Molecules and Blood 🩸
1/74
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
75 Terms
Explain the potency of cells
Potency refers to how much the cell can differentiate:
Totipotent - can differentiate into any cell type in the body
Pluripotent - can differentiate into any cell type except the placenta, they are found in the embryo
Multipotent - can differentiate into blood cells, they are found in the bone marrow also known as adult stem cells
Unipotent - can only differentiate into one cell type eg skin
What is Haematopoiesis
Haematopoiesis is the differentiation of a multipotent stem cell into myeloid projector cells or lymphoid projector cells they can then further differentiate into blood cells such as RBS, lymphocytes, neutrals, monocytes, platelets, NK cells.
What is a zymogen
An inactive substance which is responsible for activating proteins
where is erythropoietin produced
kidneys
where is thrombopoietin produced
liver
function of erythropoietin
signals to RBC precursors in bone marrow to increase RBC proliferation
function of thrombopoietin
signals to platelet precursors and megakaryocytes in bone marrow to increase megakaryocyte production which will result in platelet shedding
How is RBC regenerated?
Signals are sent to RBC projector cells (erythropoietins) in the bone marrow, this triggers proliferation of the RBC, resulting in increased RBC production.
What are some advantages and disadvantages of stem cells
Adult stem cells have a fewer ability of differentiation, and are more difficult to isolate and culture, although embryonic stem cells are better at this there is ethical concerns around this such as destruction of an embryo, when does it become life, some believe it becomes life at conception.
Discuss Stem cells in cancer
There can be two types of stem cells transplant, autologous and allogenic. Allogenic is when a donors stem cells are transplanted, used for treatments in leukemia, thalassaemia, sickle cell anaemia. Autologous is used for some cases of MS, lymphoma, myeloma.
What is the definition of shock
Shock is a form of acute circulatory failure with inadequate oxygen delivery and utilisation of cells and it can result in organ dysfunction or death.
What are the different types of shock
Distributive; vasoregulation fails, so blood vessels often go leaky and dilated. anaphylactic, sepsis, neurogenic. Anaphylaxis is a response to allergic reaction. Sepsis is a toxic effect of inflammatory response. Neurogenic is vagal tone problems caused by spinal cord damage.
Hypovalaemic; haemorrhage and non-haemorrhage. Haemorrhage is a loss of blood and non-haemorrhage is the loss of fluids.
Obstructive; obstruction to the flow of blood to and from the heart
Cardiogenic; the heart fails to pump effectively
What is the symptoms of type 1 shock
Mental; normal
BP; normal
Pulse; <100
Resp; 14-20
Urine; >30
Blood loss; <750
% of blood volume; up to 15
What are the symptoms of type 2 shock
Mental; mildly anxious
BP; normal
Pulse; >100
Resp; 20-30
Urine; 20-30
Blood loss; 750-1500
% of blood volume; 15-30
What are the symptoms of type 3 shock
Mental; anxious
BP; decreased
Pulse; >120
Resp; 30-40
Urine; 5-15
Blood loss; 1500-2000
% of blood volume; 30-40
What are the symptoms of type 4 shock
Mental; confused
BP; decreased
Pulse; >140
Resp; >40
Urine; negligible
Blood loss; >2000
% of blood volume; >40
What are the types of wound
Abrasion; first layer of skin removed
Laceration; uneven edges, often goes deep
Incised; slash or a stab, can appear small but often go very deep and can be very dangerous
Degloving; the skin and the blood supply both come away
Biting; very unhygienic, can be human or animal
How should trauma be managed
Airways - is anything blocking their airway
Breathing - is the patient managing to breathe properly or do they sound wheezy etc
Circulation - pressure and elevation
What is the central dogma
Central dogma is the flow of genetic information. DNA > RNA > proteins
Explain the process of transcription
Initiation; RNA polymerase II binds to promoter and DNA strands separate
Elongation; RNA strand grows
Termination; RNA polymerase II dissociates
Compare the genome, transcriptome and the proteome
Genome; the entire genetic material composition that an organism has
Proteome; all of the proteins produces by an organism
Transcriptome; all of the mRNA of an organism
How can multiple proteins be produced from the same gene
Due to alternative RNA splicing of pre-RNA-transcript. This creates different mature mRNA transcripts which then code for different proteins.
