dental embry, histo, and anatomy ch 9-10 quiz
1/129
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
130 Terms
oral mucosa properties
continuously lines the oral cavities and serves as a “mirror” for the health of the rest of the body
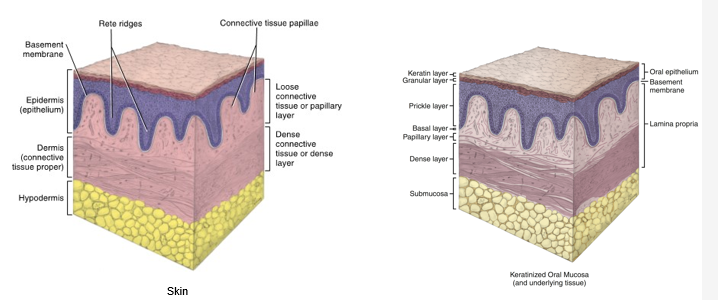
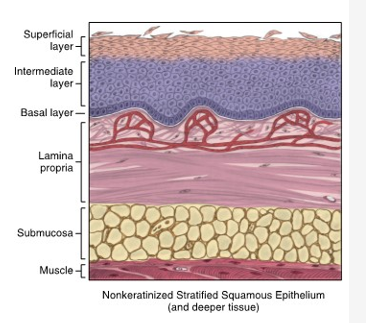
composed of stratified squamous epithelium overlying lamina propria and sometimes a deeper submucosa
basement membrane lies between epithelium and connective tissue
three main types:
lining
masticatory
specialized
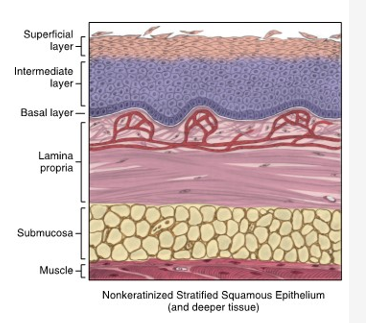
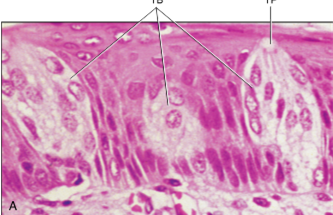
nonkeratinized epithelium
lining mucosa
basal, intermediate, and superficial layers present
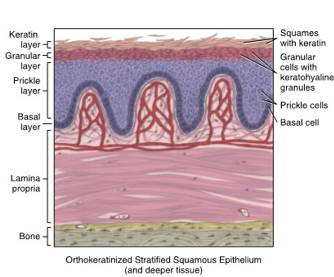
orthokeratinized mucosa
masticatory mucosa
basal, prickle, granular, keratin layers present
more layers superficial to basal layer
CELLS CONTAIN ONLY KERATIN AND NO NUCLEI!!
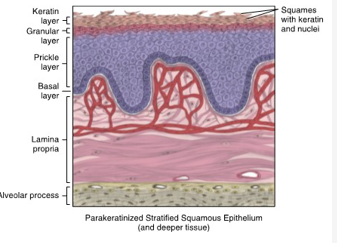
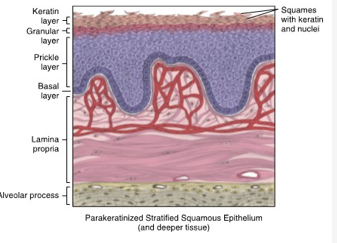
parakeratinized epithelium
masticatory mucosa
basal, prickle, granular, keratin layers
CELLS CONTAIN KERATIN AND NUCLEI
keratinocytes
epithelial cells in oral mucosa that produce keratin in low levels or higher levels when the tissue becomes traumatized
nonkeratinocytes
cells that do not produce keratin
present in much smaller numbers in oral mucosa
keratin
waterproof protein
tough, fibrous, opaque, waterproof protein that is impervious to pathogenic invasion and resistance to friction
produced during maturation of keratinocyte epithelial cells as they migrate from basement membrane upwards
microplicae
cellular ridge-like folds
microridges known to be typical of the surfaces of the body covered with protective mucus, or in the case of the oral cavity, saliva
superficial surface layer of most epithelium in oral mucosa contain these
lining mucosa
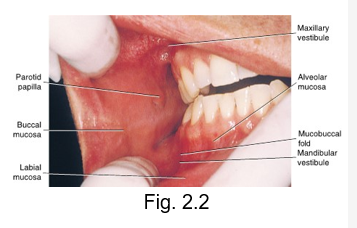
covers 60% of the mouth
made of nonkeratinized stratified squamous epithelium
noted for its softer surface texture, moist surface, ability to stretch, act as cushion
buccal mucosa
labial mucosa
alveolar mucosa
mucosa lining of the ventral surface of tongue
floor of mouth
soft palate
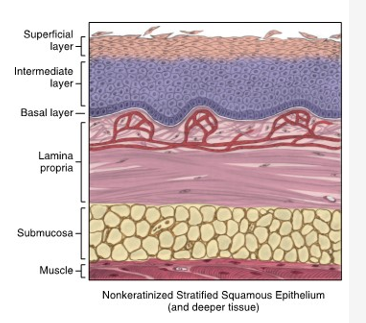
lining mucosa basal layer
also known as stratum basale
deepest of the three epithelial layers
single layer of cuboidal epithelial cells overlying basement membrane
produces basal lamina of basement membrane
germative due to mitosis of epithelial cells
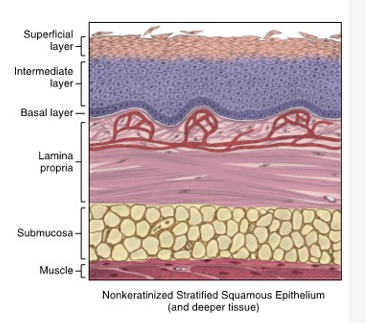
lining mucosa intermediate layer
stratum intermedium
layer of epithelium superficial to the basal layer in nonkeratinized epithelium
composed of larger, stacked, polyhedral-shaped cells
larger, plumper, more fluid within cytoplasm
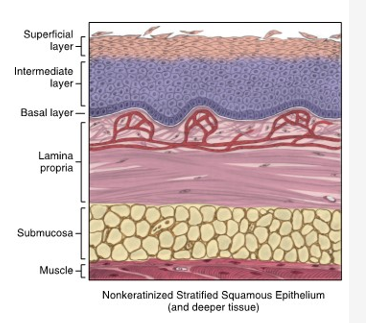
lining mucosa superficial layer
stratum superficiale
