Blood Physiology Lecture 5 (Platelets)
1/67
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
68 Terms
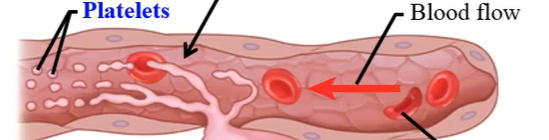
What is hemostasis?
The prevention of blood loss
Platelets are important in:
Hemostasis
Platelets are found:
in the middle “buffy coat” mixed with the white blood cells
Pro-hemostatic or pro-coagulant factors prevent:
Blood loss
Anti-hemostatic or anti-coagulant factors are factors which:
keep the blood fluid
Our body tries to maintain a state where blood can circulate:
smoothly, without formation of unnecessary clots
What are the steps of hemostasis?
Vasoconstriction, primary hemostasis or platelet plug, secondary hemostasis or blood clotting/coagulation (red thrombus)
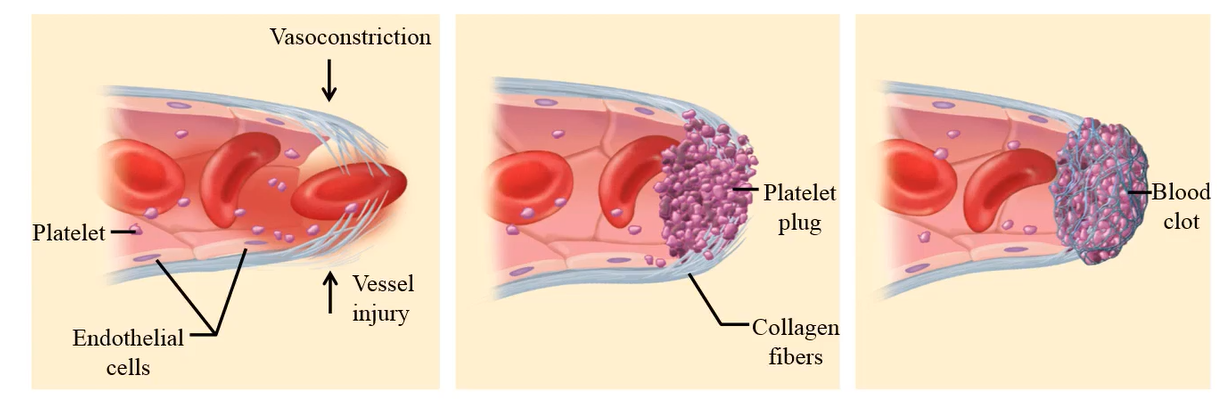
What is vasoconstriction in hemostasis?
When a ruptured blood vessel contracts to minimize blood loss at the site of the cut
What causes vasoconstriction?
Injury (blood vessel, smooth muscle) stimulates pain receptors that activate nerve endings that are directly affected by the cuts.
