BPK 205 Midterm 3
1/192
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
193 Terms
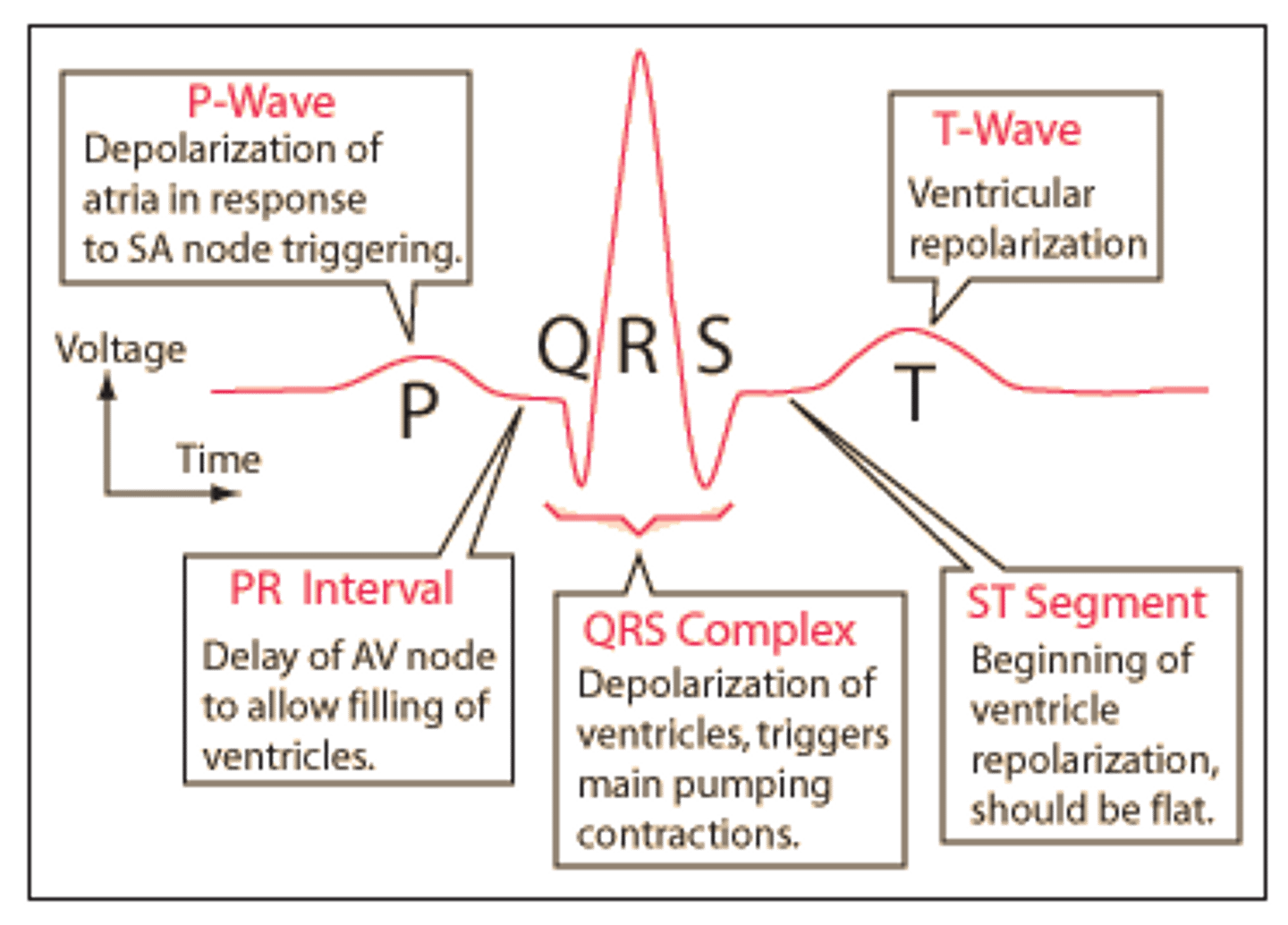
Draw & label an ECG
What does an ECG represent
Summed electrical activity of all cells recorded from the surface of the body
What does the P wave represent
- Atrial depolarization
What does the QRS wave represent
- Ventricular depolarization
What does the T wave represent
- Ventricular repolarization
What is tachycardia
- HR faster than normal (>100 BPM)
What is bradycardia
- HR slower than normal (<60 BPM)
What is fibrillation
- ECG is disorganized
Is atrial fibrillation extremely problematic?
