NURS 344 (Health Assessment): Types of Pain
1/80
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
81 Terms
How can pain be classified?
Pain may be classified according to its duration, its localization/location, or its etiology (cause)
Acute Pain
Rapid onset, last less than 6 months, warning sign, resolves when underlying cause goes away
Chronic Pain
Persists > 3 months, may have periods of remission and exacerbation, can be difficult to locate (e.g fibromyalgia, back pain, chronic pain from cancer)
Chronic Primary vs. Secondary Pain
Primary: Chronic pain itself is considered the disease—this includes diagnoses such as fibromyalgia or back pain.
Secondary: Chronic pain results from cancer, surgery or trauma, an issue in the nervous system (neuropathic), headache or orofacial issues, visceral (organ) conditions, or musculoskeletal diseases
For pain to be considered chronic, how long does it have to persist for?
Chronic pain is 3 months at least
For pain to be considered chronic, does it have to persist consistently? How can chronic pain exhibit itself?
Chronic pain can be continuous or can be episodic with periods of remission (disease is present, but the person does not experience pain) and exacerbation (the symptoms reappear), or pain that is recurring and contains elements of both chronic and acute pain
Classifications of Pain based on Location (4)
Cutaneous: skin or subcutaneous tissue - superficial
Somatic: tendons, ligaments, bones, blood vessels, nerves; often easy to localize
Visceral: poorly localized, originates in body organs (thorax, cranium, abdomen)
Referred: pain perceived distant from its origin
Cutaneous Pain: Definition and Examples
Pain that originates from skin or subcutaneous tissue - superficial (e.g paper cuts, minor burns, and lacerations that produce sharp pain with a burning sensation)
Somatic Pain: Definition and Examples
Pain that originates from tendons, ligaments, bones, blood vessels, nerves; often easy to localize
Stimuli in tissues activates nerve receptors and produces sensation of pain
EX: Joint pain from arthritis, fractured bone, strong pressure on a bone, damage to tissue that occurs with a sprain, torn ligament
Visceral Pain: Definition and Examples
Poorly localized, originates in body organs (thorax, cranium, abdomen); nerves in internal organs are stimulated
EX: Ureteral colic, appendicitis, ulcer pain, menstrual cramps, IBS, bladder pain from cystitis, and pain related to abnormally distended, ischemic, or inflamed internal organs
Radicular Pain: Definition and Examples
Generated by stimuli at nerve root at connection to spinal nerves (e.g cervical or lumbar radiculopathy)
Cancer Pain
Little to no pain, acute, chronic, nerve, bone, tissue, referred, phantom, inflammatory
Referred Pain: Definition and Examples
Pain perceived distant from its origin
EX: Myocardial infarction pain being felt in neck, shoulder, chest, or left arm; shoulder pain after pelvic procedures
Classifications of Pain based on Etiology/Cause (4)
Nociceptive: activated by actual or threatened damage to non-neuronal tissue ("normal" pain)
Neuropathic: caused by lesion or disease of nervous system, often chronic and described as burning, tingling, electric
Intractable: persistent, detrimental to quality of life
Phantom: occurs after amputation, no identifiable physiologic or pathologic cause
Nociceptive Pain: Definition and Examples
Activated by actual or threatened damage to non-neuronal tissue ("normal" pain); nerve receptors detecting harmful stimuli
EX: Kidney stones, jammed finger, sprained ankle, pulled or strained muscle, arthritic joint pain
Neuropathic Pain: Definition and Examples
Caused by lesion or disease of nervous system, often chronic and described as burning, tingling, electric; damage or dysfunction of any level of nervous system
EX: Trigeminal neuralgia (severe facial pain), diabetic neuropathy (nerve damage from diabetes), post-stroke pain, phantom limb pain, and spinal cord injuries
What causes neuropathic pain, and where can it originate from?
The exact cause of neuropathic pain is unknown, but it can originate either peripherally (e.g., phantom leg pain) or centrally (e.g., pain from spinal cord injury)
Pain that is not classified as nociceptive or neuropathic in nature is referred to as _____________ and is addressed in the classification of chronic primary pain.
Nociplastic Pain
Intractable Pain
Pain that cannot be relieved, is incurable, or is resistant to treatment; detrimental to quality of life
EX: Severe migraine headaches, advanced cancer pain, fibromyalgia
Phantom Pain
Occurs after amputation, no identifiable physiologic or pathologic cause
Psychological Pain
Emotional or mental pain
Psychosomatic or Psychogenic Pain
Psychological pain becomes physical
Inflammatory Pain
Two aspects: inflammatory and immune responses accompanying and causing both nociceptive and neurologic pain and inflammatory pain syndromes
A patient presents with a sudden onset of severe lower back pain after lifting a heavy object. The pain lasts for a few days but improves with rest and medication. What type of pain is being described?