most superficial level in nonkeratinized epithelium
layer shows even larger similarly stacked polyhedral epithelial cells, with outer layer flattening into squames
squames shed as they age and die during turnover of tissue
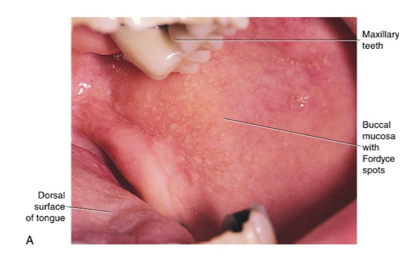
clinical appearance of labial and buccal mucosa
both appear as an opaque, pink color, shiny, moist, compressible tissue that stretches easily
areas of melanin pigmentation may be noted
epithelium is thick, and overlies a lamina propria with an extensive vascular supply which give it such a red color
fordyce spots (granules)
variable number of these are scattered throughout the tissue
are a variant usually present in the oral cavity, which are visible as small, yellowish bumps on the surface of oral mucosa
correspond to deposits of sebum from misplaced sebaceous glands in submucosa
hyperkeratinization
nonkeratinized epithelium may transform into keratinizing type in response to frictional or chemical trauma
in which case, it undergoes hyperkeratinization
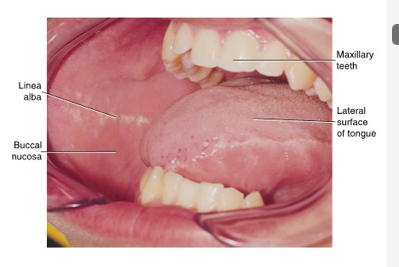
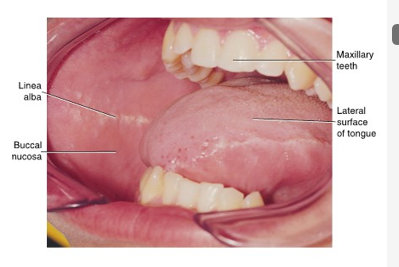
linea alba
a change to hyperkeratinization commonly occurs on the usually nonkeratinized buccal mucosa when _ _ forms
a white ridge of calloused tissue that extends horizontally at the level where the maxillary and mandibular teeth come together to occlude
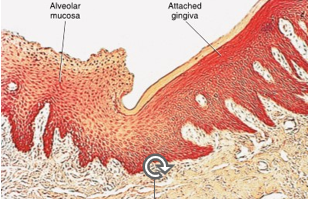
alveolar mucosa clinical appearance
reddish-pink tissue with blue vascular areas
shiny, moist region which is extremely mobile (allows you to stretch lips) and lines the vestibules of the oral cavity
lining mucosa
alveolar mucosa histology
epithelium is extremely thin nonkeratinized epithelium that overlies but does no obscure
an extensive vascular supply in the lamina propria making mucosa redder than the labial or buccal mucosa
connective papillae are sometimes absent and numerous elastic fibers are present in the lamina propria allowing mobility
minor salivary glands in submucosa
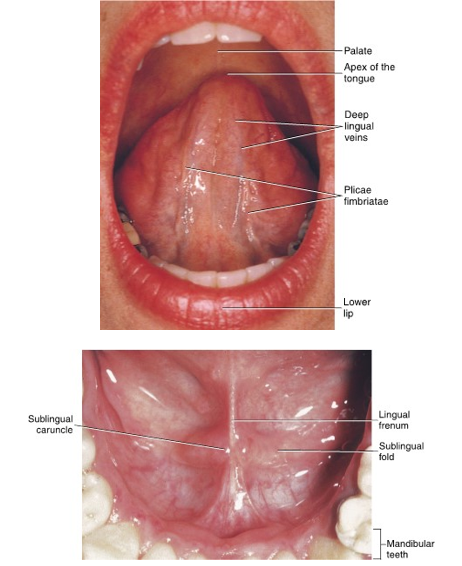
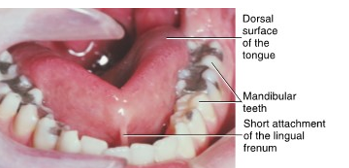
clinical appearance of the ventral tongue and floor of mouth
both appear as a reddish-pink tissue with vascular blue areas of veins
moist, shiny, compressible
floor of the mouth has mobility, ventral surface of tongue firmly attached with some stretching
lining mucosa
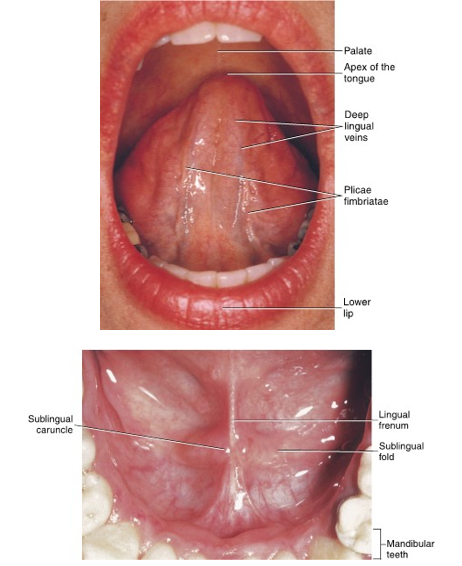
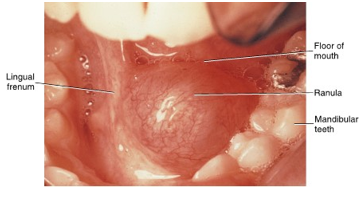
floor of mouth clinical appearance
lingual frenum is a midline fold of tissue between ventral tongue and floor of mouth
ridge of tissue on each side of the floor, sublingual fold, joins in a V-shape
small papilla, sublingual caruncle, at the anterior end of each sublingual fold contains openings of the submandibular and sublingual ducts from both salivary glands
mandibular torus
tori
