9. Corneal Edema and Metabolism
1/86
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
87 Terms
What is the water content when there is cornea edema?
>78%, it occurs when the leak mechanism outweighs pump function
How much does the cornea's water content need to change before its transparency is affected?
>5% increase in hydration can cause light scattering and decreased refractive function
Which regions of the cornea is affected by edema?
The stromal and epithelial portions of the cornea
Are the regions affected simultaneously?
Yes, but can occur independently.
What physical changes occurs with corneal edema?
The posterior curvature is affected, anterior curvature is typically not affected due to interweaving of lamellae resisting expansion.
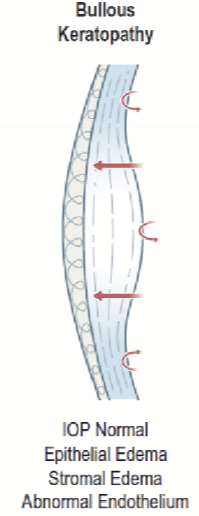
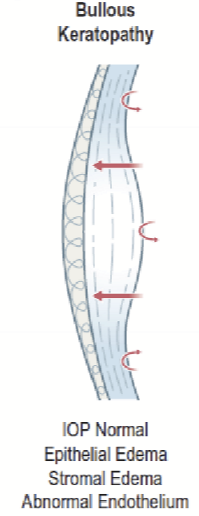
What is bullous keratopathy?
A condition where the endothelium fails to maintain proper fluid balance leading to corneal edema and epithelial blisters
What causes bullous keratopathy?
Fuch's Endothelial dystrophy
Injury
Surgery
Hypoxia
What forces regulate corneal hydration?
Imbibition pressure (IP)
Stromal Swelling Pressure (SP)
Intraocular Pressure (IOP)
Endothelium pump
Tear evaporation/Osmosis (minor)
What is imbibition pressure?
The normally negative pressure that draws fluid into cornea. It is generated by the negatively charged GAGs drawing in Na+ from aqueous humor.
What is the normal imbibition pressure value?
-40 mmHg
What does a positive imbibition pressure indicate?
Water is leaving the stroma.
What force counteracts imbibition pressure?
Endothelial pump
What is imbibition pressure dependent on?
Water content. It increases, approaches zero, with increasing water content. It decreases with decreasing water content. It is also affected by IOP.
What is swelling pressure (SP)?
An outward force generated by GAGs repelling against each other.
What is the normal value of swelling pressure (SP)?
55 mmHg
What is the relathioonship between SP and water content?
It is inversely related to each other. It decreases with increased water content and increases with decreased water content.
What is the normal value for Intraocular pressure (IOP)?
15 mmHg
What regulates IOP?
It is regulated by equilibrium of aqueous production and drainage.
Where is the force directed?
From the anterior chamber towards the endothelium as water is “forced” inot the cornea via hydraulic pressure
How is Imbibition pressure calculated?
Imbibition pressure = IOP - Swelling pressure
What happens to IP and Sp when the endothelial pump is compromised/decreased?
IP increases/ is less negative and SP decreases
What forces are not at normal during bullous keratopathy?
Lowered SP, causing a lowered IP. The stromal edema is due to leak exceeding pump function and the epithelial edema is due to IOP exceeding pump function, causing excess water to be forced between epithelial cells.
What causes stromal edema?
Leak exceeding pump function
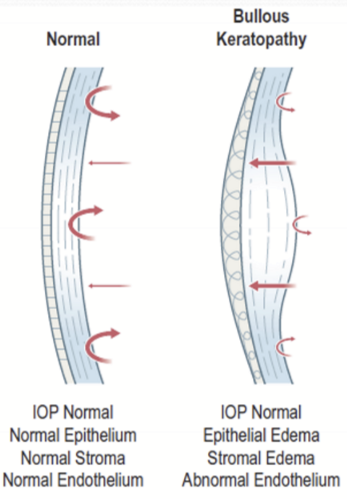
What causes epithelial edema?
IOP exceeding pump function, forcing excess water between epithelial cells
What happens if the IOP exceeds the SP?
Epithelial edema without stromal edema. IP becomes positive, causing water to be pushed out of the stroma. Epithelial microcysts are often present.

What happens if there is a loss of pump function?
IOP becomes zero and there is only stromal edema. Epithelium does not have IP, so no water is drawn into the epithelium. Over time, IP and SP will become zero.