A) Acute
B) Chronic
C) Cutaneous
D) Somatic
E) Visceral
F) Referred
G) Nocireceptive
H) Neuropathic
A) Acute
A 65-year-old woman has experienced joint pain from osteoarthritis for the past five years. She describes it as a dull, aching discomfort that worsens with activity. What type of pain is this?
A) Acute
B) Chronic
C) Cutaneous
D) Somatic
E) Visceral
F) Referred
G) Nocireceptive
H) Neuropathic
B) Chronic
A patient who recently had a leg amputation complains of pain and itching in the missing limb. What type of pain is being described?
A) Acute
B) Chronic
C) Cutaneous
D) Somatic
E) Visceral
F) Referred
G) Phantom
G) Phantom
A patient experiences a sharp, burning pain that radiates down their leg after a herniated disc compresses the sciatic nerve. What type of pain is being described?
A) Acute
B) Chronic
C) Cutaneous
D) Somatic
E) Visceral
F) Referred
G) Nocireceptive
H) Neuropathic
H) Neuropathic
This is an example of Sciatica
A man presents with deep, aching pain in his left arm, but tests reveal he is actually experiencing a heart attack. What type of pain is this?
A) Acute
B) Chronic
C) Cutaneous
D) Somatic
E) Visceral
F) Referred
G) Nocireceptive
H) Neuropathic
F) Referred
A woman with stage IV cancer has severe pain that does not respond to standard pain management, including opioids. What type of pain is this?
A) Acute
B) Intractable
C) Cutaneous
D) Somatic
E) Visceral
F) Referred
G) Nocireceptive
B) Intractable
A patient accidentally cuts their finger while chopping vegetables and feels an immediate, sharp pain. What type of pain is this?
A) Acute
B) Intractable
C) Cutaneous
D) Somatic
E) Visceral
F) Referred
G) Nocireceptive
C) Cutaneous
A person with a broken rib reports sharp pain that worsens with deep breaths or movement. What type of pain is this?
A) Acute
B) Intractable
C) Cutaneous
D) Somatic
E) Visceral
F) Referred
G) Nocireceptive
D) Somatic (fractured or broken bone)
A patient with severe abdominal pain is diagnosed with a perforated ulcer. The pain is deep, cramping, and difficult to pinpoint. What type of pain is this?
A) Acute
B) Intractable
C) Cutaneous
D) Somatic
E) Visceral
F) Referred
G) Nocireceptive
E) Visceral
A patient with shingles describes a burning and electric shock-like pain along a specific nerve distribution. What type of pain is this?
A) Acute
B) Chronic
C) Cutaneous
D) Somatic
E) Visceral
F) Referred
G) Nocireceptive
H) Neuropathic
H) Neuropathic
A patient experiences pain from a surgical incision. The pain is localized and worsens with movement. What type of pain is being described?
A) Acute
B) Chronic
C) Cutaneous
D) Somatic
E) Visceral
F) Referred
G) Nocireceptive
H) Neuropathic
D) Somatic
A patient with gallstones reports deep, cramping pain in their abdomen, along with nausea and sweating. What type of pain is this?
A) Acute
B) Chronic
C) Cutaneous
D) Somatic
E) Visceral
F) Referred
G) Nocireceptive
H) Neuropathic
E) Visceral
A patient describes their pain as persistent and resistant to strong pain medications. Despite multiple treatments, they still experience severe, unbearable pain daily. What type of pain is this?
A) Intractable
B) Chronic
C) Cutaneous
D) Somatic
E) Visceral
F) Referred
G) Nocireceptive
H) Neuropathic
A) Intractable
A patient with a broken rib experiences dull, aching pain that worsens with movement and deep breathing. This pain is caused by stimulation of pain receptors in the tissues. What type of pain is this?
A) Intractable
B) Chronic
C) Cutaneous
D) Somatic
E) Visceral
F) Referred
G) Nocireceptive
H) Neuropathic
G) Nocireceptive
Common Responses to Pain (3)
Behavioral: voluntary body movement (withdrawal and moving away, facial grimacing and frowning, moaning)
Physiologic: involuntary body responses
Affective: mood and emotions
Behavioral Responses to Pain
Clenching teeth
Moving away from painful stimuli
Restlessness
Bent Posture
Facial grimacing, moaning, and crying
Restlessness
Protecting the painful area and refusing to move
Focused Pain Assessment: Observations for Posture, Gross motor Activities
Does patient rub or support a particular area? Make frequent position changes? Walk, pace, kneel, or assume a rolled-up position? Does patient rest a particular body part? Protect an area from stimulation? Lie quietly?
