Advanced Nursing Exam 4
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
100 Terms
ABCDEFGH Acronym:
A. Airway & Alertness
B. Breathing
C. Circulation
D. Disability
E. Exposure & Environmental Control
F. Facilitate Adjuncts & Family
G. Get Resuscitation Adjuncts
H. History & Head-to-Toe Assessments
Steps of the Emergency Nursing Assessment: Alertness & Airway
- determine LOC
- AVPU:
alert - opens eyes when you enter room
response to voice - opens eyes when you say name
response to pain - opens eyes only to painful stimuli
unresponsive
Steps of the Emergency Nursing Assessment: Breathing
- assess for signs of dyspnea
- intervene with lowest intervention first
- for life-threatening conditions, use a bag valve mask with 100% oxygen
Steps of the Emergency Nursing Assessment: Circulation
- Check for central pulse (carotid or femoral), assess skin, assess for signs of shock
- Insert two IV lines into upper extremity veins and start aggressive fluid resuscitation with NS or LR
Steps of the Emergency Nursing Assessment: Disability
- monitor patient LOC using GCS (< 8 we intubate!)
- monitor for PERRLA
Steps of the Emergency Nursing Assessment: Exposure & Environmental
- Has patient been exposed to a trauma or agent?
- Remove clothing (do not cut through clothes that have evidence AKA cut around bullet holes), prevent heat loss
Steps of the Emergency Nursing Assessment: Family Presence
- Research supports allowing family during resuscitation and invasive procedures as it gives family closure and reminds care team of the personhood of the patient
- Assign a care team member to be with the family to explain procedure
Steps of the Emergency Nursing Assessment: Get Resuscitation Adjuncts
Equipment used to assist in resuscitation, like mechanical chest compressors
Steps of the Emergency Nursing Assessment: History & Head-to-Toe Assessment
Secondary Survey
Components of Primary Survey:
- Focuses on ABCDEFG
- Obtain bilateral BP & HR, RR, oxygen saturation, temperature
- Catastrophic hemorrhage is top priority!
- The nurse should apply direct pressure, apply a sterile dressing, then address ABCs
Components of Secondary Survey:
- History & Head to Toe ("H")
- Obtain history & mechanism of injury or illness
- Be sure to inspect posterior surfaces by logrolling patient (support the head!)
