HF, Cardiogenic shock, cardiac arrest, pericardial effusion, pulmonary edema with HF
1/35
Earn XP
Description and Tags
the other dieases chapter 14
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
Patients with complications of heart diease
heart diease is a chronic condition
HF is always will last for long
Cardiopulmonary resuscitation
Pulmonary edema
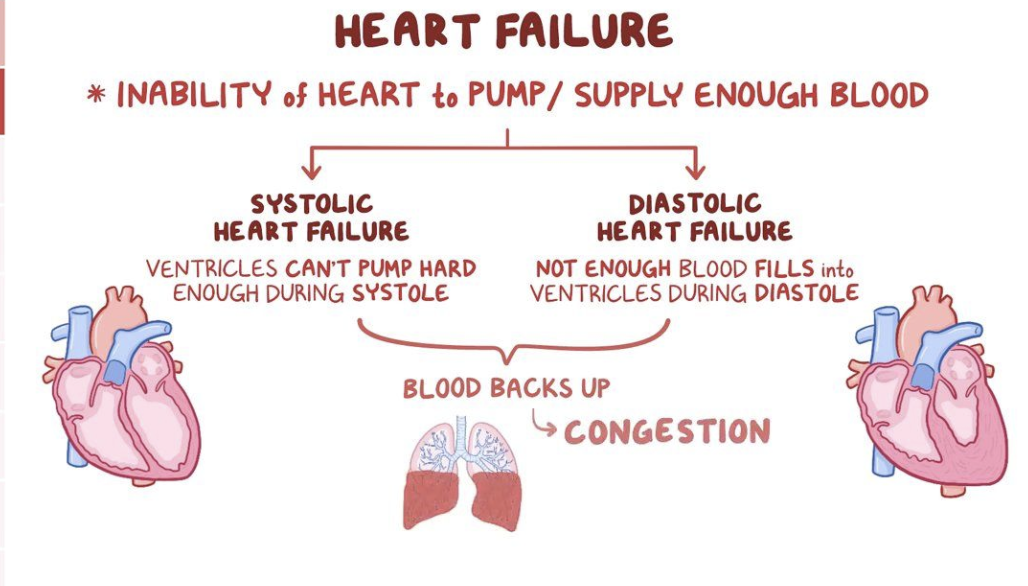
What is heart failure?
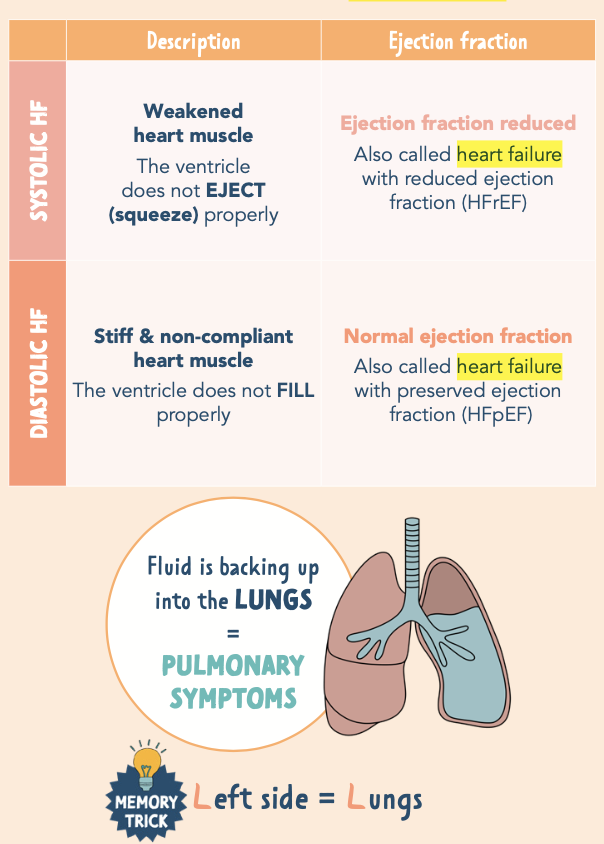
Heart failure sys vs dis
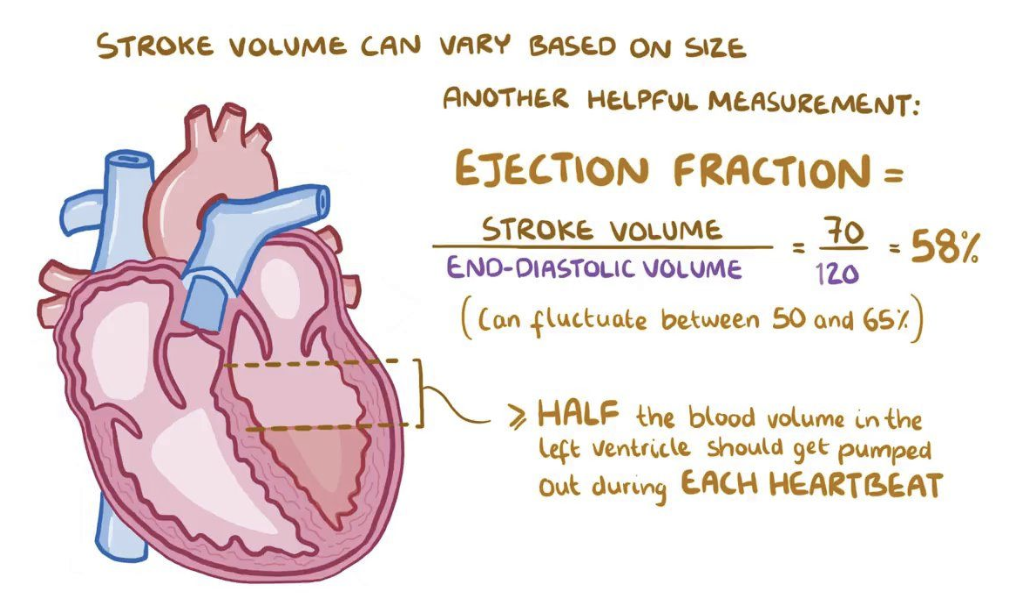
what is Ejection fraction
Recognized as a clinical syndrome characterized by signs and symptoms of fluid overload or of inadequate tissue perfusion → caused when heart cannot generate a cardiac output sufficient to meet the body’s demands
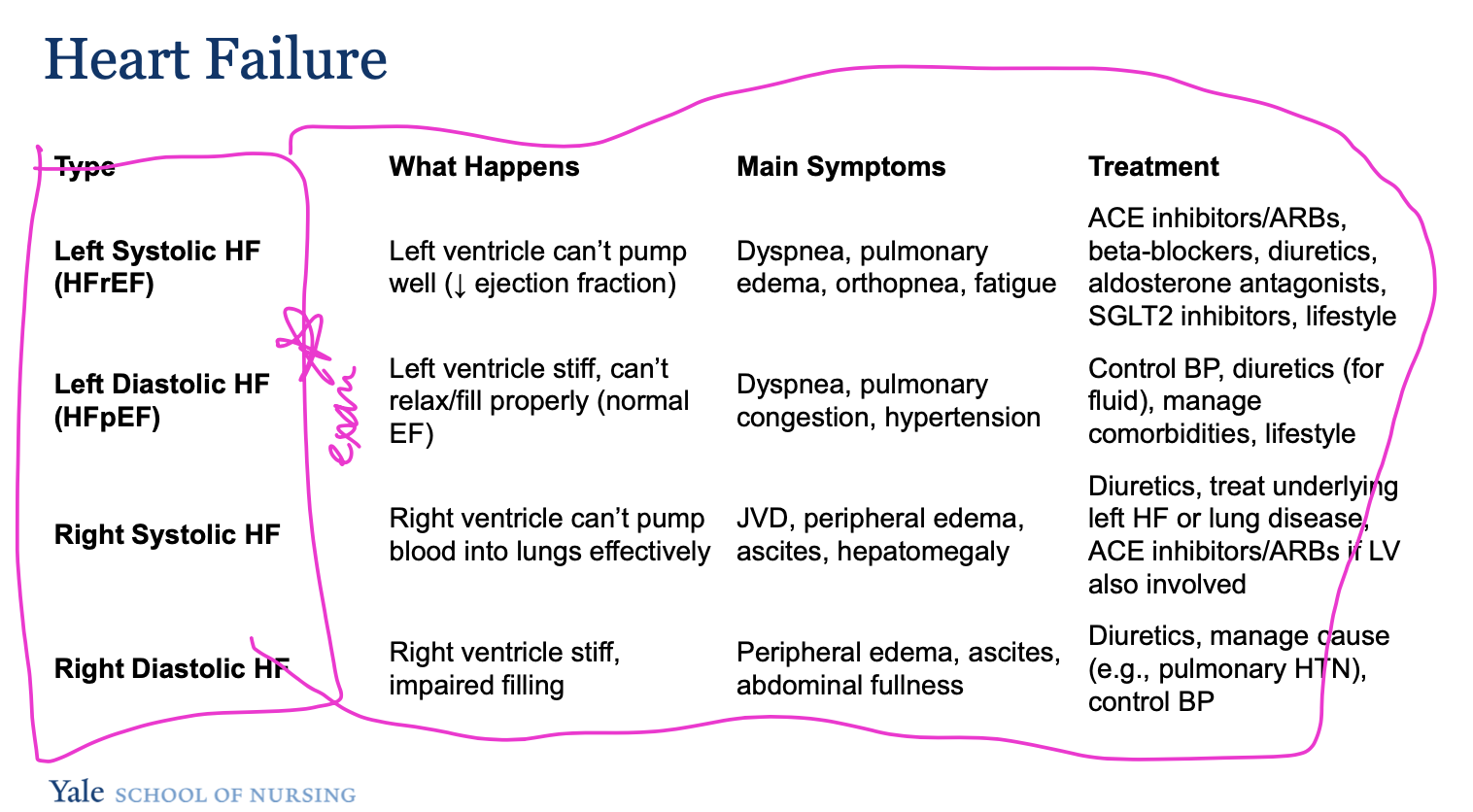
systolic failure - heart is not a sufficient pump - weakened heart muscle (HFrEF) <40%
diastolic failure - heart is not getting blood back efficiently - stiff not complient heart muscles (HFpEF)>50%
Normal ejection fraction: 50-70% total amount of blood pumped with each heartbeat
HF with Mildly Reduced EF (41–49%)
HF with Improved EF – baseline EF ≤40%, improved >40% by ≥10%.
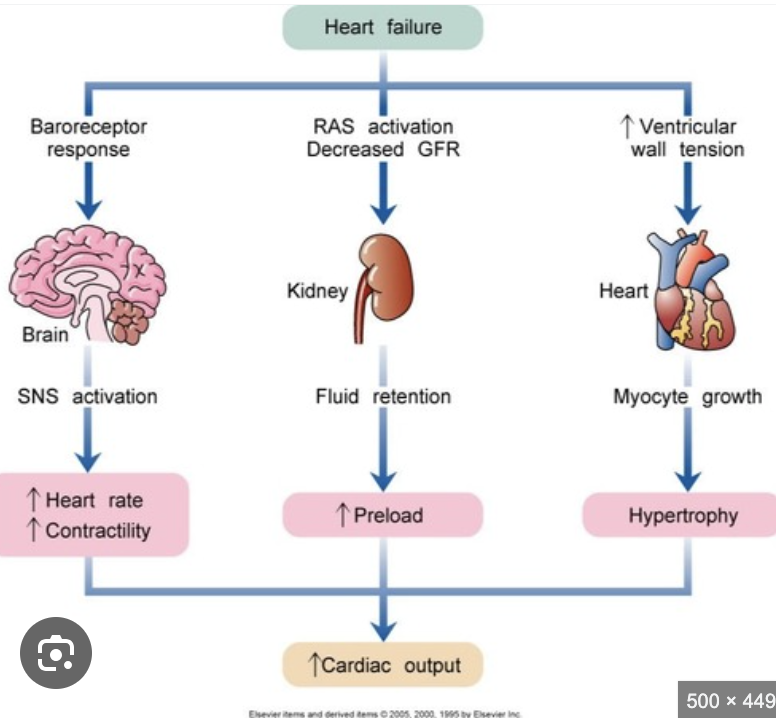
Compensatory mechanisms tend to ultimately exacerbate the sign and symptoms of HF
Risk factors of heart failure
Age, sex, hypertension, left ventricular hypertrophy, MI, Valvular heart dieases and obesity
Modifiable: Hypertension (primary cause in females), diabetes, cardiometabolic syndrome, CAD.