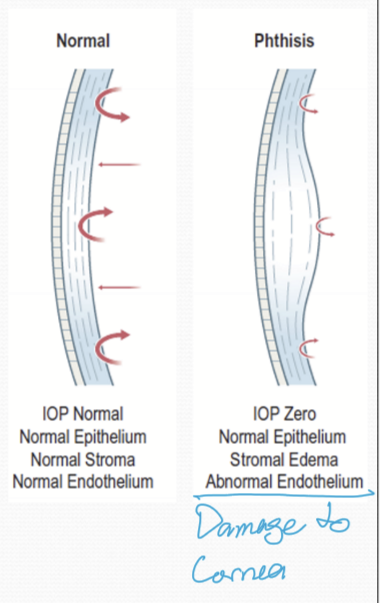
Why does IP and SP become 0 mmHg over time after pump function is loss?
As water is drawn into the stroma, IP gets closer to zero and SP is reduced towards zero too.
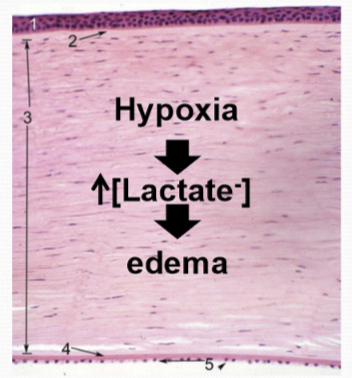
What happens to the stroma during hypoxia?
There is an increase in anaerobic metabolism, causing a build up of lactate → oxmotic draw of water. the pH is also reduced → inhibits pump function and ion transport efficiency reduced. This causes edema.
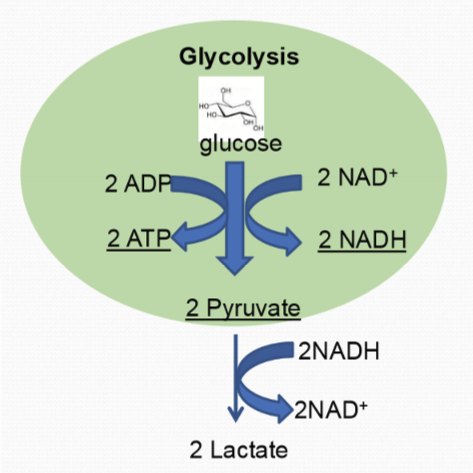
What are some characteristics of the glycolytic pathway?
It occurs in teh cytoplasm
No O2 requirement
From 1 glucose → 2 ATP, 2 NADH, 2 Pyruvate
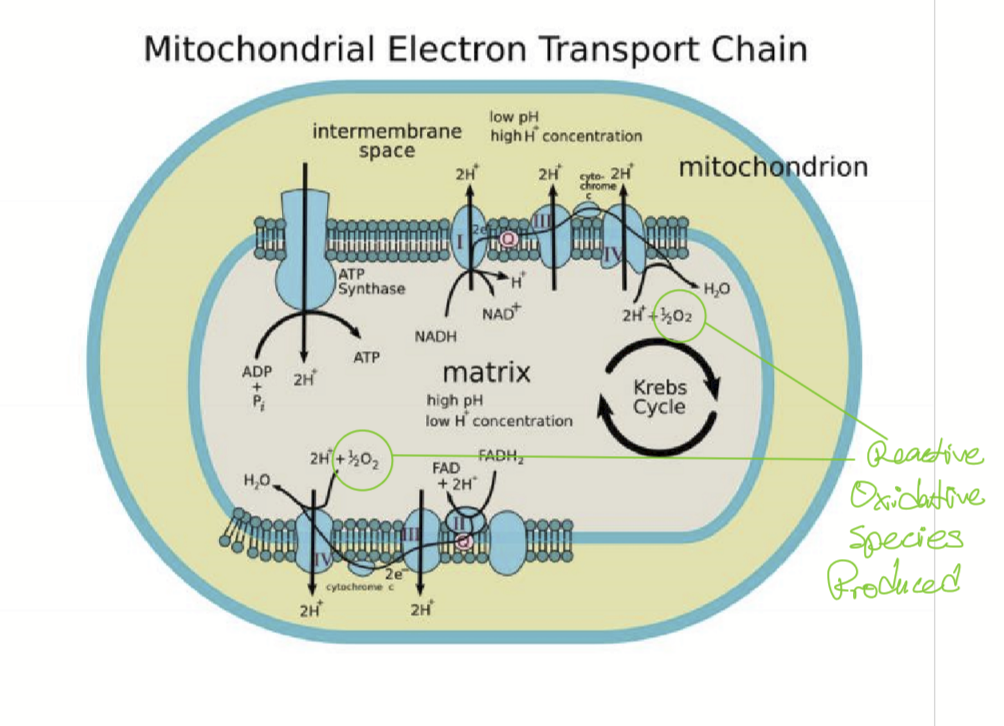
Where does Oxidative Phosphorlyation/TCA take place?
