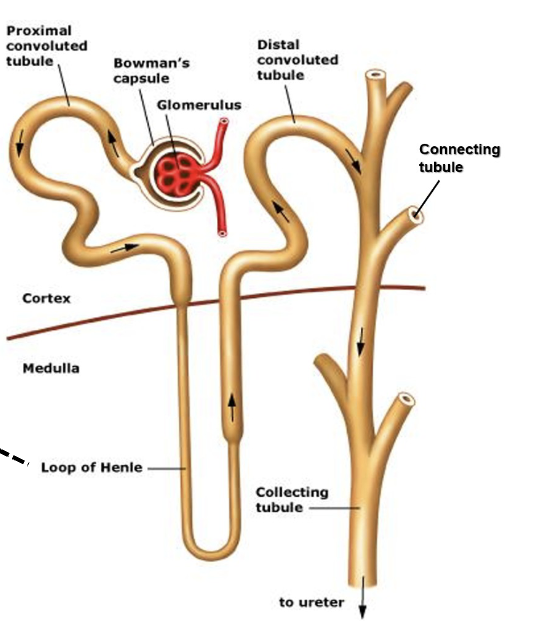
DCT: no burshborders (microvilli) → site where regulation of Na + K
PCT: Contains Brushborder (microvilli) → reabsorbs large amounts of water
Cortical: filters blood and forms urine (Cortex Mainly), the short Loop of Henle
Juxtamedullary: flood blood and form urine, but mainly move salt and urea (50%) into medullary tissue “creates osmotic gradient” for water absorption (Medulla mainly)
Renal Vasculature - Reabsoroption
Renal artery → Segmental artery → Interlobar artery → Arcuate artery → Interlobular artery → Afferent arteriole → Glomerulus → Efferent arteriole → Perritubular capillaries → Vasa recta(only in juxtamedullary) → Interlobular vein → Arcuate vein → Interlobar vein → Segmental vein → Renal vein
Perritubular capillaries reabsorb nutrients in the PCT, and the Efferent arteriole keeps the kidney alive
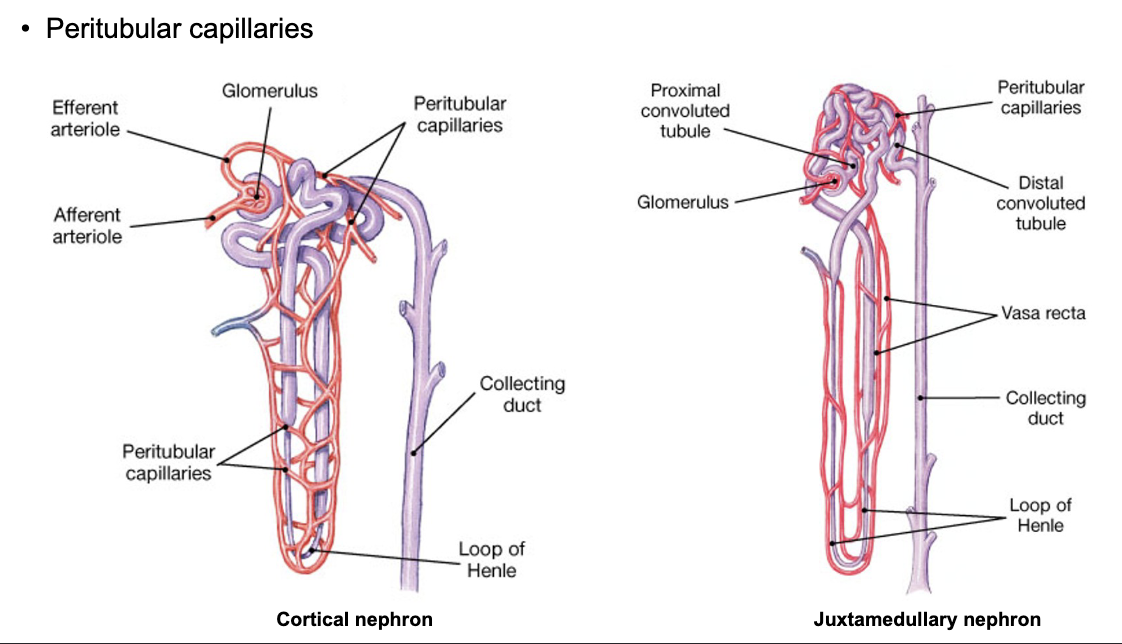