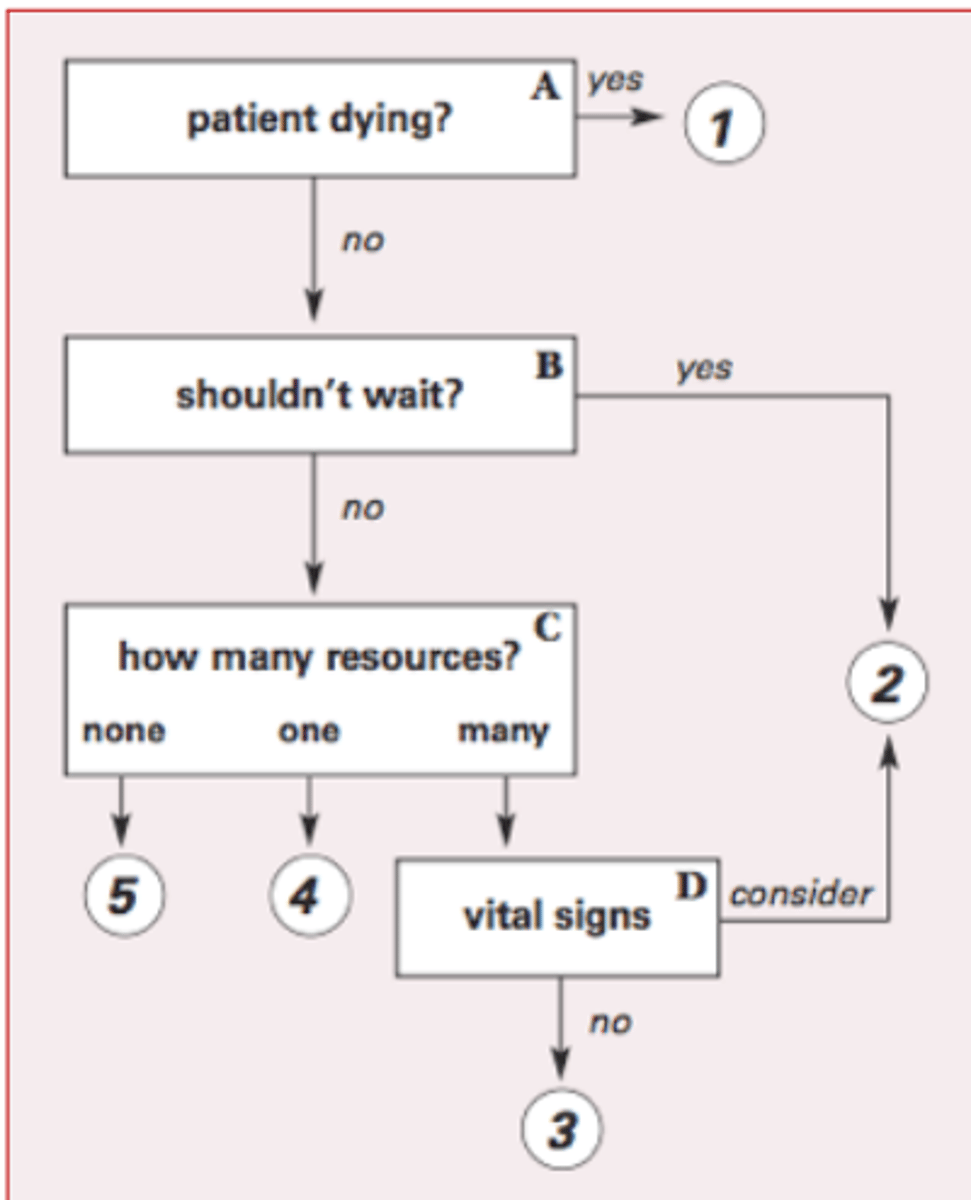
Triage System:
- Categorizes patients so the most critical are treated first
- Emergency Severity Index: see picture
Heat Exhaustion:
- S/S: fatigue, vomiting, thirst, anxiety, tachycardia, change in LOC, temp < 105.8*F
- Interventions: remove clothing, start IV NS, use a moist sheet
Heat Stroke:
- Medical emergency!
- S/S: hypotension, tachypnea, hyponatremia, no sweating temp > 105.8*F, hot skin, hallucinations, cerebral edema
- Interventions: remove clothing, cover with wet sheets, use fans, cool bath, apply ice packs, peritoneal lavaging, give 100% oxygen, continuous EKG, CONTROL SHIVERING, do not use salt tabs or antipyretics
- Monitor for signs of rhabdomyolysis, myoglobinuria, DIC
Hypothermia: Mild
- 93.2-96.8*F
- S/S: shivering, lethargy, confusion, behavioral changes
- Passive warming: remove damp clothing, use radiant lights, place warm blankets on patient
- Active warming: air-filled warming blankets, warm water immersion
Hypothermia: Moderate
- 89.6-93.2*F
- S/S: rigidity, bradycardia, bradypnea, metabolic and respiratory acidosis, no shivering, dysrhythmias
- Intervention: heated oxygen, warmed IV fluids, peritoneal lavage, extracorporeal circulation (cardiopulmonary bypass, rapid fluid infuser)
Hypothermia: Severe
- < 89.6*F
- S/S: undetectable VS, absent reflexes, bradycardia, V fib, asystole
- Warm patient until 86*F before pronouncing dead
General Tips for Rewarming Patient with Hypothermia:
- Rewarm core before extremities
- When warming, monitor for after-drop, hypotension, and dysrhythmias
- DC warming once core temperature reaches 89.6-93.2*F
Agents, Purpose of Agent Use & Prevention of Biological Warfare:
- Involves overt actions for the expressed purpose of causing harm
- Biologic agents: hemorrhagic fever - no treatment, smallpox - highly contagious w/ prolonged incubation period
Reasons for a "Low Pressure Alarm" to go off on an Arterial Line:
- High and low-pressure alarms can be customized by the nurse based on patient needs
- Alarms may go off if there is a leak in the system, ventilator issues, tubing disconnect, or an excess removal of gas from the system
- System may need to be leveled
Nursing Priority Action when alarm goes off on an arterial line:
Check on the patient first!