Cardiometabolic Syndrome: Presence of ≥3: abdominal obesity, high triglycerides, low HDL, HTN, high fasting glucose
Prevention: Early management of risk factors can reduce HF onset.
Lifestyle risks: alcohol, smoking, diabetes, sleep disorder, breathing, CKD, low socioeconomic status, psyco stress, sedentary lifestyle, and genetics
Classic manifestations of heart failure
Dyspnea, cyanosis, cachexia, tachycardia, S3 heart sounds, crackles, edema, dizziness or lightheadedness, elevation in JVD
What are the key diagnostic tests and findings for heart failure?
Imaging:
Chest X-ray → cardiomegaly, pulmonary congestion
ECG → arrhythmias, LVH, prior MI
Echocardiogram (2D/3D + strain) → structure, valves, EF, early dysfunction
Cardiac MRI → gold standard for function & prognosis
Labs:
CBC, electrolytes, renal/liver function, urinalysis, TSH
BNP ↑ → ventricular stretch → vasodilation → volume overload
Right/Left heart catheterization → pressures, EF, coronary arteries → guides diagnosis & therapy
Patho of Heart Failure
Low CO
Compensatory Mechanisms:
Sympathetic activation → ↑ heart rate, vasoconstriction.
RAAS activation → angiotensin II → ↑ blood pressure & afterload; aldosterone → sodium/water retention → fluid overload.
Natriuretic peptides (ANP, BNP) attempt to counteract volume overload but are often insufficient.
Structural Changes:
Ventricular dilation → increased wall stress → hypertrophy → ventricular remodeling → further dysfunction.
HFpEF: Stiff ventricle → impaired filling → low CO.
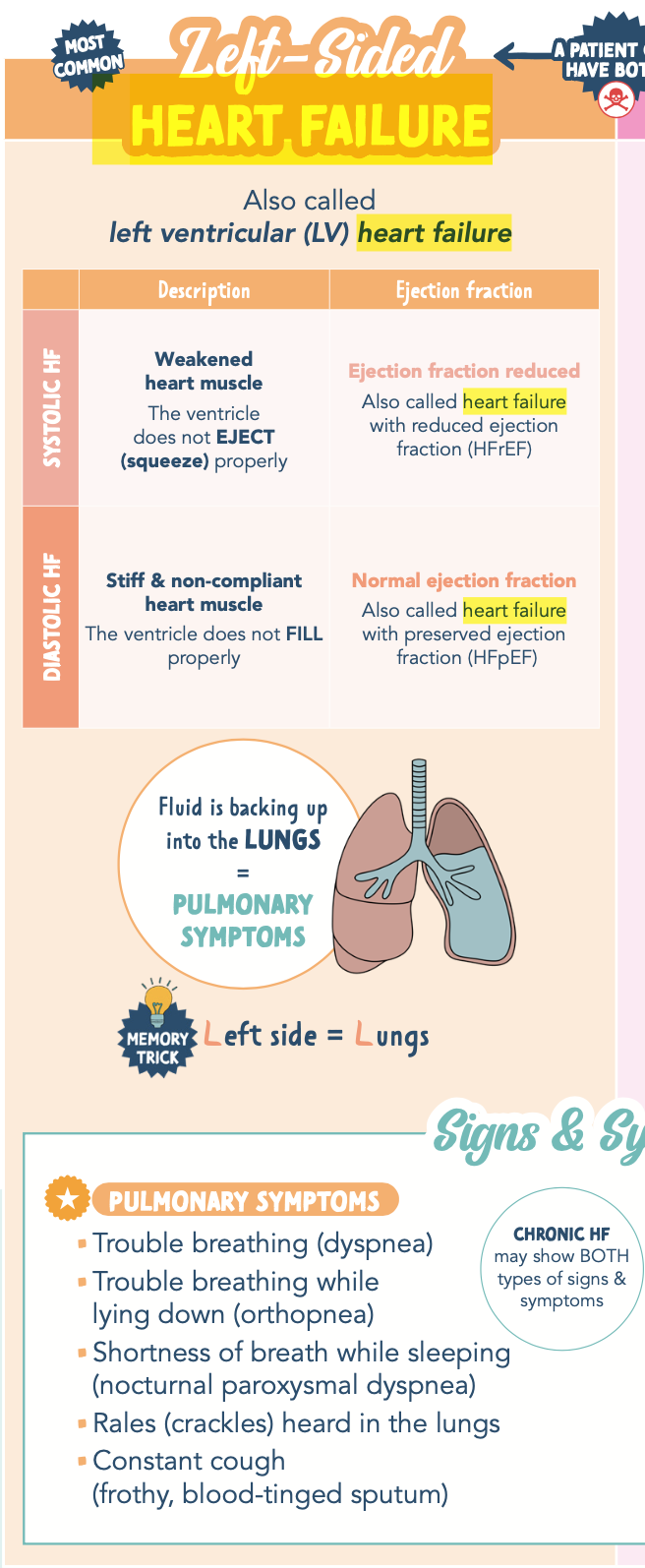
