MIC 205 Exam 4: 18: Immunologic Disorders
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
83 Terms
Immunologic Disorders
Results in an overreaction or undereaction of the immune response
Over-Reaction
Allergy & Autoimmune
Undereaction
Immunodeficiency Diseases
Allergy
Immune system reacts to an antigen it usually ignores and typically results in a hypersensitivity condition
Any immune response against a foreign antigen exaggerated beyond the norm
Type I, Type II, Type III, Type IV
Autoimmune
The immune system is reacting to “self” therefore, has lost the ability to distinguish self/non-self
Autoimmune affects the
blood cells, endocrine organs, nervous and connective tissue, and other major organ systems
Immunodeficiency Diseases
No or little directed immune response
Primary ( at birth ) or acquired immunodeficiency diseases
Type I ( Immediate Hypersensitivity)
Exposure to allergens will cause the release of inflammatory molecules
histamines, kinins, proteases, leukotrienes, and prostagladins
Occurs in seconds to minutes
Examples of Allergens
Pollen-hay, cats, bee stings, foods, drugs, ragweed, dust mites
Type I ( Immediate Hypersensitivity) has a two step process that is IgE mediated, what are those two steps?
Sensitization
Degranulation
Sensitization ( Type I)
Primary exposure to the allergen
B cell activation will start the specific immune response
Plasma cells will produce an IgE response against the allergen (antigen)
IgE bind to mast cells, basophil, or eosinophil
Degranulation
Subsequent Exposure
Allergen binds IgE on mast cells, basophil, or eosinophil
Release of histamines and other cytokines ( degranulation)
Starts the inflammation response
Degranulation prompts a mild reaction ( localized), how does this happen?
Dependent on the portal of entry
reddening of skin, swelling, watery eyes, hives
Small inhaled allergens may reach the lungs and cause asthma
Systemic Anaphylaxis ( Anaphylacitc Shock) ( part of Type I)
starts localized then spreads systemic
many mast cells may degranulate at once, releasing large amounts of histamine and inflammatory mediators
What happens during Anaphylaxis?
drop in blood pressure
violent contractions of the bronchial muscle
airway constricted and fills with mucous
death within minutes
Treatment for Type I
Prevention of Desensitization ( staying away from allergen)
For mild reactions: antihistamines, corticosteroids, bronchodilator for asthma
Systemic Anaphylaxis: Immediate use of Epinephrine
3 different testing for Type 1
ImmunoCAP specific IgE blood test
Skin Test
Immunotherapy
ImmunoCap specific IgE blood test
Diagnosis based on detection of high levels of IgE against specific allergen within the patient’s blood
Immunotherapy
administer a series of injections of diluted allergen
must be repeated every two to three years
Type II ( Cytotoxic Hypersensitivity )
Reults when cells are destroyed ( cytotoxic) by an immune response
Combined activities of complement and antibodies ( IgM and IgG)
Occurs as a component in many other autoimmune diseases
Examples of Type II ( Cytotoxic hypersensitivity)
Destruction of blood cells following an incompatible blood transfusion
Destruction of fetal red blood cells in hemolytic disease of the new born
Drug inducted ( Pencillin reaction)
Blood Transfuion gone wrong ( Type II)
Donor’s blood group antigens may stimulate the production of antibodies in the recipient that binds to the transfused cells
Activates the complement system
Destruction of donated blood cells can occur in hours to days
Triggers blood clotting within vessels and circulatory failure
Hemolytic anemia
Hemolytic Disease of the new born ( Type II)
Rh antigen - common to EBCs of humans and rhesus monkeys
Rh- woman carrying a Rh+ fetus may be at risk for hemolytic disase
Usually in 2nd pregnancy: mother has rh- antibodies, but the baby has Rh+ antigens —> Rh- antibodies will diffuse into the placenta of the baby and cause a hemolytic disase
What is adminstered to prevent hemolyrtic disease of the newborn?
