Inflammatory and NonInflammatory Conditions of the Conjunctiva
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
Pemphigoid (Ocular Cicatricial Pemphigoid) pathophys
Autoimmune and chronic condition that causes subepithelial scarring of mucus membrane surfaces within the conjunctiva
signs/symptoms of Pemphigoid (Ocular Cicatricial Pemphigoid)
• Chronic unilateral conjunctivitis that progresses to bilateral
• Significant scarring
palpebral conj will scar to bulbar conj = symblepharon
• Severe FBS and pain
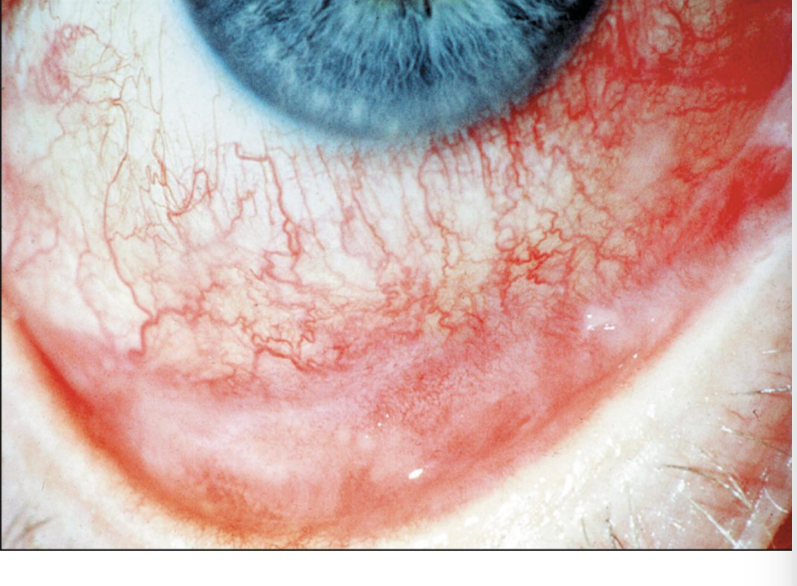
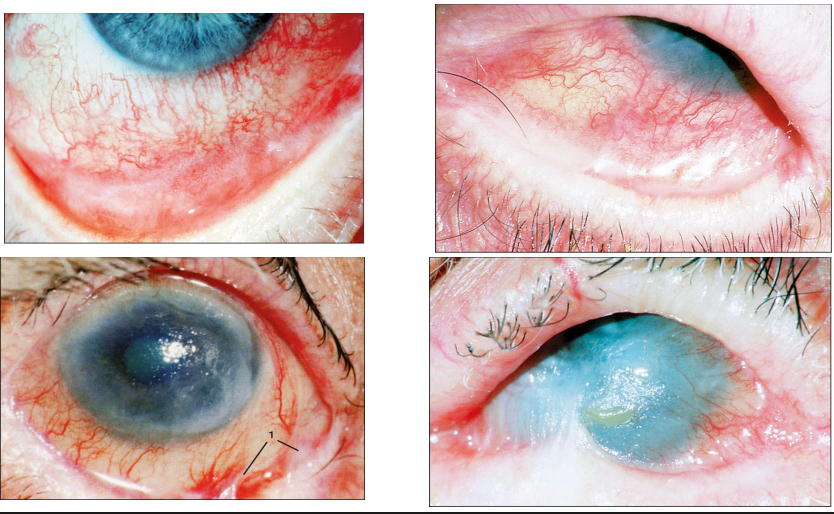
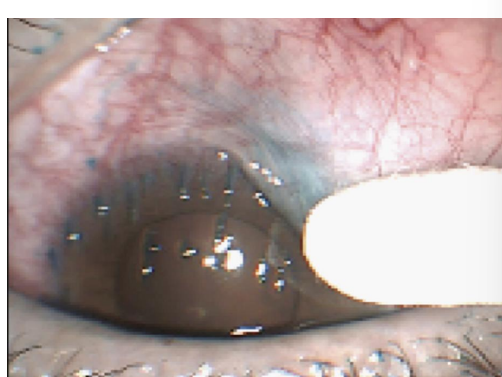
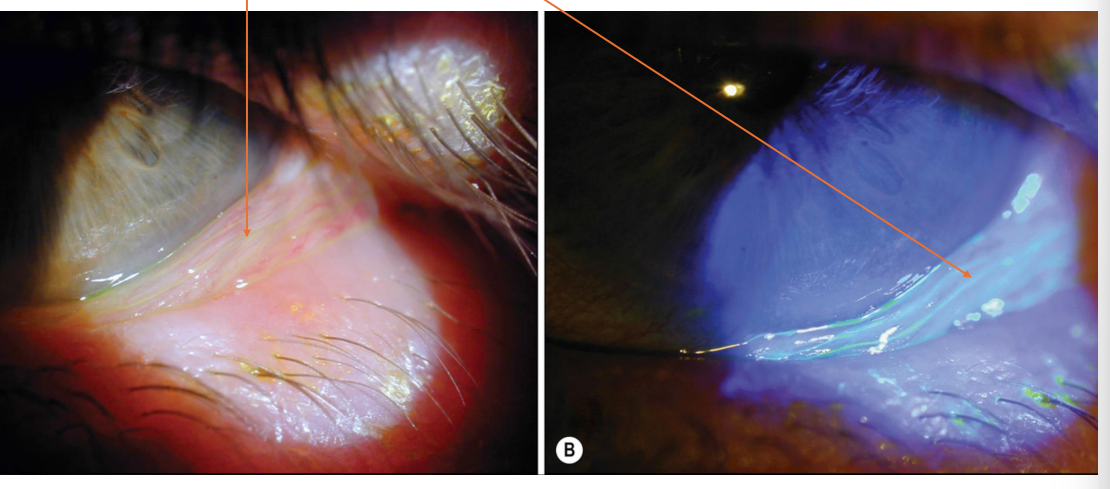
what this
Ocular Cicatricial Pemphigoid
conj should be clear but its becoming white
how do you diagnose OCP
biopsy
need to rule out all other kinds of auto immunes
how do we treat OCP
multidisciplinary approach w derm, oculoplastic, cornea
• Combination of dry eye therapy, antibiotic ungs, punctal occlusion, topical steroids, mucus membrane grafts, and keratoprosthesis as an end stage treatment
KERATOPROSTHESIS
limbal stem cells are dead so this is the best we got to keep the cornea viable
last case scenario
Steven Johnson Syndrome
A life-threatening condition that can cause a painful rash, and blistering of the skin and mucus membranes that results in scarring of the ocular surface and lids
Immune complex–mediated hypersensitivity reaction caused by many agents
• Medication
• Infections
• Auto immune conditions
• Idiopathic in 50% of cases

what are the ACUTE ocular findings of SJS
– first 7-10 days
• Mucopurulent or pseudomembranous conjunctivitis
• Episcleritis and Iritis
what are the CHRONIC ocular findings of SJS
weeks after initial presentation
• Symblepharon formation
• entropion, trichiasis, and instability of the tear film.
