Feeding, Eating, Sleep, and Rest
1/143
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
144 Terms
Feeding
Setting up and bringing food to mouth.
Eating
Manipulating the food or fluid in the mouth and swallowing.
Pediatric Feeding Disorder
Impaired oral intake that is not age-appropriate and is associated with medical, nutritional, feeding skill, and/or psychosocial dysfunction.
Common Challenges Associated with Feeding and Eating
- Gastroesophageal reflux disease (GERD)
- food allergies
- poor oral motor function
- difficulties with tongue function
- drooling
- challenging behaviors such as gagging and sensory-related responses.
Gastroesophageal reflux disease (GERD)
frequent or chronic vomiting after eating (normal for babies until it is persistent, or affects child's health or ability to eat successfully
Poor oral motor function
difficulty with chewing and swallowing (ex: suck-swallow coordination and drooling) that may lead to food refusal, selectivity behaviors, vomiting, prolonged mealtimes, poor weight gain, and failure to thrive
macroglossia
The tongue is disproportionately large in comparison to the mouth or jaw, often seen in Down syndrome, and may require therapy to reduce tongue-thrust movements, anterior food loss, and drooling
At what age is drooling considered atypical or pathological?
after 4 y/o
3 multiple choice options
sensory-related responses
- oral hypersensitivity
- oral sensory awareness
- low sensory registration
oral hypersensitvity
adverse reaction to oral stimuli
Children who are less willing to explore food with their hands to finger-feed independently or become upset with spilling food may have what kind of sensory-related response?
oral hypersensitivity
2 multiple choice options
Children who seek oral sensory stimulation by mouthing on objects, have limited awareness of drooling, and show preference for specific altering food textures or flavors may have what kind of sensory-related response
poor oral sensory awareness
2 multiple choice options
Children who tend to eat a slow pace and require frequent cueing to persist with eating at mealtimes may have what kind of sensory-related response?
low sensory registration
2 multiple choice options
OT practitioners collaborate with all the following people for feeding and eating therapy except:
social workers and case managers
3 multiple choice options
What is the benefit of a multidisciplinary approach for feeding and eating interventions?
can lead to successful weaning from tube feedings, increased oral intake, improved mealtime behaviors, and reducing parenting stress.
t/f OT practitioners should use a holistic approach for eating and feeding interventions
true
consider the setting, cultural expectations, and experience with feeding and eating
universal safety precautions
- wash hands frequently
- wear gloves
- abide by dietary restrictions
- recognize signs of distress or safety concerns
feeding and eating interventions