What is a TF
A transcription factor is a factor which binds to small specific regions of DNA and can turn on/off transcription.
What is the role of activators and represseors
This is due to activators and repressors. Activators promote the binding of RNA polymerase II to promoters and repressors inhibit the binding of RNA polymerase II.
How can TFs be turned on/off
Enhancers promote the TF and gene expressions and Silencers prevent the TF and gene expression.
What is meant by primary, secondary, tertiary & quaternary
Primary; the order of amino acids
Secondary; the first role of amino acids and can be alpha helix, beta pleated sheets.
Tertiary; the 3D structure of a polypeptide
Quaternary; when two or more polypeptides are joined together.
What are some post translational modifications
Phosphorylation; alter activity of protein
Ubiquitination; label protein for degradation
Acetylation; regulate gene transcription
Glycosylation; folding in the ER
And there is proteolytic cleavage where proteins can be turned from inactive to active eg prothrombin > thrombin
What is constitutive gene expression
Genes which are always expressed, in every cell, at same stages. They are the genes which maintain basic cell function
What is inductive gene expression
Genes which are not always expressed, only expressed in certain cells and only at certain times.
How do mutations alter protein function and result in disease
A mutation causes amino acid sequence to be altered, the protein will then be wrongfully coded for and can result in it having a different function or shape so can’t carry out the role that it was intended to do. Eg Cystic Fibrosis is a mutation to CFTR protein which normally regulates mucus transport in the lungs and pancreas.
Outline the process of fibrinolysis
This is the process of converting fibrin into fibrin degradation products. Plasminogen is converted to plasmin and this is catalysed by tPA and thrombin, this causes the breakdown of fibrin, however there is also the inactivation of factor XIII as this will prevent fibrin from re-cross-linking.
What is the process of the coagulation pathway
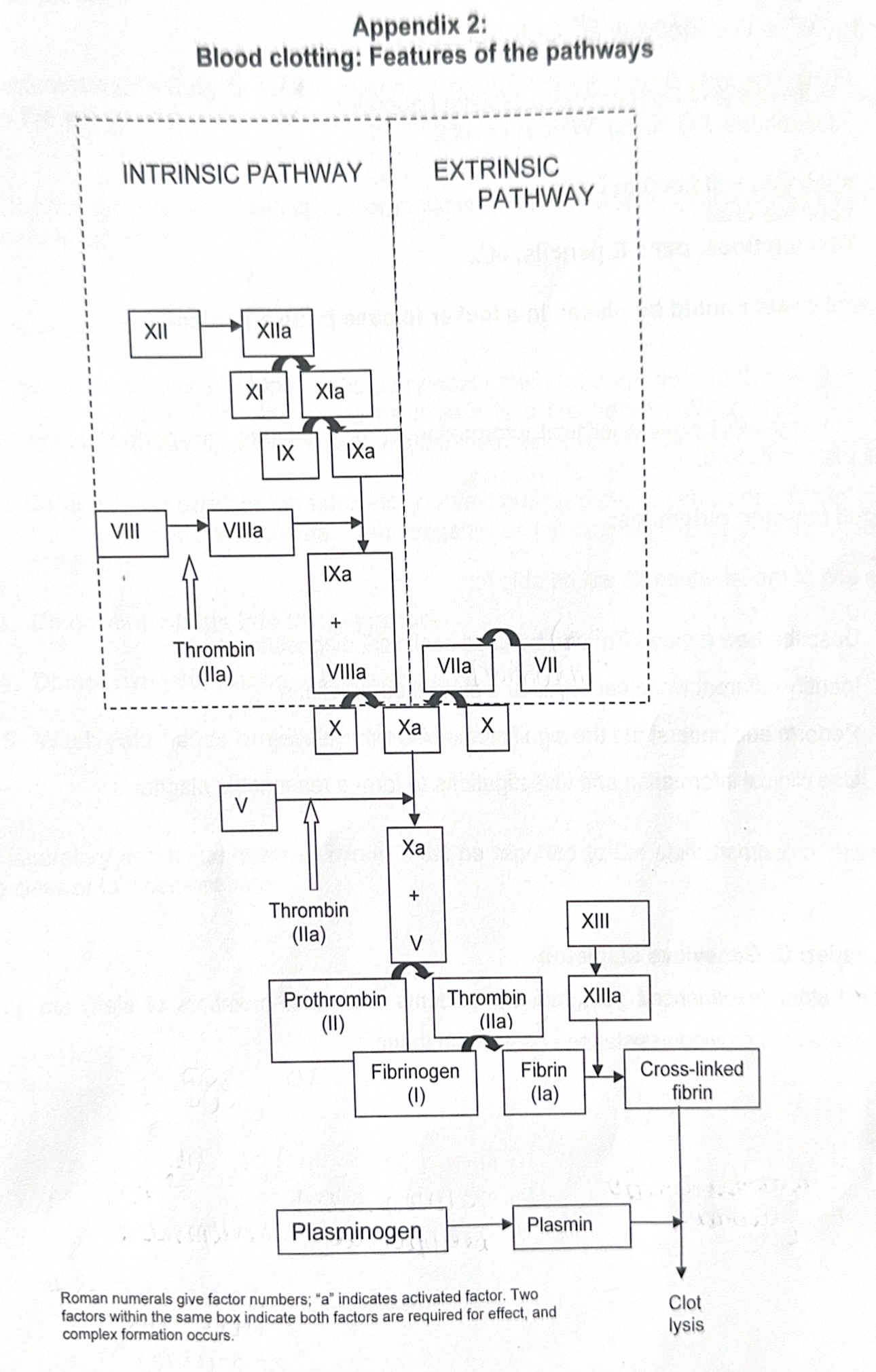
What effect does heparin have on coagulation
Heparin binds to and enhances the role of AT III, this inhibits both the intrinsic and common pathway
How does Warfarin effect the coagulation pathway
warfarin is a vitamin K antagonist so it blocks the liver from using vitamin K to create coagulation factors, meaning this can effect the whole pathway.