- No, the heart can still function as a pump b/c most blood flow into ventricles is passive
Is ventricular fibrillation problematic?
- Yes, the heart cannot function as an effective pump
Systole vs. Diastole:
- S: Rhythmic contraction of chambers
- D: Rhythmic relaxation of chambers
What occurs in Atrial vs. Ventricular systole:
- A: Blood is pumped from atria to ventricles
- V: Blood is pumped from ventricles to aorta/pulmonary artery
Describe the 5 events in 1 cardiac cycle
*See notes for details
- Late diastole, Atrial systole, Isovolumic ventricular contraction, Ventricular ejection, Isovolumic ventricular relaxation
What is end diastolic volume
- The volume of blood in the ventricles at the end of ventricular diastole
What is the end systolic volume
- The volume of blood left in the ventricles at the end of ventricular ejection
What does wigger's diagram combined?
- ECG, pressure, heart sounds and volume
What causes first heart sound?
- Bicuspid valves slamming shut at the end of atrial systole
What causes the second heart sound?
- Aortic semilunar valve closing at the end of ventricular systole
What is an isovolumic contraction
- Build up of ventricular pressure without changing vol.
What is isovolumic relaxation
- Ventricles are emptied and relaxation results in decreased pressure
- Eventually closes aortic & opens bicuspid
Draw & describe events of the cardiac cycle
* See notes
When does the bicuspid valve close
- In ventricular systole when the increase in ventricular pressure exceeds atrial pressure
When does the aortic semilunar valve open
- In ventricular systoles when ventricular pressure exceeds aortic pressure
What is stroke volume + equation + normal amount + what SV is proportional to
- Amount of blood pumped by 1 ventricle during a contraction
- EDV - ESV = SV
- ~ 70 mL/beat
- SV = proportional to contractile force
What is cardiac output + equation + normal amount
- Volume of blood pumped by 1 ventricle in a given period of time
- HR x SV = CO
- ~ 5 L/min @ rest
Chronotropic vs Inotropic effects
- Chronotropic: Modulation of HR by sympathetic and parasympathetic input
- Inotropic: Modulation of contractility by sympathetic input
Sympathetic vs parasympathetic effects on HR (chronotropic)
- Sympathetic: Releases norepinephrine on B1 receptors, increases HR
- Parasympathetic: Releases ACh on muscarinic receptors, decreases HR
What determines contractile force
- Sarcomere length, which is proportional to EDV
- An increase in venous return results in a need for more pressure/contractility, therefore more force
- Determined by intracellular Ca2+
What did Frank Starling say
- The heart pumps all the blood that is returned to it
What causes an increase in EDV
- Increased venous return
- Decreased HR (more time to passively fill)
How the SNS affects contractility (GPCR pathway)
- Norepinephrine binds B1 receptor
- Activates Gs protein
- Activates cAMP > PKA
- PKA phosphorylates voltage gated Ca2+ channels > Open faster > Increased Ca2+ entry from the ECF
- PKA phosphorylates phospholamban > No longer inhibits SERCA > Increases Ca2+ stores in SR, more forceful contraction, Ca2+ removed from cytosol faster, shortens duration of contraction
Describe arteries: Function (2) "Title" Structure
- Receive an propel high pressure blood flow
- Pressure reservoir
- Maintain blood flow during ventricular relaxation
- Large amounts of smooth muscle/elastic tissue
Describe arterioles: Function/structure
- Vary resistance by changing diameter
- Large amounts of smooth muscle
Describe capillaries: Function/structure
- Where exchange occurs
- Thin, 1 layer of endothelium
Describe venules: Function/structure
- Collect blood from capillaries
- Thin, some fibrous tissue
Describe veins: Function/structure/"Title"
- Maintain venous return
- Large amounts of smooth muscle, elastic tissue & fibrous tissue
- Volume reservoir
How does blood flow vary in how it's distributed in exercise vs rest
- Rest: Large amounts go to the brain, liver, digestive tract and skeletal muscle
- Exercise: Majority of blood is diverted to skeletal muscle by vasoconstriction arteries
How do pressure/resistance change in circulation
- Pressure decreases w/ distance due to friction, creates pressure gradient
- Resistance increases as the radius of blood vessels decreases
What is blood flow rate:
- Volume of blood moved past a certain point per unit of time (L/min)
What is velocity of blood flow: When does it increase/decrease?