In acute pain, postural and gross motor activities are often altered; in chronic pain, the only signs of change may be postures characteristic of withdrawal.
Focused Pain Assessment: Observations for Facial Expressions
Does the patient have a pinched look?
Are there facial grimaces? Knotted brow?
Overall taut, anxious appearance? A look of fatigue is more characteristic of chronic pain.
Focused Pain Assessment: Observations for Verbal Expressions
Does the patient sigh, moan, scream, cry, or repetitively use the same words?
Physiologic Responses to Pain: 2 Divisions of ANS
Activated sympathetic (increased HR and BP, increased respiratory rate, dilated pupils, sweating, pallor (peripheral vasoconstriction), muscle tension, hormonal changes like increased cortisol and adrenaline release
Activated parasympathetic (nausea and vomiting, fainting, unconsciousness, rapid irregular breathing, decreased HR and BP, prostration)
Physiologic Responses to Pain: Sympathetic Nervous System
Increased heart rate and blood pressure
Dilated Pupils
Sweating
Pallor (peripheral vasoconstriction)
Muscle tension
Hormonal changes like increased cortisol and adrenaline release
Physiologic Responses to Pain: Parasympathetic Nervous System
Nausea and Vomiting
Fainting
Unconsciousness
Rapid and irregular breathing/respiratory rate Decreased heart rate and blood pressure
Prostration
Warm, dry skin
When there is deep and severe pain, which division of the nervous system is activated?
Contrary to common belief, the parasympathetic nervous system activates when there is deep and severe pain. In contrast, the sympathetic nervous system activates when pain is superficial and less severe.
Affective Responses to Pain (Mood and Emotions)
Exaggerated weeping and restlessness
Withdrawal
Stoicism
Anxiety/Depression
Fear/Anger
Fatigue
Hopelessness/Powerlessness
Insomnia and other sleep disturbances
Focused Pain Assessment: Signs of Anxiety to Observe
May include decreased attention span or ability to follow directions, frequent asking of questions, shifting of topics of conversation, avoidance of discussion of feelings, acting out, or somatization (physical symptoms arise from emotional or psychological distress).
Focused Pain Assessment: Questions to assess Anxiety (AFFECTIVE RESPONSES)
Do you feel anxious? Are you afraid? If so, how bad are these feelings?
Focused Pain Assessment: Questions to assess Depression (AFFECTIVE RESPONSES)
Do you feel depressed, down, or low? If so, how bad are these feelings?
Are your feelings about yourself mostly good or bad? Do you have feelings of failure?
Do you see yourself or your illness as a burden to those you care about?
Focused Pain Assessment: Observation Points for Interaction with Others
How does the patient act when in pain in the presence of others?
How does the patient respond to others when not in pain?
How do significant others and caregivers respond to the patient when the patient is in pain? When the patient is not in pain?
Focused Pain Assessment: Degree to which pain interferes with patient's life (use past performance as baseline)
Does the pain interfere with sleep? If so, to what extent? Is fatigue a major factor in the pain experience?
Is the conduct of intimate or peer relationships affected by the pain?
Is work function affected? Participation in recreational-diversional activities?
Focused Pain Assessment: Perception of Pain and Meaning to Patient (AFFECTIVE RESPONSES)
Are you worried about your illness?
Do you see any connection between your pain and the nature or course of illness? If so, how do you see them as related?
Do you find any meaning in your pain? If so, is this beneficial or detrimental to you? Are you struggling to find some meaning for your pain?
Focused Pain Assessment: Adaptive Methods Used to Cope with Pain (AFFECTIVE RESPONSES)
What do you usually do to relieve stress? How well do these things work?
What techniques do you use at home to help cope with the pain? How well have they worked?
Do you use these in the hospital? If not, why not?
Focused Pain Assessment: Outcomes (AFFECTIVE RESPONSE)
What would you like to be doing right now, this week, this month, if the pain were better controlled?
How much would the pain have to decrease (on the 0-10 scale) for you to begin to accomplish these goals? What is your pain goal (on the 0-10 scale)?
Keep in mind that NO pain may not be an option for some patients. Helping them to identify a realistic goal promotes effective pain management.
Pain Assessment (COLDSPA Acronym)
C: Character or description of the symptom
O: Onset of the symptom
L: Location of the symptom
D: Duration of the symptom
S: Severity of the symptom
P: Pattern of the symptom
A: Associated factors, such as other symptoms or suspected causes
COLDSPA: Questions to assess Character (AKA Quality)
"Can you describe how the pain feels?"