In the mitochondria and requires O2
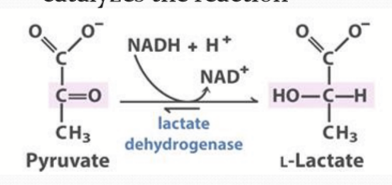
What happens to pyruvate in anaerobic glycolysis?
Lactate Dehydrogenase converts the 2 pyruvate and 2 NADH to 2 lactate and 2 NAD+.
What happens to the cornea during sleep?
It swells due to the hypotonic tears and hypoxic metabolism.
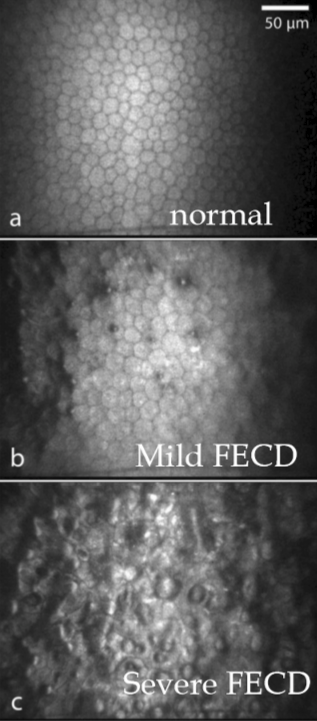
What happens in Fuch’s corneal dystrophy (FCD) or Fuch’s endothelial corneal dystrophy (FECD)?
There is a gradual loss of endothelial cells, which appears as guttata formation. As endothelial cell density decreases, the guttata expand, leading to mild corneal edema. Over time, the severity of edema increases, resulting in corneal opacification, pain, and vascularization.
What are the risk factors for FCD or FECD?
Sex: FCD more common in women vs men
Genetics: family history
Age: affects typically observed in 30-40s
Why does guttata negatively affect the endothelial cell layer?
It affects the adhesion of the endothelial cell layer to the stroma, pump function, and cell viability, reducing the endothelial cells ability to pump water out of the stroma.
What are the layers of Descemet’s membrane?
Banded layer
Posterior non-banded layer (PNBL)
What is unique about the PNBL?
It increases in thickness ~1 micron/year and is made up of Collagen Type IV
What collagen does the banded layer of descemet’s membrane use?
Primarily Collagen VIII. It is formed during embryonic/fetal development. It does NOT increase with age.
What congenital mutation causes FCD or FECD?
COL8A2 gene, encoding Collagen VIII protein, causing a thicker Descemet’s membrane, abnormal accumulation of COLVIII in posterior, and disturbed assembly of COLVIII in banded layer.
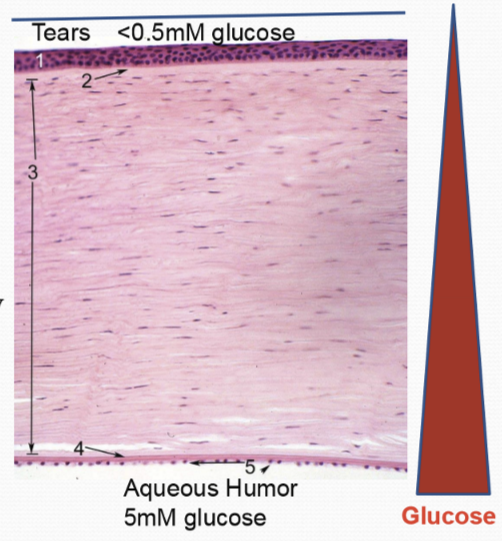
What provides the main source of glucose for the entire cornea?
Aqueous Humor, at 5 mM of glucose concentration provides 90% of glucose for entire cornea.