- The distance travelled by a fixed volume of blood per unit of time (cm/min)
- Increases as flow rate increases
- Decreases as x-section area of vessels increases
What assists with venous return to the heart:
- Skeletal muscle pump: Skeletal muscle contracts, compresses veins, forces blood back towards the heart
- Valves: Prevent back flow by closing after skeletal muscle contracts
Where is blood flow the slowest, why?
- Capillaries
- Have the largest total cross-sectional area
What do pre-capillary sphincters do?
- Modify the amount of blood entering a capillary bed by opening/closing in response to local metabolic conditions
What do metarterioles do?
- Act as a bypass channel
- Divert blood flow if sphincters are closed
- Allow large materials to bypass narrow capillaries to reach venous flow
What is the purpose of the lymphatic system?
- Pick up tissue fluid which leaks into the interstitial fluid at the capillaries
- Returns fluid to venous flow via left subclavian vein
- Screens lymph at nodes to ensure there are no toxins before returning to venous circulation
systolic pressure vs diastolic pressure
- Systolic: Pressure in the left ventricle during systole ~ 120 mmHg
- Diastolic: Pressure in the left ventricle during diastole ~ 80 mmHg
Pulse pressure equation + normal value
- Systolic pressure - Diastolic pressure
- ~ 40 mmHg
Equation for Mean arteriole pressure + normal value + "title"
- Diastolic pressure + 1/3 pulse pressure
- ~ 70-110 mmHg
- Driving pressure
What is MAP proportional to?
- Cardiac output x resistance
- HR x SV x resistance
Factors that influence MAP (4)
- Blow flow distribution btwn arterioles/veins
- Resistance of flow (changing diameter of arterioles)
- Cardiac output (change HR or SV)
- Blood volume (Fluid intake/loss)
How the cardiovascular system compensates for increased blood vol
- Vasodilation and decreased CO leading to decreased BP
- Immediate response
How the Kidneys compensate for increased blood vol
- Excrete fluid into the urine therefore decreasing the blood vol & decreasing the BP
- Slow response
What is arteriole resistance proportional to
- R = proportional to Ln/r^4
- L = length, n = viscosity of blood, r = radius of arteriole
Myogenic response @ blood vessels in response to increased pressure
- Increased pressure stretches the arterioles, opens mechanically gated cation channels on smooth muscle, depolarizes, Ca2+ channels open Ca2+ enters, increased contraction
- Increased arteriole resistance, decreased blood flow, decreased pressure in vessels
Paracrine response @ blood vessels in response to increased pressure
- Acts on neighbouring cells, release of ADP causing vasodilation
Norepinephrine effect on blood vessels in response to increased pressure
- NE released from post-ganglionic sympathetic neurons, binds to alpha-1 adrenergic receptors, Gq-protein activates Phospholipase C, forms IP3, binds to IP3 receptors on SR, increased Ca2+ release, smooth muscle contracts, vessels constrict
- alpha-1 adrenergic receptors are found on vascular smooth muscle supplying skin and visceral organs, diverts blood flow to these areas in fight-or-flight
Epinephrine effect on blood vessels in response to increased pressure
- Released from adrenal medulla, binds to beta-2 adrenergic receptors, Gs-protein activates adenyl cyclase, produces cAMP, PKA, inhibits MLCK, smooth muscle relaxes, vessels dilate
- Beta-2 adrenergic receptors are found on vascular smooth muscle supplying heart, lungs and liver
Where are beta-1 adrenergic receptors found, what do they do?