"What words would you use to describe your pain?"
COLDSPA: Questions to assess Onset
"When did it begin?"
"Can you tell me when you first noticed this pain?"
"Did the pain start suddenly or gradually?"
"What were you doing when the pain began?"
"Was there anything specific that seemed to trigger the pain?"
COLDSPA: Questions to assess Location
"Where is your pain?"
"Is your pain external or internal?"
"Does it radiate? Does it occur anywhere else?"
"Can you point to where the pain is located?"
"Are there any specific areas within the location that are more painful than others?"
Asking the patient with acute pain to point to the painful area with one finger may help to localize the pain. Patients with chronic pain may have difficulty trying to localize their pain.
COLDSPA: Questions to assess Duration
"How long have you been experiencing pain?"
"How long does a pain episode last?"
"How often does a pain episode occur?"
"Is the pain constant or does it come and go?"
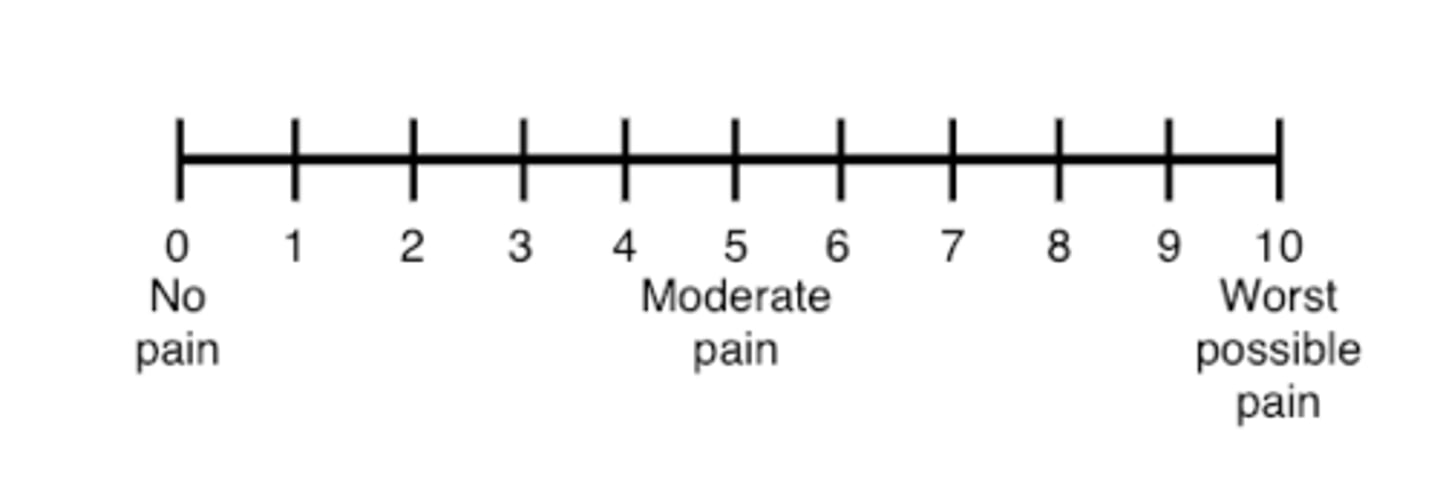
COLDSPA: Questions to assess Severity
"On a scale of 0 to 10, where 0 is no pain and 10 is the worst pain you can imagine, how would you rate your pain?"
Ask the patient to indicate the degree (amount) of pain currently experienced on the 0-10 numeric rating scale (1-3 is mild, 4-7 is moderate, 8-10 is severe)
COLDSPA: Pattern (Alleviating and Contributing Factors)
"What makes your pain better or worse?"
"Have you noticed any changes in the pain over time?"
Alleviating Factors: "What makes the pain go away or lessen?" "What methods of relief have you tried in the past? "How long were they used and were they effective?"
Contributing Factors: "How does the pain develop and progress? Has the pain changed since it first began? What makes the pain occur or increase in intensity?"
COLDSPA: Questions to assess Associated Factors
"Are there any other factors that seem to relate consistently to your pain?"
"Any other symptoms that occur just before, during, or after your pain?"
Why is important to establish a pattern related to pain?
If pattern can be identified, interventions early in a pain sequence will often be far more effective than those used after the pain is well established.