1) Glomerular filtration (filtration in the glomerulus)
2) Tubular reabsorption: Reabsorption occurs between the PCT and the Peritubular Capillary (Tubular fluid → Paritubular fluid → Intravascular fluid)
3) Tubular secretion (moves drugs/toxins into the DCT from the IVF, to be excreted)
4) Excretion
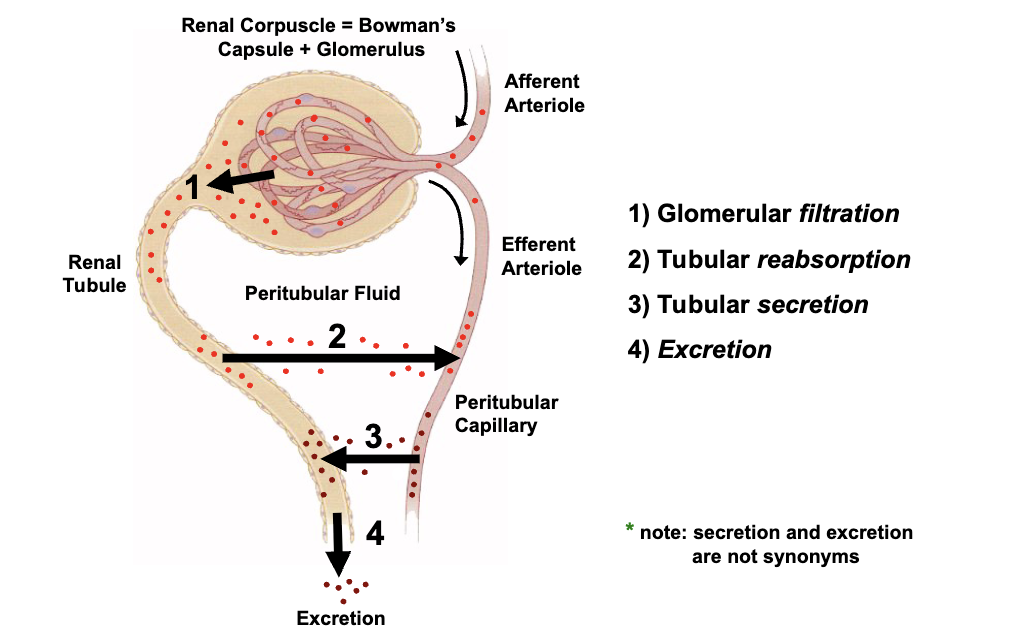
*Secretion involves the release of useful substances within the body, while excretion involves the removal of waste products from the body.
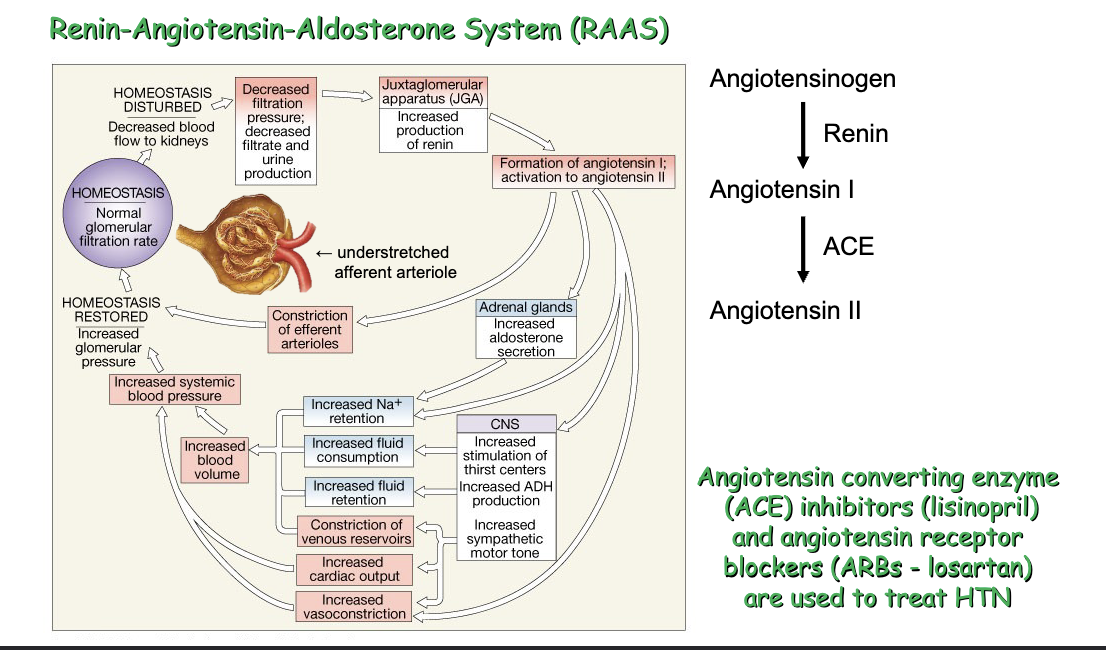
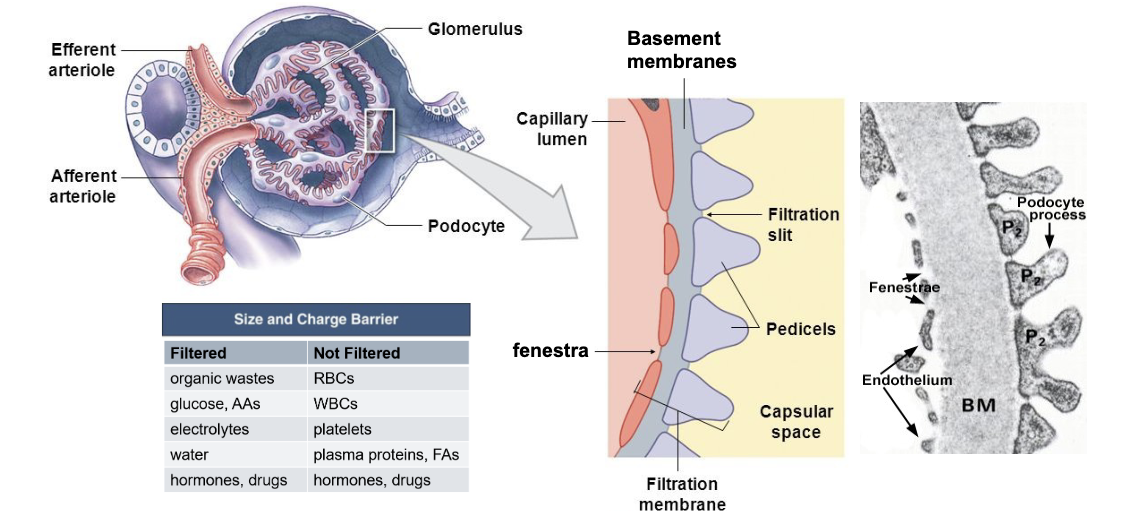
Bowman’s Capsule + Glomerular Filtration Membrane (RAAS / Renin)
Paretial membrane (Bowman’s) is made of Simple Squamous Epithelium while Glomerulus is made of Podocyctes w/ pedicles that create filtration slits. Juxtaglomerular (JG) Cells are at the vascular side and secrete renin when low BP is sensed.