What is the worst-case scenario when a "low pressure" arterial line alarm goes off?
PEA, vfib, or vtach
What to Monitor for on Arterial Lines:
- Allen Test: occlude either radial or ulnar artery then assess perfusion of the hand; done before art line placement to ensure that hand will be perfused afterwards
- Continuous irrigation system that delivers 3mL saline per hour to maintain patency
- Nurse should monitor neurovascular status distal to the site hourly
Swan-Ganz Pulmonary Artery Catheter:
- Can measure CVP and CO, draw blood, give fluids & drugs
- Measures oxygen saturation, EF, acts as IV access
Complications of Placing a Pulmonary Artery Catheter & Nurse's Role: Infection & Sepsis
- Maintain aseptic technique!
- Nurse's Role: change flush bag, tubing, transducer, and stopcock every 4 days
Complications of Placing a Pulmonary Artery Catheter & Nurse's Role: Air Embolus
Nurse's Role: Monitor balloon integrity, ensure connections are maintained
Complications of Placing a Pulmonary Artery Catheter & Nurse's Role: Pulmonary Infarcts or Rupture
Nurse's Role: do not inflate balloon with > 1.5mL, monitor EKG waveforms continuously, maintain continuous flush
Complications of Placing a Pulmonary Artery Catheter & Nurse's Role: Ventricular Dysrhythmias
Nurse's Role: monitor during insertion & removal, monitor for migration
What is an Intraaortic Balloon Pump (IABP)?
- Provides temporary circulatory assistance by reducing afterload
- Goal: increase perfusion, decrease workload
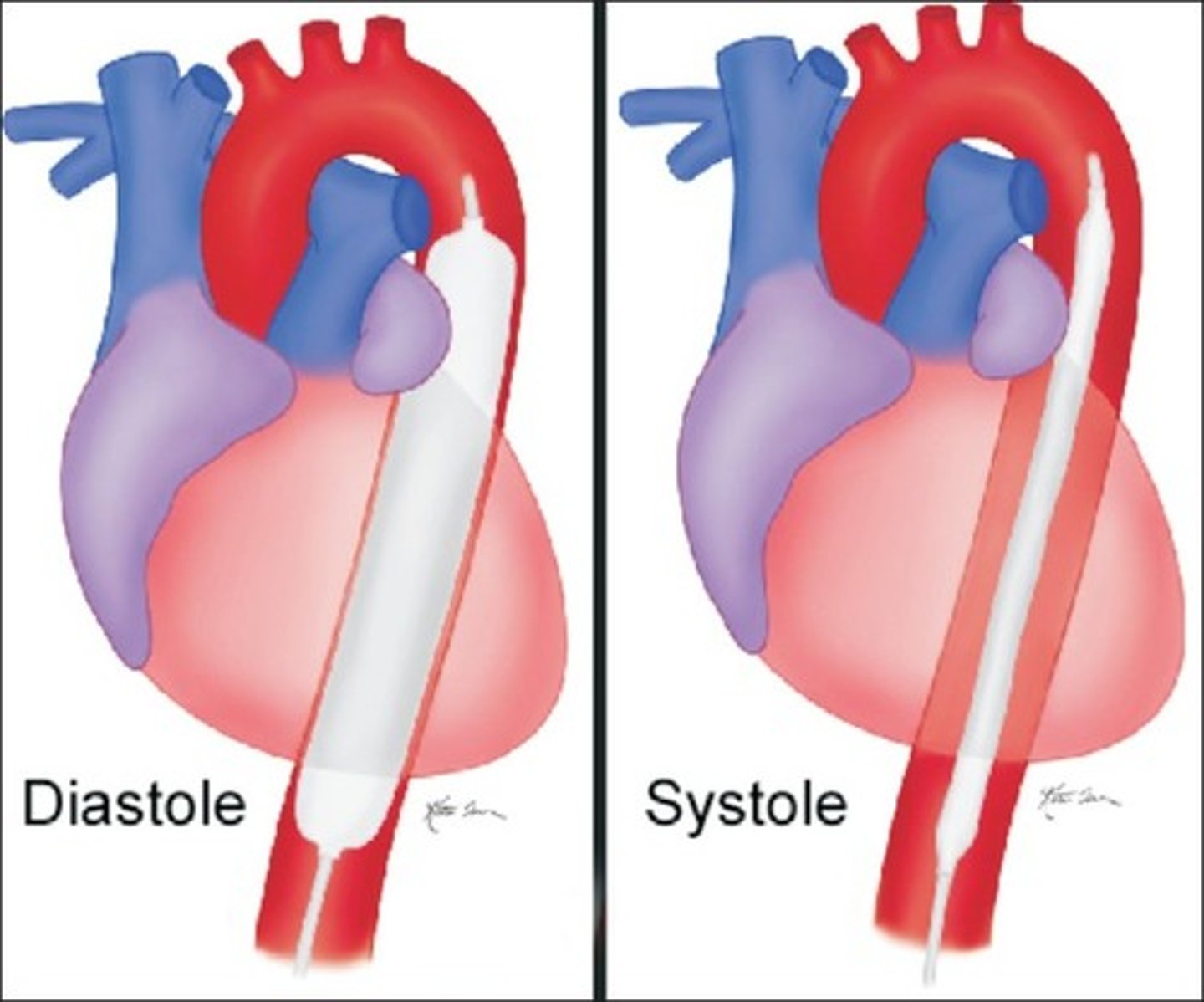
Function of IABP:
- Requires ventricular function
- Uses counterpulsation because the timing of balloon inflation is opposite to ventricular contraction (pumps during diastole)
- Timed with an EKG to ensure proper function
IABP Placement Procedure:
- Balloon inserted into femoral artery and sits between subclavian and renal arteries
- Placement confirmed with X-ray
- Patients must be on bedrest and lay flat with an IABP
Complications of IABP:
Vascular injury (aortic dissection)
Thrombus
Thrombocytopenia
Ischemia from migration
Infection
Mechanical Complications of IABP & Fail-Safe Measures:
- Leak - pump will automatically stop; monitor for increased alarms for gas loss and blood backing up
- Malfunction of balloon - automatically shuts down but must be removed within 15 minutes
Purpose & Function of Ventricular Assist Device:
- Offers more mobility than an IABP
- Indicated if the patient fails to wean from bypass, has heart failure from an MI, or is waiting for transplant
- Augments or replaces ventricle
- Note: patient must be on anticoagulation and will need batteries or plugged into wall at all times
Definition of Cardiac Output (CO):
- Total blood volume the heart pumps to the circulatory system per minute
- CO = SV x HR
Definition of Stroke Volume (SV):
- Volume of blood ejected from the ventricle per beat
- Effected by preload, afterload and contractility
Definition of Ejection Fraction:
Percentage of blood forced out of the left ventricle with each beat
Definition of Central Venous Pressure (CVP):
Measurement of preload on the right side of the heart
Definition of Arterial Blood Pressure (ABP):
- Obtained through peripheral artery cannulation
- Shows blood pressure within the artery
- Nurse should immobilize sutured insertion site of arterial line
Definition of Peripheral Artery Wedge Pressure (PAWP)/PAD:
- Measurement obtained with a swan which shows function of the left side of the heart
- Measures the preload of the left side of the heart
Definition of Afterload:
- Resistance the heart has to pump against to eject blood
- Measured with SVR for left ventricle and PVR for right ventricle
Definition of Preload:
- Measure of filling pressure at the end of diastole
- Preload = volume
Preload is decreased in ...
shock, hemorrhage, dehydration
Measures to increase preload include IV fluids and vasopressors
Preload is increased in...
HF
Measures to decrease preload include diuretics and vasodilators
Definition of Phlebostatic Axis:
- Level of the atria @ 4th ICS @ Level of Heart
- Referencing swan: position the stopcock at axis
- If the transducer is too low, your numbers are falsely high. If the transducer is too high, your numbers will be falsely low.
Definition of Systemic Vascular Resistance (SVR):
Measurement of afterload of the left side of the heart
SVR is increased in...