RhoGAm
Drug-induced cytotoxic reactions ( Type II cytotoxic hypersensitivity)
Penicillin and most drugs are too small to trigger an immune reaspone, but they can be antigenic if they bind to larger moleculs trigerringan immune response
Pencillin and Drug-induced cytotoxic reactions example ( Type II)
1.) Penicllin binds to platelets, thus triggering an immune response
2.) Complex triggers the humoral response and recruit the complement to form MAC and lyses the cells
3.) Inhibits the ability of the blood to clot due to a decrease in platelets
4.) Causes agranulocytosis and hemolytic anemia
Type III ( Immune complex-mediated)
Caused by the formation of immune complex
Some of the complexes are removed by phagocytes
Othr complexes will bind to blood vessel walls or be trapped in organs and joints
Inflammation response will cause tissue damage
can cause localized or systemic reactions
Type III can cause
Localized and systemic Reactions
Examples of Localized Reactions ( Type III)
Hypersensitivity Pneumonitis
Glomerulonephritis
Hypersensitivity Pneumonitis ( Localized Reaction)
inhalation of antigens into lungs stimulates antibody production
Subsequent inhalation of the same antigen results in the formation of immune complexes and activates comlment system
eg. Farmer’s lung from Hay spores, Pigeons’s lung from dust from pigeon feces
Glomerulonephritis ( localized reaction)
immune complexes in the blood are deposited in glomeruli (kidneys)
damage to the glomerular cells impedes blood filtration
causes kidney failure and ultimately, death
Examples of Systemic Reaction of Type III
Rheumatoid Arthritis
Systemic Lupus
Rheumatoid Arthritus ( systemic reaction)
immune complexes deposited in the joints result in the release of inflammatory chemicals
Loss of the cartilage of the joint and bone loss
Treated with anti-inflammatory drugs
0.5-1 percent of the U.S adult population
Systemic Lupus ( systemic reaction
Antibodies bind to DNA to form immune complex formation
DNA-antibody complexes are deposited in the skin
Many other auto-antibodies can also occur
16,000 diagnosed yearly in the US ( 90% women)
Symptoms of Systemic Lupus
Rash, light sensitivity, joint pain, bleeding disorder, kindey damage, neurological symptoms
Treatment for Systemic Lupus
Immunosuppresive drugs and Glucocorticoids
Type IV ( Delayed or Cell-Mediated)
Inflammation 12 to 24 hours after contact with certain antigens
Due to antigen, antigen-presenting cells, and T cells
Delays reflect the time it takes for macrophages and T cells to migrate and proliferate at the site of the antigen
3 major classes of Type IV
1.) Tuberculin Response
2.) Contact Dematitis ( poison ivy, latex, soaps)
3.) Graft Rejection ( rejection of tissues or organs that have been transplanted
Example of Type IV
Wearing gloves for a day and not getting a reaction —> Wearing gloves the next day and getting a reaction ( specifically latex gloves apply to this situation)
Contact Dermatitis ( Type IV)
cell-mediated immune response ( T-cells)
results in an intensely irritating skin rash
acellular, fluid-filled blisters develop in severe cases
What is contact dermatitis triggered by ?
Chemically modified skin proteins that the body regards as foreign
What is the treatment for contact dermatitis
Glucocorticoids
Tuberculin Response ( Type IV)
An injection of tuberculin beneath the skin causes a reaction in an individual exposed to tuberculosis
Used to diagnose contact with antigens of M. tuberculosis
-24 to 73 hr post exposure
The Immediate response is generated by memory T cells
Tuberculin Response is used to diagnose contact with antigens of M. tuberculosis, what does a “no response” results yield?
No response means that the individual is not infected or vaccinated
This is also may indicate that the individual may susceptible to micro bacterial tuberculosis
Tuberculin Response is used to diagnose contact with antigens of M. tuberculosis, what does a “red, hard swelling” results yield?
Red, hard swelling indicates that the person has been previously infected or immunized.
If a person has a “red,hard swelling” result but 2x worse on the Tuberculin Response test, what does that indicate?
A overreactive immune response which indicates that the immune system doesn’t remove it self accurately.
It can’t distinguish self from non-self
Graft Rejection ( Type IV)
Rejection of tissues or organs that have been transplanted
Grafts perceived as foreign by a recipient undergo rejection due to differences in MHC I or II molecules
Why is immune response against foreign MHC on graft cells difficult?
They are a difficult because of a high degree of variability
Example of a Graft Rejection
Organ Transplants
What type of drugs stop graft-versus-host disease?
