Extensor Tendons and Flexor Tendons
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
49 Terms
Zone 1 & 2 Protocols
No passive flexion for 3 months
If Swan Neck develops place PIP joint in 35-45 degrees of flexion while maintaining DIP in extension
Weeks 1-6 (could be up to 8 weeks)
DIP in full extension (0 to +10 degrees hyper)
Monitor for signs of swan neck deformity
Week 6
DIP ROM 25-35 degrees flex - monitor for extension lag
If extension lag persists, continue splinting for two more weeks
>15 degrees
Week 7
Progress DIP flex ROM to 35-45 degrees flexion - monitor ext lag
Week 8
Progress DIP flex ROM to 45-55 degrees
Week 9
Progress to full flexion
initiate tendon glides
**5-10 degree lag normal in hypermobile joints**
Zones 3 & 4 Protocol (No Lateral Band Involvement)
Weeks 1-4 (could be up to 6 weeks)
Orthotic or plaster of paris to immobilize PIP in ext; DIP not included
Initiate DIP flexion ROM within confines of orthotic
done to centralize lateral bands and prevent ORL ligament shortening
Week 6
Wean out of PIP ext orthotic/cast
Begin gentle PIP flex ROM to 30 degrees flexion
Week 7
Advance PIP flex ROM to 40-50 degrees flex
Week 8
Advance PIP flex ROM to 60-85 degrees flex
PIP joint blocking can begin here
Week 9
Advance to full PIP flex ROM
Tendon gliding exercises
continue joint blocking
Week 10
Begin progressive strengthening
Zones 3 & 4 Protocol (Lateral Band Involvement)
Weeks 1-4 (could be up to 6 weeks)
Orthotic or plaster of paris to immobilize PIP in ext with DIP included
Initiate DIP flexion ROM at week 4
Week 6
Wean out of PIP ext orthotic/cast
Begin gentle PIP flex ROM to 30 degrees flexion; continue isolated DIP ROM
Week 7
Advance PIP flex ROM to 40-50 degrees flex
Week 8
Advance PIP flex ROM to 60-85 degrees flex
PIP joint blocking can begin here
Week 9
Advance to full PIP flex ROM
Tendon gliding exercises
continue joint blocking
Week 10
Begin progressive strengthening
Zones 3 & 4 SAM Protocol (with and without lateral band involvement)
Zone 3: Boutonnière Deformity
Week 1
Fabricate volar immobilization orthotic with PIP/DIP at 0 degrees
Fabricate ½ two volar static exercise orthoses
Orthotic #1 Lateral Band Involvement: PIP 30 degrees flexion, DIP 20 degrees flexion - done to centralize lateral bands and prevent ORL ligament shortening
Orthotic No Lateral Band Involvement #2 : PIP 0 degrees, DIP free
Remove immobilization splint hourly for 10-20 reps of AROM PIP and DIP motion using both orthoses as template
Wrist held in 20-30 deg flexion, MP at 0 deg
if lateral bands repaired, limit DIP flex to 30-35 in orthosis #1; if not injured, fully flex and extend DIP
Week 2
If no extensor lag: progress orthosis #1 Lateral Band Involvement to PIP 40-50, DIP 30-40
Remove immobilization splint hourly for 10-20 reps of AROM PIP and DIP motion using both orthoses as template
Wrist held in 30 deg flexion, MP at 0 deg
if lateral bands repaired, limit DIP flex to 30-40 in orthosis #1; if not injured, fully flex and extend DIP
Week 3
If no extensor lag: progress orthosis #1 Lateral Band Involvement to PIP 50-60, DIP 40-50
Remove immobilization splint hourly for 10-20 reps of AROM PIP and DIP motion using both orthoses as template
Wrist held in 30 deg flexion, MP at 0 deg
if lateral bands repaired, limit DIP flex to 40-50 in orthosis #1; if not injured, fully flex and extend DIP
Week 4
If no extensor lag: progress orthosis #1 Lateral Band Involvement to PIP 70-80, DIP 50-60
Remove immobilization splint hourly for 10-20 reps of AROM PIP and DIP motion using both orthoses as template
Wrist held in 30 deg flexion, MP at 0 deg
if lateral bands repaired, limit DIP flex to 50-60 in orthosis #1; if not injured, fully flex and extend DIP
Week 5
Wean from orthoses
Continue flexion without restriction
Week 6
D/C orthosis
Begin strengthening
Conservative management involves 6 weeks of immobilization
Sagittal Bands
Zone 5 injury can include this
Typically on radial side of digit
RA patients and cause of ulnar drift
Conservative Tx: Yoke orthosis; but if from RA, it may need primary repair
Affected in Zone 5; watch out for subluxation
If ulnar one is lost, EDC drops off radially
If radial one is lost, EDC drops off ulnarly
Juncturae Tendinae
Zone 6 injury
If the EDC is repaired proximal to the juncturae tendinum, all metacarpals are splinted in extension.