HTN, aortic stenosis, and pulmonary HTN
To decrease SVR, use ACE inhibitors, ARBs, and vasodilators (sodium nitroprusside)
SVR is decreased in...
shock and sepsis
To increase SVR use vasopressors
Definition of Pulmonary Vascular Resistance (PVR)/PAP:
Measurement of afterload on the right side of the heart
Definition of Mean Arterial Pressure:
- Average arterial pressure through one cardiac cycle of systole and diastole
- Formula: MAP = (SBP + 2DBP)/3
Definition of Pulse Pressure:
- Difference between systolic and diastolic blood pressures
- Can predict risk for cardiovascular disease
Definition of Diastole:
Filling of the heart where coronary arteries are supplied with blood
Definition of Systole:
Contraction of the heart
Definition of Cardiac Index:
- Cardiac output calculation with patient's total body surface area in consideration
- More exact than CO
What is SvO2?
- Reflects balance between oxygenation of arterial blood, tissue perfusion, and oxygen consumption
- Normal = 60-80%
If SvO2 is low...
Nurse should use pulse oximetry and obtain ABG. If normal, assess for other causes of increased oxygen consumption like fever and pain.
If SvO2 is high...
- May indicate improvement or sepsis
- Nurse should assess for signs of sepsis
Define Shock:
- Syndrome characterized by decreased tissue perfusion and impaired cellular metabolism
- Imbalance in supply/demand for O2 and nutrients
Cardiogenic Shock (cause, patho, s/s):
Cause: damage to the heart
Pathophysiology: ineffective blood perfusion leads to decreased oxygenation and impaired cellular metabolism
S/S: tachycardia, hypotension, tachypnea, clammy skin, narrowed pulse pressure, decreased CO
Hemodynamic Changes in Cardiogenic Shock:
decreased CO, increased HR, increased CVP/PAP, increased SVR, decreased O2
Treatment of Cardiogenic Shock:
cardiac catheterization, supply oxygen, nitrates for dilation, diuretics to reduce preload, vasodilators to reduce afterload, circulatory assist devices
Hypovolemic Shock (causes - absolute & relative, s/s, treatment):
Cause - absolute : loss of intravascular fluid volume (hemorrhage, GI loss, diuresis)
Cause - relative: edema/third spacing
S/S: anxiety, tachypnea
Hemodynamic Changes: increased then decreased CO, increased HR, decreased CVP/PAD, increased SVR, decreased O2
Treatment: 3:1 fluid resuscitation (3 isotonic fluid: 1 blood loss)
A patient may compensate for a loss of up to ____% of the total blood volume (approximately 750 mL). If they continue to lose volume, the SNS is activated.
15%
Distributive Shock: Neurogenic (cause, s/s, hemodynamic changes, treatment)
Neurogenic: No Compensation
Cause: SCI T6+; no SNS response, PNS runs wild
S/S: hypotension, bradycardia, poikilothermia
Hemodynamic Changes: everything DECREASED
Treatment: spinal stabilization, vasopressors for BP, atropine for HR, monitor for hypothermia, fluids for BP
Distributive Shock: Anaphylactic (cause, s/s, hemodynamic changes, treatment)
Cause: allergic reaction
S/S: anxiety, impending doom, chest pain, incontinence, edema, stridor, urticaria, respiratory distress
Hemodynamic Changes: decreased CO, increased HR, decreased CVP/PAD, increased then decreased SVR, decreased O2
Treatment: IM epinephrine, maintain airway, fluid replacement
Distributive Shock: Septic (cause, s/s, hemodynamic changes, treatment)
Cause: bacterial infection
S/S: hypotension, microthrombi, tachypnea (respiratory alkalosis), decreased UO, altered LOC, GI dysfunction, MODS
Hemodynamic Changes: increased CO, increased HR, decreased CVP/PAD, decreased SVR, increased SVO2
Treatment: 30-50mL/kg isotonic fluid replacement, vasopressors/norepinephrine if fluid replacement does not work, blood culture, antibiotics within one hour, keep BS slightly high, stress ulcer prophylaxis with protonix, DVT prophylaxis
Phases of Shock: Initial
- No S/S
- Metabolism changes anaerobic (without oxygen)
Phases of Shock: Compensatory
- Neural, hormonal, and biochemical systems kick in to compensate for anaerobic metabolism
- Baroreceptors activate SNS to increase BP
- Vasoconstriction occurs to supply oxygen to heart and brain
- Respiratory: V/Q mismatch, decrease arterial O2, tachypnea
- Skin is cool and clammy, except for septic shock ("warm shock")
- Medical interventions must begin here!