located on the lingual aspect of the mandibular arch
present bilaterally in the area of premolars
covered in oral tissue and of hereditary etiology
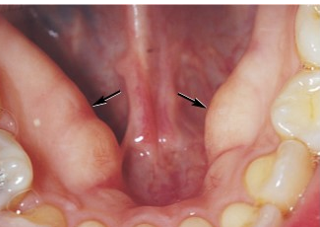
ankyloglossia
short lingual frenum attachment that extends to tongue’s apex
restricts movement of the tongue to varying degrees
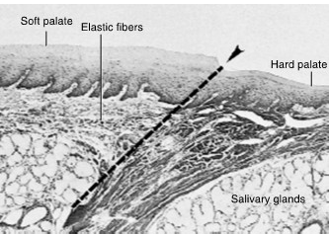
soft palate clinical appearance
posterior part of palate is a deep pink with yellowish hue
compressible and elastic for speech and swallowing
lining mucosa
soft palate histology
thin nonkeratinized epithelium overlying a thick lamina propria
lamina propria has numerous connective tissue papillae and distinct elastic layer for mobility
submucosa is extremely thin and has a firm attachment to underlying muscle for speech and swallowing. contains adipose CT (yellow color) and minor salivary glands
masticatory mucosa
noted for rubbery surface texture and resiliency
includes hard palate, attached gingiva, and dorsal surface of tongue
associated with orthokeratinized statified squamous epithelium parakeratinized stratified squamous epithelium
absent submucosa
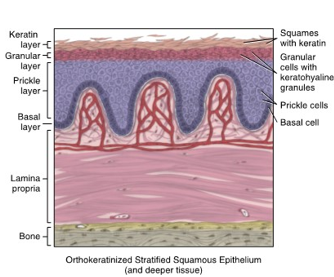
masticatory mucosa: orthokeratinized stratified squamous epithelium
demonstrates a keratinization of the epithelial cells throughout most superficial layers
hard palate
attached gingiva
specialized mucosa of the lingual papillae on the dorsal surface of tongue
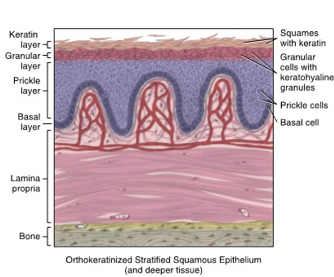
orthokeratinized stratified squamous epithelium basal layer
stratum basale
single basal layer undergoing mitosis
produces basal lamina of the adjacent basement membrane
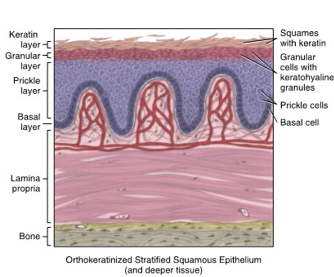
orthokeratinized stratified squamous epithelium prickle layer
stratum spinosum
superficial to basal layer
cells migrate to this superior level in tissue and lose ability to undergo mitosis
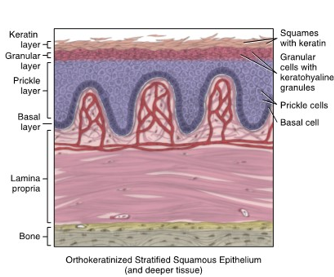
orthokeratinized stratified squamous epithelium granular layer
granular layer known as stratum granulosum
superficial to prickle layer
epithelial cells in this layer are flat and stacked in a layer three to five cells thick
each cell has nucelus with prominent keratohyaline granules
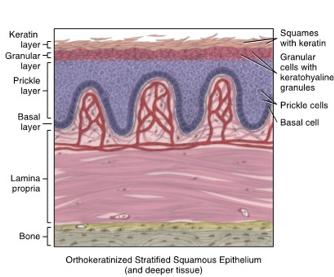
orthokeratinized stratified squamous epithelium keratin layer
most superficial layer
stratum corneum
shows a variable thickness depending on oral cavity region
cells are flat and have no nuclei, increasingly flatten and eventually shed
cytoplasm filled with keratin
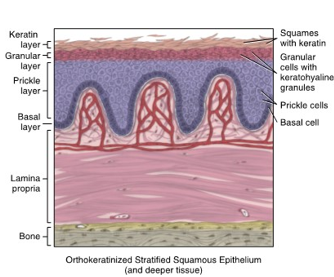
keratohyaline granules
complex
forms chemical precursor for keratin which is a soft, opaque, waterproof protein
appear microscopically as dark spots
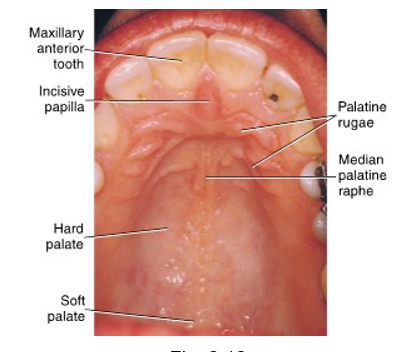
hard palate clinical appearance
anterior part of palate appears as whiter-pink tissue that is immobile and firm