Local injury to the platelets causes the release of:
serotonin, which acts as a vasoconstrictor
What is primary hemostasis or platelet plug formation?
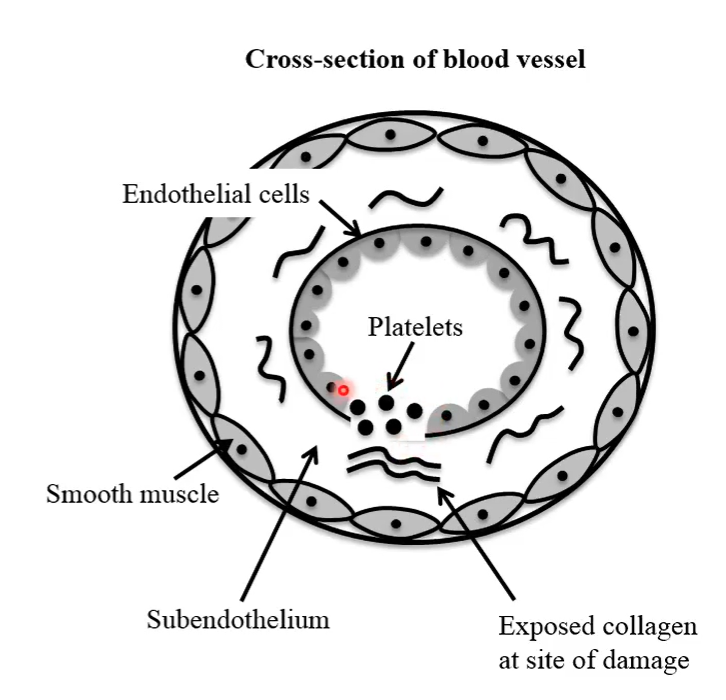
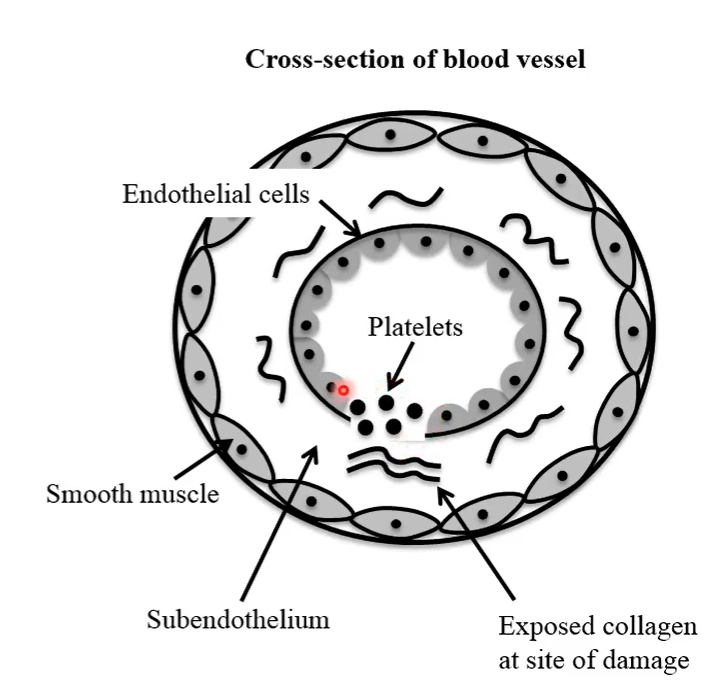
When platelets aggregate to form a platelet plug or a white thrombus (It is known as white thrombus because platelets are colorless cells)
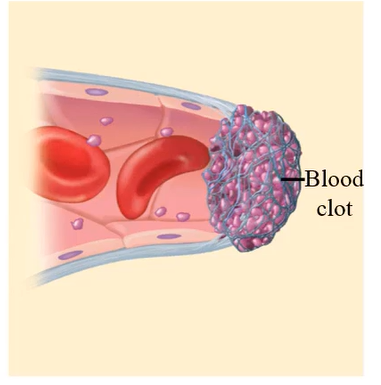
What is secondary hemostasis or blood clotting/coagulation (red thrombus)?
If the bleeding does not stop after the formation of the white thrombus, blood clotting enzymes are activated to form a stronger gel-like clot at the cut site.
The word thrombus refers to a:
blood clot
Where Do Platelets Come From?
pluripotent stem cells of the bone marrow
Pluripotent stem cells are converted to what to become platelets?
Megakaryocytes
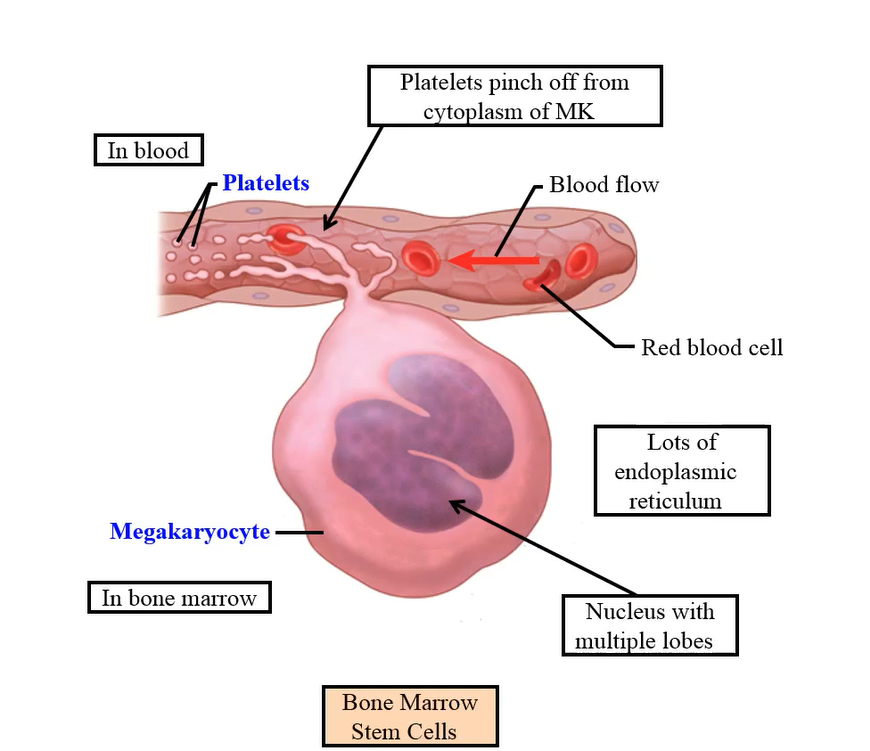
Platelets are pinched off from what part of megakaryocytes?
Cytoplasmic
Platelets contain what within?