LEFT SIDED HEART FAILURE
Most common type of HF
Caused by left ventricular dysfunction (heart attack, hypertension, CAD)
When the left ventricle fails, blood backs up into the left atrium and the lungs, pulmonary veins(the blood vessels that carry blood away from the lungs) → leads to pulmonary congestion and edema (SOB)
trouble breathing or coughing – especially during physical activity
Pulmonary edema impairs gas exchange in the alveoli → increase in CO2 and decrease in O2 can lead to respiratory distress
SIGNS AND SYMTOMS OF LEFT SIDED HEART FAILURE
pulmonary edema/crackles, S3 heart sound, fatigue, weak pulses, decreased organ perfusion.
Dyspnea, orthopnea, PND
Paroxysmal nocturnal dyspnea (PND) is a sensation of shortness of breath that awakens The patient, often after 1 or 2 hours of sleep, is usually relieved in the upright position
Cough, Pulmonary crackles (rales), Decrease O2 saturation levels, S3 ventricular gallop, Oliguria if kidney perfusion is diminished, Decreased perfusion to other systemic organs (advanced failure):
Sluggish GI motility, Dizziness, lightheadedness, confusion, restlessness, Anxiety, Skin is cool and clammy, Decrease in EF (ejection fraction), Tachycardia and/or weak, thready pulse, Fatigue or activity intolerance
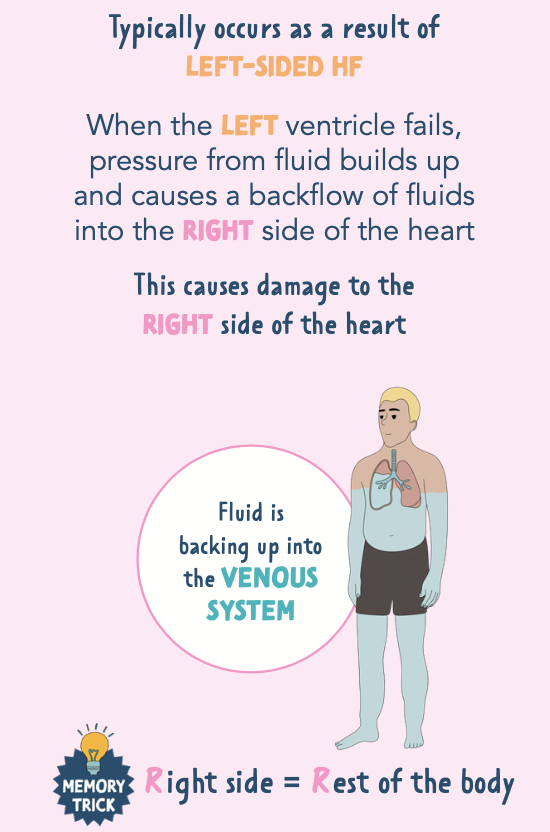
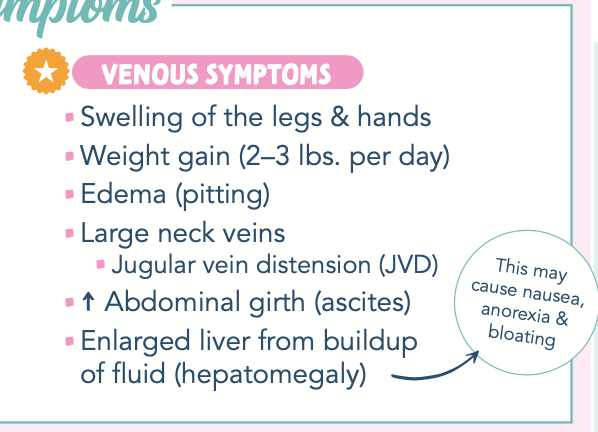
RIGHT-SIDED HEART FAILURE
Usually occurs secondary to left-sided heart failure, May also be caused by cor pulmonale (pulmonary heart) or right ventricular myocardial infarction
