Psychopathology
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
Schizophrenia
1% of the population has this
Impaired logical thought – Key symptom.
Positive symptoms – Abnormal behaviours that are gained:
Hallucinations
Delusions
Excited motor behavior
Usually acute
More likely to respond to antipsychotic medications
Negative symptoms result from lost functions:
Slow thought and speech
Emotional and social
withdrawal
Blunted affect or emotional expression
Cognitive symptoms:
Disorganized thoughts
Difficulty concentrating and following instructions
Partly heritable
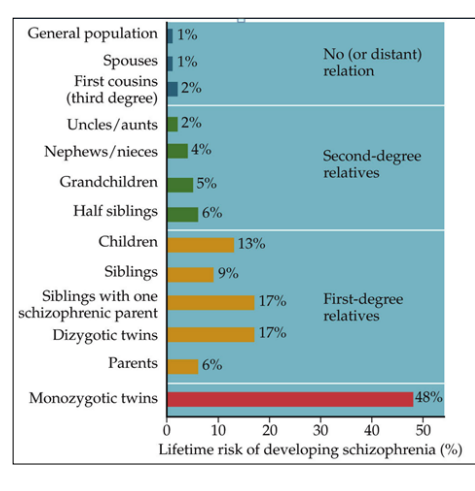
Causes of schizophrenia
Environmental exposures + genetic vulnerability
Illness occurs if a threshold is exceeded
Factors up-regulate and down-regulate gene function
Epigenetics: People with the same genome can have different outcomes.
Brain defects in schizophrenia apparently stem from environmental exposures during pregnancy
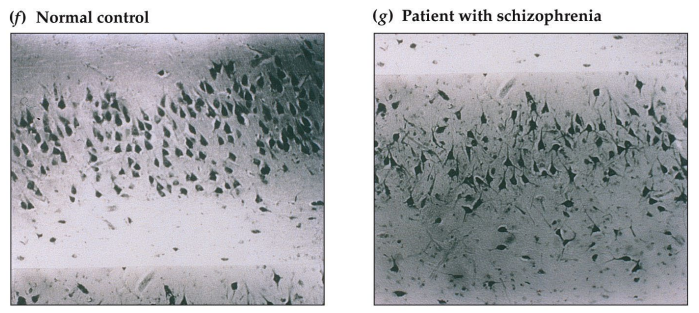
Pyramidal neurons in hippocampus are disorganized in schizophrenia.
Hippocampus and amygdala are smaller in some schizophrenics.
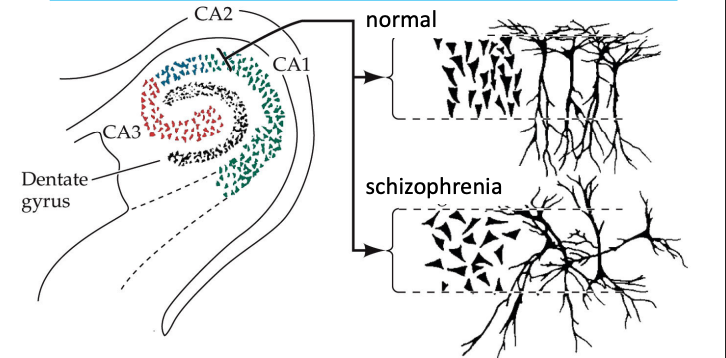
Cellular Disarray of Hippocampus in Schizophrenia
Some schizophrenics have a deficiency of Reelin: A stop signal for migrating cells in hippocampus and prefrontal areas.
Accelerated Loss of Gray Matter in Teens with Schizophrenia
‘Hypofrontality’
Underactivity of temporal and frontal lobes
Some studies show loss of gray matter and less metabolic activity in frontal and temporal lobes.
Accelerated aging and neuron loss.
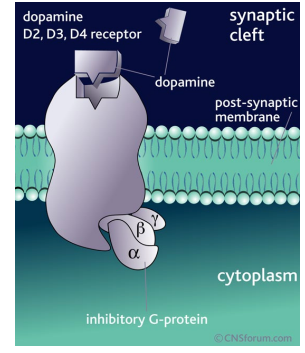
Dopamine hypothesis of schizophrenia
Results from excess synaptic dopamine or increased postsynaptic sensitivity to it.