Renin converts Angiotensinogen (liver) → Angiotensin I -(ACE)→ Angiotensin II, which regulates BP, stimulates thirst, stimulates release of ADH, and helps the zona glomerulosa secrete Aldosterone—released in response to DECREASED BLOOD PRESSURE.
ANG II directly stimulates the release of aldosterone
Blood thinners include Lisinopril (ACE inhibitor) and ARBs (block ANG II receptors)
Glomerular filters by size and polarity. They have a capillary endothelium (visceral), basement membrane x2, and podocyte. (RBCs, WBCs, Platelets, and Fatty Acids aren’t filtered)
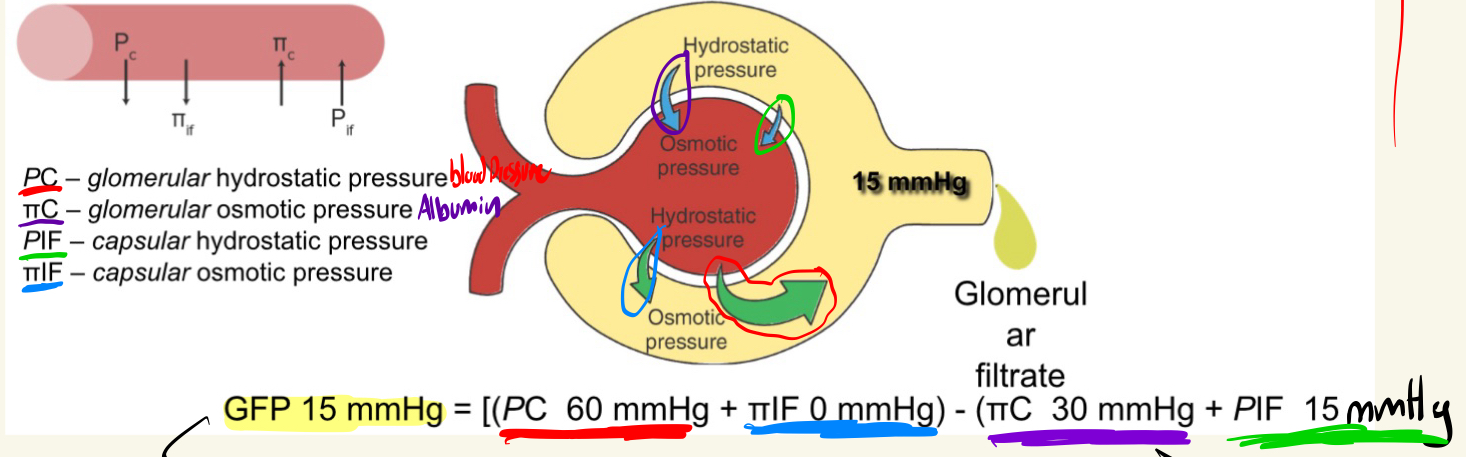
Renil Starling Forces
Capillary hydrostatic pressure drives water/solutes across the glomerular filtration membrane and into Bowman’s capsular space
*180 L/day of plasma gets filtered, but 178 L/day gets reabsorbed
GFP 15 mmHg = [(PC 60 mmHg + πIF 0 mmHg) - (πC 30 mmHg + PIF 15 mmHg)]
Hemodialysis + Inulin (Glomerular Filtration Rate)
AV fistula is made for a high flow environment + low clotting.