Cor pulmonale: when a lung issue causes your right ventricle (heart chamber) to get so big that your heart starts to fail
When the right ventricle fails, blood backs up into the right atrium and to the venous systemic circulation
Can lead to systemic congestion and peripheral edema/ascites
Increased pressure of blood back flow causes jugular vein distention, hepatomegaly, and splenomegaly
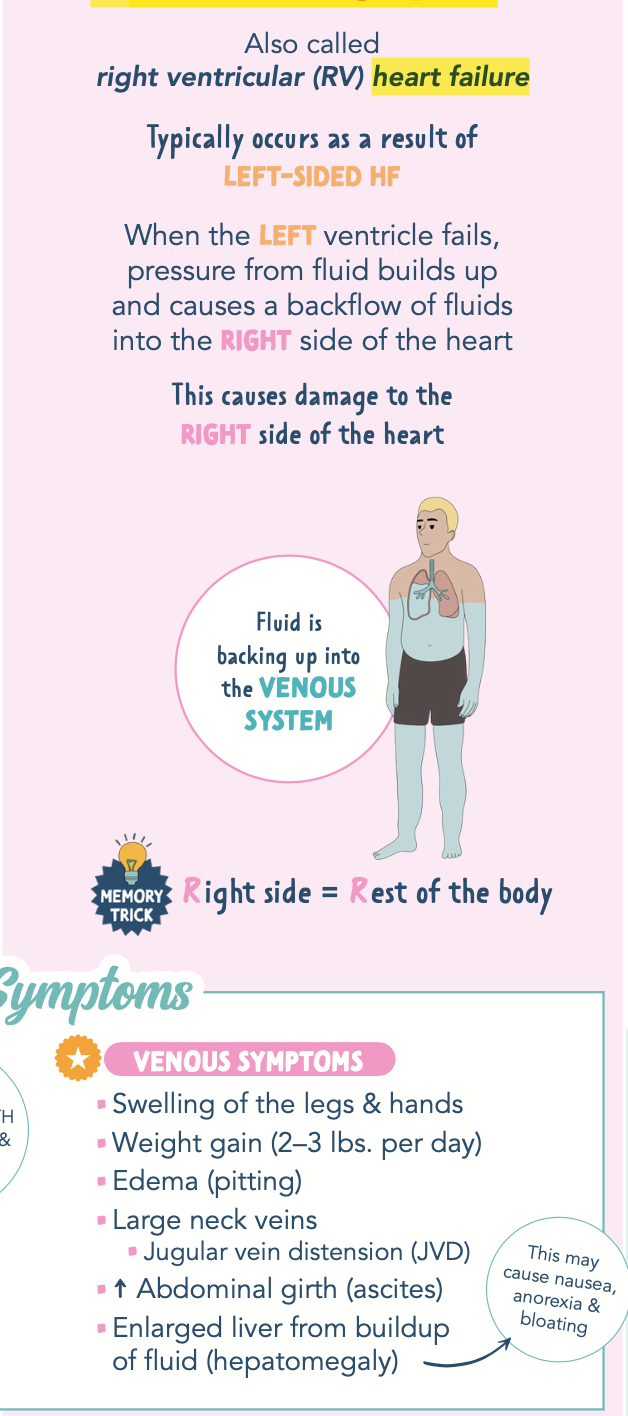
SIGNS AND SYMPTOMS OF RIGHT SIDED HEART FAILURE
Lower extremity dependent edema (follows the positioning of the body), Legs and feet, May progress to thighs, external genitalia, lower trunk, abdomen, and sacral edema (in bed-bound pt)
Pitting edema
Hepatomegaly (enlargement of liver)
Ascites (fluid buildup in peritoneal cavity)
Anorexia and nausea\
Weight gain due to retention of fluid
Weakness or fatigue from reduced CO (carbon monoxide)and impaired cognition
Decreased perfusion to other systemic organs (advance failure)
chest discomfort, breathlessness, palpitations, and body swelling
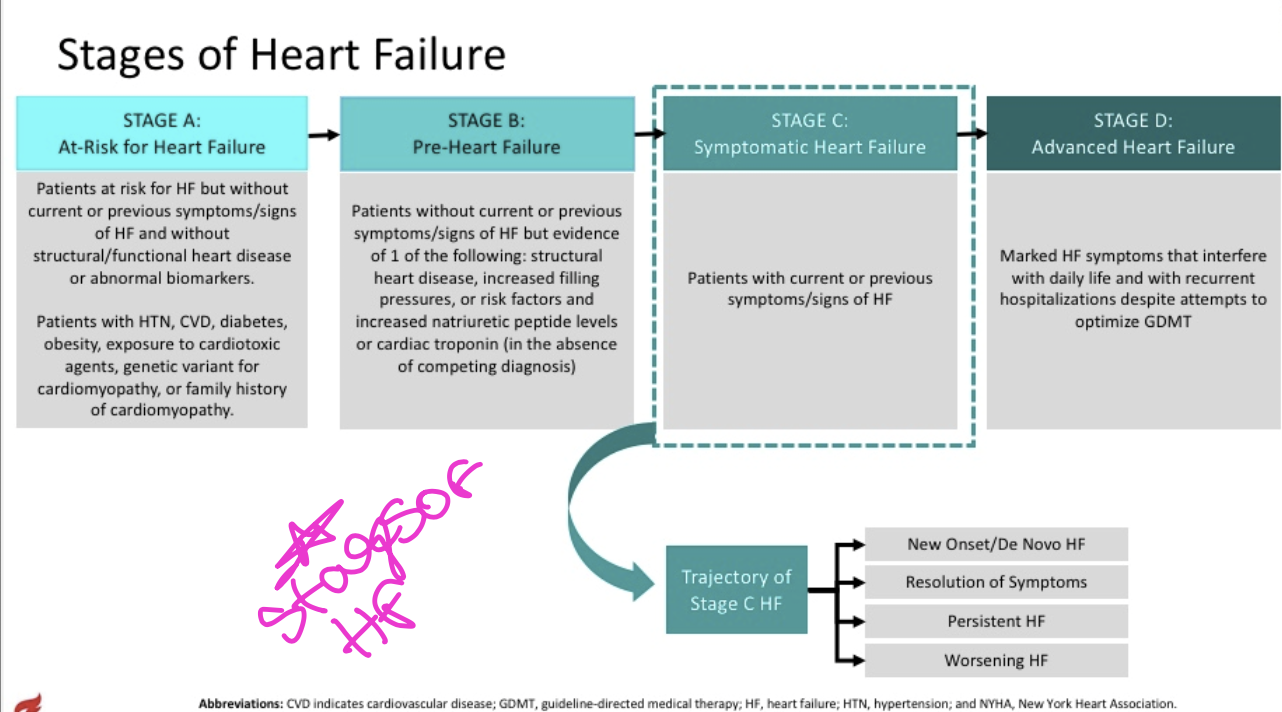
Classifications and stages of heart failure
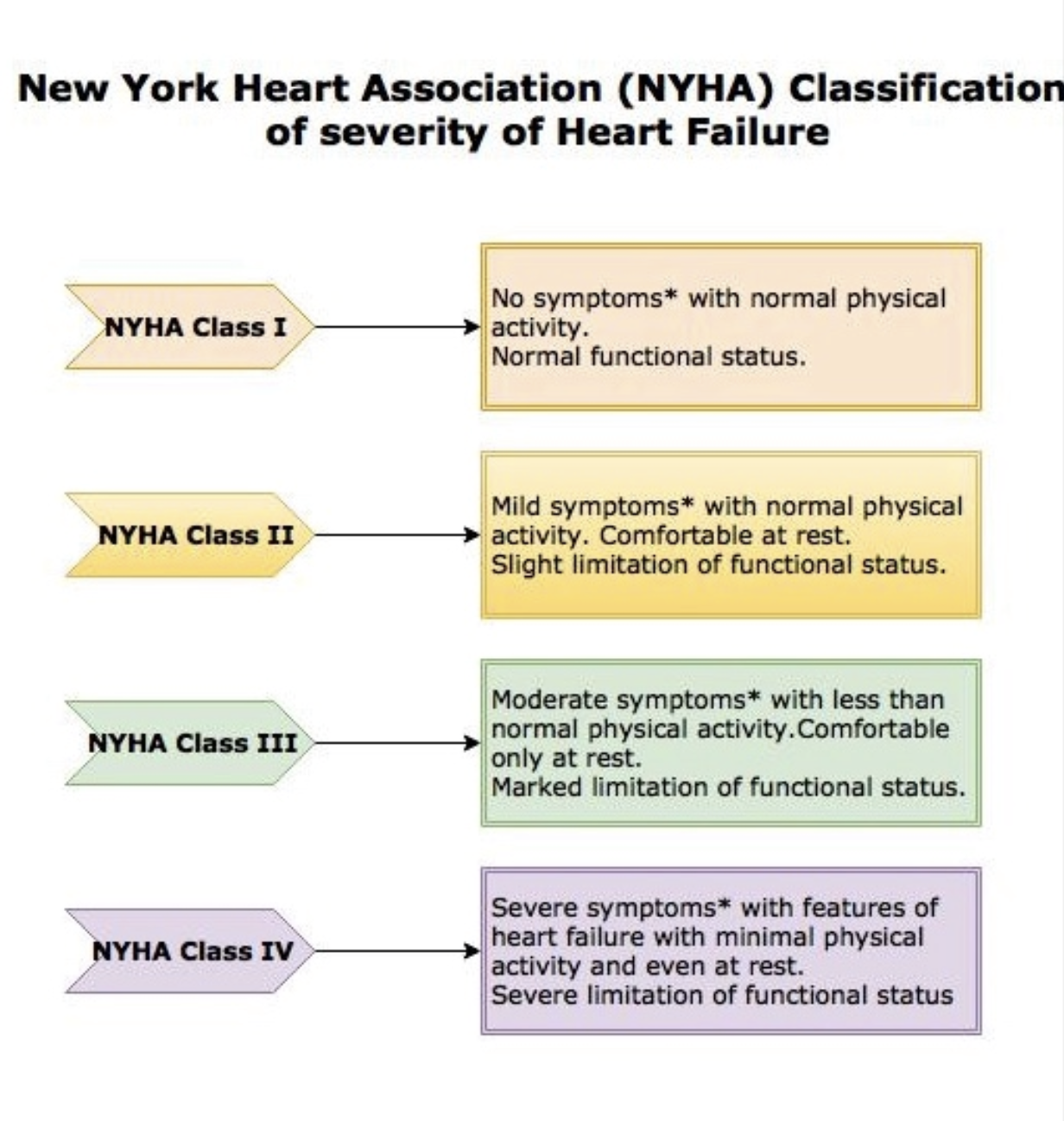
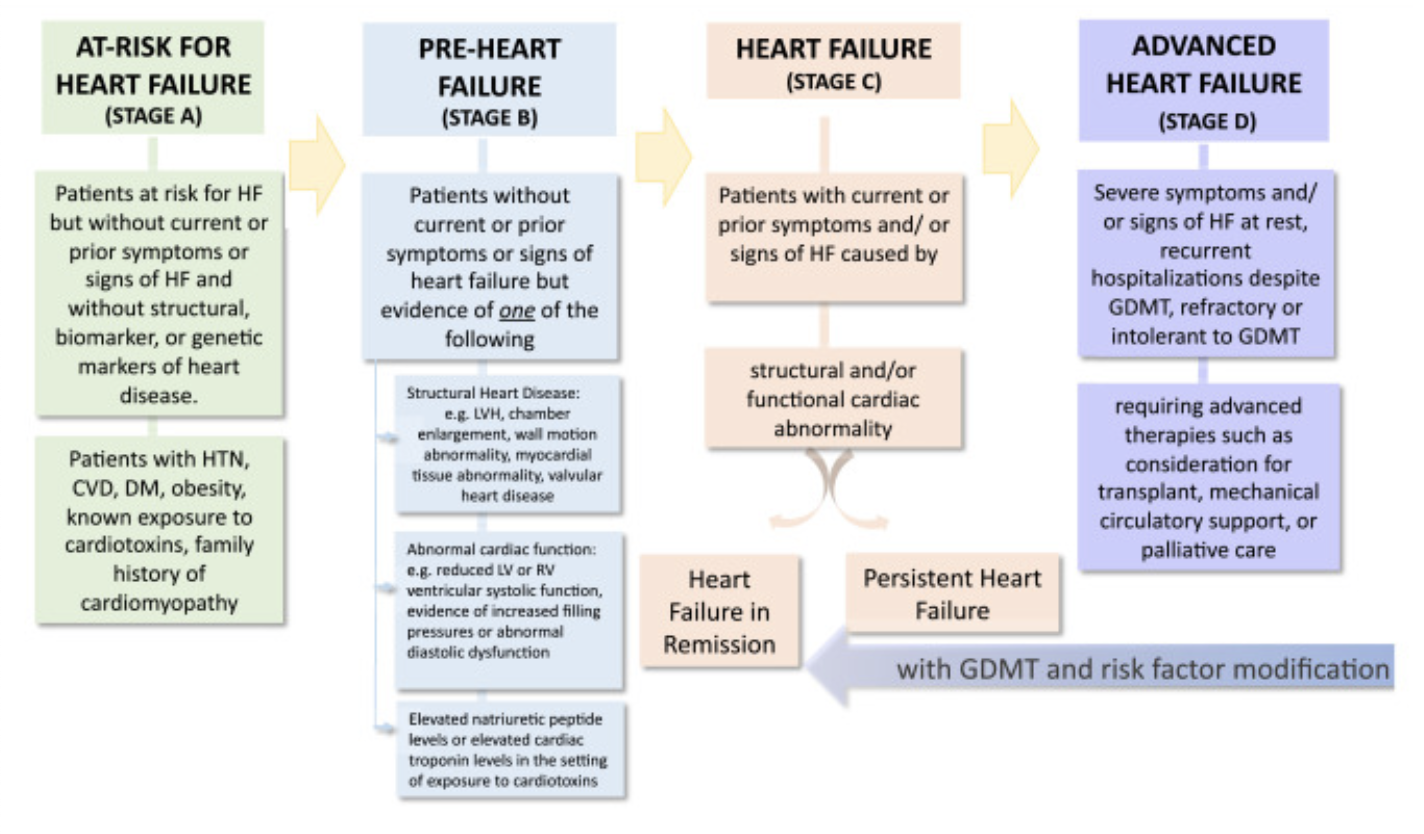
Classifications of heart failure
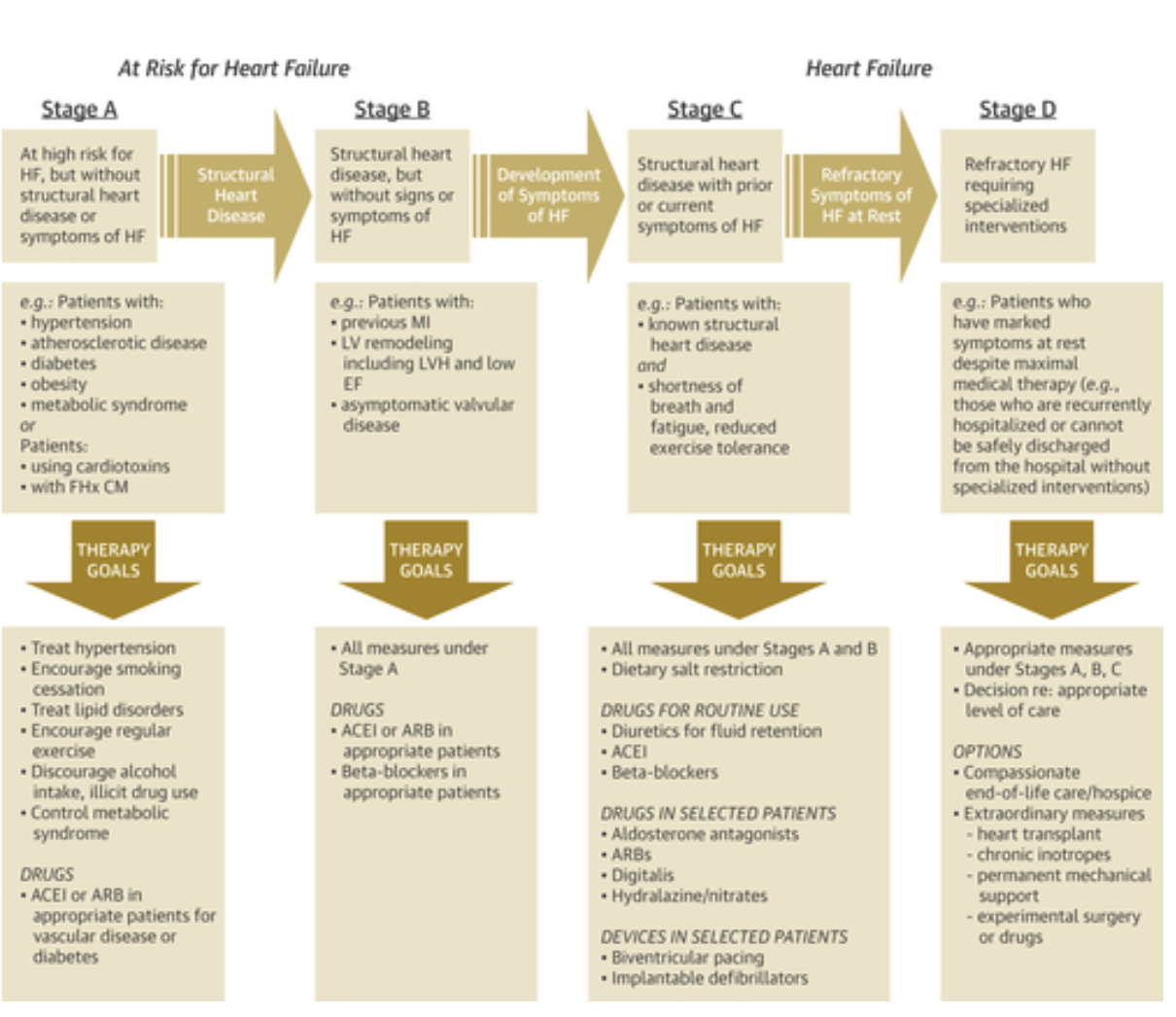
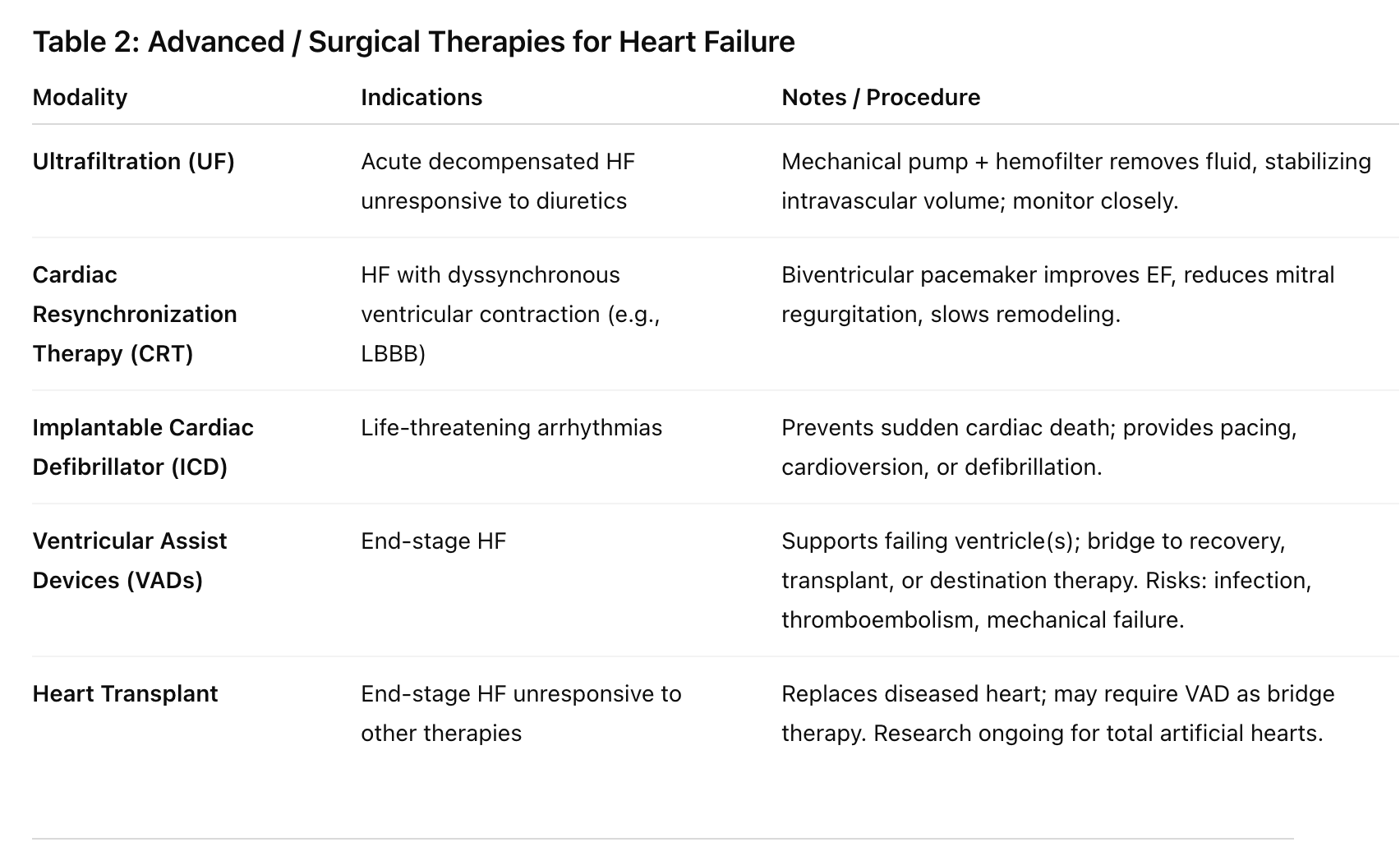
MANAGMENT OF HEART FAILURE
Relieve symptoms, improve quality of life, extend survival.
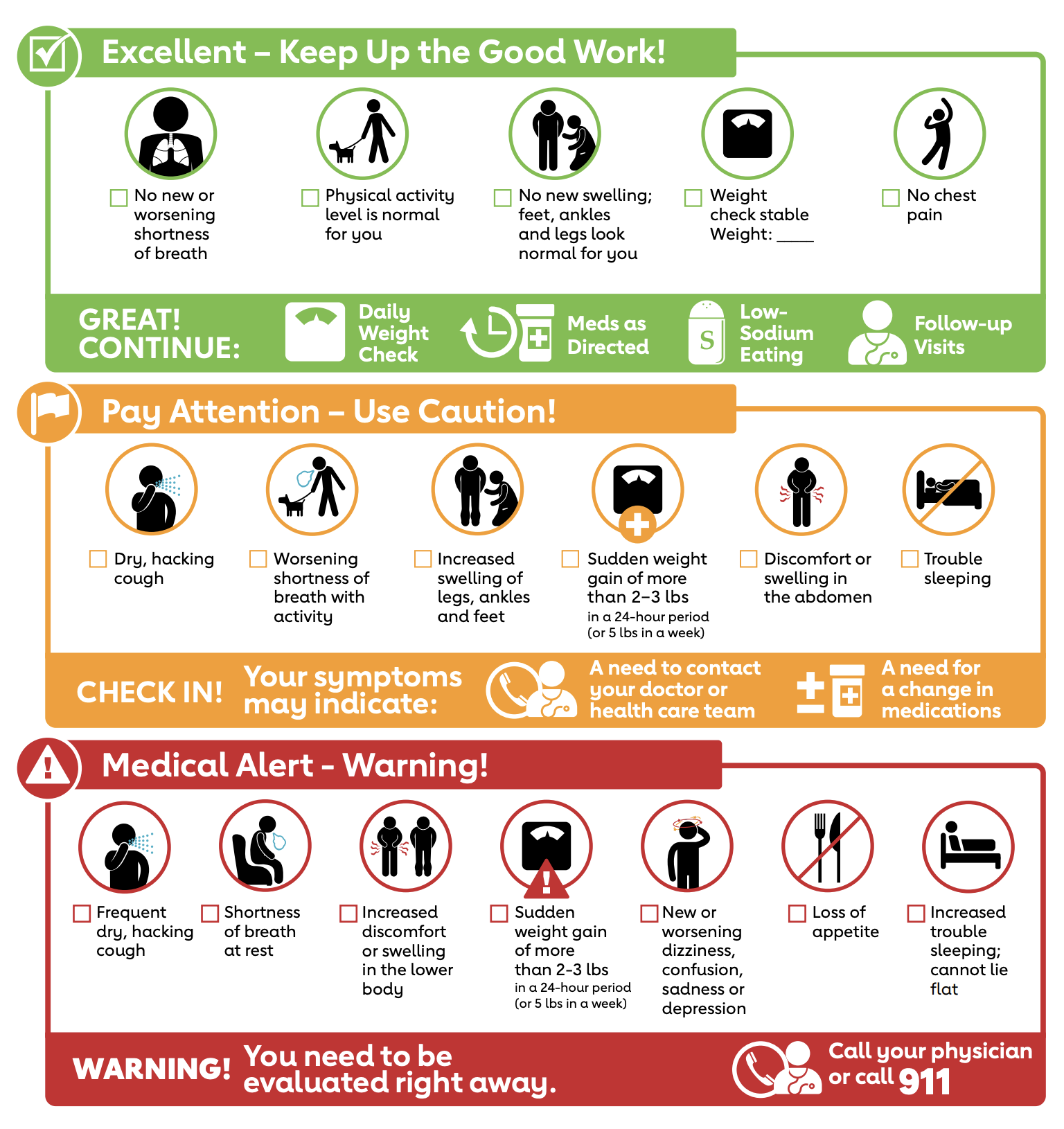
Lifestyle changes: Sodium restriction, fluid moderation, avoid alcohol & smoking, weight control, exercise, symptom monitoring.