Neuroleptics are DA antagonists
Chronic amphetamine use produces a schizophrenia-like syndrome
L-dopa treatment of Parkinson may produce psychosis
D2 levels in auditory thalamus are higher in schizophrenics
All current antipsychotic drugs modulate the function of dopamine D2 receptor.
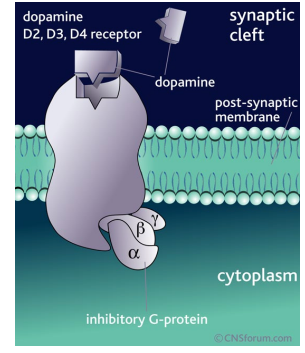
Problems with DA hypothesis
Schizophrenics have normal DA metabolite levels
Drugs block DA receptors much faster than symptoms are reduced
Positive symptoms respond better to DA blocking drugs
Some patients don’t improve on anti-dopamine drugs
Atypical neuroleptic drugs
(Risperidone & Abilify) block serotonin and D2 receptors; some increase dopamine in frontal cortex.
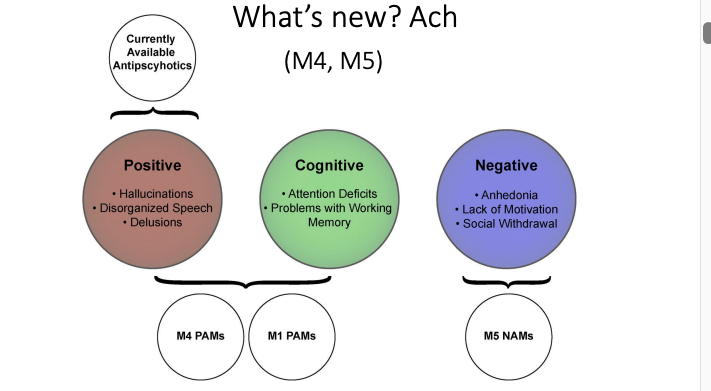
New things in the hypothesis of Schizophrenia
Ach agonists improve the Cognitive and Negative symptoms of schizophrenia.
Glutamate hypothesis of Schizophrenia
Schizophrenia is due to under-activation of glutamate receptors
PCP is an NMDA receptor antagonist; it prevents glutamate from acting normally.
Prolonged NMDA receptor under-activation → symptoms of acute schizophrenia
Atypical antipsychotics decrease glutamate reuptake by downregulating glutamate transporter gene (increasing synaptic glutamate levels)
Overactivity of Endocannabinoids & Schizophrenia
EC act on CB1 receptors → Inhibits other neurotransmitters.
EC levels are elevated in CSF of schizophrenics
Post-mortem brains show increased CB1 receptor binding.
THC in cannabis can precipitate pschosis and schizophrenia in at-risk patients. THC can worsen symptoms and prognosis in diagnosed patients.
Depression
Most common mood disorder
Sad mood
Feeling worthless or guilty
Loss of interest or pleasure in activities
Increased or decreased appetite & weight
Changes in pattern of sleep
Suicidal thoughts or plans
Normal vs Clinical depression
Normal:
Normal reaction to life events (e.g., death of loved one)
Mood described as ‘blue’
Few other symptoms
Short duration (hours-days)
Little if any impairment in functioning
Clinical
Mood described as ‘black’
Many symptoms
Long duration (weeks-months)
Significant impairment in functioning (can be debilitating)
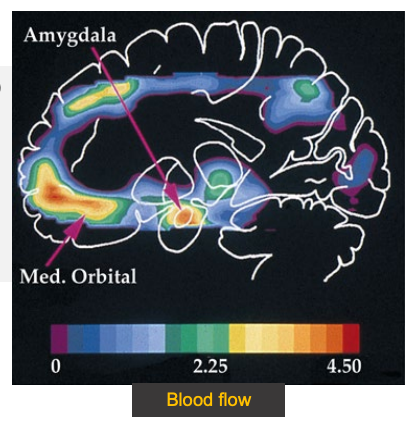
Brain activity patterns in depression
Increased activity (blood flow) of emotional orbitofrontal cortex and amygdala.