Pain Assessment Scales (MOST RELEVANT TO THIS COURSE)
0-10 Numeric Pain Rating Scale
Wong-Baker FACES Pain Rating Scale
Iowa Pain Thermometer
Pain Assessment Scales (FULL LIST)
0-10 Numeric Pain Rating Scale
Wong-Baker FACES Pain Rating Scale
Iowa Pain Thermometer
Adult Nonverbal Pain Scale (NVPS)
Behavioral Pain Scale
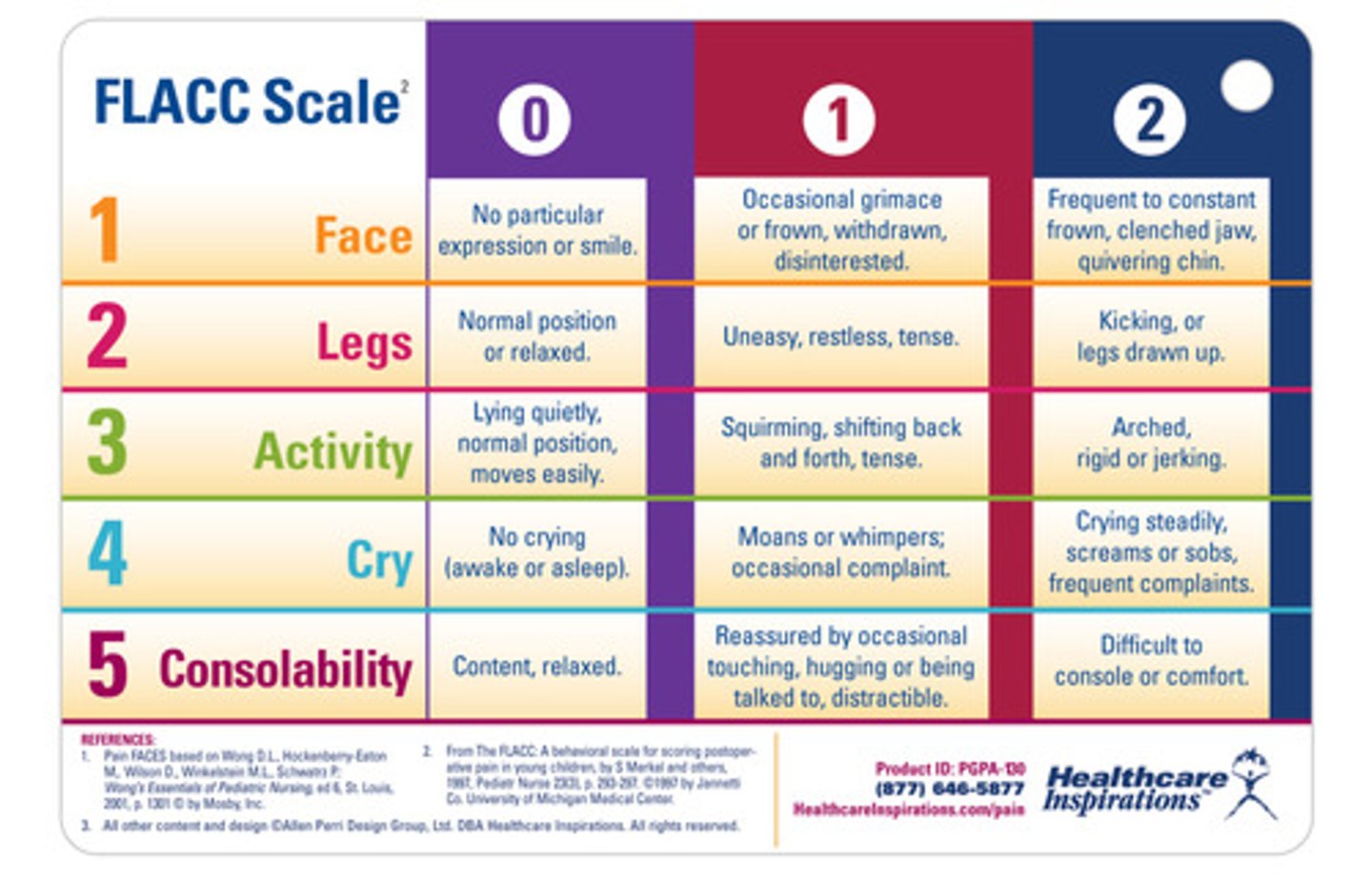
FLACC Behavioral Scale
Pain Assessment in Advanced Dementia Scale
0-10 Numeric Rating Scale
It assigns numerical values to self-reported and verbally rated pain levels, ranging from 0 (no pain) to 10 (worst possible pain)
1 to 3 is considered mild pain
4 to 6 is moderate pain
7 to 10 is considered severe pain
Used for adults and children (>9 years old) in all patient care settings who are able to use numbers to rate the intensity of their pain
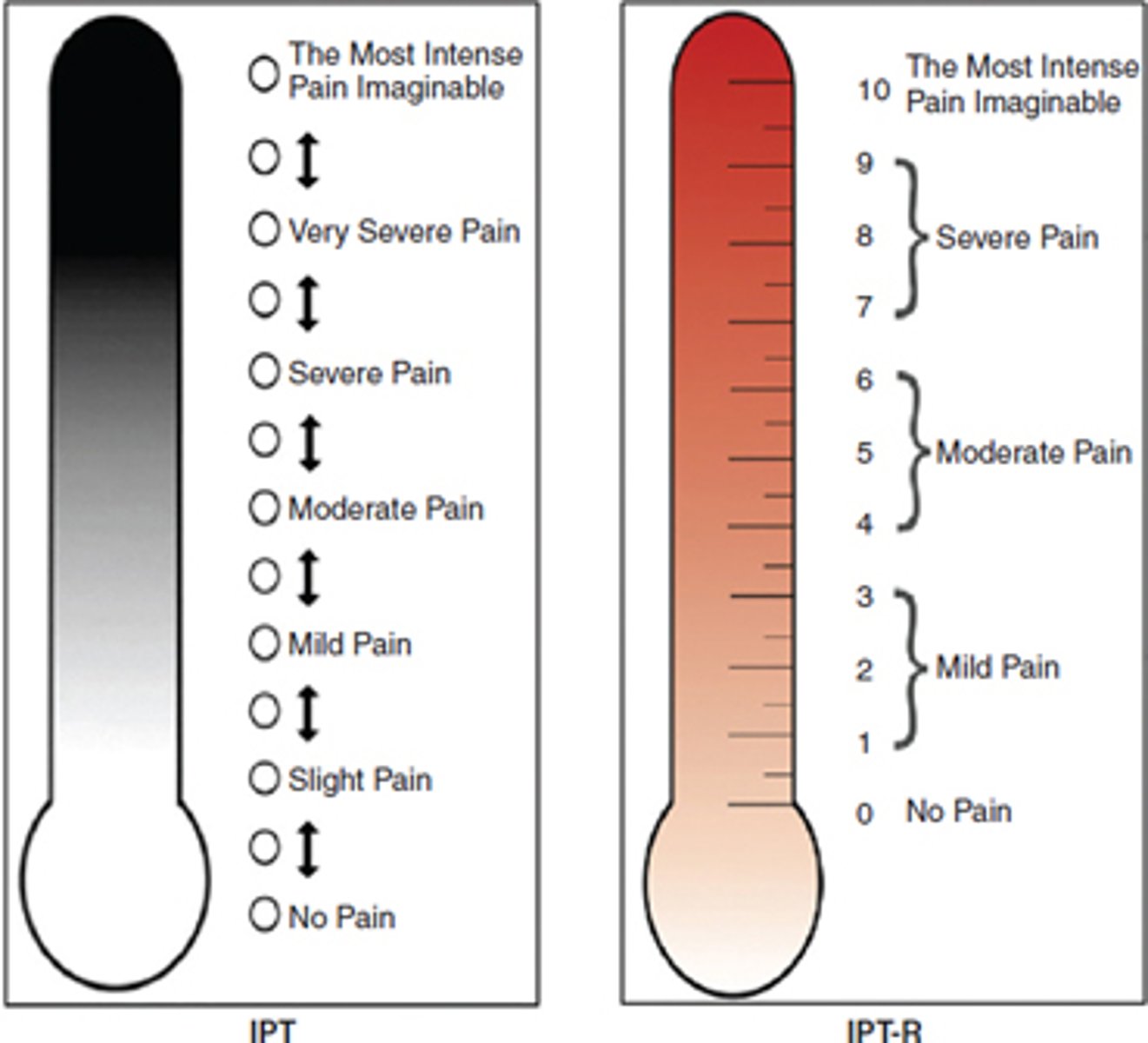
Iowa Pain Thermometer
Pain assessment tool that helps people assess and describe their pain. It's a modified Verbal Descriptor Scale (VDS) that includes a pain thermometer and a 13-point scale. The IPT is a good choice for older adults, including those with mild to moderate cognitive impairment