Lower blood volume = lower BP
Rx - more common medications used:
ACEi (-pril) - lowers BP
Beta blockers (-olol) - lowers HR
Diuretics (ex: furosemide) - lower fluid retention
Digoxin
Nursing Managment
Nursing assessment prioritizes symptoms of pulmonary and systemic fluid overload, health history and monitoring of intake and output
Assessment: Monitor for fluid overload, weight changes, edema, orthopnea, bendopnea, fatigue, SOB, PND, and adherence to self-care.
I&O & Daily Weights: Track fluid balance; positive fluid balance correlates with weight gain. Notify provider for ≥2–3 lb/day or ≥5 lb/week weight increase.
Patient Education:
Teach HF disease process and self-management.
Reinforce education during hospital stay and at discharge.
Use teach-back, mobile apps, family involvement, and follow-up calls.
Monitor adherence, knowledge, and learning preferences.
Psychosocial Support: Address emotional response, coping strategies, and quality-of-life impact.
Safety: Monitor electrolytes, renal function, and hemodynamic status with medications or devices.
Pharmacologic Therapy for Heart Failure
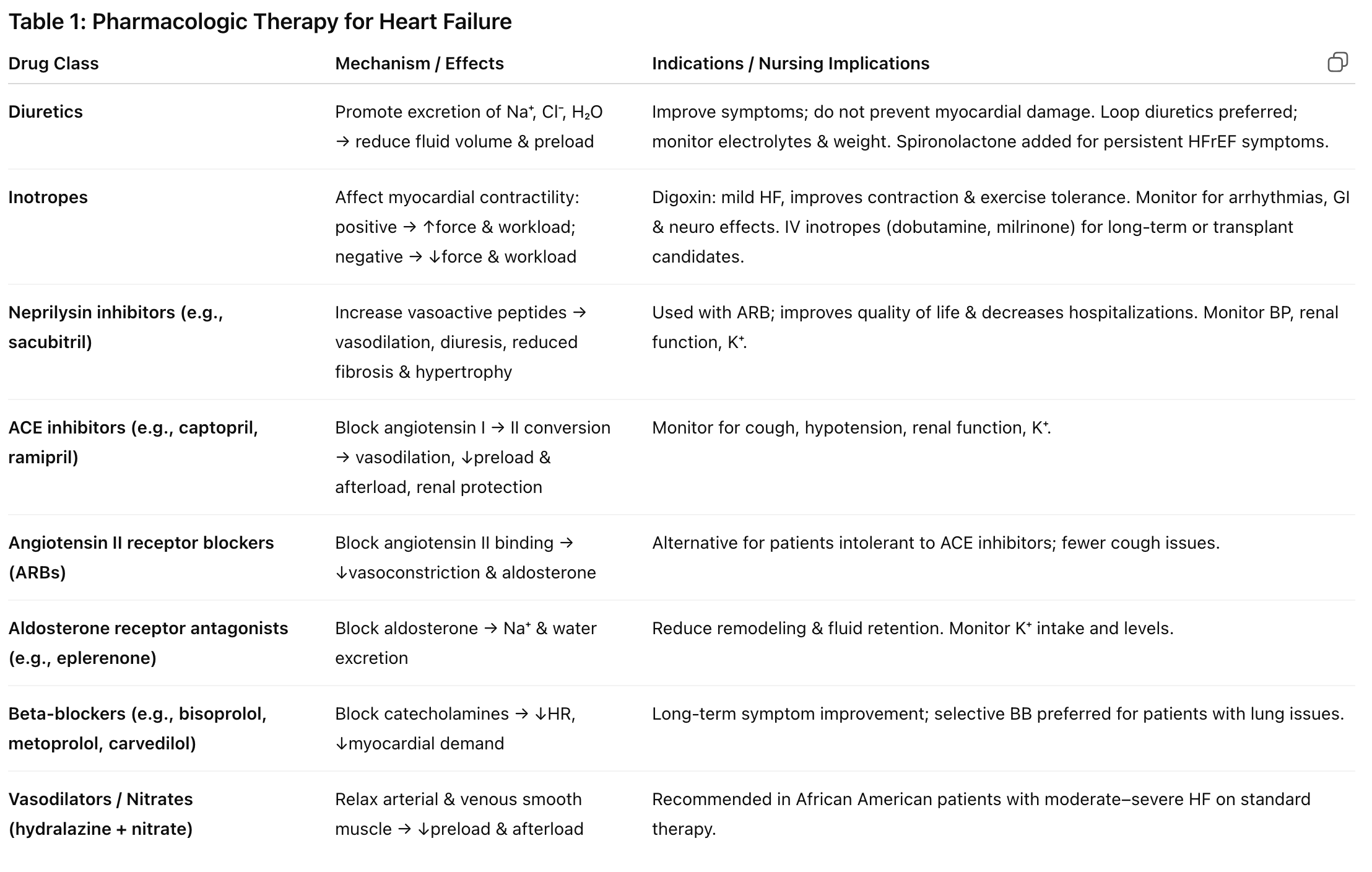
Advanced / Surgical Therapies for Heart Failure
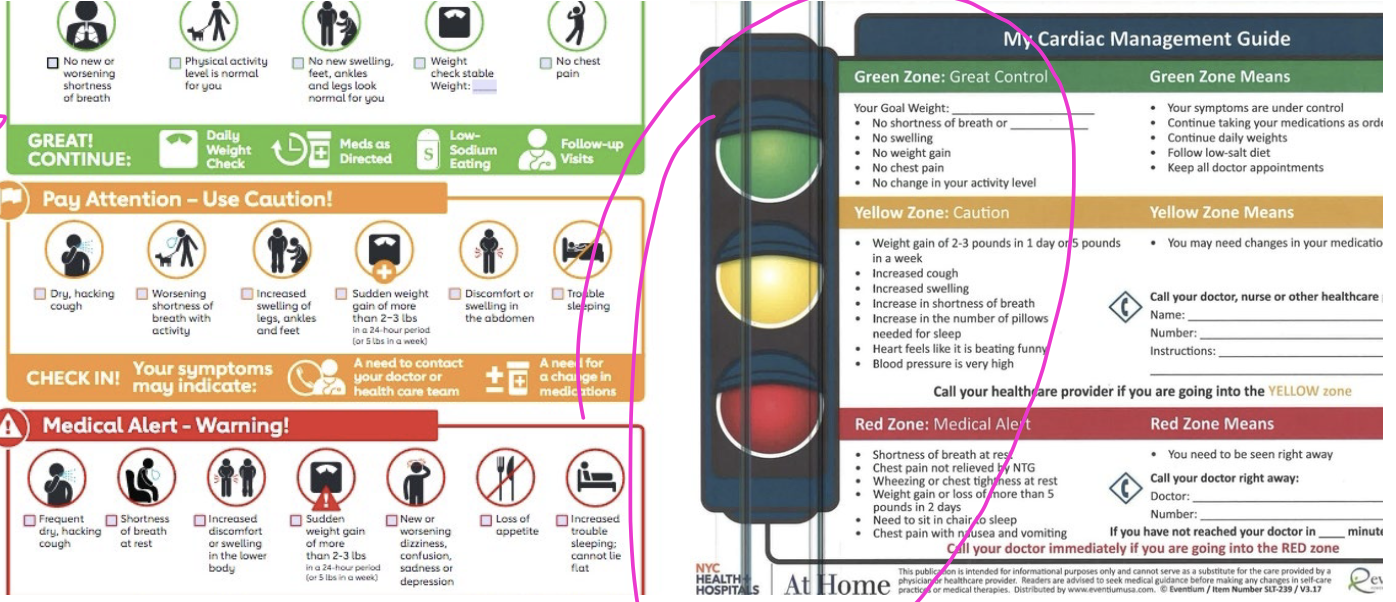
Important patient education for coming into hospital for heart failure
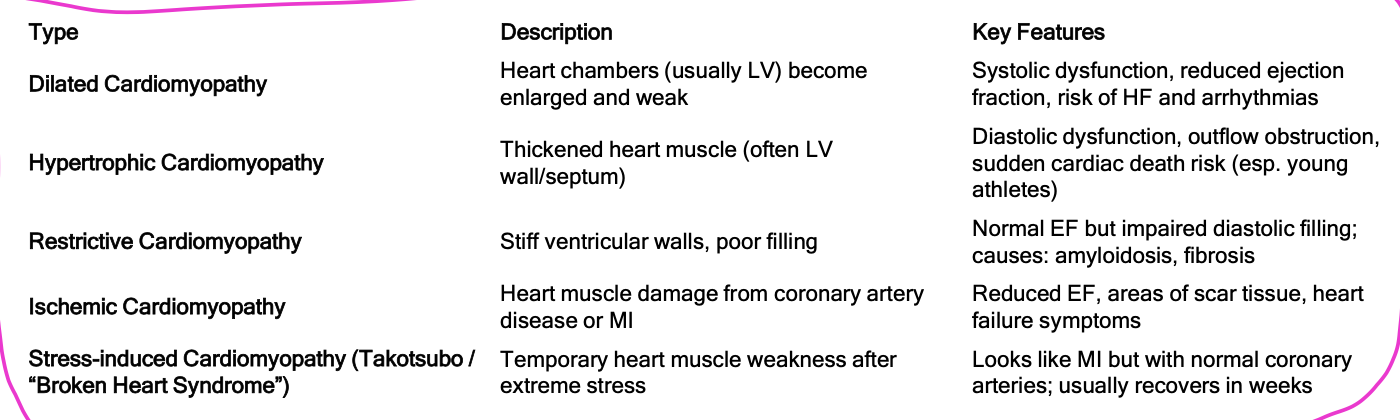
Cardiomyopathy
Disease of heart muscle that makes it harder for the heart to pump blood to rest of the body → either mechanical and/or electrical dysfunction
Results in impaired cardiac output
Normal muscle in the heart can thicken, stiffen, thin out, or fill with substances body produces that don’t belong in the heart muscle
Can lead to heart failure
Stress-induced cardiomyopathy “broken heart syndrome”
Cardiomyopathy different types
Dilated cardiomyopathy: Most common; dilation of all chambers, ↓ contractility.
Hypertrophic cardiomyopathy: Hypertrophied, nondilated LV → may obstruct LV outflow.