- adaptive equipment
- activities that promote grasp and release and AROM
- positioning for oral prep phase
- oral motor skills for oral prep phase
- reduce oral motor control for drinking
- drooling
- pharyngeal phase
- aspiration risk
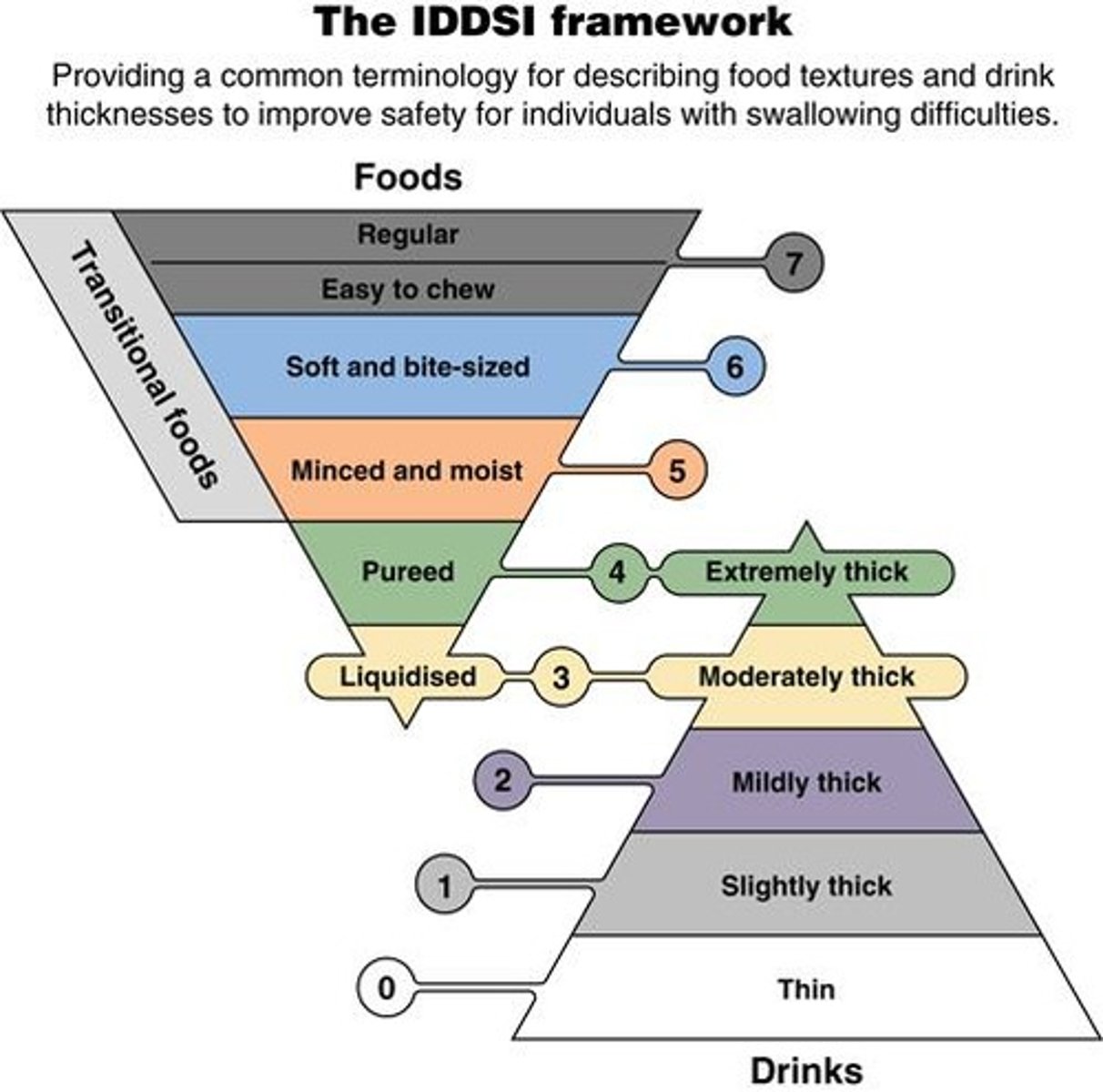
- modifications for food and liquid consistency
- esophageal phase
- improving behaviors
- sensory interventions
A child has weak hand grip and limited finger strength, making it difficult to hold a spoon or fork. Which adaptive equipment would be most beneficial?
Lightweight utensil with a built-up handle
3 multiple choice options
A child tends to knock over bowls and plates while eating due to uncoordinated arm movements. What adaptation would help the most?
Nonskid place mat or suction cup dish
2 multiple choice options
A child has difficulty keeping food on the spoon because it slides off the edge of the plate. What adaptation could increase independence during self-feeding?
Scoop dish or sectioned plate with raised edges
3 multiple choice options
A child with poor fine motor skills struggles to lift and control a cup. Which adaptation is most appropriate?
Cup with a handle
3 multiple choice options
A child frequently spills drinks when setting a cup down on the table. Which adaptation would best prevent spillage?
Cup with lid or wide base
3 multiple choice options
A child has limited arm movement and cannot easily lift a cup to drink. Which option would best promote independence?
Long straw in a secured cup holder
3 multiple choice options
A child needs extra trunk and arm stability when self-feeding. Which adaptation is most helpful?
Adaptive seating with stable tray
3 multiple choice options
A therapist wants to reduce fatigue and improve endurance for a child who tires easily while eating. What strategy would help?
Stabilize the elbow on the table or tray
3 multiple choice options
Promote Grasp & Release & AROM
Utilizes biomechanical and developmental approaches, motor learning techniques, ROM, strengthening, endurance, and coordination.
A child with severe and complex physical limitations needs a way to eat independently. Which adaptation is most suitable?
Mobile arm support or electronic feeding system
3 multiple choice options
A child with visual discrimination difficulties has trouble locating food and utensils on the table. What environmental adaptation would best support them?
Consistent food placement and contrasting colors for tableware
3 multiple choice options
Using the biomechanical and developmental approach, what feeding skills are mainly targets for grasp and release interventions?
- pinching finger foods
- grasping utensils
- scoop foods and successfully bring to mouth
- cutting food into pieces
Which body functions are mainly addressed in intervention activities using the Biomechanical Approach?
ROM, strength, endurance, and occupation
How is motor control different than the biomechanical approach?