cushioned feeling is noted when hard palate palpated in posterior lateral zones and firmer in the medial zone as a result of the absence of submucosa in the middle
lateral zones consists of submucosa and salivary glands
masticatory mucosa
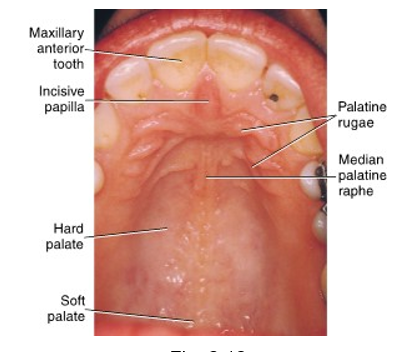
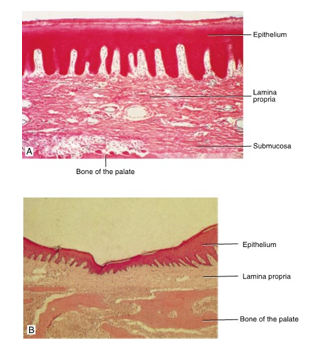
hard palate histologic feature
thick layer of orthokeratinized epithelium overlying thick lamina propria
only lateral zones have a submucosa overlying the bones of the palate, giving the tissue here a cushioned feeling when palpated
submucosa in anterior part of lateral zone contains adipose
submucosa in posterior part of lateral zone contains salivary glands
oral mucosa directly attached to periosteum of the underlying bone of hard palate
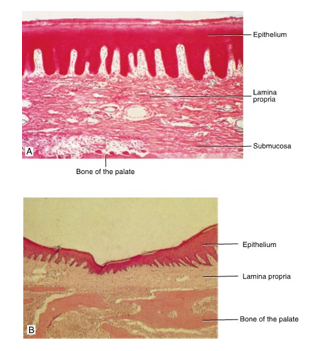
mucoperiosteum
a structure consisting of a mucous membrane combines with the periosteum of the adjacent bone
palatine rugae and median palatine raphe have histologic features similar to those of the __ zone of the hard palate
medial
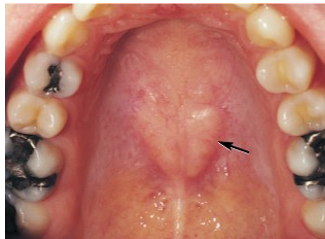
palatal torus
variation noted in the midline of the hard palate
developmental growths of bone with a hereditary etiology
vary in size, slow growing, asymptomatic, may be seen on radiographs
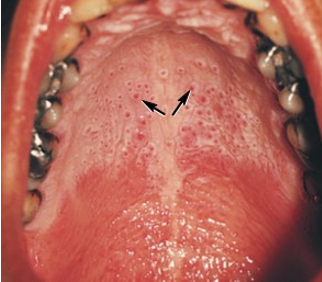
nicotinic stomatisis
lesion associated with salivary glands
hard palate whitened by hyperkeratinization due to heat from tobacco use or hot liquid consumption
masticatory mucosa: parakeratinized stratified squamous epithelium
associated with masticatory mucosa of the attached gingiva in higher levels
it is also associated with specialized mucosa of the lingual papillae on the dorsal surface of tongue
basal → prickle→ granular→ keratin
granular layer may be indistinct or absent all together
cells of the keratin layer contain not only keratin but NUCLEI
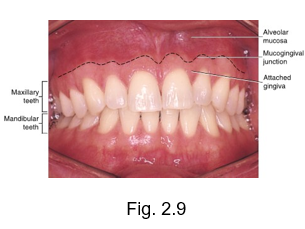
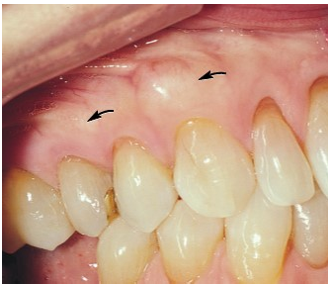
attached gingiva and mucogingival junction
clinical appearance of attached gingiva
opaque pink, and areas of melanin pigmentation may be present
when dried, tissue is dull, firm, and immobile
masticatory mucosa
stippling observed
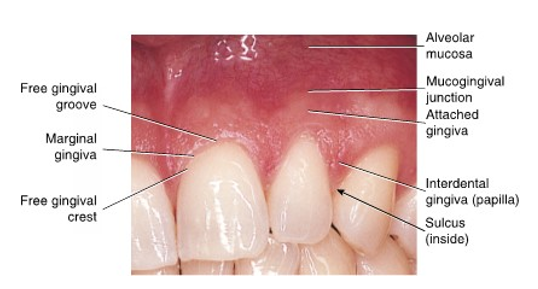
stippling
observed clinically as small pinpoint depressions, which give the surface of the attached gingiva an orange-peel appearance
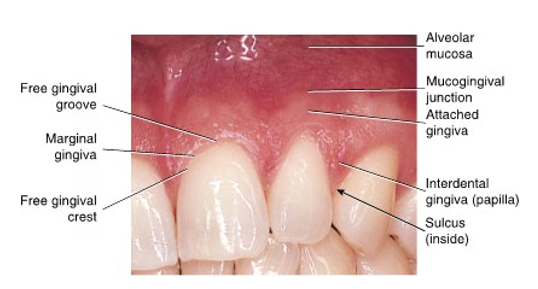
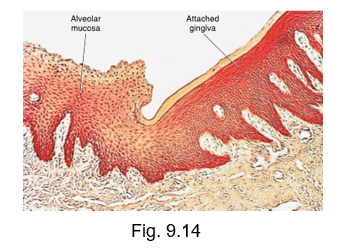
attached gingiva histologic feature
thick layer of mostly parakeratinized epithelium that obscures the extensive vascular supply in the lamina propria making the tissue appear opaque and pinkish
lamina propria has tall and narrow connective tissue papillae (noted as stippling)
no submucosa present
directly attached to underlying alveolar process of jaws
mucogingival junction clinical appearance