If the EDC is repaired distal to juncturae tendinum, only the metacarpal of the repaired tendon is splinted in extension, and the adjacent MP’s can either be splinted in slight flexion or left free
links all branches of EDC from IF - SF
When there is excursion distally, with MCP flexion of digits, it brings the one with the injury, forward and backwards with it; must keep adjacent digits to injured digit in extension to promote stability while healing
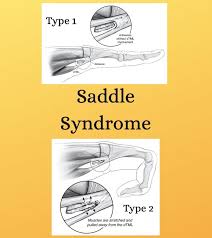
Saddle Syndrome
Differential diagnosis in Zones 4, 5, & 6
Results in stiffness to MCPs and can look like they are unable to extend
Common causes of this injury include crush injuries, a contusion from a direct blow, a fall on an outstretched hand, and torquing stresses
Two different types: both cases it involves a deep transverse metacarpal ligament on volar surface of MCP joints
Lumbricals and volar interossei split like scissors and deep transverse MCP ligament rides between the split
If lumbricals and volar interossie adhere to each other and not the dTML, when attempting intrinsic plus position, with proximal excursion of lumbricals and Volar interossei, the dTML ‘splits’ the adhesion, resulting in pain
If lumbricals adhere to volar interossei AND the dTML with distal excursion, there is pain with intrinsic minus position as the adhesion pulls away from dTML
Extensor Tendon Protocol Zones 4 (proximal aspect of P1), Zone 5, Zone 6
Week 1-3
Orthotic: place wrist in 30-45 degrees of extension and MCPs at 0 degrees of ext; PIP/DIP free
Depending on affected tendons:
If only EDC, EIP, or EDM affected, able to begin very gentle tenodesis of wrist to 40 deg ext to 10 degrees wrist extension
If wrist extensors (ECRL, ECRB) affected, begin very gentle wrist tenodesis to 40 deg ext to 20 deg wrist ext
Begin hook fisting within confines of orthotic
Wound care/edema management
Week 3
Progress MCP flexion to allow 40-50 degrees flexion (progress by 10-20 degrees each week)
Modify orthosis to place wrist in neutral
Weeks 4-6
Progress MCP flexion to 50-60 degrees flexion (progress by 10-20 degrees each week)
Begin wrist AROM within pain free arc: wrist extension, wrist flexion, wrist radial/ulnar deviation
Start weaning from splint at ~ week 5
Week 6
Begin tendon glides
progress full wrist AROM
d/c splint (if no extension lag noted)
After achieving full fist, begin progressive strengthening
Extensor Tendons Dynamic Outrigger Protocol Zones 4 (proximal aspect of P1), Zone 5, Zone 6
Cumbersome and expensive protocol due to dynamic orthotic
Orthotic outrigger holds MCPs in extension
Weeks 1-3
Forearm based dynamic digital extension splint Wrist 25-30 degrees ext, MP at 0, PIPs free
Fabricate static forearm based Splint at night, wrist at 30-40 ext, MPs at 0, PIPs free.
AROM flexion: isolated joint and tendon gliding (hook and straight fist).
Passive extension via elastic recoil of the dynamic splint. 10-20 reps hourly.
Begin active MP flexion to 30-40 degrees (via flexion block on dynamic splint).
Progress MP flexion as tolerated.
Perform wrist and digit PROM in extension and tenodesis out of splint 10 repetitions hourly
Weeks 4-6
Come out of splint for exercise
Progress MP flexion to 40-60 (week 4), 70-80 (week 5).
Initiate full fisting if not already done.
Composite wrist and finger flexion.
Active digital extension exercises out of splint.
Week 6
D/C splint. Dynamic flexion splinting PRN.