Phases of Shock: Progressive
- Begins as compensatory mechanisms fail
- Monitor for change in LOC!
- Increased systemic edema (anascaria)
- Weak peripheral pulses due to hypoperfusion
- Cardiac: dysrhythmias, MI, heart failure
- Pulmonary: edema, bronchoconstriction, crackles
GI bleeding, migration of bacteria from GI tract to lungs
- Liver: jaundice, elevated enzymes, risk for DIC
Phases of Shock: Refractive
- Exacerbation of anaerobic metabolism
- Accumulation of lactic acid
- Decreased CO, vasoconstriction
- Hypotension, tachycardia, MODS
- Patient is unlikely to recover
How are the kidneys affected in shock?
- During compensatory phase, blood to the kidneys is decreased which activates RAAS system
- During progressive phase, renal tubular ischemia occurs due to hypoperfusion
- S/S: decreased UO, increased BUN, increased creatinine
What is a base deficit?
Base refers to the amount of bicarb needed to correct the blood pH
- Normal is -2 – 2
Base deficit = excess acid
- Base will be very low in shock (ex = -14)
Give sodium bicarb
Nutritional Support in Shock:
- Start enteral nutrition within 24 hours
- Protein-calorie malnutrition is one of the main manifestations of hypermetabolism in shock
- Full calorie replacement is not recommended for previously well-nourished adults early on in critical illness.
Rationale for having patients on enteral feedings vs. TPN:
- Only use parenteral nutrition if enteral feedings are contraindicated
- If GI tract is active, use enteral feedings
DKA (cause, patho, s/s):
- Cause: Sepsis, Sickness (ex: flu), Stress/Surgery, Skipping insulin
- Pathophysiology: deficiency in insulin, breakdown fat creating ketones, glucose release -> high BS; leads to hypokalemia, hyponatremia, hypomagnesemia, hypophosphatemia, and hypovolemia
- S/S: dehydration, anorexia, vomiting, metabolic acidosis (Kussmaul respirations), BS > 250, ketones in urine, abdominal pain
Interventions for DKA:
- Bolus of NS
- Lower glucose slowly - if > 250, give regular insulin bolus then a drip
- If > 200, use subcut insulin
- Replace potassium & place on monitor (insulin and potassium drop together)
- Hourly BS checks via arterial line
DIC (causes, patho, s/s, lab changes):
- Causes: sepsis, trauma, OB complications
- Pathophysiology: overdrive clot formation leads to organ damage (often kidneys, liver, lungs, and brain); formation of clots depletes supply of platelets leading to bleeding
- S/S of bleeding: pale, prolonged bleeding, hematomas, tachycardia, hypotension, change in LOC, dizziness
- S/S of clots: cyanosis, oliguria, SOB w/ tachypnea (PE)
- Lab Changes: low platelets, low fibrinogen, high PTT, high PT, high D Dimer
Interventions for DIC:
- FIND THE CAUSE
- Ventilator support, hemodynamic support, blood transfusions, thrombus prevention
SIRS (patho, causes, nursing interventions):
- Pathophysiology: generalized inflammation in organs other than the initial injury
- Causes: trauma, abscess, ischemia, microbial invasion, endotoxins
- Nursing Interventions: address inflammation to prevent MODS
MODS (definition, assessment focuses, interventions):
- Definition: failure of two or more organ system, resulting from SIRS
- Assessment Focuses: monitor for respiratory changes, LOC changes, electrolyte imbalances & DIC, AKI, jaundice
- Interventions: POOR PROGNOSIS; prevent infection, maintain tissue oxygenation, support failing organs
Normal Blood Gas Values:
pH: 7.35-7.45
PaO2: 80-100
CO2: 35-45
HCO3: 22-26
Pathophysiology of ARDS:
- Sudden, progressive form of respiratory failure where alveolar-capillary membrane becomes damaged, leading to inflammation, and is more permeable to intravascular fluid
- Neutrophils cause formation of microemboli and pulmonary artery vasoconstriction
- Alveoli fill with fluid, do not make surfactant, and are unable to expand for oxygenation.