“the volume of plasma filtered (by both kidneys) per minute”
*The rate at which inulin is cleared from the body is the glomerular filtration rate. This is the “Gold Standard of Kidney Function.”
Autoregulation of GFR

PCT Reabsorption
Reabsorbs:
50% of urea
100% glucose, AAs, vitamins
65% H2O
Secondary Active Transport moves glucose, AAs and vitamins from the Tubular Fluid → Peritubular Capillary
*caffeine and theophylline(tea) causes diuresis by inhibiting Na+ and H2O reabsorption in the PCT
*Jaundiance (SGLT-2 Inhibitors) blocks secondary transport (can’t reabsorb glucose)
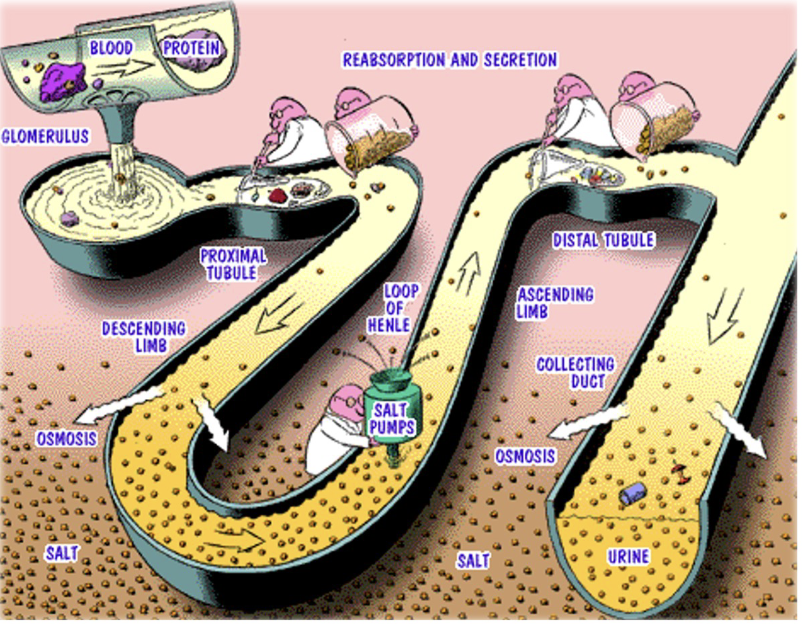
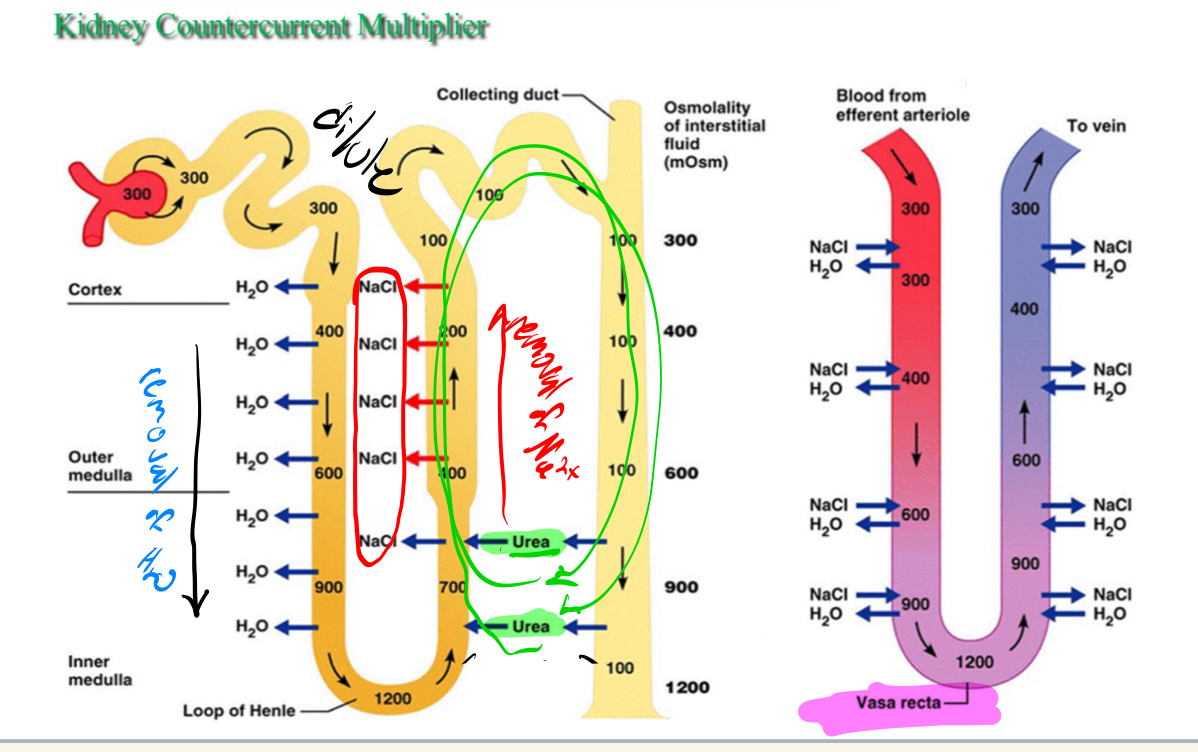
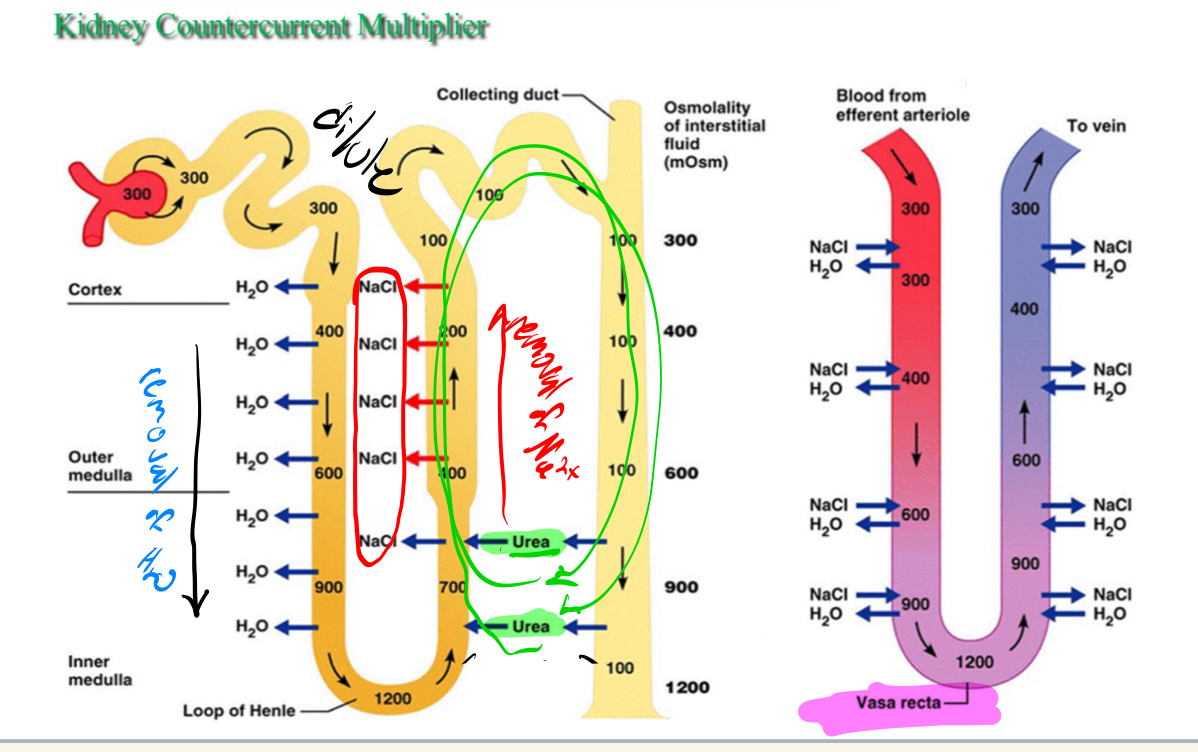
Acending and Decending Loops of Henle
JUXTAMEDULAR NEPHRONS
Descending: only permeable to water (20% absorbed), Na2+ isn’t absorbed here. This causes more and more concentrated solute concentration descending the Loop of Henle.
Ascending: (TAL → NKCC2,symporter NOT a pump) only permeable to Na2+
*50% of urea leaves the Collecting Duct and adds to the osmotic gradient; the urea loop occurs between the Ascending Loop of Henle and the Collecting Duct
*Loop diuretics (Lasix) inhibit NKCC2s, can’t absorb as much water (20%), ⬇ BP ==== Can still absorb 65% from PCT
Collecting Duct: AVP Regulates reabsorption of water
Vasa Recta is permeable to both H2O and Na2+ and is superimposed on the Loop of Henle, maintaining salt conditions in the medulla.
DCT
Aldosterone up-regulates sodium/potassium pumps.
Na/K ATPase pumps are on the outside of DCT cells, and Na/Cl symporters are on the inside. → water is dragged in blood from Na/K ATPase → Na/Cl symporters.