How does Benzamide effect the coagulation pathway
it competitively inhibits prothrombin and factor X, without these fibrinogen will not be converted to fibrin so a clot will not be formed
How does amino-caproic acid affect the coagulation cascade
Amino-caloric acid is an anti-fibrinolysis, meaning it inhibits the plasminogen to prevent the formation of plasmin, so clots cannot be broken down
What is the role of chelated calcium
Chelated calcium is an anti-coagulant, it is formed when sodium citrate/EDTA is added to calcium
What is an APTT assay
An APTT assay measures the length of time it takes for a clot to form from the initiation of the INTRINSIC pathway.
What is a PT assay
A PT assay measures the length of time it takes for a clot to form from the beginning of the EXTRINSIC pathway.
What does it mean if an APTT assay with a low value
This means that there is an increased chance of blood clotting which can be very dangerous, this could be due to an excess in any of the factors involved.
What does it mean if an APTT assay is too high
This means that a person is not forming clots fast enough and they may be experiencing excessive blood loss, this could be due to factor deficiency resulting in haemophilia, a presence of an inhibitor, VWD or vit K deficiency.
What happens if someone has a vitamin k deficiency or liver disease
If someone has a vit K deficiency then they may fail to create coagulation factors. If they have liver disease then this the liver may fail to signal to vit K to produce coagulation factors.
What can occur when APTT is too low
DVT; a blood clotting in the leg which has the ability to move elsewhere
PE; a blood clot in the lung which can prevent oxygen as it blocks a pulmonary artery
Stroke; a blood clot in the brain due to a lack of blood and oxygen to the brain, can cause brain damage if it goes without oxygen for so long or can cause death
Heart; blood clot in the heat can prevent blood from leaving/entering the heart, this can cause cardiac muscle to die ore cause a myocardial infarction.
What is the causes of haemophilia
Haemophilia A - factor VIII deficiency
Haemophilia B - factor IX deficiency
It is an X-linked genetic disorder
What is the effect of VWD
This is when there is a deficiency in VWF making it more difficult for platelets to bind or prevents them, making the formation of a platelet plug more difficult or preventing the formation.