- Found on cardiac muscle
- Increase contractility by increasing SV
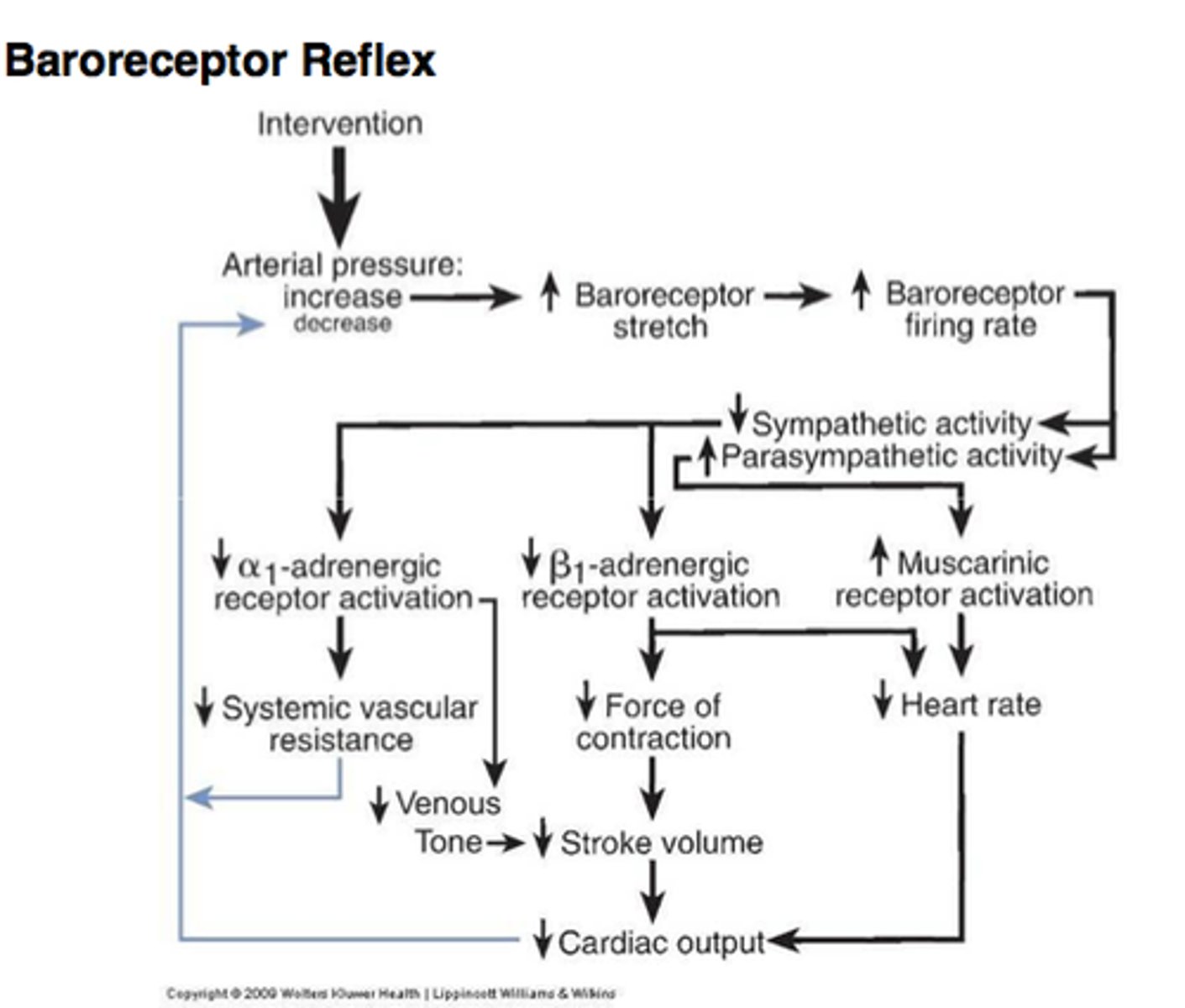
What is a baroreceptor, where are they located, what do they maintain
- Pressure "sensors"
- Located in carotid sinus and aortic arch
- Maintain homeostasis by ensuring sufficient MAP for adequate blood flow to heart and brain
Steps in the baroreceptor reflex in response to increased blood pressure (should also do it for decreased)
- Increased BP, vessels stretch, channels open, depolarization, receptor potential, AP sent to medulla which integrates info, decreases sympathetic output (NE), increases parasympathetic output (ACh)
- SNS output acts on smooth muscle (vasodilation), cardiac muscle (decreased contraction strength/CO) and theSA node (decreased HR/CO)
- PNS output acts on SA node, decreasing HR/CO
Composition of blood
- Watery extracellular matrix: plasma
- Cellular elements: RBCs, WBC, Platlets
What is a hematocrit, what are normal values for it
- % total blood vol occupied by packed RBCs
- 42% RBC, 58% plasma, <1% WBC
Where are blood cells made, what are the approx. %s produced
- Made in bone marrow of flat bones such as pelvis, spine, ribs, cranium
- 25% RBC 75% WBC
Lifespan of RBC vs WBC
- RBC: 120 days
- WBC: 6-12 hours
What is erythropoietin
- Protein that influences production/growth of RBCs. Found in the kidneys
What is thrombopoietin
- Protein that influences the production/growth of megakaryocytes (break into platelets). Produced in liver
Colony stim. factors, interleukins, stem cell factors
- growth/production of all types of blood cells, mobilize hematopoietic stem cells