Restrictive cardiomyopathy: Diastolic dysfunction with impaired ventricular filling during diastole.
Ischemic cardiomyopathy: Due to coronary artery disease or prior MI.
Arrhythmogenic right ventricular cardiomyopathy (ARVC): Inherited (autosomal dominant); fatty/fibrous replacement of RV → arrhythmias.
Stress-induced (Takotsubo) cardiomyopathy: “Broken heart syndrome” → acute, reversible LV dysfunction triggered by severe emotional or physical stress.
Medical Managemnt of cardiomyopathy
Echocardiogram to evaluate the structure/function of the ventricles and ejection fraction
Medications: ACEi, aldosterone antagonists, diuretics, beta blockers, and CCBs
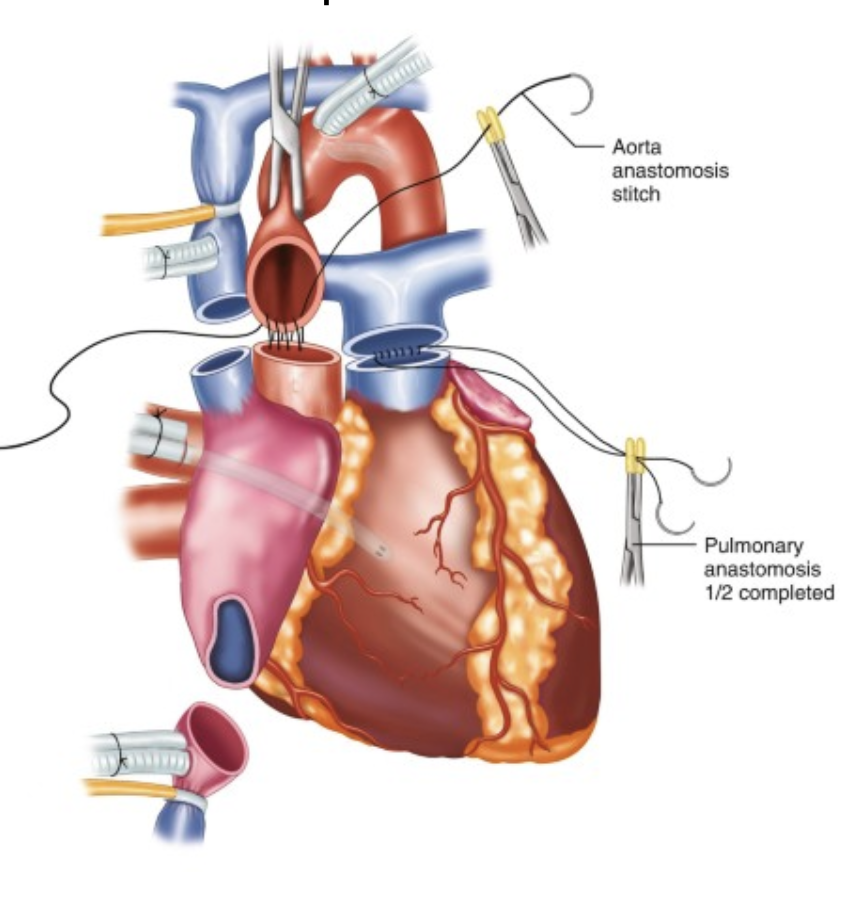
Surgical interventions: cardiac transplantation
Ventricular assist devices:
Bridge to transplantation
Sustain life until donor heart becomes available- Destination therapy in patients with end-stage heart failure who are ineligible for transplant and for whom ventricular recovery is not possible
Orthotopic heart transplantation: most common surgical procedure
Nursing managmet of Cariomyopathy
Assessment for signs of worsening heart failure, dyspnea, congested lungs, peripheral edema, and the presence of abnormal lung sounds
Heart Transplantation - Postop Care:
Balancing risk of rejection with the risk of infection
Assess for complications including cardiac allograft vasculopathy and atherosclerosis of the coronary arteries
Address the many stressors faced by the patient
Acute Heart Failure and Pulmonary Edema
Pulmonary edema: Abnormal fluid accumulation in the lungs, occurring in the interstitial spaces and alveoli.
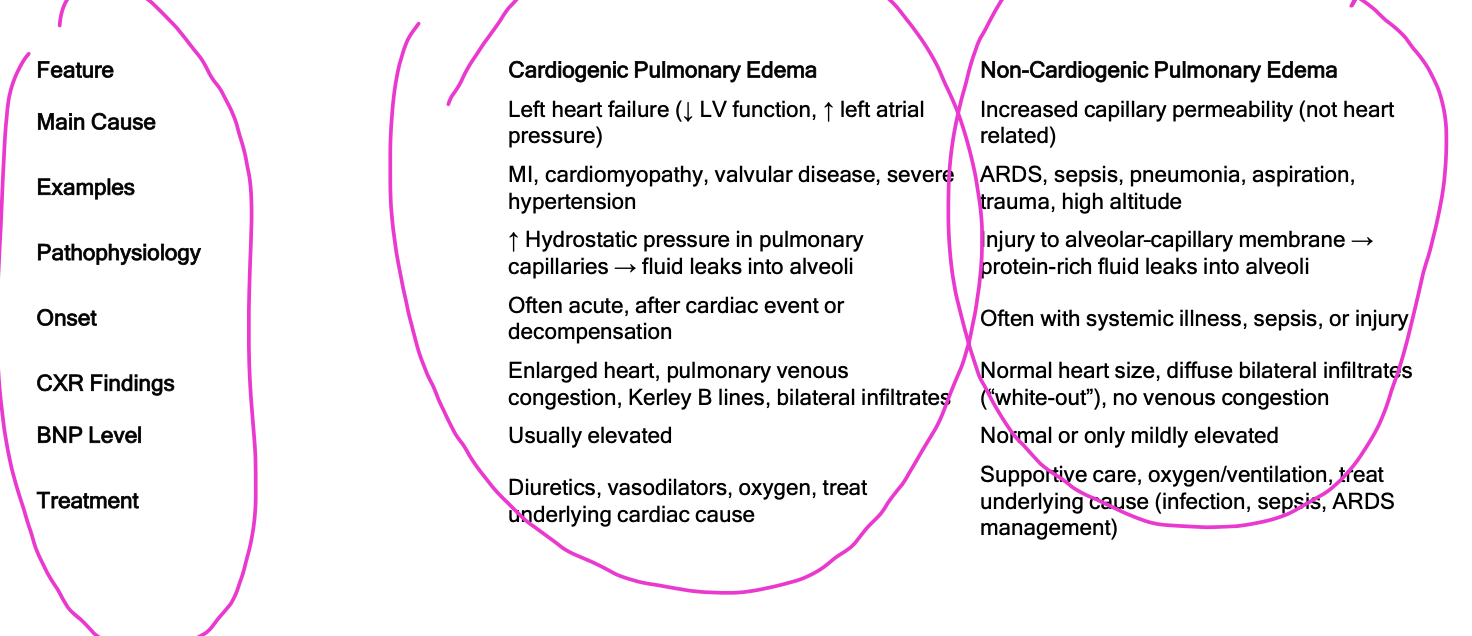
Two main types:
Cardiogenic: Caused by heart dysfunction (e.g., acute MI, HF exacerbation).
Non-cardiogenic: Caused by other conditions (e.g., kidney failure, liver failure, oncologic fluid retention).
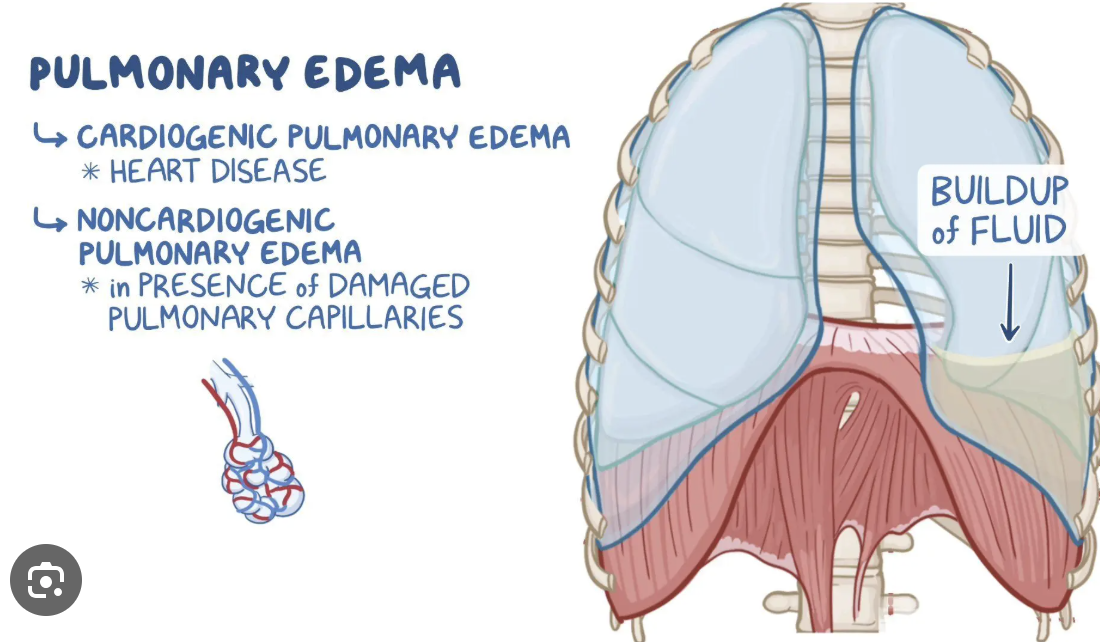
PULMONARY EDEMA- patho, onset, main-cause, treatment
Pulmonary edema and acute HF signs and symtoms
What are risk factors of pulmonary edema?
How do you manage pulmonary edema?