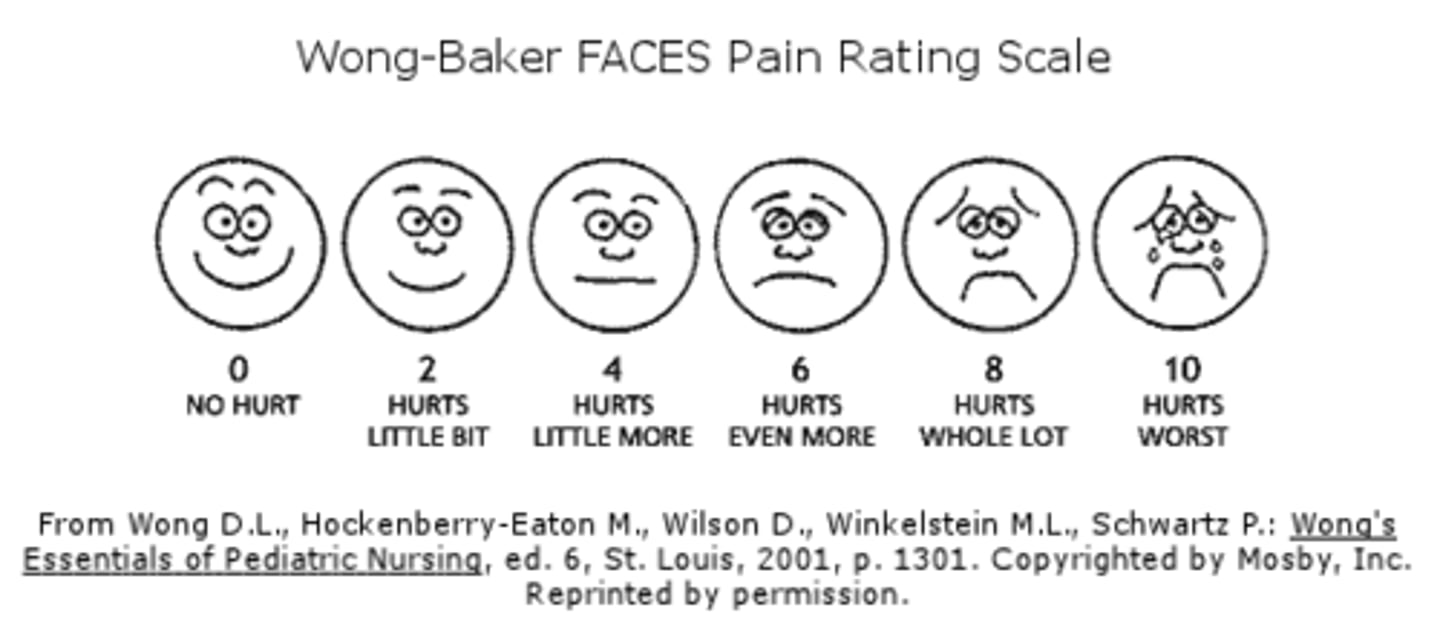
Wong-Baker FACES pain rating scale
A pain assessment tool that uses six cartoon faces to represent different levels of pain, ranging from a smiling face indicating "no hurt" to a crying face signifying "hurts worst," allowing patients, especially pediatric patients, to easily communicate their pain level by choosing the face that best matches how they feel.
Used for adults and children (>3 years old) in all patient care settings
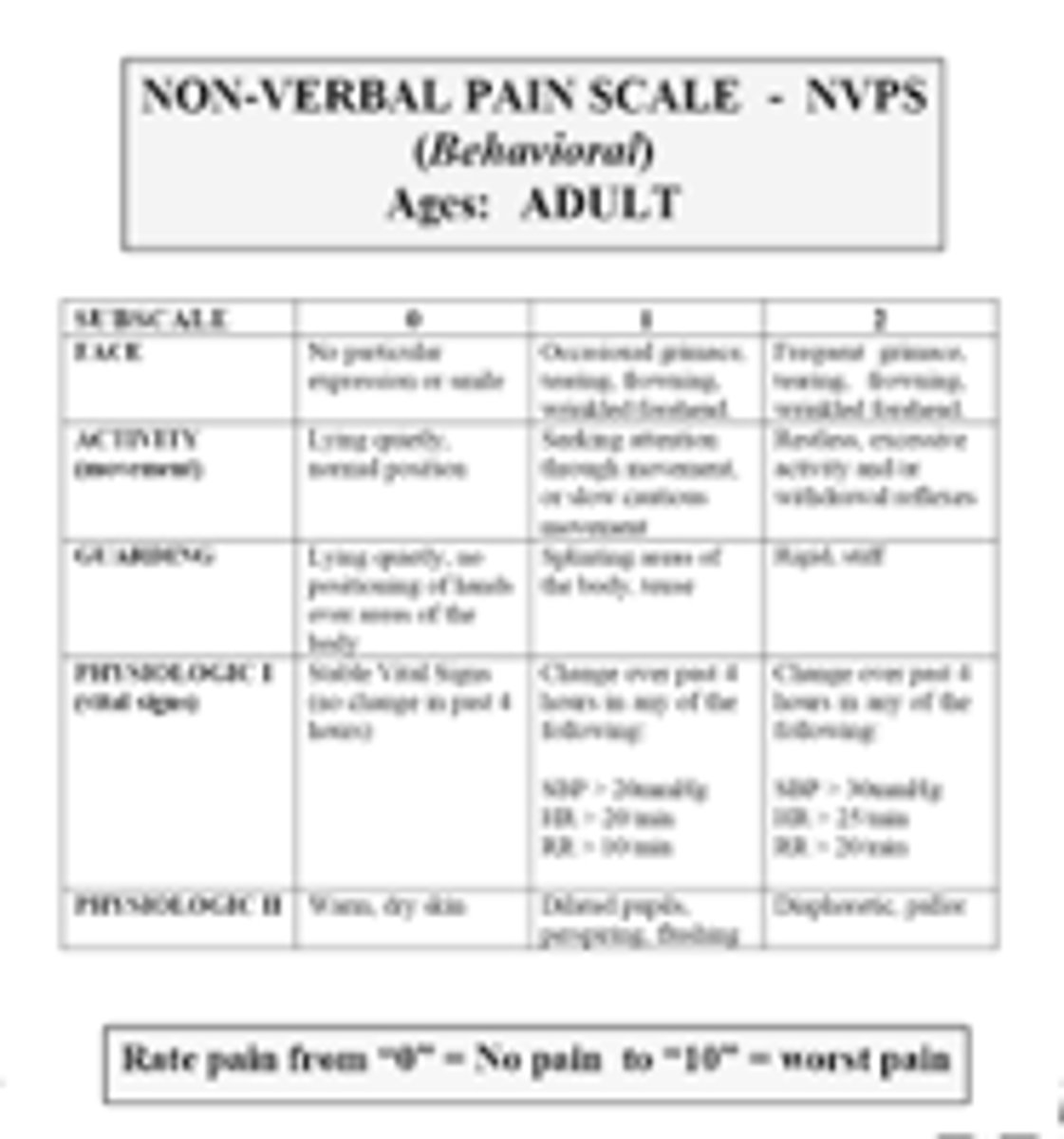
Adult Nonverbal Pain Scale (NVPS)
Pain assessment for sedated and nonresponsive patients (face, activity, guarding, VS, respiration)
Behavioral Pain Scale
Useful with intubated, critically ill patients; measurement of bodily indicators of pain; and tolerance of intubation.
FLACC Behavioral Scale
Infants and children (2 months-7 years) who are unable to validate the presence of or quantify the severity of pain
Descriptive Terms for Quality of Pain: Sharp Pain