*Thiazide (Na/Cl symporter inhibitor), a decrease in BP occurs. “water pill”
- Can cause hypokalemia, low Potassium in blood → possibly life-threatening → created aldosterone antagonist: decreases Na/K ATPase activity causing decreased H2O → created amiloride: blocks sodium channel causing decreased H2O
spironolactin + amiloride (can be taken for acne: ⬇ BP, and 🔼 HR)
Blood Volume / Pressure Regulation
*ADH/AVP is tonically released, causing reabsorption of water in the Collecting Duct (tells them to put aquaporins in the membrane to reabsorb water)
High solute concentration in blood (dehydration) → Supra Optic neurons sense (alcohol can inhibit) → ADH is sent → binds to collecting ducts to put aquaporins in the apical membrane (reabsorb water)
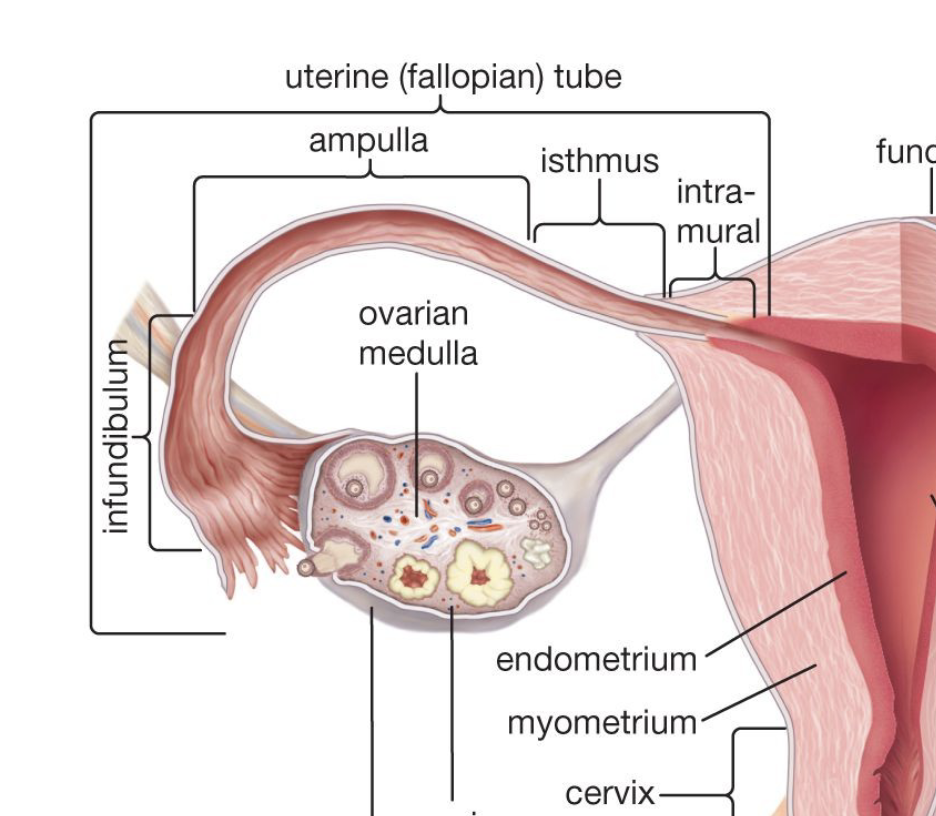
Ovaries - Eggs
Ovaries: Cortex (oogenic cells, developing eggs) and Medulla (loose connective tissue)
Cortex: contains oogonia (germ(stem) cells), developing ovarian follicles
Follicle: an oocyte surrounded by support cells that are called follicular cells, also surrounded by stromal cells (CT cells)
“Oagonium = egg = oocyte” —- “follicle contains an egg”
Eggs develop in the yolk sac, mitotically divide, and migrate to the ovarian cortex
≈ 7 million eggs to start → at birth, only ≈ 1 million → because of follicular atresia at menarch, only ≈ 300,000 remain → essentially 450 oocytes to work with.
Oocytes get stuck in meiosis I (prophase) and can’t divide until ovulation, where they develop to meiosis II and get stuck again.
Female Repro. - Endocrinology
Similar endocrinilogy for males/females: GnRH (8-13). Chilhood obecity causes a lower age of menarche.
*need a 12% body fat to initate puberty (menarche)
Leptin(fat) → KISS1 → GnRH → LH and FSH
Follicular Development - Order + Description
Primordial follicles - Primary follicle (only when the cells that surround the oocyte become cuboidal are the cells called Granulosa Cells) → Secondary follicle → Tertiary follicle (have an antrum (hormone-filled sacs)) → Mature follicle → Ovulation