Focuses on addressing movement through meaningful, whole, and repetitive practice
t/f It is best to use fake food outside of regular meal/snack times to engage the child in feeding and eating activities
false
it is best to use actual food at regular meal/snack times
oral preparatory
container to oral manipulation = food bolus
oral propulsive
moves bolus posteriorly
pharyngeal phase
swallow is triggered
esophageal phase
food moves through the esophagus towards stomach
What is the ideal position for infants who are breat or body feeding during the oral prep phase?
Midline positioning with full support of head and body and gently flexed posture
What is the ideal feeding position for older children during the oral prep phase?
hips>90/knees 90/feet flat on the surface or on a step will assist with coordination
What kind of position assists with swallowing?
Slight flexion in trunk and neck
What kind of position may reduce tonic bite (CNS issue) or tongue thrust?
slight head flexion
Which position poses a choking pazard?
supine
Side-lying on incline positions may be recommended for what skill performed in the oral prep phase of eating?
May be recommended for suck-swallow-breathing coordination
Why is side-lying on incline position recommended for suck-swallow-breathing coordination?
Gravitiy eliminated positions allow fluids to go down slower which gives infants more time to suck, swallow, and breath in order and in rhythm
When is the upright position for efficient oral preparation in eating recommended?
More upright position recommended.
High-chairs adaptation
Can be adapted with small towels to maximize lateral support, stability, alignment and improve oral motor skills for oral intake.
How does a Tumble form feeder chair and Special tomato chair assist with positioning during the oral prep phase of eating?
Offers support and an adjustable feeding angle
Why is strengthening the lips and cheeks important oral motor skills for the oral prep phase?
Adequate lip closure and lip seal are needed for sucking and oral control (prevent spillage and drooling).
What kind of interventions can be used for a child with a cleft lip that has difficulties with oral motor skills?
- adaptive equipment (such as adaptive bottles)
- upright positioning (uses gravity and liquids spend less time in mouth)
How do OTs address abnormal tightness in the lips and cheeks to improve oral motor skills?
Requires AROM/PROM.
How do OTs address limitations in oral motor skills that present as open jaw and drooling in children?
Strengthening interventions due to weak lips and cheeks
What kind of tongue activities can OTs implement for children with deficits in oral motor skills?
Silly faces in the mirror, lick (lollipops, frosting, whipped cream), stimulating tongue and cheeks with a Nuk brush.
Dissociation from jaw
Refers to the ability to move the tongue independently from the jaw.
Lateralization
Beneficial for children with a tongue thrust
How can OTs elicit tongue lateralization to improve oral motor skills?
present spoon or food to side of mouth instead of midline to promote backward movement of tongue
What are the presentations of limited jaw posture?
Open mouthed posture, drooling, food/liquid loss during feeding/drinking.
Non-nutritive chewing activities
Repetitive chewing on a resistive device (p & q) to strengthen jaw
Nutritive activities
Provide fruits and vegetables in a mesh bag and progressively chewy foods to decrease the choking risk and strengthen the jaw
What is the purpose of providing jaw support, handling, and positioning for a child who has difficulties with eating in the oral prep phase?
To improve oral motor skills and provide stability for the child to maintain adequate head alignment
When introducing foods to a child who is developing chewing skills, which type of food consistency should be introduced first?
Smooth and even consistencies
1 multiple choice option
A child is learning to transition from purees to solid foods. Which type of food would be most appropriate to introduce next to promote safe chewing practice?
Meltable solids (e.g., puffs, crackers that dissolve easily)
3 multiple choice options
To help a child improve chewing skills safely, a therapist might recommend progressing from:
Smooth purees → Meltable solids → Dense or crunchy foods
3 multiple choice options
What structures and skills are considered when creating interventions to improve oral motor skills?
- lips and cheeks
- tongue
- jaw
- chewing
Infants with weak suck, limited endurance, and/or anatomic differences (such as a cleft lip) may benefit from these.
Adaptive bottle systems

Why is introducing smaller straws better for drinking interventions?
requires less suction and delivers smaller amounts of liquid.
What are examples of devices that can be used to support drinking for children with limitations oral prep phase?
- Honey Bear
- sippy cups
- u-shaped cut out cups
What is the Honey Bear device used for in eating interventions? Bottles with squeeze assist
Assists with the squeeze to support drinking

How are sippy cups beneficial for supporting drinking?
Different spout varieties and non-spill valves.
What are U-Shaped cut out cups used for and what kind of deficits are addressed with this device?
Maintaining a neutral head position during drinking for children with extensor tone or poor head control.