Organelles
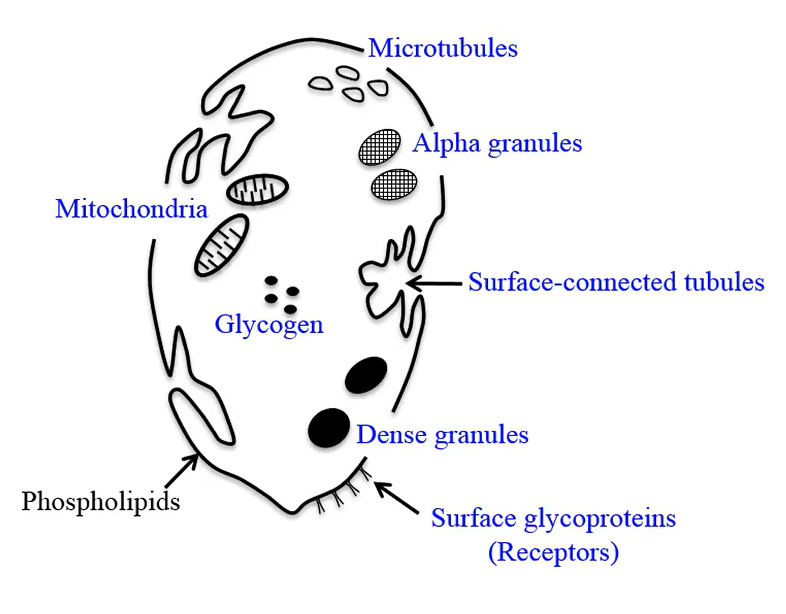
Platelets contain granule organelles called:
alpha, and dense
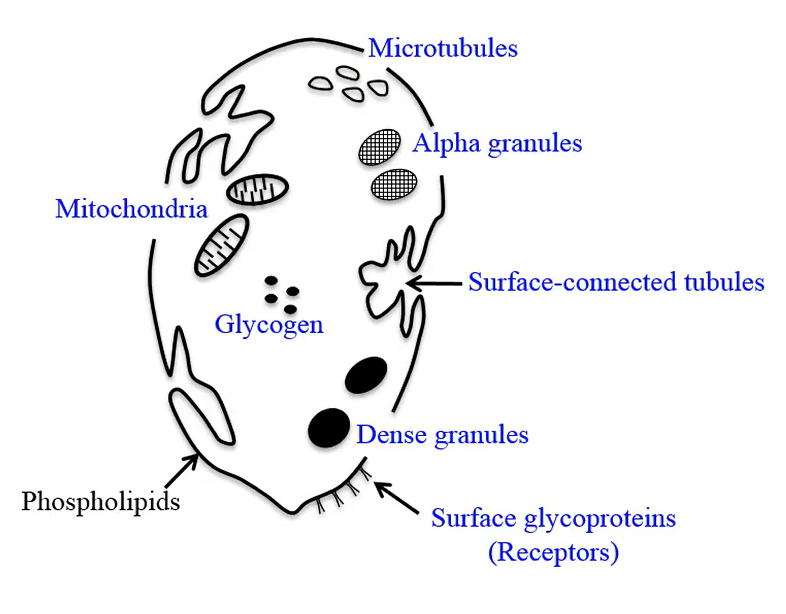
Platelets do not contain what kind of organelle?
Nucleus
Platelets contains what for energy?
glycogen
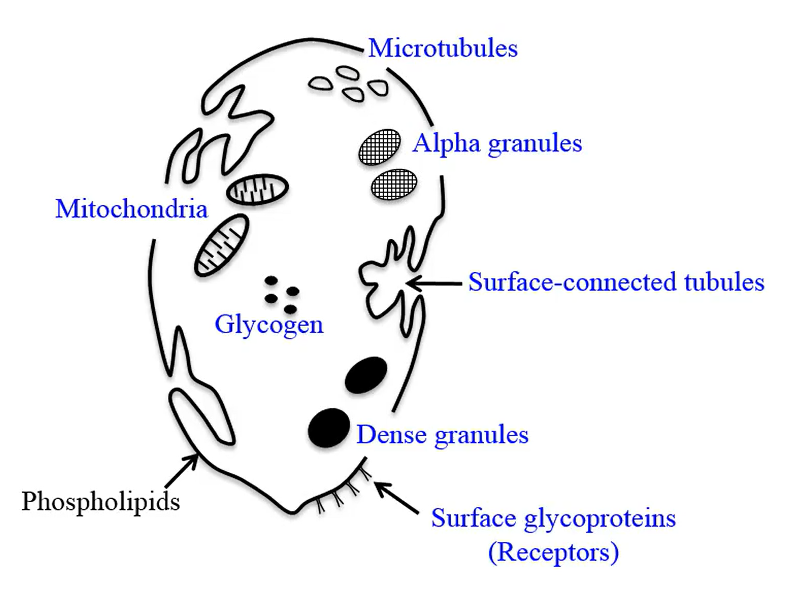
Platelets contains contractile proteins:
actin and myosin
Platelets contain what which acts as receptors for clotting proteins?