What is hypoxia
- Low O2 levels in arterial blood
- Sensed by cells in kidneys, makes EPO, stimulates RBC production
What makes up hemoglobin
- 4 protein globular chains w/heme group at each centre containing porphyrin ring w/ iron
- iron binds to O2
- Each hemoglobin binds to 4 O2
What is anemia
- Either a decrease in RBCs or a decrease on functional RBCs due to low iron
- Results in a decreased O2 carrying capacity
Sources of accelerated RBC loss
- Blood loss
- RBC degradation > RBC production (genetic or acquired)
Sources of decreased RBC production
- Aplastic anemia, drugs/radiation
- Dietary insufficiencies, Iron, folic acid vit. B12
4 steps of hemostasis
- vasoconstriction
- Platelet plug formation
- Coagulation
- Dissolution of clot (fibrinolysis)
3 steps in formation of platelet plug
- Exposed collagen binds and activates platelets
- Release of platelet factors, factors attract more platelets
- Platelets aggregate and form platelet plug
Intrinsic pathway of Coagulation
- Involves plasma proteins & is initiated by exposure of collagen
Extrinsic pathway of coagulation
- Initiates due to a release of tissue factors from damaged tissue
Coagulation cascade AFTER intrinsic/extrinsic pathways
- Series of enzymes are activated which lead to activation of factor 10
- Factor 10 converts prothrombin to thrombin
- Thrombin converts fibrinogen to fibrin
- Fibrin cross-links to form a mesh that a stabilizes the platelet plug
What dissolves the clot when tissue repair is complete
- plasmin
Blood types, what antigens/antibodies do they have? What type of donor blood can they receive?