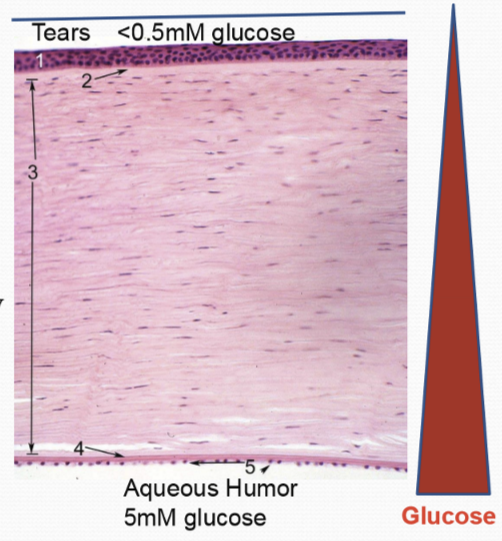
What are some other sources of glucose for the cornea?
Minor amount comes from glycogen stores in epithelium (10%)
A negligible amount comers from tears and limbus
What is the major transporter of glucose into corneal cells?
GLUT, glucose co-transporter.
Where are GLUT expressed?
In the epithelial and endothelial cells
What is glucose used for in the cornea?
Anaerobic glycolysis (85% utilization)
Aerobic glycolysis
Hexose-Monophosphate Shunt (HMS)
What dictates the pathways that glucose is utilized?
O2 concentrations
Mitochondrial number
Active enzymes available
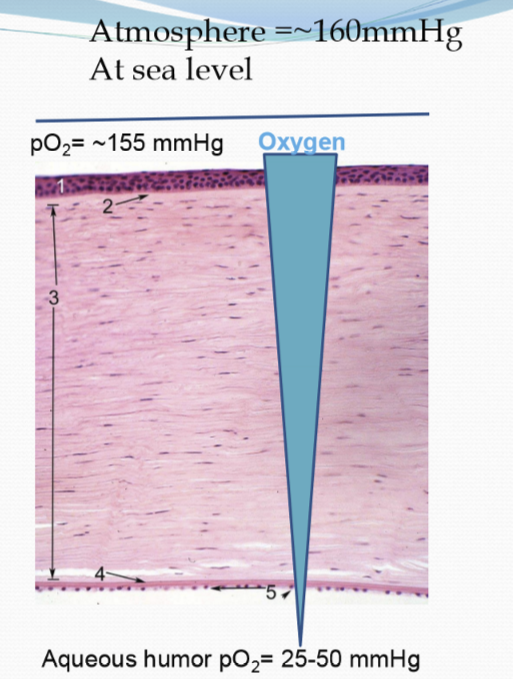
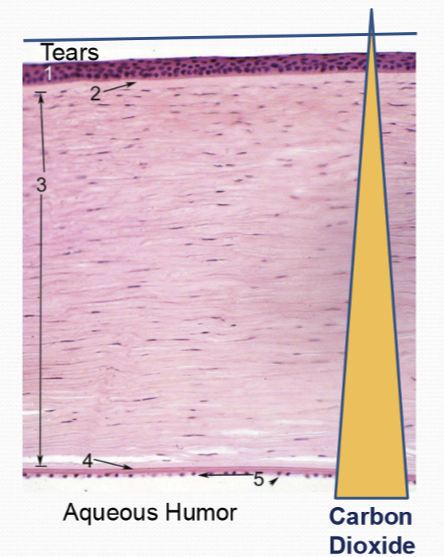
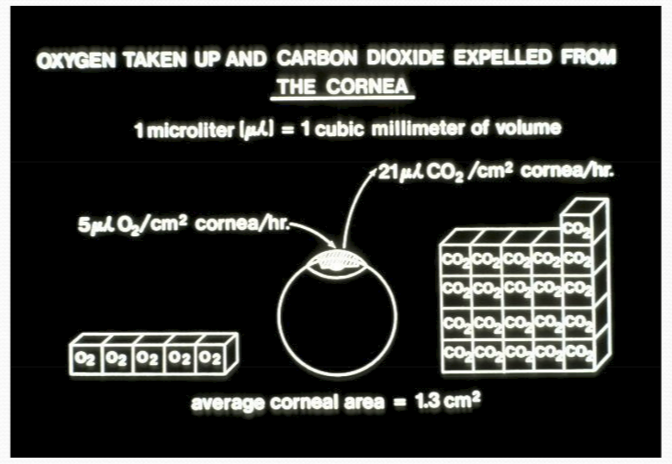
Where does the oxygen for the cornea come from?