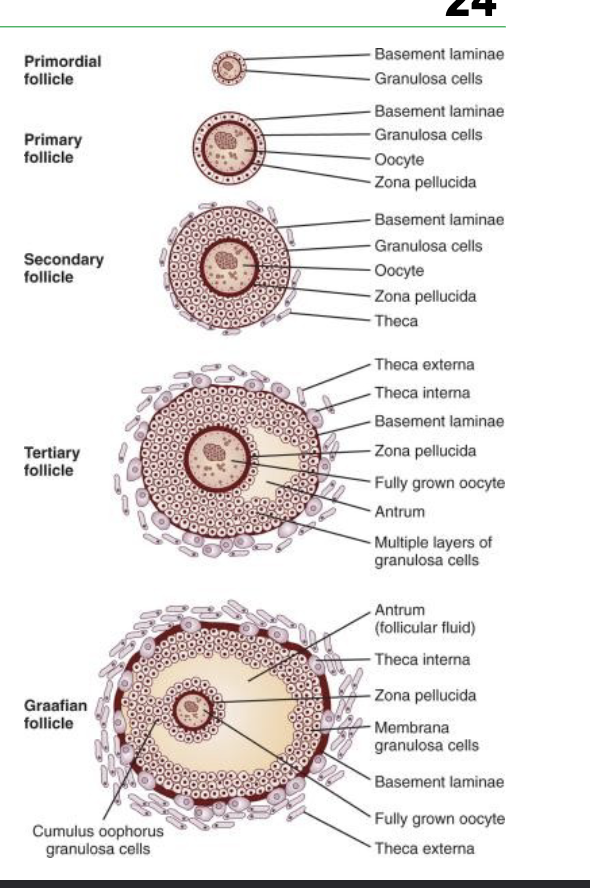
Primary follicles - DOESN’T need FSH, become granulosa cells (cuboidal) → Stroma cells surround primary follicles, forming the theca interna (secretes androstenedion) and the theca externa (Connective Tissue)
Secondary follicles - need FSH (WHY non-dominant follicles expereince ATRESIA, decreased FSH Concentration) → secrete liquor folliculi (estrogen, progesterone, inhibin) which regulates FSH/LH “selection and dominance between eggs”
*Inhibin decreases FSH
*Estrogen decreases FSH
*Progesterone decreases LH
functions as a temporary endocrine organ
Tertiary (Antral) follicles - FSH needed - theca and granulosa cells undergo hyperplasia
Granulosa cells become Cumulus Oophorus (surrounds the primary oocyte) and Mural Granulosa (around the liquor of the folliculi)
creates fluid-filled spaces (antrum)
Mature (Graafian) follicles - FSH needed - further theca and granulosa cell proliferation - Cumulus Cells detach from Mural Granulosa Cells
Once fully detached, it is now in Meiosis II ( secondary oocyte)

Ovulation
Ovulation starts with the release of the 2º oocyte from the Graafian follicle, it starts when FSH stimulates theca interna cells to express LH Receptors.
LH stimulates steroidogenic cells to produce androgens (converted to estrogen in granulosa cells)
Estrogen increase causes a surge of LH on the 14th day, causing Ovulation
LH surge: 1) secretes (MIS), moves 1º oocyte to 2º oocyte
2) Loosen mural granulosa, loses blood supply, eventually ruptures, which leads to the release of the egg from the ovary on the 14th day
3) Remnant of the Graafian follicle becomes the corpus luteum, then the corpus albicans
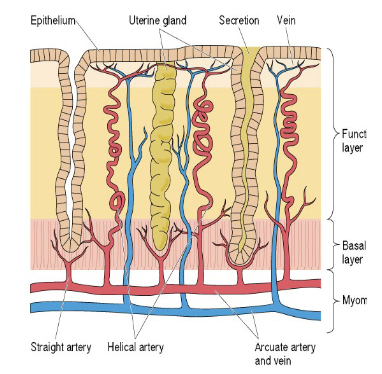
Uturus - Anatomy
The uterus has 3 layers: Perimetrium, Myometrium (muscle), Eand ndometrium (glands & vasculature)
Endometrium has 2 layers - Functional Layer (lost in menstrual flow) and Basal Layer (stem cells)