Immunosuppressive drugs
Different causes of Development of Autoimmune disease
Loss of recognition of self vs. non self
Occurs more often in elderly
More common in women than in men
Genetic and Environmental ( Examples: Diseases)
Autoimmunity affecting endocrine organs
Type I diabetes mellitus juvenile ( T-cells destroy the insulin-secreting cells of the pancreas)
Autoimmunity affecting nervous tissue
Multiple sclerosis ( T cells destory the Myelin sheaths that surrounding neurons)
Autoimmunity affecting connective tissue
Rheumatoid arthritis
Autoimmunity affecting blood cells
Autoimmune hemolytic anemia
Why are City kids prone to autoimmune diseases instead of rural kids?
They are prone to autoimmune diseases because they are constantly inside, so when they exposed to microbes, their body produces an overresponse
Why are rural kids less prone to autoimmune diseases?
They are less prone to autoimmune diseases because they are constantly exposed to microbes because they are out playing with dirt/hay, so their body builds immunity towards an infection. Thus making them less likely to develop autoimmune diseases
What are the two types of Immunodeficiency diseases?
1.) Primary ( inborn: genetic defects)
2.) Acquired
3 Examples of Primary ( Inborn: genetic defects)
1.) Agammaglobulemia
2.) DiGeorge Syndrome
3.) Severe Combined Immunodefiency (SCID)
Agammaglobulemia
B-cell deficiency
Treated with mass doses of immune serum & antibiotics
IgA deficiency is most common
DiGeorge Syndome
Due to the lack of thymus gland
T-cell deficiency
Viruses poses a greater threat
How is DiGeorge syndrome treated?
Thymic Stem Cells
Severe Combined Immunodeficiency (SCID)
Deficiency of lack of T and B-cells
Example of Severe Combined Immunodeficiency (SCID)
Bubble Boy
2 types of Acquired Immunodeficiency Diseases
1.) Infectious agents that cause these diseases leprosy, tuberculosis, AIDs
2.) Immunosuppressants that damage T and/or B cells
Examples: Chemotherapy/Radiation Therapy
Problem in Chemotherapy?
It targets cells that are actively replicating
Examples: Loss of hair, problems are immune system ( WBCs are actively growing)
AIDS ( Acquired Immunodeficiency Syndrome)
caused by Human Immunodeficiency Virus ( HIV)
What are the target cells of AIDS ( Acquired Immunodeficiency Syndrome) ?
T-helpers and macrophages
Death isn’t caused by AIDS itself, what is it caused by?
Infections/ Cancer
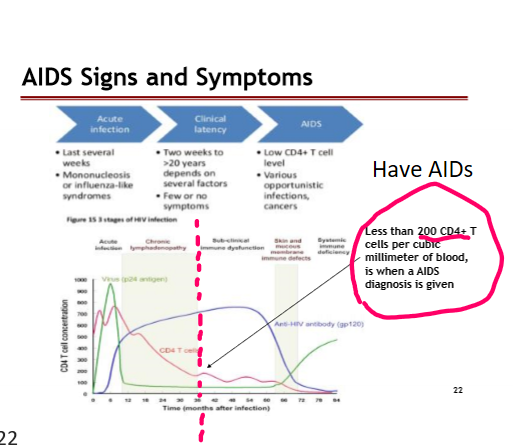
AIDS Signs and Symptoms: When do you know if you have AIDS?
Less than 200 CD4+ T cells per cubic millimeter of blood, is when an AIDS diagnosis is given
AIDS Signs and Symptoms ( Picture)
What are the 3 types of transmission of HIV?
1.) Sexual
2.) Blood Products
3.) Mother to Child
Sexual Transmission of HIV ( 0.5 to 1.0% transmission)
The majority of all HIV have been passed through unprotected sexual relations.