glycoproteins
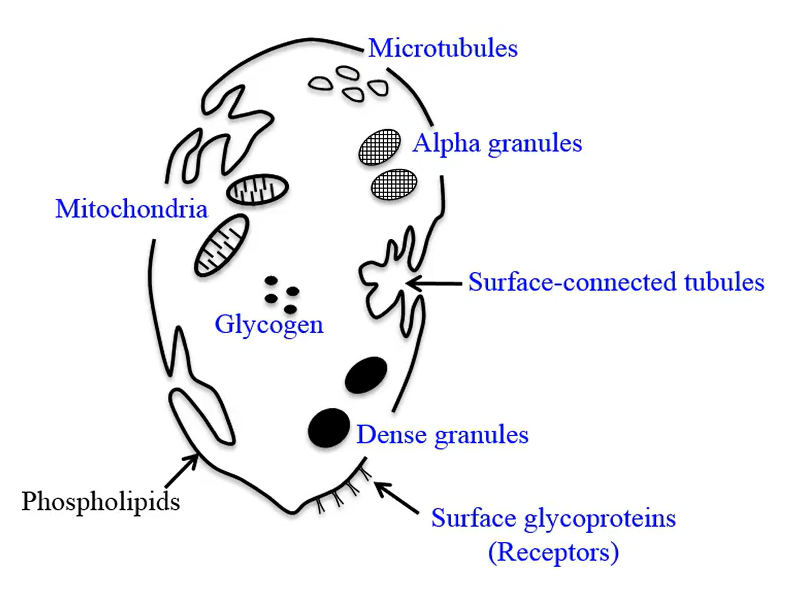
Platelets contains canaliculi (small passageways), also known as:
Surface connected tubule
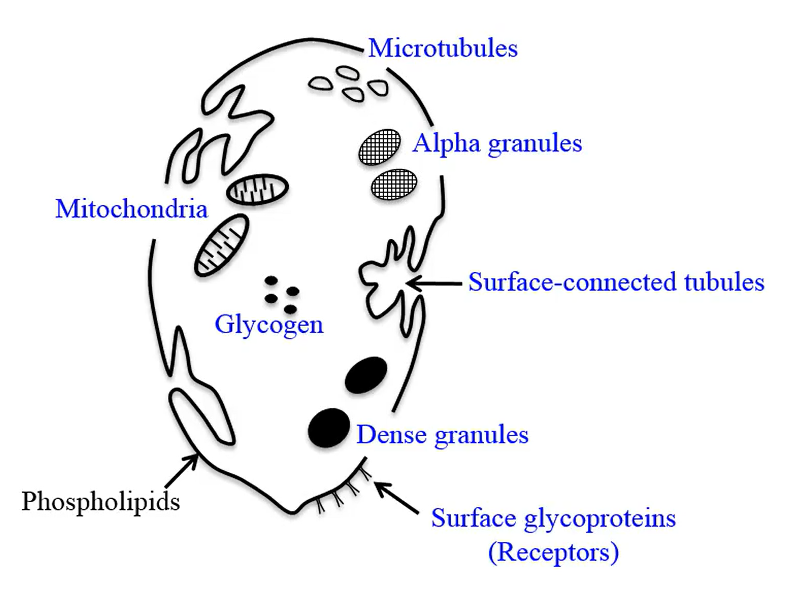
Alpha granules contain:
Large molecules: adhesive protein Von Willebrand factor, growth factors, some blood clotting factors and cytokines
Dense granules contain small molecules:
ADP and ATP, 5-hydroxytryptamine (serotonin) and calcium
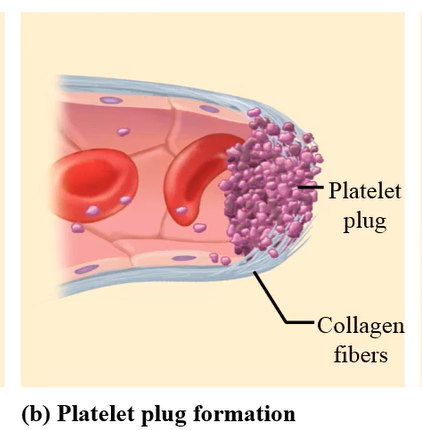
What is the 1st step of platelet plug formation?