Fallopian tube has the ampulla (lined with cilia that move the ovum to the uterus and PEG cells that capacitate sperm to fertilize) and infundibulum ( finger-like structure that catches the egg released from the ovary during ovulation)
Fertilization
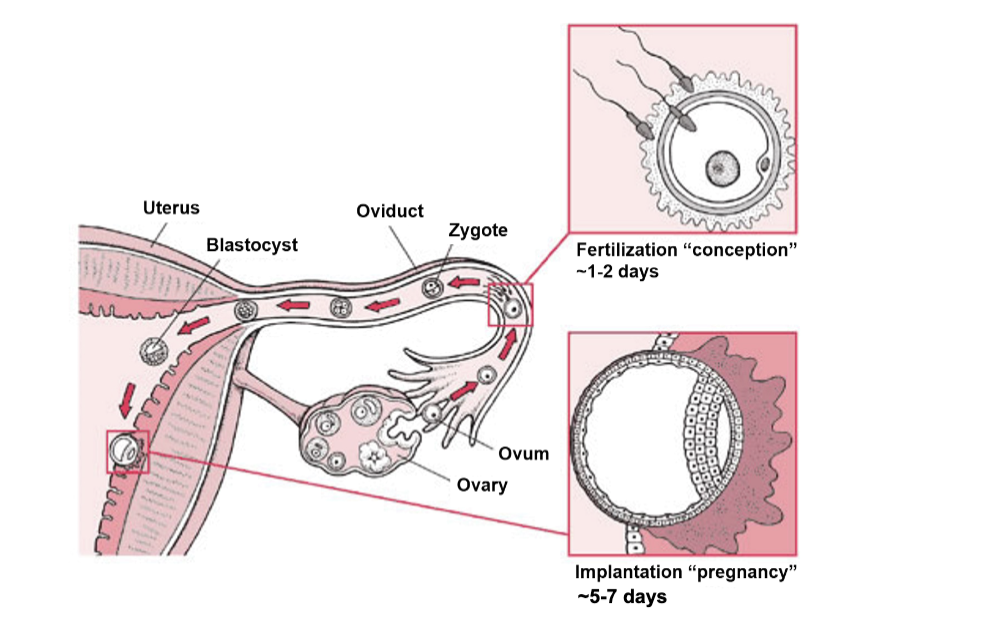
1) 2º Oocyte w/ cumulus is picked up by the fimbrae of the oviduct
2) oocyte gets fertilized in the Ampulla within 1-2 days of ovulation
3) fetillized ovum develops into a zygote → embryo
*fertility is peak -2 days from ovulation as sperm as time to “stage” and has a better chance to actually fertilize the egg in that (12-48hr) window
Graafian (Mature) follicle and Corpus Luteum
The Graafian follicle becomes a Corpus Luteum after ovulation
The follicle secretes a lot of estrogen and less progesterone
Corpus Luteum secretes a lot of progesterone and not a lot of estrogen
Corpus Luteum is composed of granulosa-lutein cells and theca-lutein cells
Granulosa-lutien and Theca-lutien cells produce progestreone and androgens
*progesterone inhibits LH, which induces degradation of the corpus luteum → self-destructive process
*Estrogen and inhibin inhibit FSH, which prevents new follicular development
*What rescues the corpus luteum from itself is hCG (human chorionic gonadotropin), which is only released by an embryo (fertilization must occur)
Pregnancy
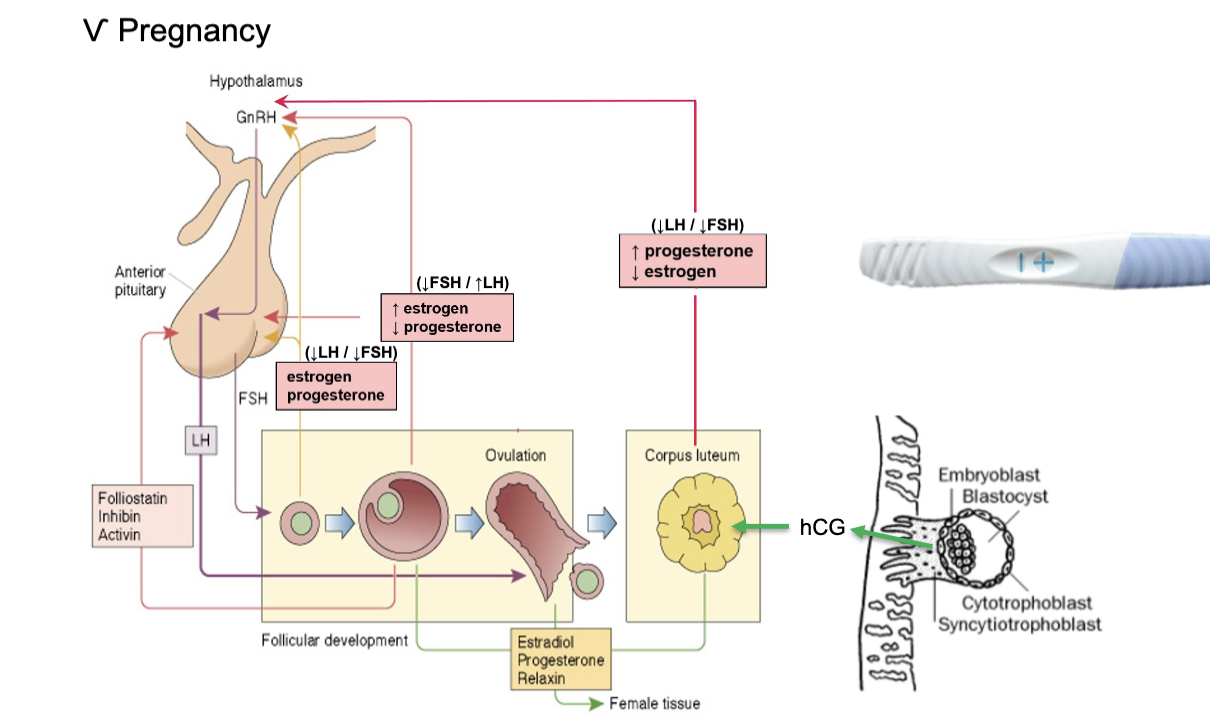
1) FSH: stimulates theca interna cells to produce LH receptors
2) LH: then binds to these receptors, producing androgens (estrogen in granulosa cells)
3) Estrogen: surges, that cause LH Surge (Ovulation) → Corpus Luteum (remnant of Graafian cells), causing increased progesterone (“crash course due to no LH”) needs to be fertilized (hCG release) to be saved
Inhibin and Estrogen decrease FSH
Progestron decreases LH
*pregnancy testers test for hCG in urine
Menstration and the Mebnstraul Cycle
*The birth control pill (COCP) is made of estrogen and progesterone (inhibits FSH & LH) → can’t ovulate
*Plan B is made of only progesterone (can’t ovulate)
*RU 486 (abortifacient) is a progesterone receptor antagonist which causes a menstrual flow