sharply defined, scalloped unction between the pinker attached gingiva and the redder alveolar mucosa
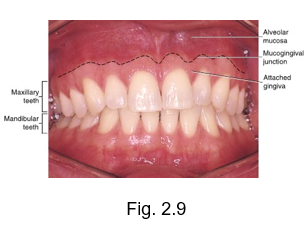
mucogingival junction histologic feature
can be seen as a diving zone between keratinized attached gingival tissue and nonkeratinized alveolar mucosa and thus between a masticatory mucosa and a lining mucosa
junction between a tissue with thick epithelial layer in the pinkish attached gingiva and a tissue with a thin epithelial layer in the redder alveolar mucosa, even though both tissue types have a similar extensive vascular supply
exostoses
variation noted usually on the facial surface of the alveolar process of the maxilla
localized developmental growth of bone with hereditary etiology
periodontal disease
marginal and attached gingiva can become enlarged, especially the interdental papilla
results from edema occurring in lamina propria of the tissue because of inflammatory response
fluid from the lamina propria capillaries flow out to flush area of injurious agents
gingival recession
with its lower or more apical gingival margin can also result from periodontal disease, tooth position, abrasion by incorrect toothbrushing, and strong frenal attachments, abfraction from occlusal tresses such as parafunctional habits, aging

gingival graft
reduces the amount of gingival recession
subepithelial connective tissue graft is from lamina propria that is taken from attached gingiva then grafted directly to root
surrounding tissue migrates to cover graft and heal area
gingival hyperplasia
effects both epithelium and lamina propria
overgrowth of interproximal gingiva caused by the intake of certain drugs for seizure control, certain antibiotics, and specific hear medications

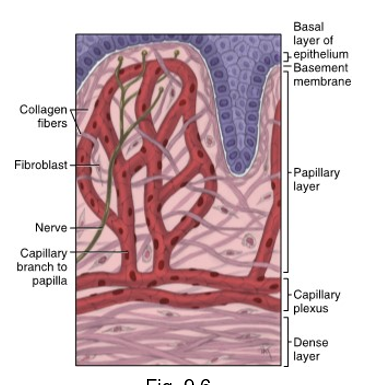
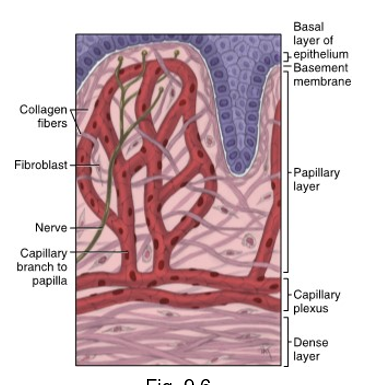
lamina propria of oral mucosa
all forms of epithelium of the oral mucosa have this layer deep to basement membrane
main fiber group is type 1 collagen
have papillary and dense layers
most common cell is the fibroblast
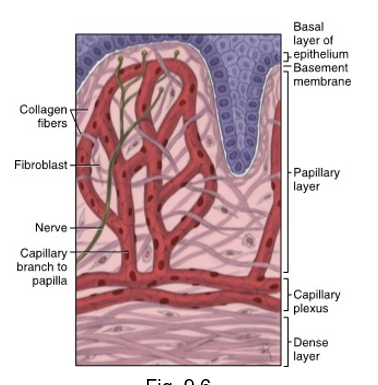
papillary layer of lamina propria
more superficial layer of lamina propria
loose connective tissue along with blood vessels and nerve tissue
equal amount of fibers, cells, and intercellular substance
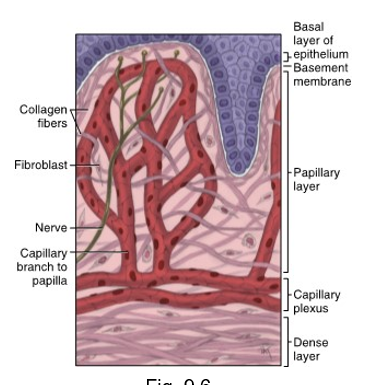
dense layer of lamina propria
deeper layer of lamina propria
dense connective tissue with a large number of fibers

between the papillary layer and deeper layers of lamina propria is a __ __
capillary plexus
fibroblasts
synthesize certain types of protein fibers and intercellular substance
submucosa
may or may not be present deep to the dense layer of lamina propria depending on the region of the oral cavity
if present, it usually contains loose connective tissue and may contain adipose connective tissue or salivary gland