Transmissions occurs when an infected person comes in contact with the genital, oral, or rectal mucous membranes of a noninfected person
Blood Products (90% transmission)
Blood present with HIV comes in contact with:
Break in the skin
Open wounds
IV Drug Use
Blood/Plasma transfusions
Organ transplants
Tattoos and piercing
There have been no reports of HIV transmission via Mosquitos
Mother to Child ( 30% transmission)
Transmitted to the child during pregnancy, at childbirth, and during breastfeeding at a rate of about 25%
ARV’s and C-sections can reduce HIV transmission by about 1%
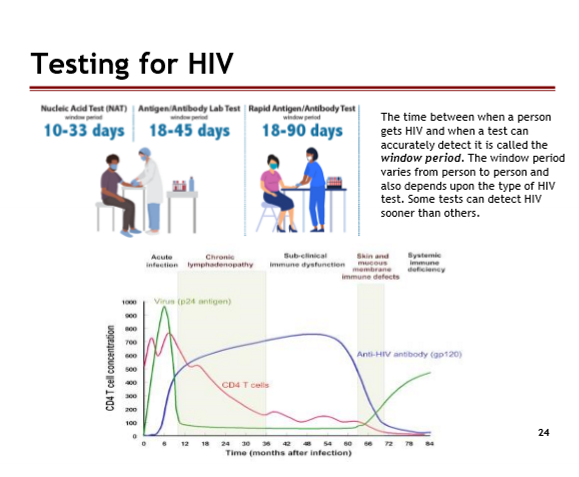
Testing for HIV: Window period
The time between a person gets HIV and when a test can accurately detect it is
It varies from person to person and also depends upon the type of HIV test
Some tests can detect HIV sooner than others
Testing for HIV ( image)
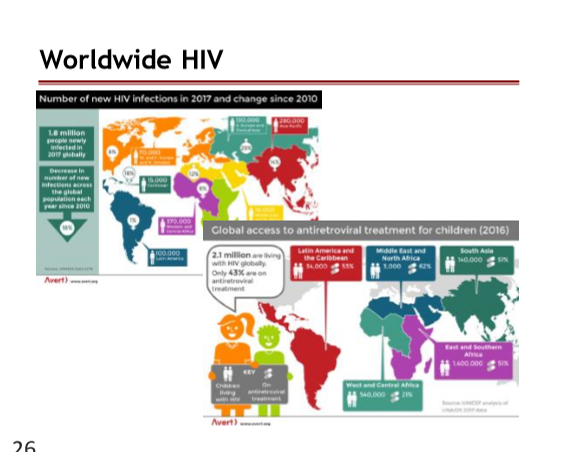
How many people worldwide live with HIV/AIDs?
36.7 million people are living with HIV/AIDS as of 2021
36.7 million were adults and 1.7% million were children (<15 years old)
54% women and girls
1.5 million new infections in 2021, this is a 23% reduction since 2014
1.3 million adults and 160 k children
How many people living in the United States have HIV/ AIDs?
1.2 million people living with HIV as of 2021
The number of HIV infections in the U.S. was 34,800 in 2019
HIV incidence declined 8% from 2015 to 2019
About 13% of people don’t know their status
How many people with HIV/ AIDS live in Arizona
18,975 people with HIV as of 2021
272 deaths in 2020
About 696 new infections, 87% were linked to care
How many people with HIV/AIDS live in the Phoenix Metro Area?
13,028 people in Maricopa COunty living with HIV in 2020
About 497 new infections of HIV in Phoenix Metro Area
Worldwide HIV ( picture)
Is an HIV Vaccine/Cure possible?
No, because the virus has the ability to integrate ( provirus) and hide in cells ( reservoir)
The virus is always creating errors and changing
Replication of the virus occurs at a rapid rate
Depletion of immune cells ( Immunodeficiency)
Immune exhaustion
Prophylaxis
However, it is important to bring awareness/ education on HIV
The HIV virus is always creating errors and changing
HIV has 1 million genetically variants
AIDS has 100 million genetically variants
10,000 defective virus partials
Why is the HIV virus always creating errors and constantly changing?
Reverse Transcriptase is sloppy and creates variations of HIV virus
Eliminate of T-helper cells = immune exhaustion
Prophylaxis (Pre/Post)
Give antiretroviral treatment and strong drugs to prevent development of virus for 6 months —> Test distributed again in 3 weeks —> Test at 6 weeks —> final test 6 months later ( to ensure if the person has been infected with HIV or not)
Pre-Exposure Prophylaxis (PREP)
Given to people who are in a relationship the drugs
The drugs are expensive, and the drugs are not good for you
Causes damage to liver and kindeys