AAROM, PREs, heat and stretch, reverse putty scraping
Sagittal Band Conservative Protocol
Most commonly injured: radial side
Weeks 1-6
24/7 wear of relative motion orthosis
Injured digit +30-40 degrees MCP extension
Edema management
Pain management
US; heat & cold modalities
Week 7-8
RMO part time
MCP AAROM and AROM activities without orthotic
EDC glides
Towel walking
Tendon glides
Extensor Tendon ICAM Protocol (Zones 4-7)
ICAM = Immediate Controlled Active Motion - digit inclusion; indicated for simple EDC lacerations only
IF only - Splint IF and SP in ext
LF only - Splint LF and RF in ext
RF only - splint RF/LF only in ext
SF only - splint SF/IF only
Not allowed:
RF and SF in ext
IF and LF in ext
3-4 digits in ext
Orthotic: per evidence, only yolk splint is needed with no static wrist support; initially evidence supported use of static wrist support, but no longer supports it - test has been updated to reflect this
Weeks 1-3
Fab RMO placing involved digit in 15-20 deg extension relative to unaffected digits
Scar management
Edema management
Weeks 3-5
Complete AROM within limits of RMO
Continue scar and edema management
Week 6
D/C RMO; buddy strapping can be used during activity and wean as tolerated
begin composite fisting
begin progressive resistive exercises
Extensor Tendon Protocol Zones 7 & 8 (When just wrist extensors involved)
Weeks 1-3
Immobilize wrist in 40 degrees extension
Begin gentle wrist tenodesis - 40 degrees ext to 20 degrees ext
Wound care/edema management
Scar management with wound closure
ROM of uninvolved joints
Week 3
Progress gentle wrist ROM within pain free range
Wrist extension/flexion with open hand
Wrist extension/flexion with closed hand
Radial and ulnar deviation
Week 4
Allow full wrist ROM; monitor for ext lag
Wrist extension/flexion with open hand
Wrist extension/flexion with closed hand
Radial and ulnar deviation
Begin aggressive scar massage
Week 5
PROM of wrist if no ext lag
Week 6
wean out of orthosis
progress resistive strengthening
Thumb Zone T1 (Mallet Th) Non-Operative - No Early Active
Weeks 1-8
Orthotic - IP in ext or hyperextension - 24/7 wear
AROM of unaffected joints
Week 9
Wear splint at night and between exercise sessions
Progress IP flex AROM between 0-20 degrees - if ext lag develops, return to orthosis for an additional week
Week 10
Wear splint at night and between exercise sessions
Progress IP flex AROM between 0-40 degrees - if ext lag develops, return to orthosis for an additional week
Week 11
Wear splint at night and between exercise sessions
Progress IP flex AROM between 0-60 degrees - if ext lag develops, return to orthosis for an additional week
Week 12
D/C orthosis
Begin progressive strengthening if there is weakness - functional tasks cans support strengthening
Thumb Zone T1 (Mallet Th) Operative - No Early Active
Weeks 1-6
Orthotic - IP in ext or hyperextension - 24/7 wear
AROM of unaffected joints
wound care ; edema management
scar management
Week 7
Wear splint at night and between exercise sessions
Progress IP flex AROM between 0-20 degrees - if ext lag develops, return to orthosis for an additional week
Week 8
Wear splint at night and between exercise sessions
Progress IP flex AROM between 0-40 degrees - if ext lag develops, return to orthosis for an additional week
Week 9
D/C orthosis if no ext lag develops
Progress IP flex AROM between 0-60 degrees - if ext lag develops, return to orthosis for an additional week
Week 10
Begin progressive strengthening if there is weakness - functional tasks cans support strengthening
Thumb Extensor Tendon Zones T2, T3, T4
Week 1-3
Orthotic - hand based TH spica with CMC in slight palmer abduction, radial extension, IP and MP at 0 degrees
Edema management
Wound care/ scar management
Week 3
Begin 25-30 degrees combined AROM of IP/MP jt flexion
AROM opposition to IF
Orthotic use between exercise sessions
Scar management
Week 4
Advance patient to 45-50 degrees of combined AROM of IP/MP jt flexion - advance pt by 20 degrees
AROM opposition to LF
Orthotic use between exercise sessions
Scar management
Week 5
Advance patient to 65-70 degrees of combined AROM of IP/MP jt flexion - advance pt by 20 degrees
AROM opposition to RF
Orthotic use between exercise sessions
Scar management
Week 6
D/C orthosis
Advance patient to full flexion of IP/MP jts.