Decreased activity of areas involving attention and language.
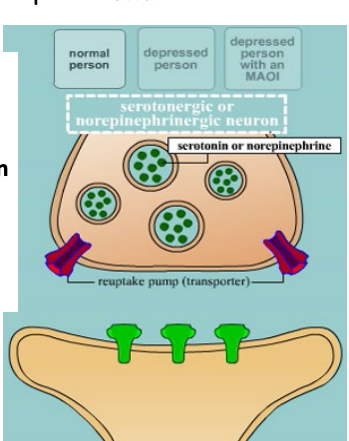
Monoamine hypothesis
Depression is due to reduced synaptic activity of norepinephrine and serotonin.
MAO inactivates monoamines.
Treatment with MAO inhibitors raises level of monoamines at the synapse and improves depression.
Reserpine reduces monoamines → can cause depression.
Antidepressants
Works via:
Inhibiting reuptake of Serotonin or Norepinephrine.
Binding to presynaptic serotonin or NE autoreceptors → enhancing neurotransmitter release
Inhibiting monoamine oxidase → Reducing neurotransmitter breakdown.
SSRI, SNRI, TCA MAO inhibitors works about the same. Equal efficacy. SSRIs are usual first choice due to less severe adverse effects and less danger with overdose.
Overactive serotonin autoreceptors
Impair serotonin release → Depression
Autoreceptor activation decreases 5HT release
Depressed patients have overactive autoreceptors
Autoreceptor function and number declines over weeks of SSRI use, increasing neuronal firing and serotonin release
A long lag time between treatment onset and reduction of symptoms
Not everyone is helped by SSRI meds
Antidepressants have ~60% response in primary care setting.
There must be other brain processes in depression.
Electroconvulsive shock therapy
Drug induced seizures alleviated depression.
ECT has similar effect → Raises monoamine levels.
ECT now used in severe depression -. suicidal ideation that requires immediate alleviation
Short-term remission rate is 87%
Long-term remission rate is 43%
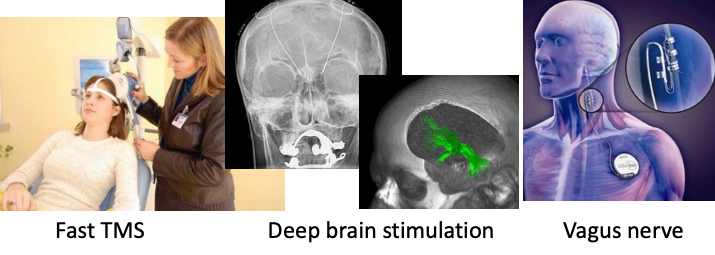
Brain stimulation treatment for affective disorders
Fast TMS (transcranial magnetic stimulation) → effects similar to ECT
Deep brain stimulation of anterior cingulate gyrus and median forebrain bundle also produces immediate effects
Stimulation of vagus nerve gradually relieves depression.