Pain is stabbing in nature and intense.
Descriptive Terms for Quality of Pain: Dull Pain
Pain is not as intense or acute as sharp pain, possibly more annoying than painful. It is usually more diffuse than sharp pain.
Descriptive Terms for Quality of Pain: Diffuse
Pain covers a large area. Usually, the patient is unable to point to a specific area without moving the hand over a large surface, such as the entire abdomen.
Descriptive Terms for Quality of Pain: Shifting
Pain moves from one area to another, such as from the lower abdomen to the area over the stomach.
Additional Terms to Describe Quality of Pain
Other terms used to describe the quality of pain include sore, stinging, pinching, cramping, gnawing, cutting, throbbing, shooting, and vise-like pressure.
Descriptive Terms for Severity of Pain (Mild, Moderate, Severe)
These terms depend on the patient's interpretation of pain. Behavioral and physiologic signs help assess the severity of pain. On a scale of 0-10, slight pain could be described as being between 1 and 3; moderate pain, between 4 and 7; and severe pain, between 8 and 10.
Descriptive Terms for Periodicity of Pain: Continuous, Intermittent, Brief
Continuous: Pain does not stop.
Intermittent: Pain stops and starts again.
Brief or Transient: Pain is intermittent and passes quickly.
What common indicators of pain should a nurse assess for patients with cognitive impairment?
Facial expressions
Verbalizations and vocalizations
Body movements
Changes in interpersonal interactions
Changes in activity patterns or routines
Changes in mental status, such as agitation and aggression
The combination of a history of pain, observations of a patient's pain by families and caregivers, and the presence of medical diagnoses associated with pain also facilitates pain assessment in this population.
Aspects and Manifestations of Pain
Physiologic result from physical response to painful stimulus
Sensory aspect: level of severity, quality, location
Person responds with verbal and nonverbal behaviors
Cultural, Spiritual, Social contexts: Can affect person's beliefs about pain, cause, and purpose