Decreased cerebral oxygenation = restless and anxious, Sudden onset of breathlessness, cough, sense of suffocation, Cold and moist skin, Cyantic, Crackles, Expiratory wheezing, Distended neck veins
Kindey failure and liver failure increasedn the risk of pulmonary edema
Manegment: O2, Diuretics, Pharmacological (similar to HF), Bronchodilator therapy
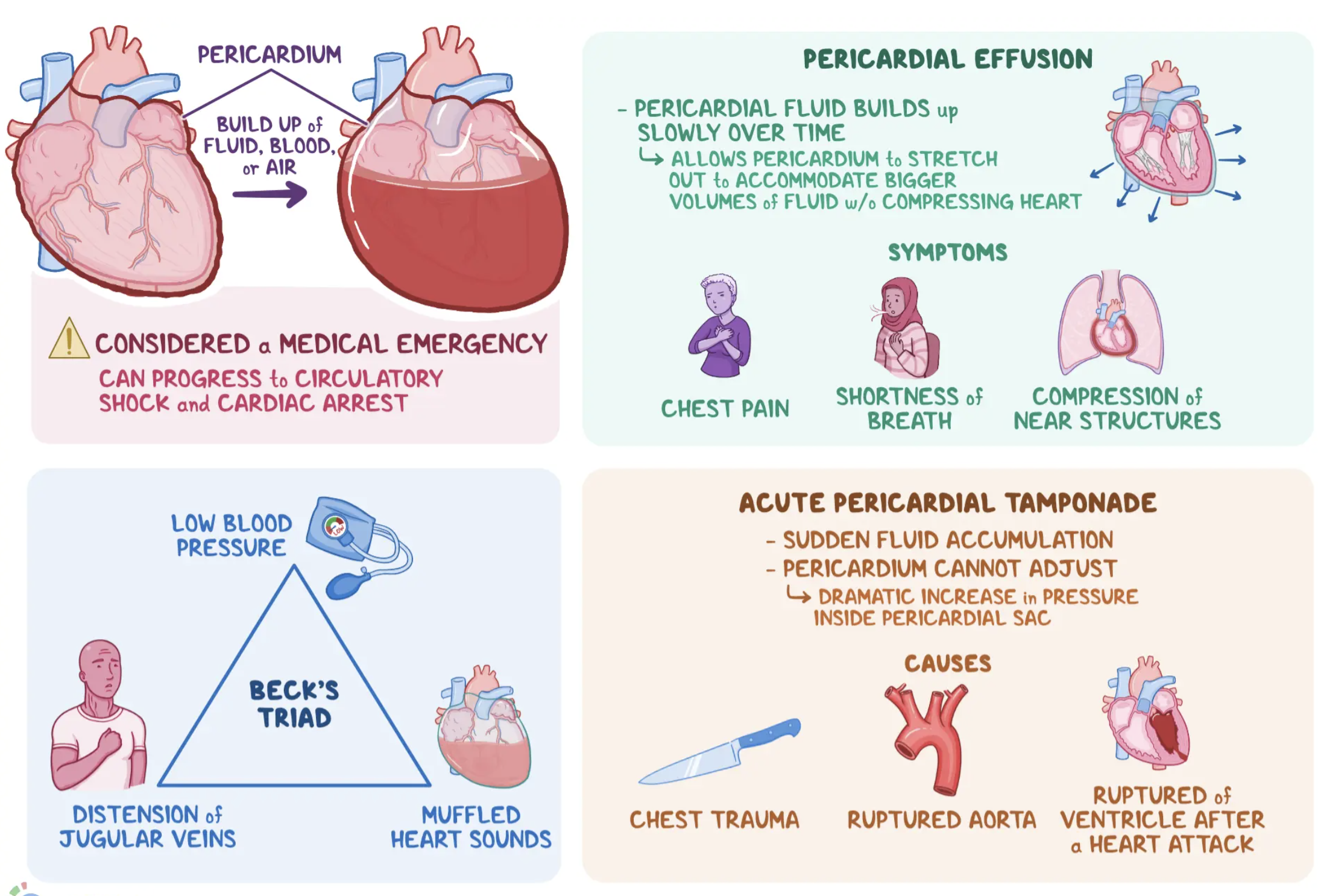
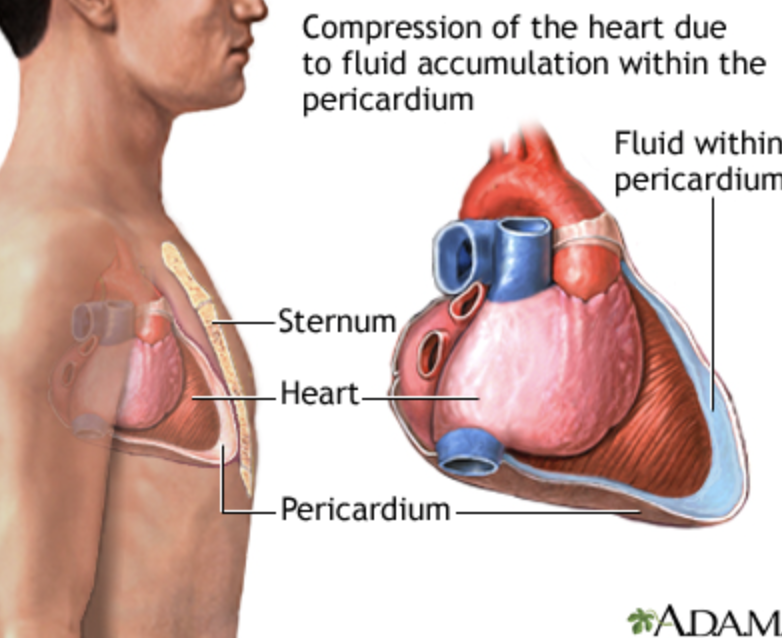
Pericardial Effusion and Cardiac Tamponade
Pericardial effusion: Fluid accumulation in the pericardial sac (normally <50 mL).
Cardiac tamponade: Life-threatening compression of the heart due to rapid or excessive effusion → decreased cardiac output (CO).
Accumulation of fluid in the pericardial sac
Increase pericardial fluid raises pressure in the sac and comprises the heart
Leads to decreased venous return
Inability of ventricles to distend and fill adequately
Increased right and left ventricular end-diastolic pressure
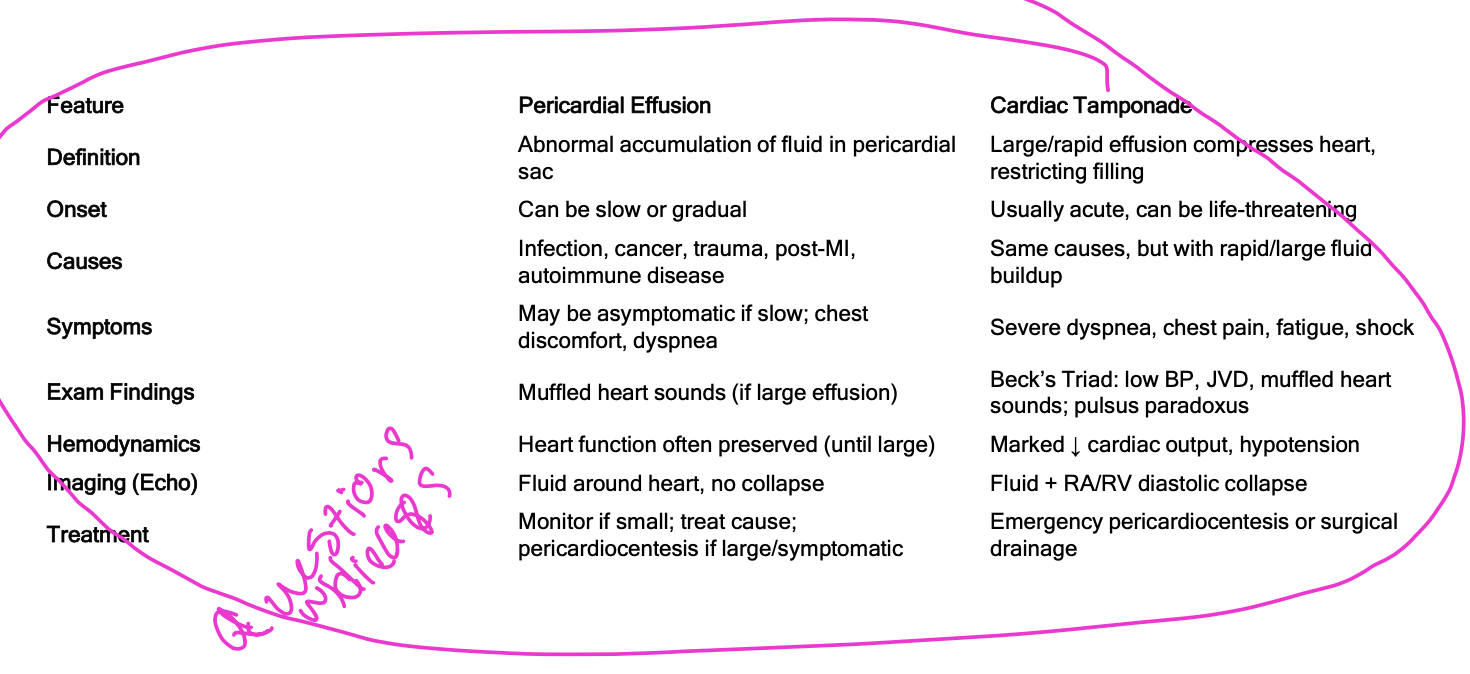
The differences between cardiac effusion and tamponade
What are the causes of pericardial effusion and cardiac tamponade
What is the patho of “……”?
Pericarditis, Advanced HF, Metastatic cancer, Chemotherapy, Cardiac surgery, Trauma
PATHO:
↑ Fluid in pericardial sac → ↑ pericardial pressure → ↑ RVEDP & LVEDP → ↓ venous return.
Ventricles can’t fill properly → ↓ stroke volume & cardiac output.
Rapid fluid accumulation stretches the pericardium → compresses the heart → tamponade (hemodynamic collapse).
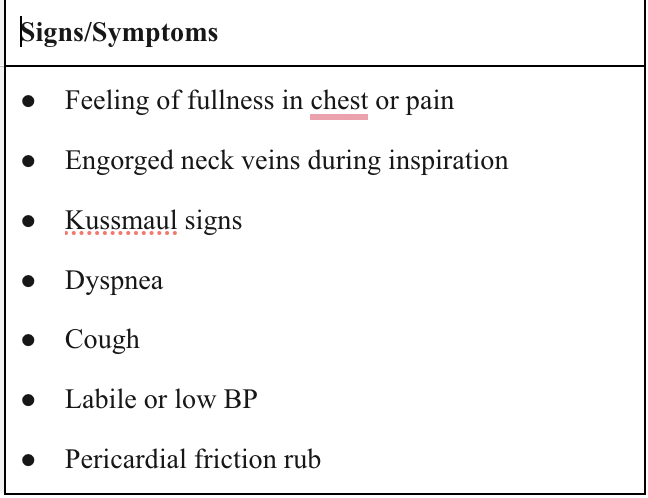
what are the signs and symptoms of cardiac tamponade and pericardial effusion?
Chest fullness or pressure, dyspnea, cough
Kussmaul sign: ↑ JVD during inspiration
Pulsus paradoxus: SBP drop >10 mmHg with inspiration
Muffled/distant heart sounds
Hypotension with narrow pulse pressure
Labile BP
Beck’s Triad (classic):
Hypotension
JVD
Muffled heart sounds
What are the medical and surgical management options for cardiac tamponade?
Pericardiocentesis:
Removes fluid to restore CO
Position: HOB 45–60°
Monitor VS, SpO₂, ECG, hemodynamics
Ultrasound-guided needle insertion
Post-procedure: monitor rhythm, BP, CVP, heart sounds
Complications: arrhythmias, coronary/ventricular puncture, pleural laceration
Pericardiotomy (Pericardial Window):
For recurrent effusions (e.g., neoplastic disease)
Creates an opening for continuous drainage into the mediastinum
What are key nursing management priorities for a patient with cardiac tamponade?