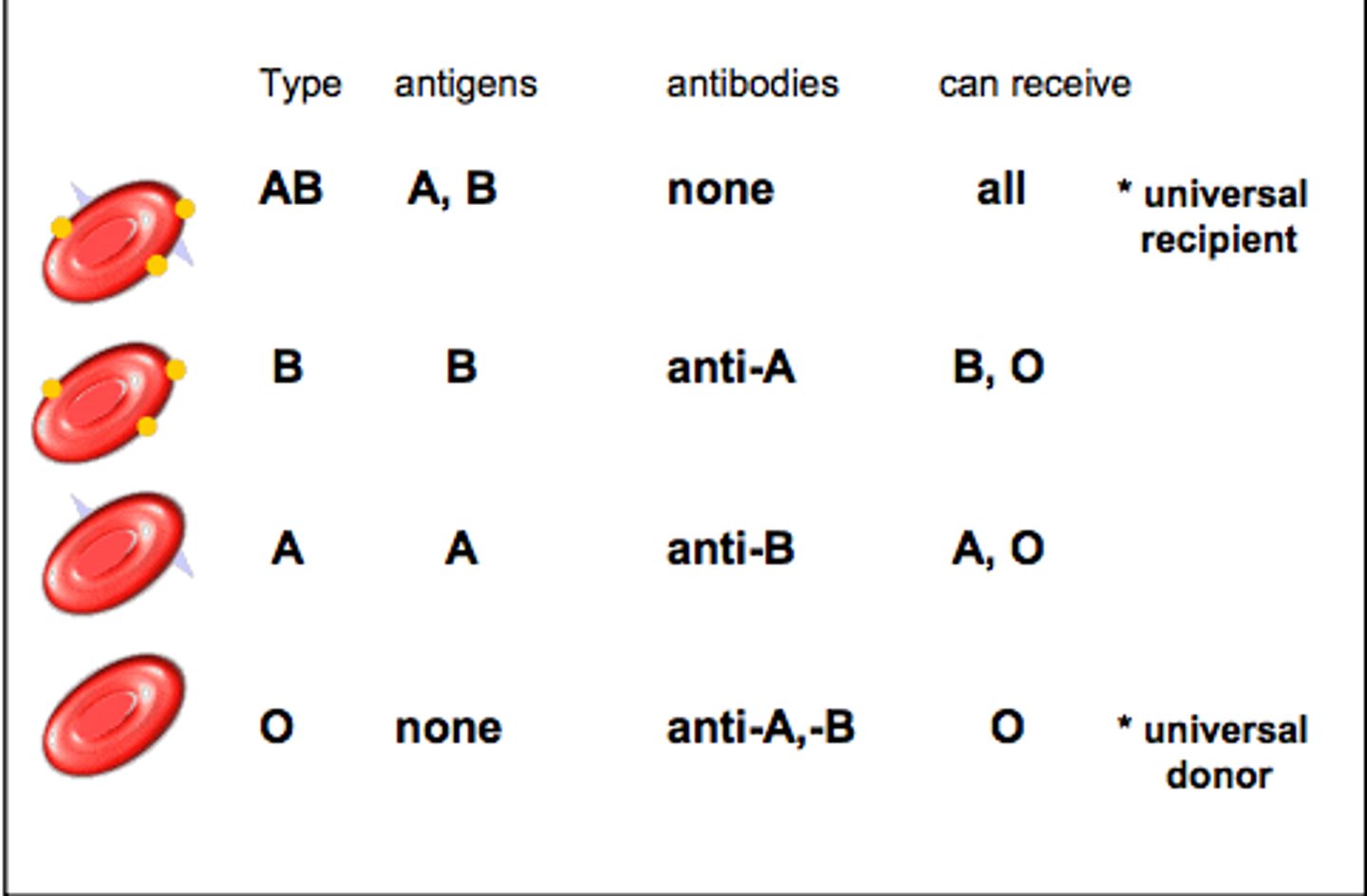
Rhesus factor antigen (Rh)
- Rh- people will only make Rh-antibodies if exposed to Rh+ blood
Rh incompatibility during pregnancy
- Father = Rh+, Mother = Rh-
- 1st baby = Rh+. During birth, mother/baby's blood mix, mother produces anti-Rh antibodies
- 2nd baby: Rh+. Anti-Rh antibodies cross the placenta causing hemolytic disease in fetus
- Prevent by injecting mother w/ anti-Rh antibodies before birth of 1st child, attack contaminating blood before mother develops her own response
What makes up the upper respiratory tract
- Nasal cavity, pharynx, larynx
What makes up the lower respiratory system
- Trachea, primary bronchi, many smaller bronchi, bronchioles, alveoli
Main functions of respiratory system (5)
- Gas exchange
- Homeostatic regulation of body pH
- Conditioning inspired air
- Protection
- Vocalization
What is respiration
- "breathing"
- Movement of air between external environment and internal environment
Muscles of inspiration at rest & forceful
- Rest: Scalenes, external intercostals, diaphragm
- Forceful: Recruit sternocleidomastoids
Muscles of expiration at rest & forceful
-Rest: Muscles of inspiration relax
- Forecful: Internal intercostals and abdominal muscles are recruited
Visceral vs parietal pleural membrane + what's between them
- Visceral: Directly contacts the lungs
- Parietal: Directly contacts the thoracic cavity
- Intrapleural fluid is between the 2
Purpose of intrapleural fluid
- lubricates membranes and allows them to slide against each other as the lungs move w/ breathing
- "Sticks" the lungs tightly to the thoracic wall (keeps lungs inflated)
What do the airways do (3)
- Filter out foreign substances (ciliated epithelium sweeps mucous layer)
- Warms air to body temp
- Adds water vapour
What is flow in the respiratory system proportional to