The tear film and diffuses posteriorly in an open eye
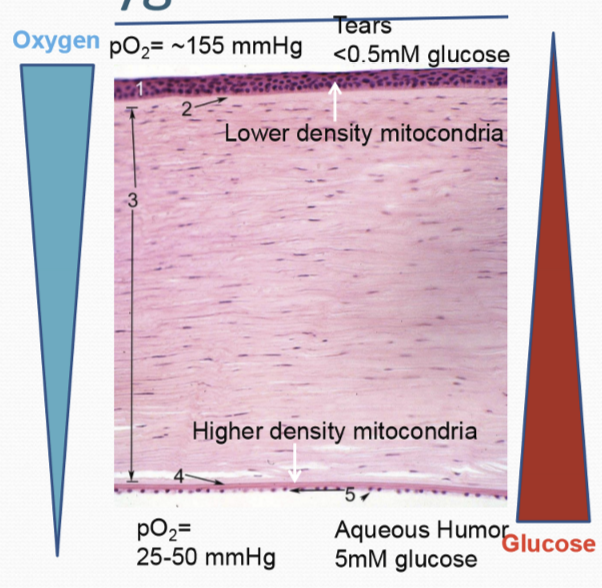
What is glucose metabolism dependent on?
Partial pressure of O2
What is metabolism affected by?
Mitochondrial density
Which corneal cell layer contains more mitochondria, the endothelium or the epithelium, and why?
The endothelium has more mitochondria due to its higher metabolic demand from the ion pumps.
How is the oxygen gradient generated?
The O2 gradient is generated by the consumption of O2 by the layers of the cornea and the difference in partial pressure of oxygen in the atmosphere vs aqueous humor.
What is the predominate metabolism in the cornea?
Anaerobic metabolism
What is the energy yield of aerobic metabolism?
36 ATP total. 2 from glycolysis, 2 from TCA, 32 from oxidative phosphorylation
What is the energy yield of anaerobic metabolism?
2 ATP total, from glycolysis. Also 2 pyruvates.
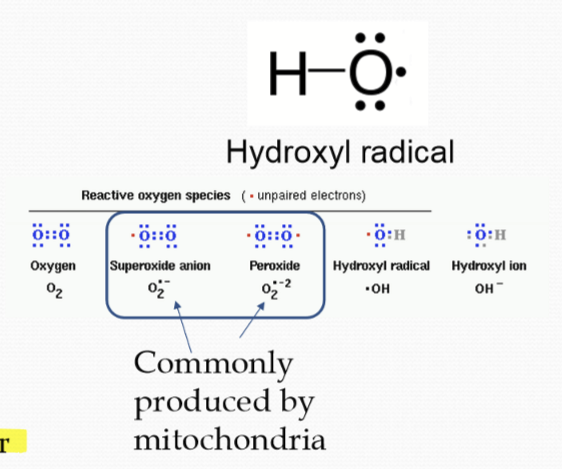
What are some byproducts of aerobic metabolism?
Reactive Oxygen Species (ROS), which are oxygen containing molecules missing an electron (radical).
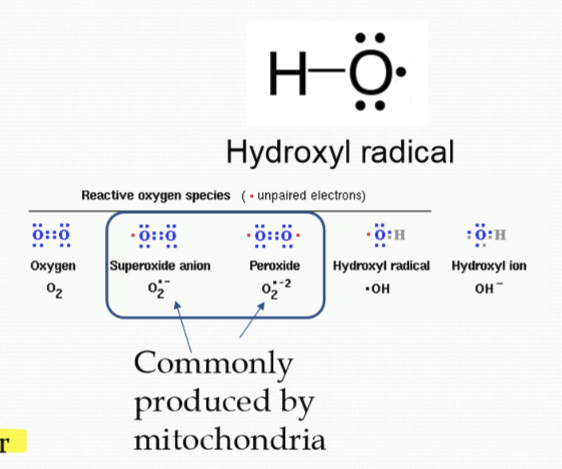
When are ROS made?
It is formed during mitochondrial metabolism.
Why are ROS bad?
They are highly reactive with other biomolecules.
What do the corneal cells use to detoxifying ROS?
Ascorbic Acid and ALDH3A1. Ascorbic acids is a strong electron donor and ALDH3A1 is an enzyme that metabolizes toxic aldehydes into carboxylic acids to reduce oxidative damage.