Adhesion: Platelets must adhere to a surface in the process of hemostasis
Normally platelets do not stick to the smooth surface of blood vessels but:
injury to blood vessels disrupts the endothelial layer and exposes the underlying collagen
Platelets adhere to the collagen tissue using:
von Willebrand factor
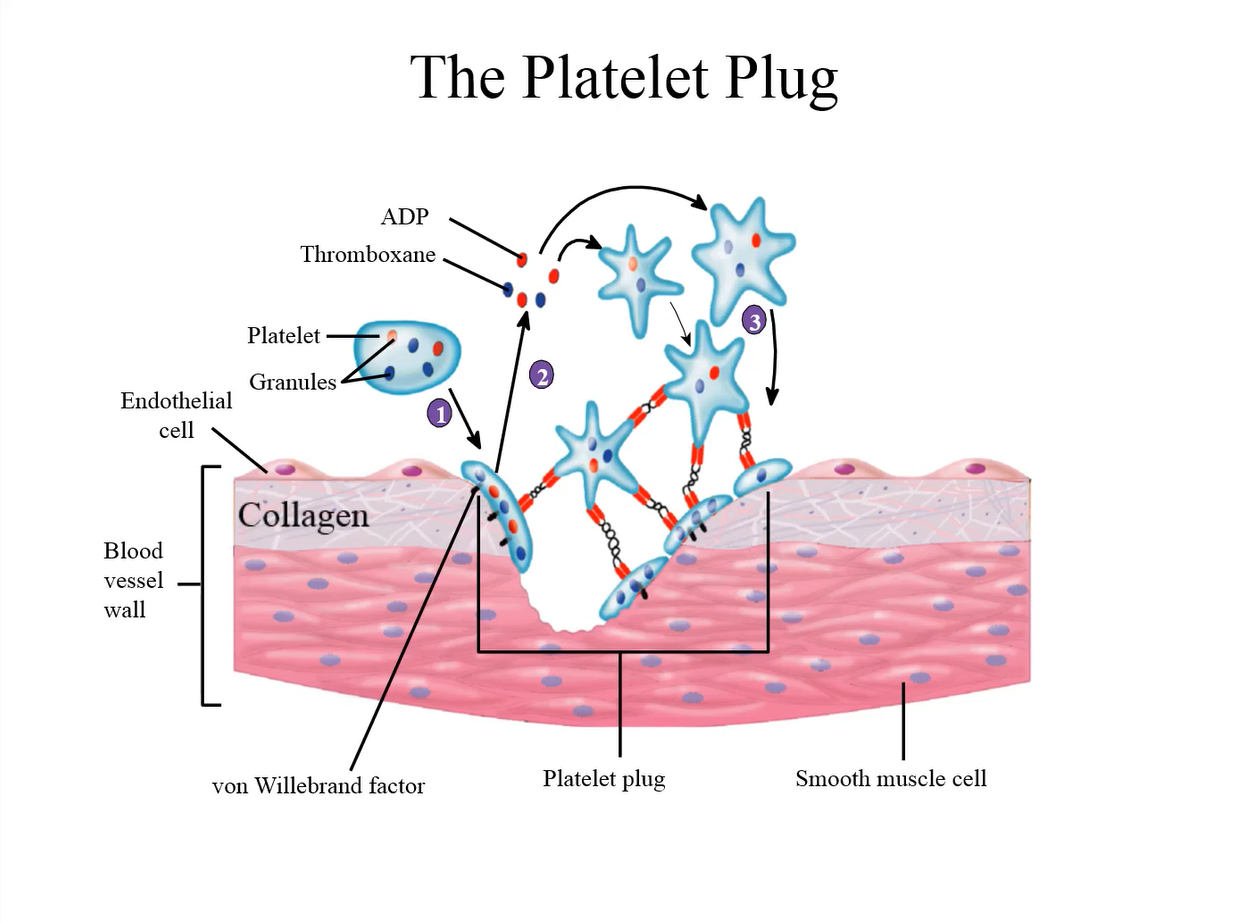
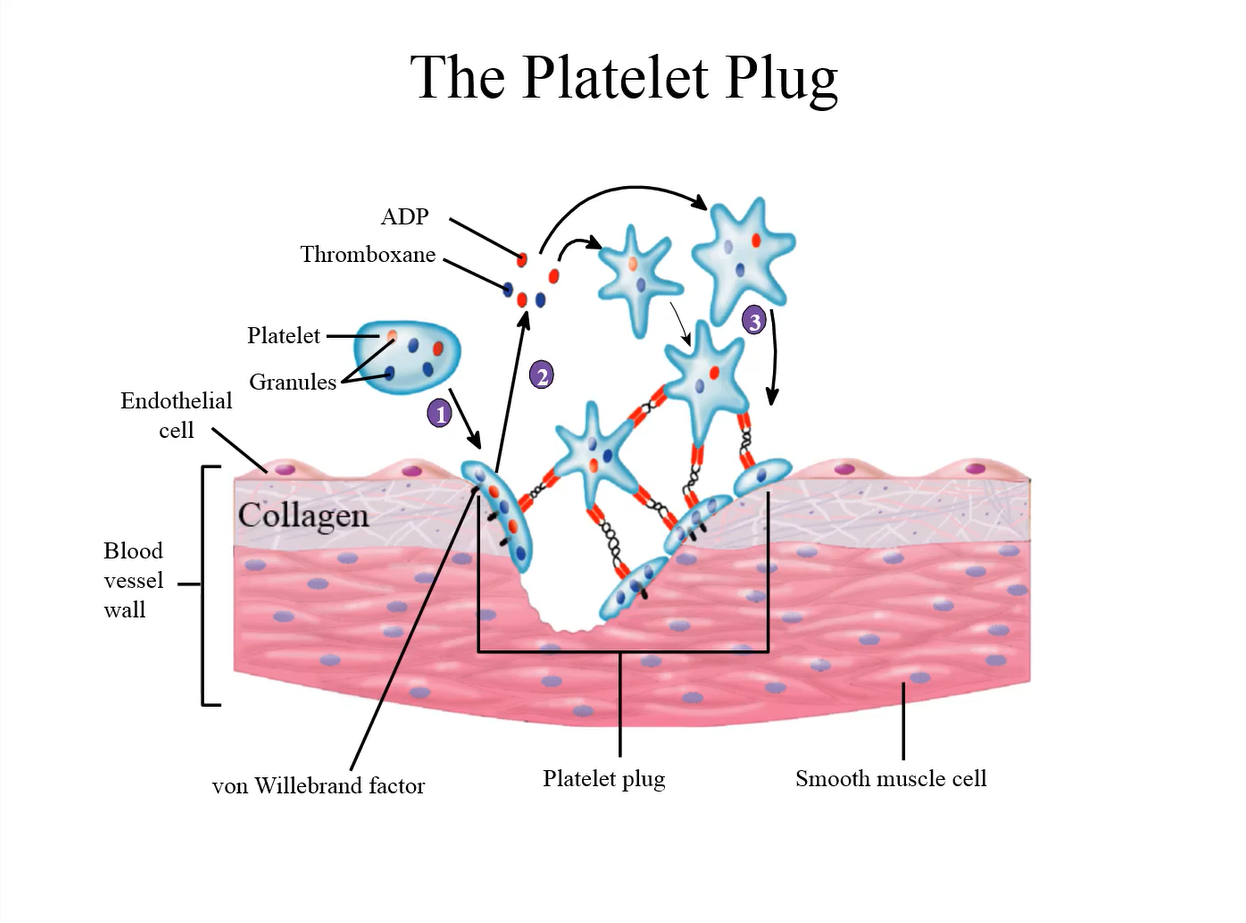
von Willebrand factor is a protein secreted by:
platelets and endothelial cells
Once secreted, von Willebrand factor can change:
conformation and bind to platelets
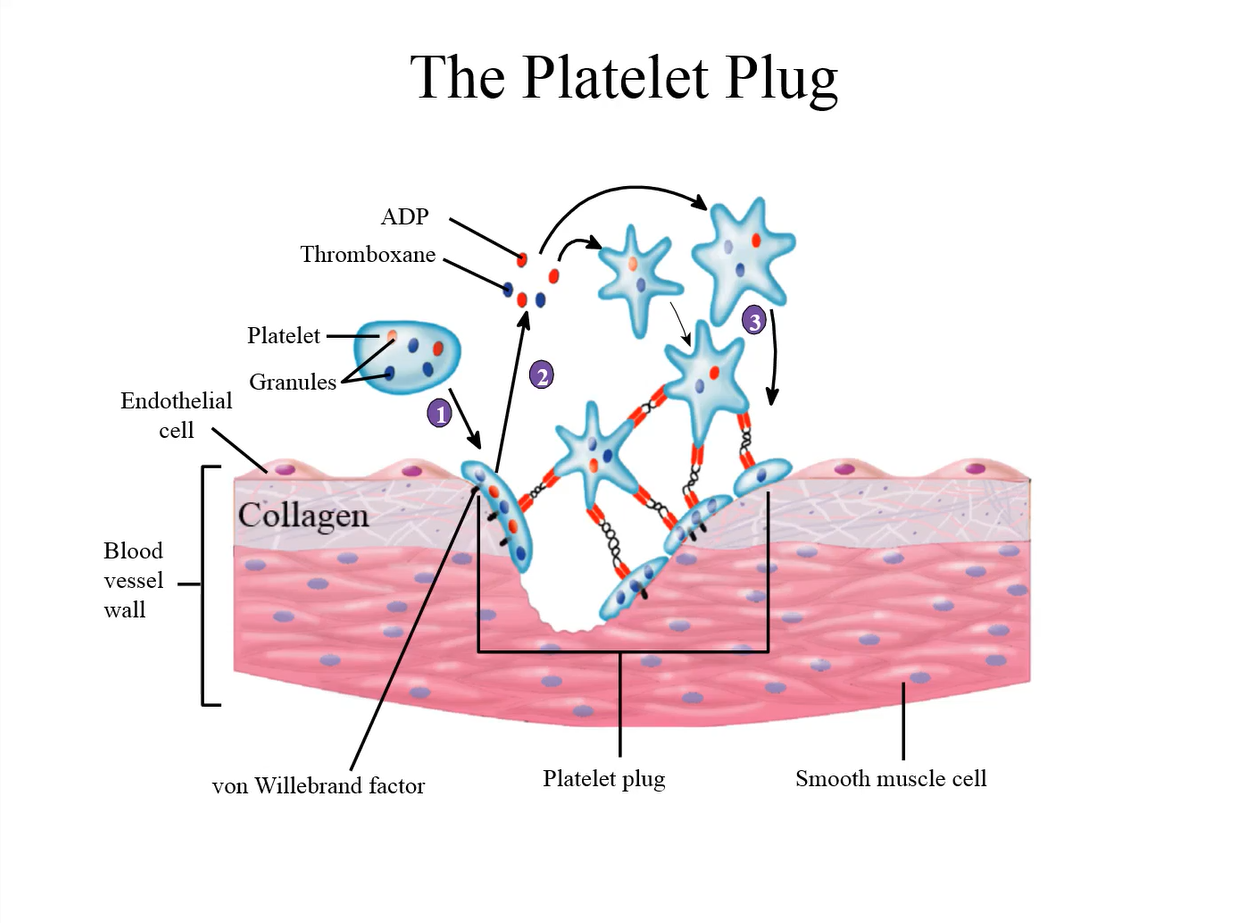
von Willebrand factor forms a bridge between the:
damaged vessel wall and the platelets
What is the 2nd step of platelet plug formation?
Binding of platelets to collagen triggers the release of chemicals from their storage granules (ADP and serotonin)
ADP and serotonin act locally on the platelets to change:
metabolism, shape, and expression of receptors on the surface of the platelet (step 2 of platelet plug formation)
What is step 3 of platelet plug formation?
New platelets to adhere to old ones by a positive feedback effect which rapidly forms a platelet plug inside the vessel
von Willebrand factor forms a:
a bridge between the damaged vessel wall and the platelets
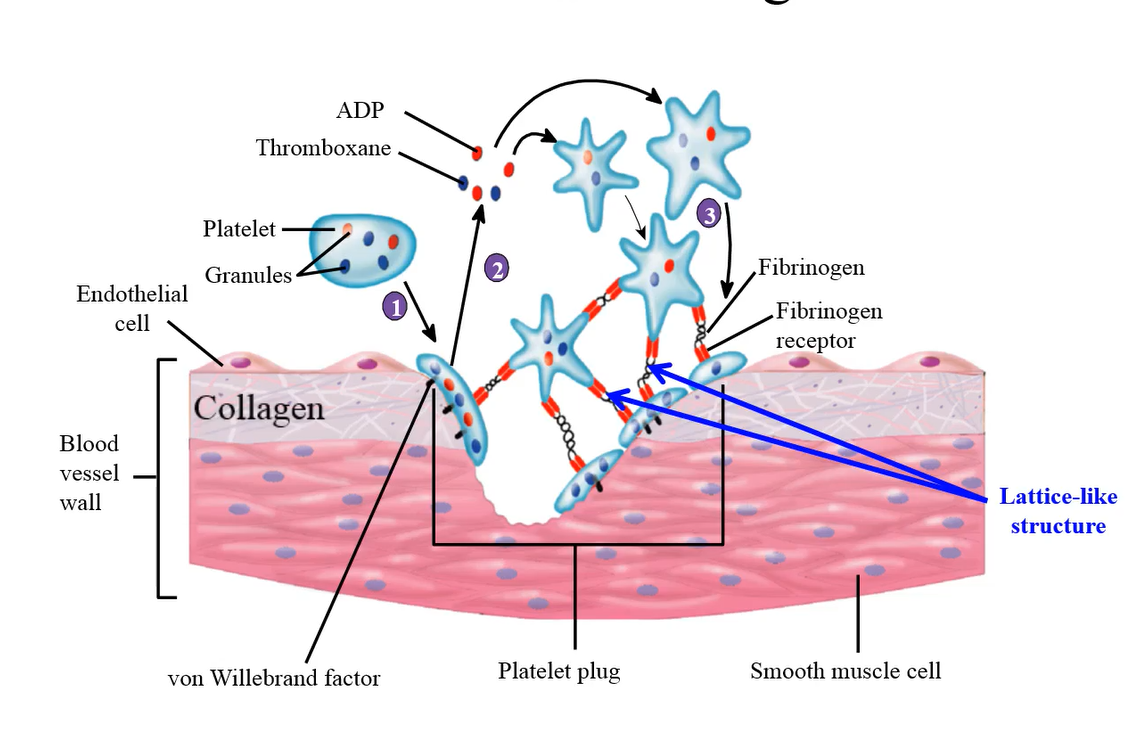
The activated platelets express a fibrinogen receptor on their surface, which can bind to:
fibrinogen, a plasma protein, and other platelets to form a network, or lattice-like structure, which ultimately forms the plug
During the platelet plug process the activated platelets also secrete:
thromboxane A2 and ADP, which attract more platelets to the cut site, and the aggregation continues
After the platelet plug is formed, the plug can contract using its
contractile proteins actin and myosin to tighten the plug and seal the cut site
What are the roles of activated platelets?