Maintain hemodynamic stability — monitor VS, BP, CVP, heart sounds closely
Keep emergency equipment (pericardiocentesis tray) ready at bedside
Administer oxygen and maintain IV access for emergency meds/fluids
Position patient semi-Fowler to ease breathing
Monitor for signs of recurrence: JVD, hypotension, muffled heart sounds
Evaluate response after fluid removal (improved CO, BP, LOC)
Provide emotional support and explain procedures to reduce anxiety
Document all assessments, interventions, and changes in condition
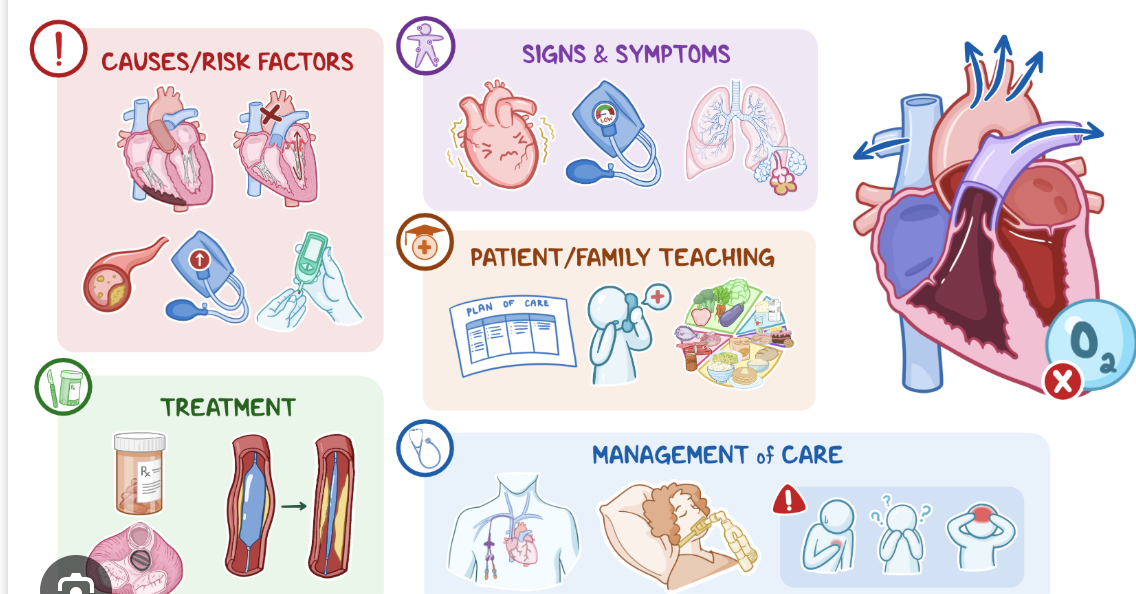
what is Cardiogenic shock
Life-threatening condition where decreased cardiac output (CO) leads to inadequate tissue perfusion
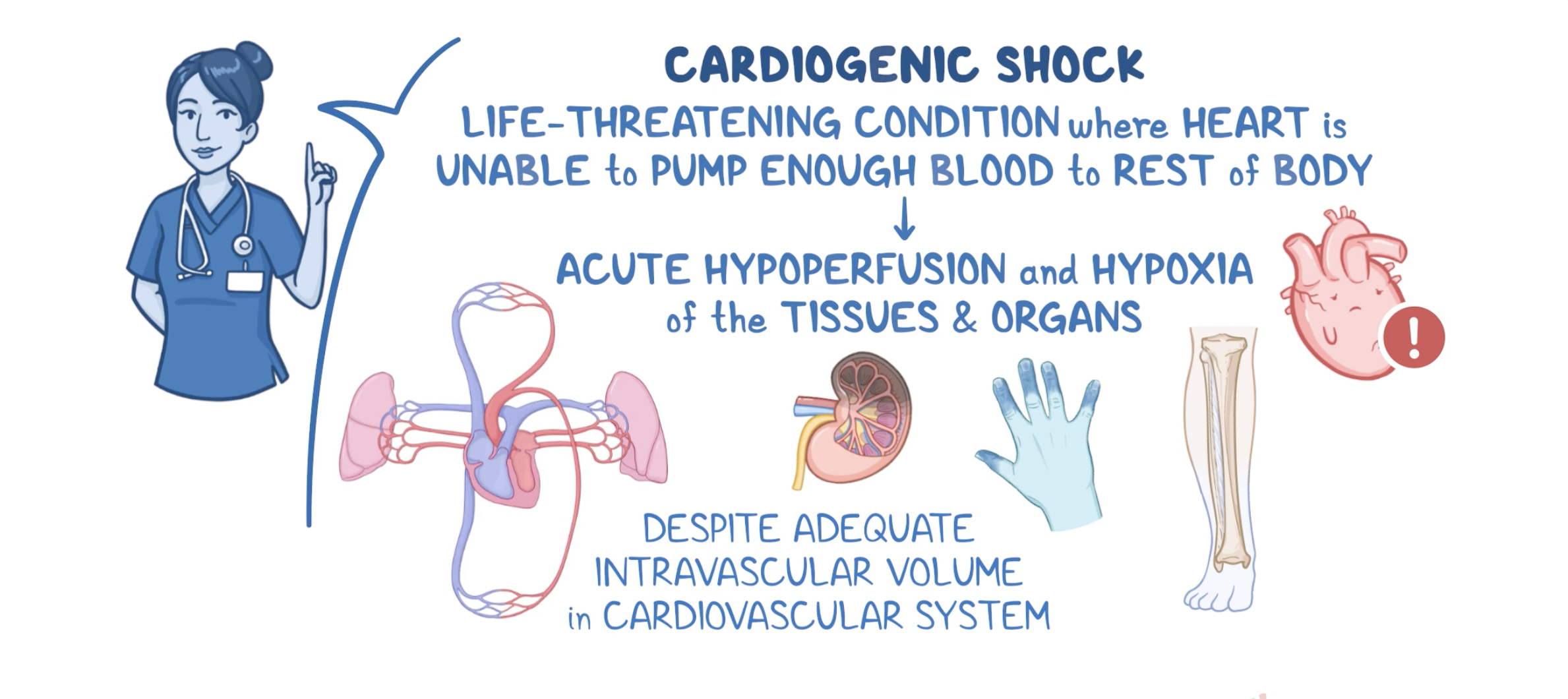
Pathophysiology of cardiogenic shock
Pathophysiology
Ventricular dysfunction → decreased stroke volume (SV) → decreased CO.
↓ CO → ↓ arterial blood pressure → inadequate tissue perfusion.
↓ Coronary perfusion → worsening myocardial ischemia → further ↓ contractility.
Ventricular failure → ↑ pulmonary pressures → pulmonary congestion/edema → hypoxia → organ ischemia.
Compensatory responses:
SNS stimulation → ↑ systemic vascular resistance (SVR), tachycardia
RAAS activation → fluid retention → further cardiac workload
Result: vicious cycle of hypoperfusion, ischemia, and pulmonary congestion.
Signs and symptoms of cardiogenic shock
Neurologic: Restlessness, confusion, agitation (cerebral hypoxia)
Cardiovascular: Hypotension, weak/rapid pulse, tachycardia, arrhythmias
Respiratory: Tachypnea, pulmonary crackles, hypoxemia
Skin: Cold, clammy, cyanotic, or mottled
Renal: Decreased urine output
Metabolic: Early respiratory alkalosis → metabolic acidosis (from lactic acid buildup)
Key S/S: Cerebral hypoxia, low BP, rapid, weak pulse, cold clammy skin, tachypnea with crackles, ↓ urine output
Medial mangemnt of cardiogenic shock
mesures of cradiogenic shock
Mesures:
Continuous monitoring: ABGs, lactic acid levels, central venous oximetr
PA catheter may be used for accurate measurement of pressures and CO
Lab results eventually show organ dysfunction if shock progresses
Goals:
Correct underlying cause (e.g., PCI for MI)
Reduce cardiac workload
Improve oxygenation
Restore tissue perfusion
Interventions:
Arrhythmia management: Treat causative rhythm disturbances
Fluid management:
Hypervolemia → diuretics, vasodilators, or mechanical support
Hypovolemia → IV fluids (NS, LR, albumin)
Oxygen therapy: Supplemental O₂, possible positive-pressure ventilation
Mechanical ventilation: Optimize oxygenation, reduce energy demand
Activity: Strict bed rest to minimize cardiac workload
Renal replacement therapy
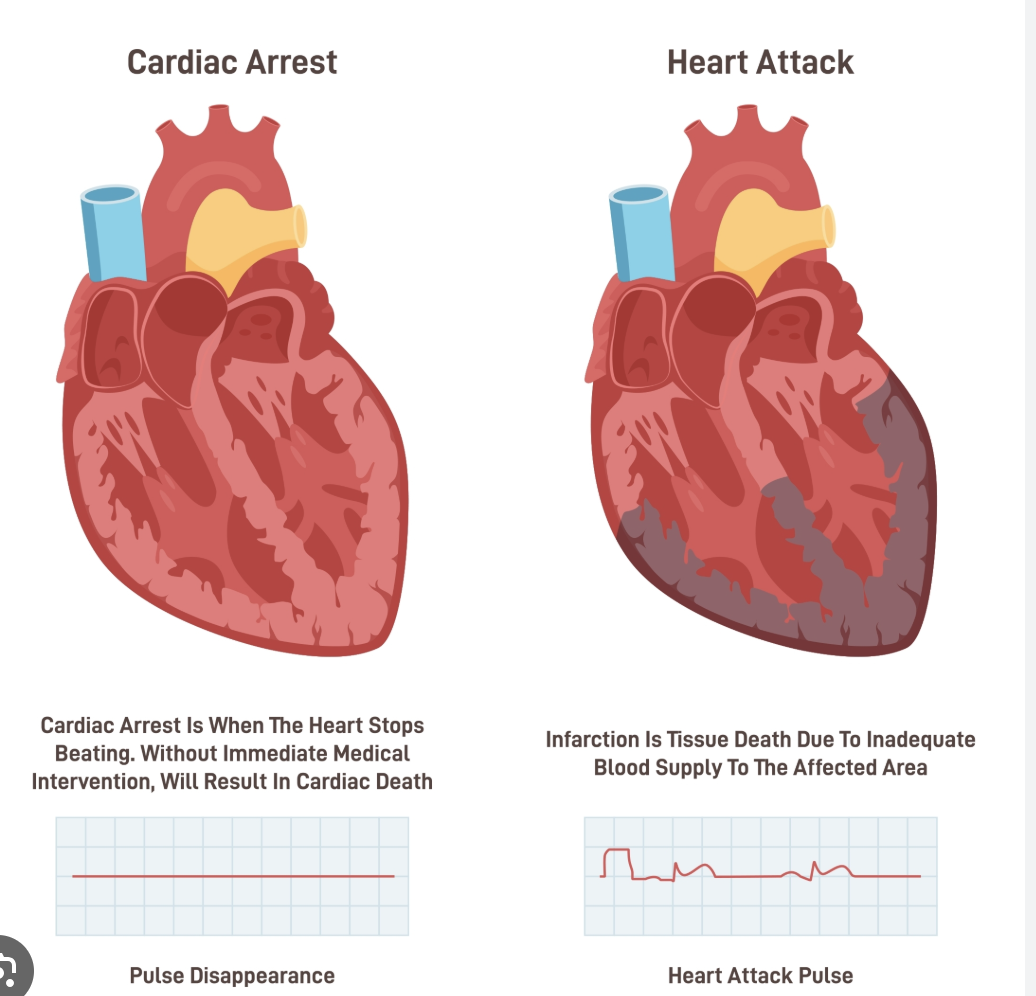
Cardiac Arrest
Patho
Signs and symtoms
mangemnt
Diagnosis/Patho | Signs/Symptoms | Management |
● Occurs when heart ceases to produce an effective pulse and circulate blood ● Caused by cardiac electrical event such as ventricular fibrillation, progressive profound bradycardia, or asystole ● Can be from resp arrest | ● Consciousness, pulse, BP lost immediately ● Ineffective resp gasping ● Pupils of eyes begin dilating within 45 seconds ● Perhaps seizures | ● CPR, allows blood flow to vital organs |
Emergency CPR and advanced cardiac life
“C-A-B” Sequence (AHA 2010/2015):
Compressions: 30 compressions, 2–2.4 in depth, 100–120/min, allow full recoil
Airway: Open airway
Breathing: 2 rescue breaths
Defibrillation: Immediate for VT/VF
Hands-only CPR is effective for bystander out-of-hospital arrest
Advanced cardiac life support:
Early defibrillation + medications (epinephrine, antiarrhythmics)
Survival inversely related to time to defibrillation