What is the components of the blood
Red blood cells, white blood cells, platelets and plasma
What is the role of plasma
Plasma carries blood cells, nutrients, hormones, antibodies around the body. It also regulate temperature and pH and maintains blood pressure and volume.
What is the function of RBC
They are necessary in the transportation of oxygen from the lungs to tissues and also transport CO2 from tissues to lungs
What is the structure of RBC
They have a biconcave shape which maximises surface area for transportation of oxygen, when oxygen binds to RBC the haemoglobin in them becomes oxyhaemoglobin. Haemoglobin is composed of 4 haem groups and 4 polypeptides (2 alpha & 2 beta). RBC are produced by the bone marrow and the bone marrow is instructed to do this by erythropoietin which are produced in the kidney of adults. RBC are removed by the spleen. When the haemoglobin within RBC clumps together it creates sickle cell anaemia.
Describe the formation of the platelet plug
Firstly there is vasoconstriction of the blood vessels to prevent the loss of lots of blood. The sub-endothelial lining is exposed as well as the collagen, collagen creates a sticky base which Von Willebrand factor binds to, the platelets then bind to the VWF and signal other platelets to bind to the VWF. Platelet aggregation then occurs and they all clump together and form a temporary clot. This is primary haemostasis.
What is the function of platelets
To form blood clots
What is the function of monocytes
They clean up damaged cells
What is the function of Lymphocytes
There is two types; T & B. They protect against viral infections by producing antibodies.
What is the function of Neutrophils
They kill bacteria, fungi and foreign debris
What is the function of Basophils
They carry out an allergic response
What is the function of eosinophils
They kill cancer cells and parasites
What are some effects of mutations in TF
Mutation to binding site; thalassaemia, the amount of mRNA produced may be reduced
Mutation to TF; p53 mutation (found in 50% of cancer patients), distrusts the normal cell cycle
What results in basal levels of transcription
basal TF binding
What is a zymogen
A zymogen is an inactive substance which activates proteins.
What are the two factors involved in gene expression
TF and the structure of DNA
How does the structure of DNA effect gene expression
Euchromatin is open - gene can be expressed
Heterochrmatin is closed - gene cannot be expressed
This is due to proteins called histones which bind DNA, modifications to histones causes DNA to wrap/unwrap. Locus control regions can also cause chromatin to open.
Define coagulation
Formation of a blood clot, blood goes from liquid to solid
Define anticoagulant
compounds which prevent blood clotting
What is haemostasis
the stopping of bleeding
What is thrombosis and thrombus
Thrombosis is the formation of a dangerous blood clot
Thrombus is the blood clot
What is the role of proteolysis in clot formation
Proteolysis can convert inactive proteins to active proteins so can activated the coagulation cascade.
Where are the different types of stem cell found
Totipotent; zygote
Pluripotent; inner cell mass of zygote
Multipotent; bone marrow
What is the cause of factor V Leiden
Factor V is usually activated/inactivated by protein C, when an individual has factor v Leiden it resists the effect of protein C causing blood clotting to go on for longer, forming excessive blood clots.
What is the effect of prothrombin gene mutation
This is when there is a mutation to the Factor II gene, this causes the production of too much prothrombin.
What is the effect of protein S deficiency
Protein S is a natural anticoagulant, without it it may be difficult for the body to control the coagulation pathway.
What is the effect of excessive clotting factors
Too many clots will be made
What is albumin and globulin
These are components which make up the blood plasma, albumin has a function in maintaining fluidity and pressure whilst globulin is responsible for transportation of substances, nutrients, hormones
What factors do vitamin K effect
Factor 2, 7,9,10
What component mimics the negative surfaces of activated platelets in the APTT?
Phospholipid/Kaolin mimics the negative surfaces of activated platelets to initiate the intrinsic pathway.
what factors does calcium impact in the cell cycle
factor 11 activating factor 9, factor 8 and 7 in activating factor 10, factor 10 in activating factor 2, and fibrin into a clot