may overlie bone or muscle within oral cavity
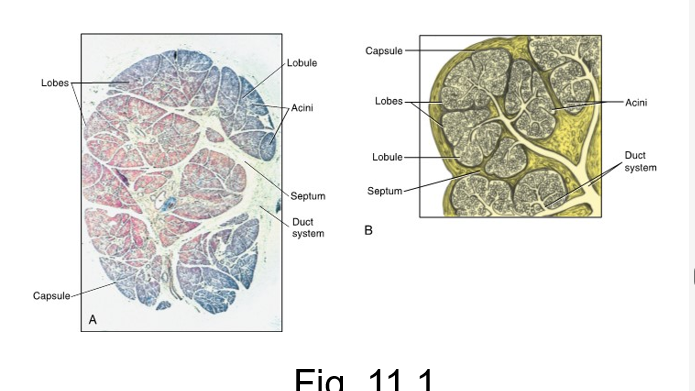
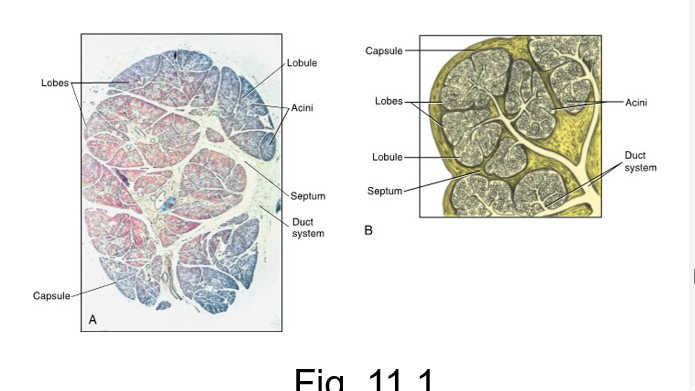
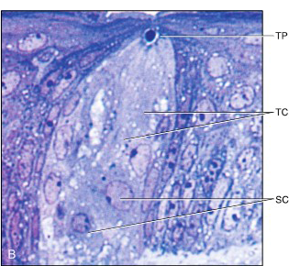
salivary gland histology
both major and minor salivary glands are compose of both epithelium and connective tissue
connective tissue of gland is divided into the capsule which surrounds the outer portion of the entire gland
each septum helps divide the inner portion of the gland into larger lobes and smaller lobules
secretory cells
epithelial cells that produce the saliva
mucous cells
serous cells
found in a group or acinus
each consists of a single layer of cuboidal epithelial cells surrounding a lumen

lumen
central opening
where the saliva is deposited after being produced by secretory cells

ranula
retention of saliva in the gland can result in this if it involved the sublingual salivary gland
lesion is managed by removal of the stone or surgical removal of gland
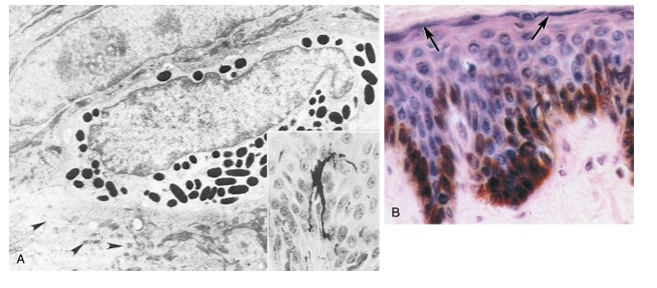
melanocytes
forms melanin
derived from neural crest cells
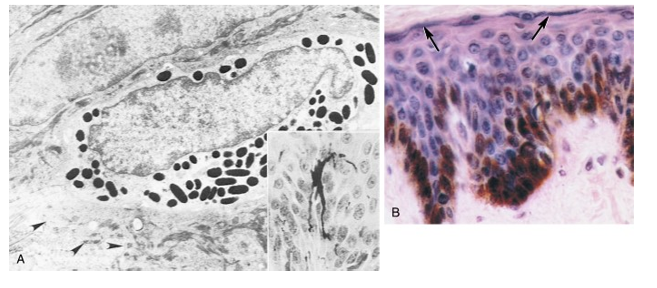
melanosomes
melanocytes have a small cytoplasmic granules or inclusions called __ which store melanin pigment
inject these granules into neighboring newly formed epithelial cells of basal layer
hard palate turnover time
24 days
floor of mouth turnover time
20 days
buccal and labial mucosa turnover time
14 days
attached gingiva turnover time
10 days
taste bud turnover time
10 days
junctional epithelium (attached to tooth) turnover time
4 to 6 days
granulation tissue
immature connective tissue
fewer fibers; increased blood vessels
may become abundant and interfere with repair process
delay in healing
assumptions should never be made of the source of lesion
followed with microscopic study is only effective way to diagnose lesion
a delay of approximately 2 weeks to allow a lesion to undergo healing
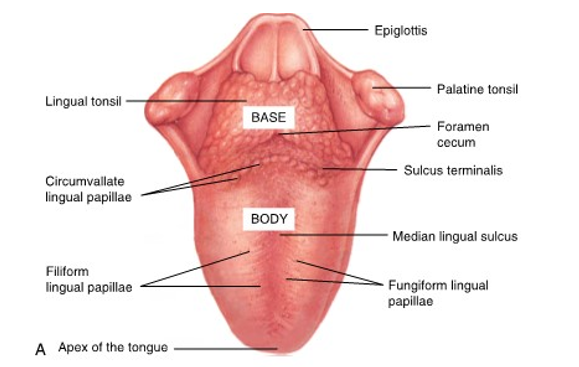
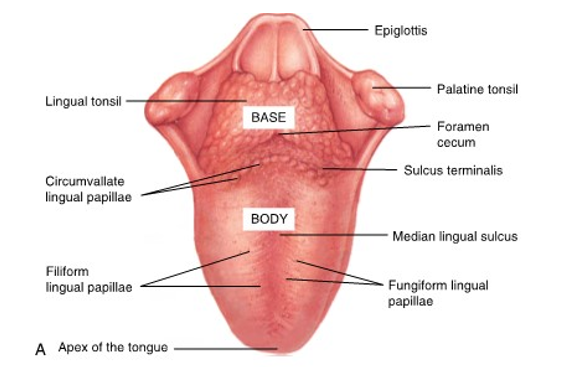
lingual tonsil
posteriorly on the dorsal surface of the base of the tongue
irregular mass of tissue
sulcus terminalis
v shaped line
divides the tongue into an anterior two thirds and posterior one third
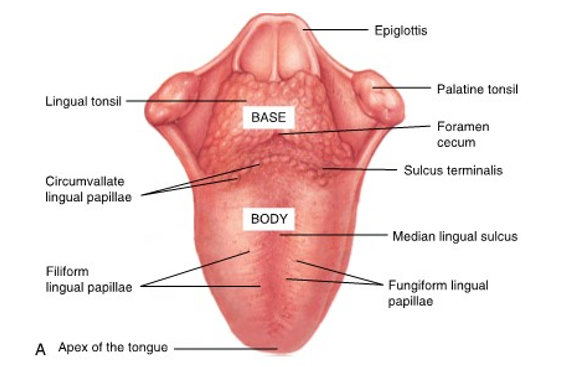
foramen cecum
where the sulcus terminalis points backward toward the pharynx
a small pit like depression
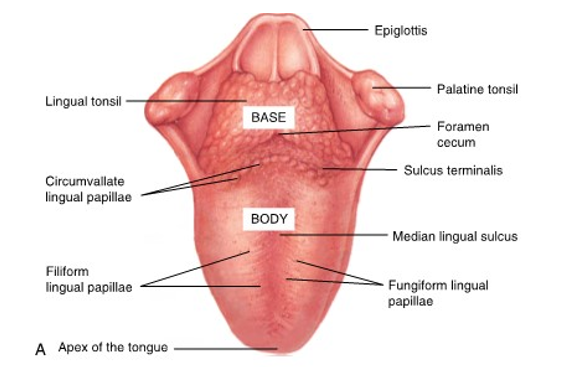
median lingual sulcus
dorsal surface
midline depression of tongue
corresponding to the position of a midline fibrous structure deeper in the tongue and fusion tissue area
pharyngeal part of tongue
base of tongue
attaches to floor of mouth and does not lie within oral cavity proper
part of pharynx
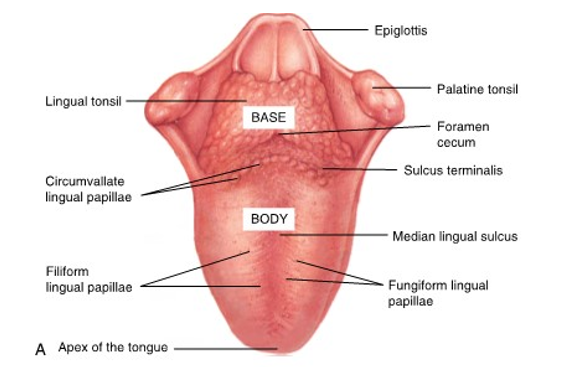
body of tongue
anterior two-thirds of the tongue
lies within oral cavity proper
contains tastebuds
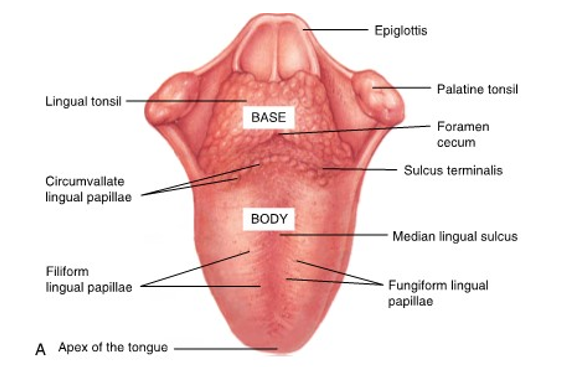