How does Ascorbic acid and ALDH3A1 regain their lost electrons?
They gets their electron via the glutathione pathway
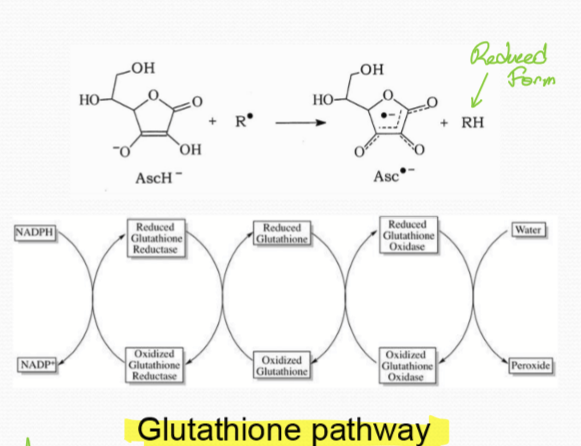
What does the glutathione pathway rely on to work?
NADPH
How does the cell know the glutathione pathway is working?
It monitors the ration of NADPH and NADP+
What metabolism does the corneal epithelium undergo?
Anaerobic metabolism/anaerobic glycolysis despite the high pO2 due to the few mitochondria found in the corneal epithelium.
What metabolism does the corneal endothelium undergo?
Since there are more mitochondria present, more aerobic metabolism , but total cornea metabolism is still predominantly anaerobic.
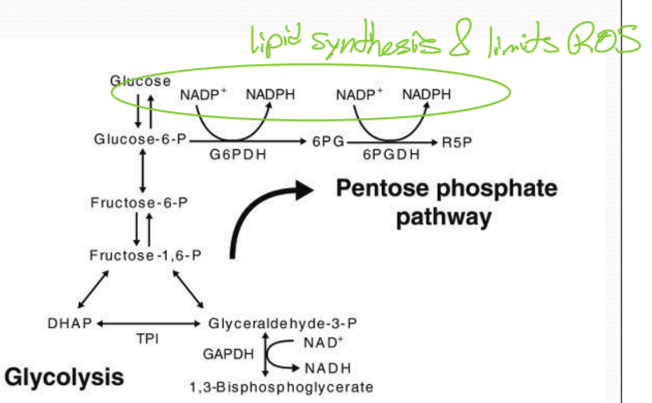
What and where is the Hexose Monophosphate Shunt (HMS)/ Pentose Phosphate Pathway used for?
The corneal epithelium utilizes it to produce NADPH and ribose-phosphate.
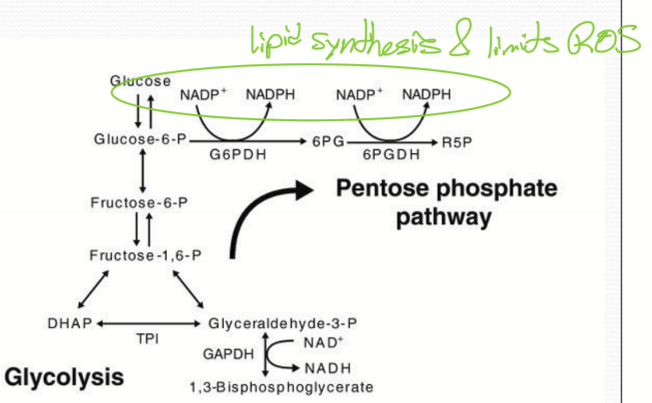
What is NADPH used for in the cell?
Synthesis of lipids
Limits ROS generated by aerobic glycolysis
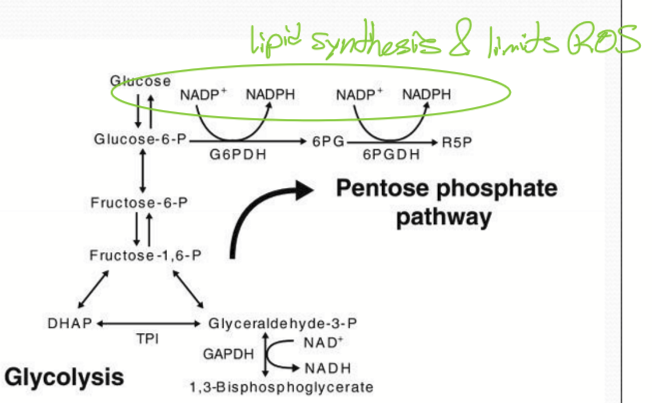
What is ribose-phosphate used for?