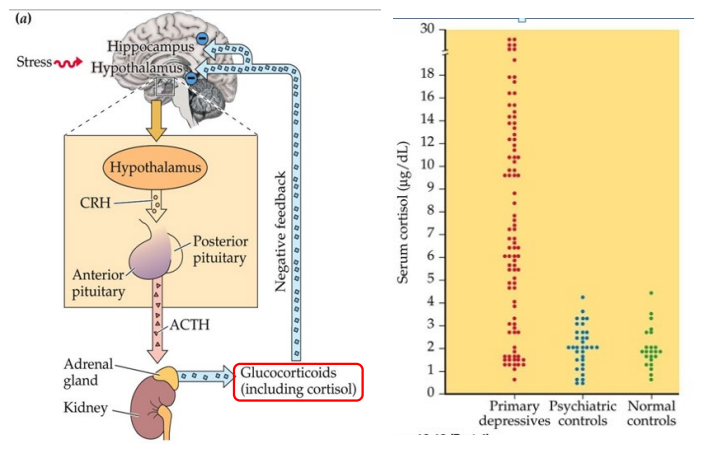
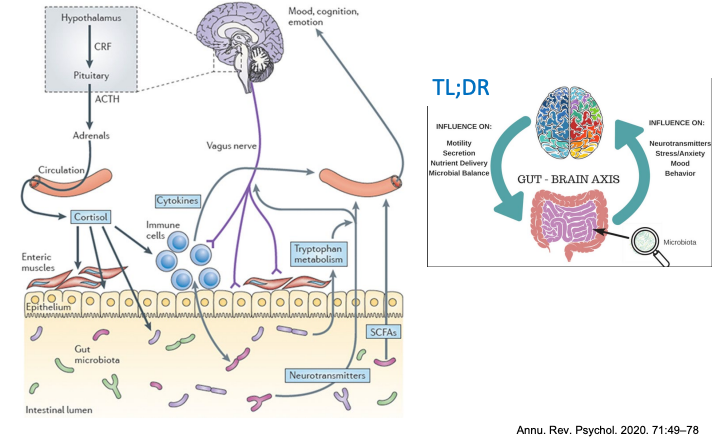
Hypothalamic-Pituitary-Adreal axis in Depression
Depression is an imbalance of the immune system, stress system, and gut microbiota.
Stress & Depression: Glutamate and ketamine
Ketamine → upsurge in glutamate, restores synaptic function

Depression and sleep
Sleep is disturbed in depression.
Deep slow-wave sleep is reduced, fragmented.
patients enter REM sleep quickly, with increased REM sleep in first half of night.
Bipolar disorder
Alternations (cycle) between depression and mania.
SIMILAR to schizophrenia.
Mania: Excess energy, confidence, grandiose thinking. Doesn’t sleep a lot, high/hyper sexual drive, drug abuse.
Bipolar psychotic symptoms:
Delusions
hallucinationsParanoia
Bizarre behaviours.

Cycling in BPD
Clock gene affected in BPD.
Cycling can be regular in some but unpredictable in others
Cycle length varies from days to months.
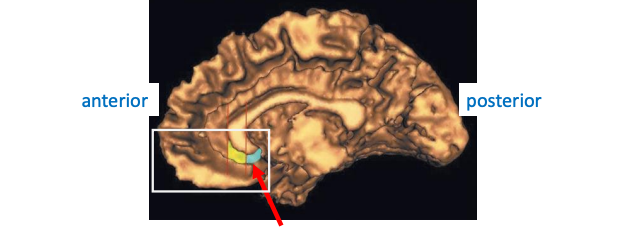
Ventral prefrontal cortex activity varies with mood state.
Ventromedial cortex is smaller in people who are depressed
Neuron number is normal, but glial cells are much reduced.
Activity increases in subgenual prefrontal cortex at start of a manic period, so it maybe a ‘bipolar switch’.

Cyclothymia
Mild form of bipolar disorder.
Patients cycle between dysthymia (mild depression) & hypomania (increased energy.)
A continuum from normal to impaired.

Anxiety Disorders
Phobic:
Intense irrational fear centered on an object/activity/situation.
Anxiety:
Panic disorder – Recurrent attacks of intese fearfulness
Generalized anxiety disorder – Persistent, excessive worry
OCD
Recurrent uncontrollable thoughts. (obsessions)
Uncontrollable need to perform an act over and over (compulsive)
Peak onset 25-44 years of age.
OCD
Antidepressants help → reducing Serotonin autoreceptor sensitivity
Antipsychotics and glutamate blocks help other patients.