ventral surface of tongue
underside of tongue
noted for its visible large blood vessels which pass close to surface
plica fimbriata lingual to deep lingual vein - fringelike projections
tongue histologic features
dorsal has both masticatory mucosa of orthokeratinized stratified squamous epithelium and specialized mucosa
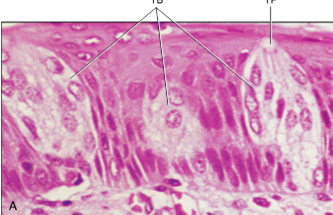
specialized mucosa
found on the dorsal surface and is associated with lingual papillae
small discrete structures or appendages of keratinized epithelium with both orthokeratinized and parakeratinized epithelium present overlying a lamina propria
taste bud
barrel shaped organ of taste derived from epithelium
30 to 80 spindle shaped cells that extend from the basement membrane of the oral mucosa to the epithelial surface of lingual papilla
supporting cells
taste cells that have taste pores
supporting cells
maintain taste bud and are usually located on outer part
taste cells
usually located on the central part and have superficial taste receptors that are responsible for making contact with dissolved molecules of food and producing a taste sensation
taste pore
dissolved molecules of food contact the taste receptor
opening in the most superficial part
associated with sensory neuron processes among the cells in the inferior part
messages then sent to CNS and identified
filiform lingual papillae
most common
fine-pointed cones giving tongue velvety texture
mechanical
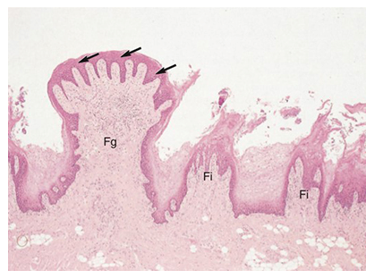
fungiform
lesser number
mushroom-shaped red dots
thin layer of keratinized epithelium overlying core of lamina propria with taste buds on most superficial part
taste
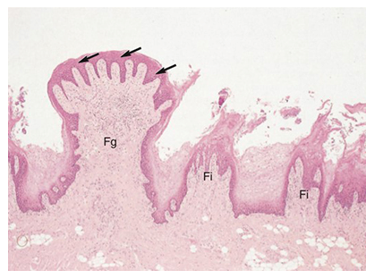
foliate
4 to 11 vertical ridges on lateral surface of posterior tongue
leaf-shaped structure of keratinized epithelium overlying core of lamina propria with taste buds in superficial lateral part
taste

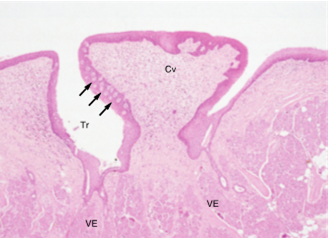
circumvallate
7-15
large raised mushroom shaped structures anterior to sulcus terminalis
similar histology to fungiform but also sunken deep to tongue surface
surrounded by trough with von Ebner minor salivary glands in submucosa
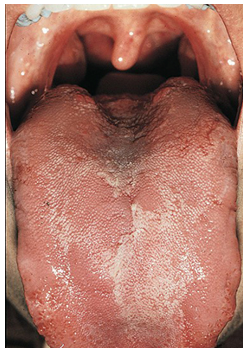
geographic tongue
appears as red and then paler pink to white patches on body of tongue
change shape with time resembling geographic map
black hairy tongue
usual level of shedding of epithelium of filliform lingual papillae does not occur
thick layer of dead cells and keratin builds up on tongue surface which becomes extrinsically stained by tobacco, medicine, or chromogenic oral bacteria

most common sites of oral cancer is
lateral border of tongue
lesion is normally asymptomatic but can be painful as lesion invades nerve tissue
periodontal therapy purpose
all of the periodontal therapy initiated and homecare instruction given are for the purpose of creating a healthy environment for the gingival tissue