The synthesis of RNA and DNA
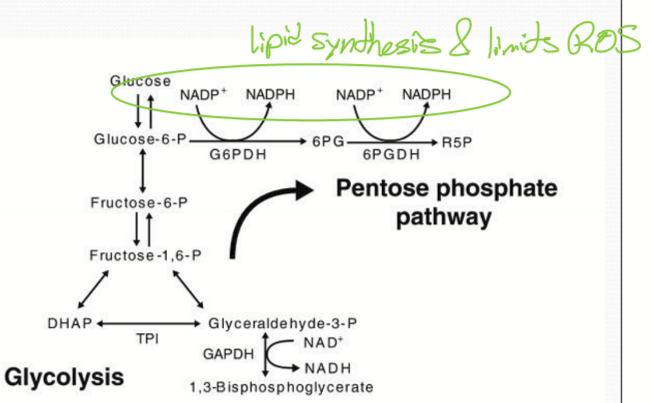
What enzyme is essential for HMS?
Glucose-6-phosphate dehydrogenase (G6PD)
What substrate does HMS use to start its pathway?
Glucose-6-phosphate diverted from glycolysis
What is the global prevalence of G6PD deficiency?
G6PD deficiency is inherited and affects 400 million people worldwide.
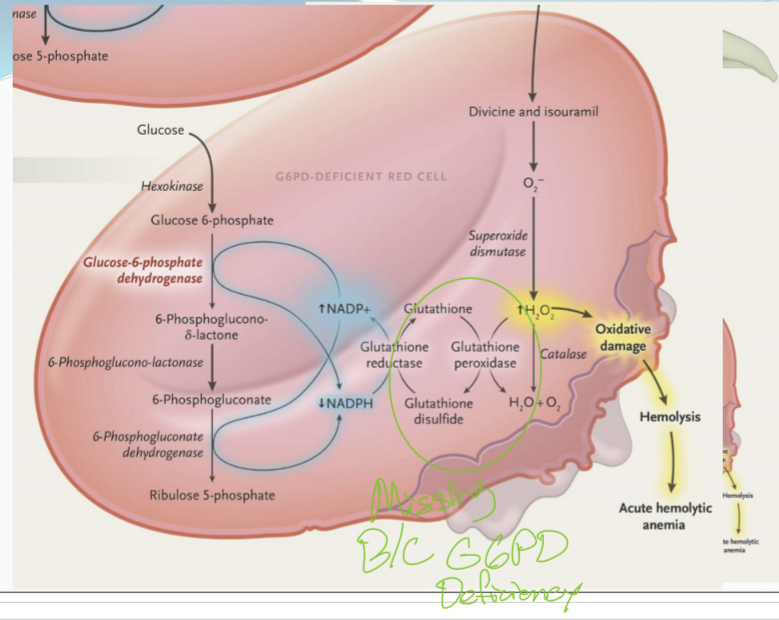
What are the risk factors associated with G6PD deficiency?
G6PD deficiency is a risk factor for pterygium and cataracts.
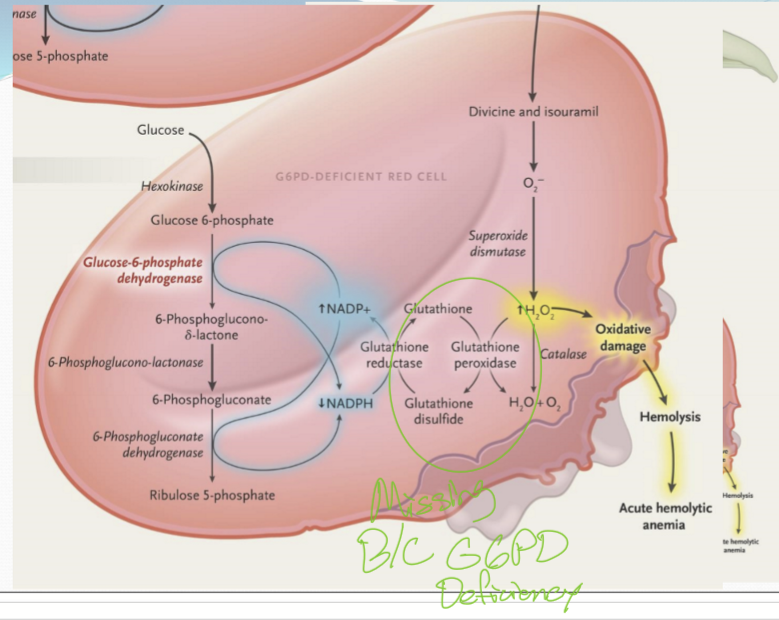
What is favism?