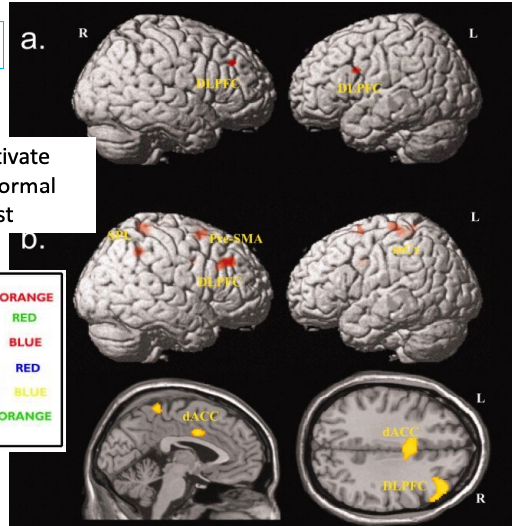
OCD patients activate DLPFC more than normal during Stroop test
Overthinking.
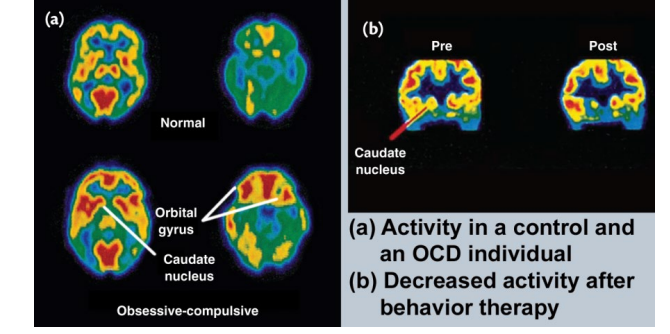
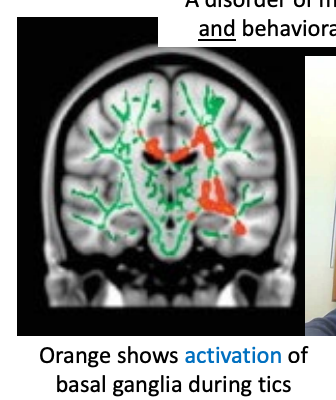
OCD patients have increased activity in orbital frontal cortex and caudate nuclei (basal ganglia)
Surgery to disconnect Orbitofrontal cortex from anterior cingulate cortex produces long lasting improvement.
Panic
Serotonin → supported by efficacy of SSRIs
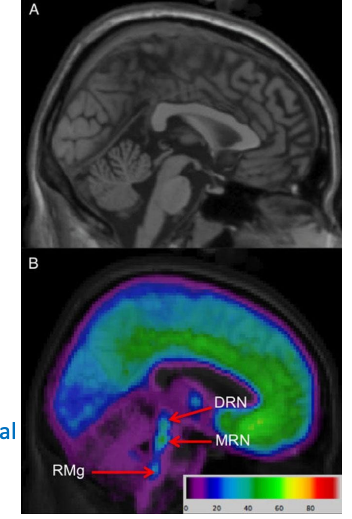
Raphe is site of 2 major nuclei.
MRN → limbic/prefrontal cortex → mediates fear/anxiety.
DRN → Prefrontal cortex, basal ganglia, PAG → Modulates cognitive/behavioural components.
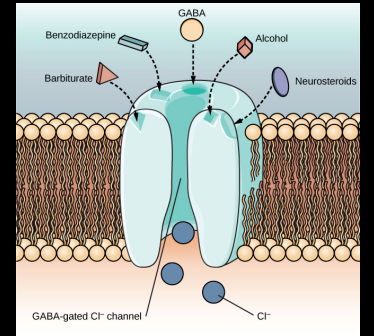
Benzodiazepines
Treat anxiety.
Bind to GABA receptors to enhance GABA inhibitory actions.
Self-medication with alcohol is very common.
Behavioural desensitization therapy works best for specific phobias.
Tourette’s syndrome is related to OCD
Disorder of motor and phonic tics & behavioural/cognitive deficits
Frontal lobotomy
Done to people with all sorts of psychiatric disorders – remission of symptoms in many patients but personality is severely affected.
Rarely performed now.
Freeman used electroshock to induce unconsciousness
Instead of drilling into the side of the skull, he got into the brain through the eye socket using a stylus like an ice pick.
Lateral cut is made by swinging the thing from side to side.
Procedure took 3-4 minutes.