Why would children benefit from drinking thickened liquids at the start of learning how to drink from a cup?
to compensate for limited oral control or swallowing abilities
Which oral motor goal is most directly related to helping a child reduce drooling?
Promoting lip closure and tongue movements
3 multiple choice options
A therapist places a small piece of food on the side of a child’s mouth to encourage chewing and licking. What specific skill is this activity targeting?
Encouraging lateral and rotary tongue movements
3 multiple choice options
Training on sensory awareness is used to help children reduce drooling by:
Helping them recognize when saliva is escaping and swallow more often
Which of the following interventions would be most appropriate for a child who has reduced oral awareness and poor lip control contributing to drooling?
Sensorimotor exercises for lips and tongue
What kind of oral motor activities and interventions can be used to reduce drooling?
- promote lip closure and tongue movements
- lateral and rotary tongue movements
- sensory awareness training
- sensorimotor exercises
Aspiration
Food in airway before, during, or after a swallow, which can lead to lung disease, pneumonia, and other medical problems.
Signs of aspiration
- coughing
- gurgly voice
- wet breathing
- multiple swallows
- frequent respiratory illnesses
- prolonged mealtimes
- oral motor dysfunction
VFSS
Videofluoroscopic swallow study.
FEES
Fiberoptic evaluation of swallowing.
what is the VFSS and FEES used for?
after signs of aspiration it can be used to observe the swallowing mechanics in children
what kind of methods might be required of chronic aspiration and medical complications?
non-oral feeding such as a feeding tube
Interventions for the pharyngeal phase of swallowing
- changes in positioning
- method of presenting foods and liquids
- adjusting food or liquid consistency
- non-oral feeding
An occupational therapist is evaluating a 3-year-old child who frequently coughs during meals, has a gurgly voice after swallowing, exhibits wet-sounding breathing, and often requires prolonged mealtimes. The child’s caregiver also reports multiple respiratory infections over the past few months. Which of the following should be the therapist’s primary concern during feeding sessions?
Monitoring for signs of aspiration and referring for a swallowing evaluation
3 multiple choice options
Chin tuck
Reduces laryngeal opening; may be contraindicated for infants with softening of the cartilage of the Larynx or Trachea which may cause damage
what kind of position is recommended for CHILDREN to reduce aspiration and support optimal swallowing? and why?
chin tuck is recommended because it reduces laryngeal opening and less food slips into the wrong pipe
what kind of position is recommended for INFANTS to reduce aspiration and support optimal swallowing? and why?
side-lying is recommended because it is in a gravity minimized position which requires less effort and time to swallow
what devices can be used to promote a Natural chin tuck for flexion in eating?
Promoted via straw or straw style sports bottle.
what age should children start drinking in an upright position?
6 months
what are some ways to change the presentation of food and liquids?
- offer an empty spoon
- change the pace of oral feeding
- present more difficult foods first
-smaller bites of foods or sips of liquid
Empty spoon technique
Offer an empty spoon in the same way as a bite of food to stimulate oral movements.
Pace of oral feeding
Provide recommendations to allow the child sufficient time to swallow between bites.
An occupational therapist is providing feeding interventions for a 4-year-old child who demonstrates delayed oral motor control and difficulty coordinating swallowing. The therapist wants to promote safe and efficient oral intake. All of the following interventions are appropriate EXCEPT:
Increasing the pace of feeding for faster eating and increase mealtime duration
3 multiple choice options
t/f Thin liquids offered from an open cup are most difficult to control during swallowing.
true
Thickened liquids examples
Simply thick, Gelmix, Purathick.
why is room temperature water the most challenging liqud?
there is minimal feedback when swallowing
An occupational therapist is working with a 5-year-old child who demonstrates difficulty safely managing thin liquids during feeding. The therapist plans to modify the child’s food and liquid consistency to promote safer swallowing. All of the following recommendations are appropriate EXCEPT:
Offering room-temperature water from an open cup to provide swallowing practice with challenging textures
3 multiple choice options
behavioral interventions for feeding and eating
- create new positive interactions and associations with feeding and mealtime
- positive reinforcement
- systematic desensitization
- CBT
Systematic Desensitization for feeding and eating
targets feeding behaviors by slowly exposing children to new or nonpreferred foods at their comfort level, with encouragement of playful food interactions to increase the child's variety of accepted foods
CBT for feeding and eating
addresses the child's feelings, thoughts, and behaviors and targets their mood and anxiety. children with ARFID may benefit from this
Structuring Mealtimes
Helps promote hunger cues and reduces access to less nutritious foods.