A condition where people with G6PD deficiency develop hemolytic anemia after consuming fava beans or being exposed to to other oxidative stressors. The fava beans contain compounds that are oxidants and the individuals with G6PD deficiency are unable to mitigate the oxidative damage to RBC, causing them to break down, leading to anemia
What affects the rate of pyruvate being converted to lactate?
The rate increases with hypoxia.
What catalyzes the reaction between pyruvate and lactate?
Lactate dehydrogenase
What is the distribution of lactate through out the cornea?
It is higher towards the epithelium, and decreases towards the endothelium.
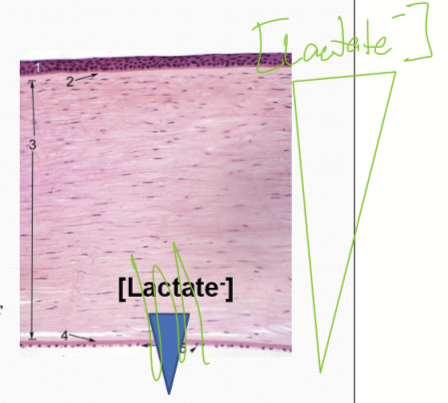
Which direction does lactate move/ is transported?
Only posteriorly as the lactate cannot pass the epithelial barrier into the tear film.
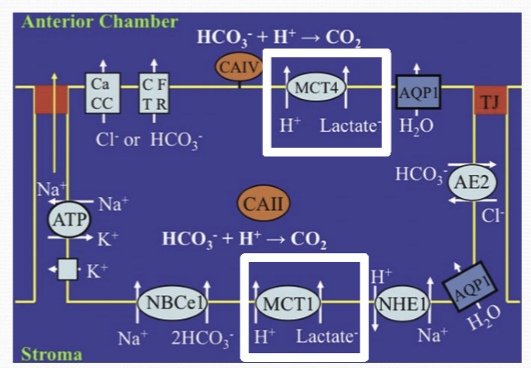
What facilitates lactate transport?
Monocarboxylate cotransporters (MCTs)
How do MCT move lactate (and protons)?
Trancellularly into the aqueous humor; with basolateral transporters moving lactate into the endothelial cells, and apical transporters moving lactate into AH.
In the posterior stroma, what GAG is favored to be produced?
Keratan production, due to: shift toward NAD+ in NADH: NAD+ ratio, from anaerobic metabolism, less O2, and more lactate production.
What inhibits the enzyme required for Dermatan?
NAD+
In the anterior stroma, what GAG is favored to be produced?
Dermatain production is favored due to: more O2, more aerobic metabolsim, reduced lactate production, and shift toward NADH in NADH:NAD+ ratio
How is the concentration of CO2 distributed through the cornea?
Larger pCO2 in AH than pCO2 of tears
What happens if there is an increase in CO2?
The pH will lower and an increase in HCO3- concentration
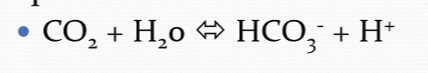
Increasing anaerobic metabolism will do what to the pH?
It will decrease it.
____ CO2 is expelled than O2 is absorbed
More
What is glycogen?
Polymerized (branched) glucose residues
When is glycogen produced in the corneal epithelium?
When excess glucose is present, it is stored as glycogen in cytoplasmic granules for future energy use.
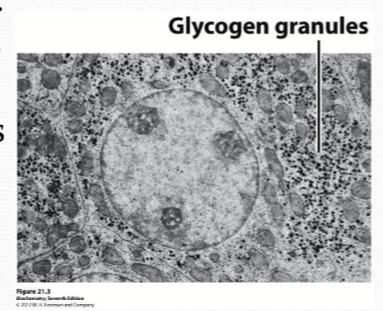
When energy is needed, what happens to glycogen?
It is converted to Glucose-6-phosphate and is used in glycolysis to produce ATP.
How does diabetes affect glycogen generation in the corneal epithelium?
Glycogen generation increases in diabetic patients due to excess glucose availability.