• Breakdown of the ocular surface leads to corneal scarring, neovascularization, and, in severe cases, keratinization of the entire eye
how do we treat SJS pt
consult w internal med
really, send to ER
ocular treatment - palliative mainly
aggressive lubrication/ dry eye treatment
uveitis
pseudomembrane peel
sx indication for symblepharon
Superior Limbic Keratoconjunctivitis (SLK)
Disease of the ocular surface characterized by bilateral chronic inflammation of the superior tarsal, bulbar conjunctiva and cornea
• True etiology is unknown but multifactorial
• Can be associated with DED, Sjogren’s, RA, mechanical friction
signs of Superior Limbic Keratoconjunctivitis (SLK)
• Superior epithelial defects and superficial punctate keratitis
sometimes have filaments —> liek when you rub dry skin and it rolls up
lissamine green stain
symptoms of Superior Limbic Keratoconjunctivitis (SLK)
Severe foreign body sensation, pain, photophobia, mucoid discharge, epiphora,
how do we treat SLK
• Essentially treating severe dry eye
• Aggressive Lubrication-preservative free ATs every 2 hours and ung at bedtime
• Cyclosporin .05% BID
• Can consider acetylcysteine 10% ophthalmic solution or Mucomyst 2-4 times per day depending on severity —> washes away mucus and filaments
• Epithelial defects- would add broad spectrum antibiotic drops such as ofloxacin QID
• Follow up in about 1 week (if epi defects presents) and in about 2-4 weeks for further management