- Change in pressure / Resistance
How does resistance of airways change?
- Build up of mucous
How bronchodilation is modulated (2)
- Paracrine response to CO2
- SNS response: NE/E bind to Beta-2 adrenergic receptors which relax bronchiole smooth muscle
- Gs-protein, adenyl cyclase, cyclic AMP, protein kinase A, MLCK = deactivated, smooth muscle relaxes, bronchodilator
How bronchoconstriction is modulated (2)
- Paracrine response to histamine released by local mast cells in immune response
- PNS response: ACh minds to M3 muscarinic receptors, activated Gq protein, phospholipase C, IP3, IP3 receptors on SR, release Ca2+, smooth muscle contraction, bronchoconstriction
Type I vs. Type II alveolar cells
- Type I: 95% of alveolar surface area, where gas exchange occurs
- Type II: 5%, make/secrete surfactant
What is surfactant
- Fluid lining alveoli, make them easier to expand, and prevents them from collapsing
- Decrease surface tension therefore decreasing pressure
Law of Laplace + surfactant in small alveoli
- P = 2T/r
- w/o surfactant inward pressure of alveoli would be high, too difficult to inflate
- Exaggerated in smaller alveoli, therefore more surfactant
- Surfactant equals pressure btwn big/small alveoli
Functional residual capacity
- Vol of air left in lungs at the end of normal expiration
- Elastic recoil of lungs inward = elastic recoil of chest wall outwards (results in neg. intrapleural pressure. -4)
Pneumothorax
- Air enters pleural sac, intrapleural pressure is no longer negative
- Bond holding lung to chest wall is broken and the lung collapse
Changes in pressure in quiet breathing
- Chest expansion causes a decrease in intrapleural pressure, and an increase in transpulmonary pressure
- Increased pressure pulls lungs to chest wall
- Lungs/alveoli expand, Palv decreases
- Air flows into alveoli until Palv = Patm