even with restorative treatment, the impact on the gingival tissue must be considered to ensure the restoration’s longevity
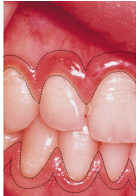
attached gingiva anatomy
gingival tissue that tightly adheres to the bone around the roots of the teeth
masticatory mucosa
pink in color with melanin pigmentation possible
stippling
interdental gingiva
the gingival tissue between adjacent teeth
extension of attached gingiva
forms the interdental papillae
col
nonvisible concave shape between the facial and lingual gingival surfaces (lies on interdental gingival)
varies in depth and width depending on the expanse of the contacting tooth surface
two teeth HAVE to be beside each other to have this
nonkeratinized tissue
attached gingiva width for incisor region
greatest usually in width
3.5 to 4.5 mm for maxillary
3.3 to 3.9 mm for mandibular
attached gingival width for posterior region
narrowest
1.9 mm and 1.8 mm on maxillary posterior and mandibular first premolars
marginal gingiva anatomy
at the gingival margin of each tooth
free gingival
follows scalloped pattern established by the contour of the CEJ of teeth
similar in clinical appearance to attached gingival
masticatory mucosa
more translucent than attached
mobile and free of underlying tooth surface which can be demonstrated with periodontal probe or blowing air into sulcus
marginal gingiva width
varies
0.5 mm to 2.0 mm from the free gingival crest to attached gingival
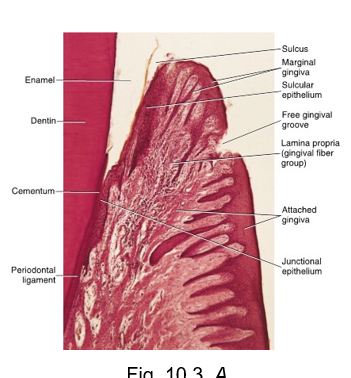
free gingival groove
separates the attached gingiva from marginal gingiva
slight depression on the outer surface of gingiva does not correspond to the depth of sulcus but rather to the apical border of junctional epithelium
masticatory mucosa
attached gingiva histology
has an overlying thick layer of mostly parakeratinized stratified squamous epithelium, which obscures its extensive vascular supply in the underlying lamina propria
pink tissue
lamina propria has tall narrow connective tissue papillae alternated with rete ridges, highly interdigitated
lamina propria directly attached to the underlying bone jaws
marginal gingiva histology
overlying surface layer of only orthokeratinized stratified squamous epithelium
underlying lamina propria has tall narrow papillae, continuous with the lamina propria of the gingival tissue that faces the tooth
is not attached to the underlying bony alveolar process → firm but mobile
nonkeratinized col
gingival fiber group located in lamina propria of marginal gingiva
biologic width
supracrestal tissue attachment
the combine heights of the suprabony soft tissue which is attached to the par of the tooth cornonal to the crest of the alveolar bone
commonly stated to be 2.04 mm
important to position of restorative margins