Parinauds Oculoglandular syndrome most common cause
Cat Scratch Disease (Bartonella henselae)
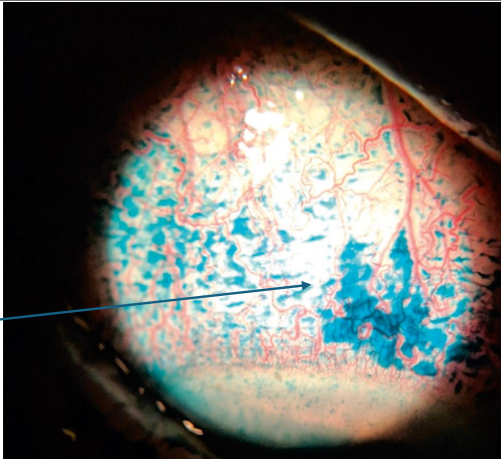
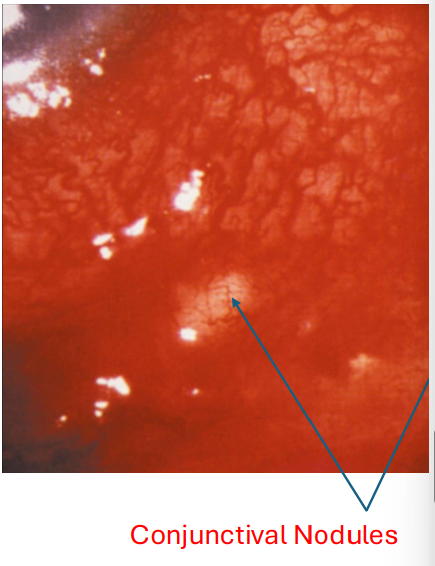
Parinauds Oculoglandular Syndrome
Characterized as a granulomatous conjunctivitis with lymphadenopathy
has conjunctival nodules
will Parinauds Oculoglandular Syndrome go away on its own
yes
some Dr use azithromycin
pathophys of Conjunctivochalasis
• Bilateral condition described has redundant, loose, non edematous bulbar conjunctiva
• Normal aging, mechanical forces
signs and symptoms of Conjunctivochalasis
• Ocular irritation, epiphora
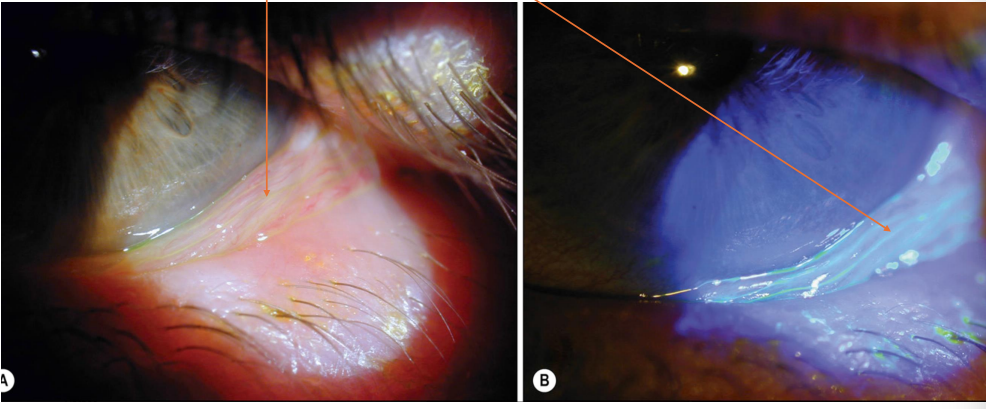
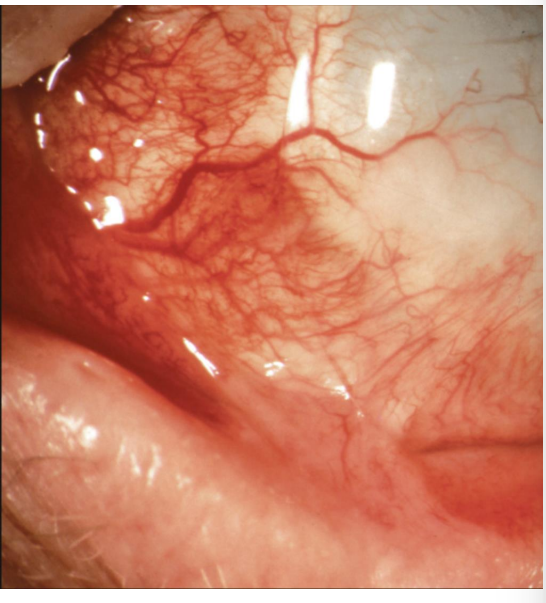
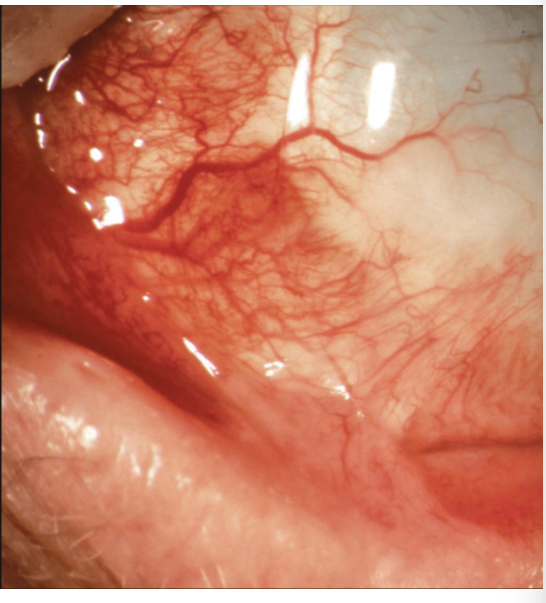
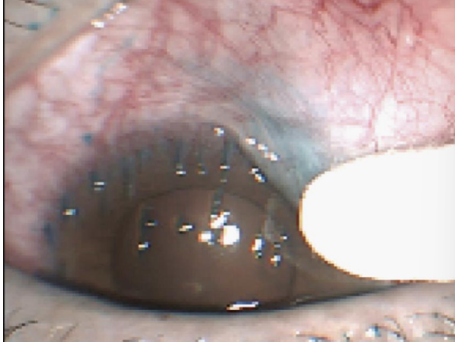
what this
Conjunctivochalasis
grooves hold more tears
how do we treat Conjunctivochalasis
often asymptomatic
DED treatment including Restasis and Xiidra
• Improve tear film stability and reduce ocular surface inflammation
• Surgical considerations
• If severely symptomatic- can consider excision
pyogenic granuloma
A benign vascular growth that typically develops on the palpebral conjunctiva following surgery, trauma or inflammation
whats pyogenic granuloma look like
• Pedunculated, fleshy, red/pink mass
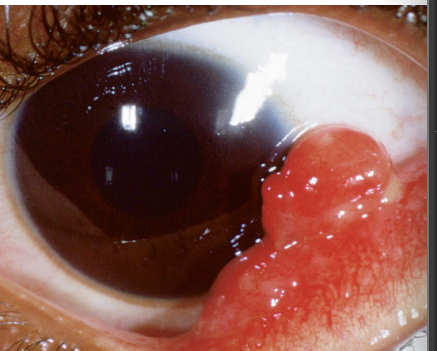
signs/symptoms of pyogenic granuloma
FBS/ minor pain
how do we treat pyogenic granuloma
sx
corticosteroids