Adhesion of platelets triggers activation of the platelets. Once platelets are activated, they secrete the compounds Serotonin, Thromboxane A2, and ADP
Serotonin does what when released by activated platelets?
vasoconstrictor for muscular smooth muscles
What does ADP do when released by activated platelets?
plays a role in further platelet aggregation
What does Thromboxane A2 do when released by activated platelets?
Promotes further platelet aggregation and vasoconstriction of the vascular smooth muscle which will reduce blood flow to the cut site
Upon platelet activation, phospholipids exposed on the surface of the platelet aid in the conversion of
prothrombin to thrombin, which acts to promote further platelet aggregation
Why does the plug not expand along the undamaged endothelium of the blood vessel?
These cells synthesize and release prostacyclin, and nitric oxide which inhibit the spread of the platelet plug along undamaged endothelium
What does prostacyclin (prostaglandin I2 or PGI2) do?
inhibits platelet aggregation
What does Nitric oxide (NO) do?
inhibits platelet adhesion, activation and aggregation
The innate response of inflammation occurs within:
seconds of the initiation of injury
Following some time lag after injury, chemicals are released from the blood vessel wall which start the process of healing by:
initiating the formation of the platelet plug at the site of the cut
Membrane damage, or a disturbance in the cell membrane, initiates the production of:
arachidonic acid from membrane phospholipids
Arachidonic acid has two pathways:
Lipoxygenase, and Cyclooxygenase
In the lipoxygenase pathway, arachidonic acid is converted to:
leukotrienes by the enzyme lipoxygenase, and these chemicals then initiate inflammatory responses of swelling
In the Cyclooxygenase pathway, Arachidonic acid is converted to:
a prostaglandin by an enzyme known as cyclooxygenase or COX
Platelets and endothelial cells both have the cyclooxygenase enzyme, but they have different:
isoforms, or variants, of the enzyme, so hemostatic responses will vary.
The prostaglandins (COX) play a role in:
hemostatic effects that help to prevent blood loss.
Generally, the acute inflammatory response precedes:
hemostatic effects (stop bleeding)
Aspirin (in the context of blood) is prescribed to:
prevent clot formation in patients that have a potential risk for heart attacks
In the cyclooxygenase pathway, arachidonic acid is produced from:
membrane phospholipids as a result of membrane rupture and injury
There are two isoforms of the cyclooxygenase enzyme, called:
COX 1 and COX 2
Healthy endothelial (facing lumen) are subject to action of what in the cyclooxygenase pathway?
COX 2 enzyme
COX 2 activity results in:
the synthesis of prostacyclin and this has an anti-hemostatic effect.
The prostacyclin synthesized from:
arachidonic acid, keeps the plug from expanding to adjacent undamaged endothelial cells.
Platelets are subject to what in the cyclooxygenase pathway?
COX 1 enzyme
COX 1 produces thromboxane A2 and has what kind of effect?
a pro-hemostatic, or favors the formation of a platelet plug
Aspirin can inhibit the actions of both:
COX 1 and COX-2
Once COX-1 is inhibited in the platelets, the chances of producing thromboxane A2 are:
Completely blocked. Platelets are non-nucleated cells and once their enzyme is inhibited, the actions of the COX 1 enzyme are completely blocked, as they cannot synthesize new COX 1 enzyme.
Once COX-2 is inhibited, healthy endothelial cells will eventually start synthesizing new:
COX-2 enzymes as they are nucleated. COX-2 enzymes then convert arachidonic acid to prostacyclin.
Aspirin can block the COX 1 pathway only and block all the:
Pro-hemostatic pathways; COX 2 pathways can overcome the inhibition of aspirin to make prostacyclin and keep the vessels vasodilated and decrease platelet aggregation
Low dose aspirin is used in patients who may have an increased risk of:
heart attacks to prevent clot formation