What is the most common cause of ARDS?
sepsis but can be caused by SIRS or MODS
Early & Late Clinical Manifestations of ARDS:
Early: dyspnea, cough, restlessness, crackles, mild hypoxemia, respiratory alkalosis; chest x-ray is normal
Late: respiratory distress, retractions, tachycardia, diaphoresis, cyanosis, pallor, course crackles, hypoxemia resistant to increasing supplemental oxygen, increased WOB; chest x-ray shows “whiteout”
What position should a patient with ARDS be placed in?
prone
Complications of Treatment for ARDS:
- Ventilator-associated pneumonia
- Barotrauma - too much pressure in fibrotic lungs leads to collapse
- Volutrauma - alveoli crack due to increased air volume
- High risk for stress ulcers
How to prevent ventilator-associated pneumonia:
Elevate HOB to 30-45*, daily sedation holidays, daily oral care
How to prevent stress ulcers:
Prevent with pantoprazole [Protonix]
What is PEEP?
- Uses puffs of air at the end of inspiration to open collapsed alveoli
- Normal PEEP = 5 but higher levels are often used with ARDS
- Can decrease preload, CO, and BP
Pathophysiology of Respiratory Failure:
- Without oxygen, cells switch to anaerobic metabolism creating lactic acid
- This leads to metabolic acidosis, decreased CO, impaired renal function, and tissue ischemia
Signs of Decompensation:
- Early: Change in LOC - restlessness, confusion, agitation, and combative behavior; tachycardia, tachypnea, mild HTN
- Patients will show pursed-lip breathing and tripod positioning
- Dyspnea (w/ inability to speak), retractions, paradoxical breathing
- Late: cyanosis
Treatment for Respiratory Failure:
- Maintain PaO2 at > 60 and SpO2 90%+ on lowest oxygen possible
- 2-3L/day PO fluid (best way to thin secretions)
- Position good lung DOWN
- Limit suctioning to once per hour
- Ambulate frequently
- Use acetylcysteine + bronchodilator for secretion control
- Use bronchodilators for bronchospasm
Noninvasive Positive Pressure Ventilation:
- Most useful in managing chronic respiratory failure
- BiPAP - different positive pressure levels are set for inspiration and expiration
- CPAP - constant positive pressure is delivered to the airway during inspiration and expiration
Invasive Positive Pressure Ventilation: (confirming placement, self-extubation action, nurse's role in insertion)
- Invasive = intubation
- To confirm placement: auscultate breath sounds, attach an end-tidal CO2 monitor, and get a chest x-ray
- If patient self-extubates: assess the patient and establish an airway
- Nurse's role in ET tube insertion: confirm placement through breath sounds and CO2, gather supplies
Hypoxemic Respiratory Failure:
- Oxygenation failure
- PaO2 < 60 while on > 60% oxygen
- Pulse oximetry shows oxygenation but not ventilation
What is Diffusion Limitation? What causes this?
- Oxygen must diffuse across the membrane
- A limitation is where membranes are thickened and diffusion is limited
- Caused by pulmonary fibrosis
What is V/Q mismatch? What causes this?
- Inequality between ventilation and perfusion
- Ventilation – ability to get gas into the lungs for the oxygen exchange to occur
- Perfusion – blood flow around alveoli to pick up oxygen
- Main cause is pulmonary embolus
What is a shunt?
- Third cause of hypoxemic respiratory failure
- Ventricular septal defect where oxygenated and unoxygenated blood is mixing
- Also caused by ARDS and pneumonia
What is alveolar hypoventilation?
- Causes both hypercapnic and hypoxic respiratory failure
- Typically from CNS dysfunction
Hypercapnic Respiratory Failure:
- Ventilatory failure
- PaCO2 > 48 with acidemia
- Main cause is alveolar hypoventilation from asthma, COPD, CF, OC, and SCI (and other conditions that cause impaired chest wall movement)