AROM opposition to SF and base of SF
Begin strengthening
Thumb Extensor Tendon Zone TV
Extensor retinaculum complicates this
Weeks 1-3
Fab volar resting pan for TH and wrist - MCP in neutral, no hyperexptension, with wrist in slight extension
Begin ROM
With the wrist, CMC, and MCP joints in extension, actively flex IP to 60 degrees and passively extend IP
With wrist in 20 degrees of flexion, CMC and MCP in neutral, perform place and holds IP extension
Week 3
Begin 25-30 degrees AROM of combined IP/MP joint flexion; monitor for ext lag
AROM opposition to IF
Orthotic use between exercise sessions
Scar management
Week 4
Advance patient to 45-50 degrees of combined AROM of IP/MP jt flexion - advance pt by 20 degrees
AROM opposition to LF
Orthotic use between exercise sessions
Scar management
Week 5
Advance patient to 65-70 degrees of combined AROM of IP/MP jt flexion - advance pt by 20 degrees
AROM opposition to RF
Orthotic use between exercise sessions
Scar management
Week 6
D/C orthosis
Advance patient to full flexion of IP/MP jts.
AROM opposition to SF and base of SF
Begin strengthening
4 types of Mallet Injuries
Sift Tissue Mallet - Type 1
Resulting for jam injury. Ex. Playing basketball and accidentally hitting DIP within flexed position resulting in stretching or tearing of the tendon
Tendon Laceration - Type 2
Sharp simple wound for closure; oftentimes conservative management
Abrasive Mallet - Type 3
Mountain bike abrasion injury; gravel or dirt can complicate things; wound care; watch for infection
Bony Mallet-Avulsive - Type 4
Test for Boutonniere Deformity
Elson’s Test: assesses for central slip and lateral band fx
If torn, DIP is rigid in extension (+)
If intact, DIP is floppy (-)
Pseudo boutonnière: flexion of the PIP but the DIP typically not involved; more likely resulting from volar plate injury.
What digit is the most common digit to have an extensor tendon injury?
Third digit; its centralized and most prominent
What percentage of the tendon needs to be lacerated for the surgeon to do a repair?
greater than 50%; if less than 50%, tendon will be able to heal as vascularity of extensor tendons is rich
Extensor tendon weakness compared to flexor tendons
3-4x/weaker
Zone 5
occurs from fight bite injury; A "fight bite" injury, also known as a clenched fist injury, occurs when a person's clenched fist strikes another person's mouth, causing a wound on the hand from the teeth.
The lumbricals originate off of the flexor digitorum profundus and attach where? And at what zone?
Extensor mechanism; zone 5 starting point into zone 3
Between what days are extensor tendons more likely to re-rupture?
7-10 days
Flexor Tendon Repair Types, Strand numbers, and suture materials
Repairs
locking - better outcomes
Grasping
# of Strands
2-8
2 = weak and does not withstand early active motion
4 = Gold standard; early active
6 = bulky-ish; early active
8 = strong, but bulky; scarring and trigger finger
Suture materials
Nylon
Epitendinous sutures - prevemts tendon from getting caught on pulley
Fiberwire = highest tensile strength
Flexor Tendon Repair Complications
PIP flexion contracture
Trigger finger: tendons cannot glide through pulley
Swan Neck: muscle imbalance
Quadriga effect: over advancement of FDP during surgical procedure, resulting in flexion lag of adjacent digits due to shortened common muscle belly
Lumbrical plus finger: rupture of FDP distal to FDS insertion
Kleinert Flexor Tendon Protocol
Orthotic:
Dorsa blocking orthotic with wrist at 45 degrees and MCPs at 40 deg flex; rubberband on affected digits for passive flexion assist
Modifications:
Palmer pulley on strap for DIP flex
Palmer pan at night for retraining D2-D5
All fingers banded for protection
Weeks 0-3 Controlled PROM
Hourly active extension against rubberband 10x
Palmer pan worn nocturnally; holding fingers against dorsal block
One handed ADLs and dressing techniques
Weeks 3-4
Adjust wrist to neutral orthosis
Hourly PROM tendon gliding
Weeks 4-6
Gentle active flexion without rubberband, every other hour; gentle active tendon glides
Week 6
D/c dorsal blocking orthosis
Static progressive as needed
Differential tendon glide
Weeks 6-8
Add light resistance
Modifications
Active extension exercises hourly without the rubberband 10-15X at 3 weeks +
Rubberband applied to all digits, not just affected one
Use of nightime volar pan to hold D2-D5 to DBS for protection
Indiana Flexor Tendon Protocol
Orthoses
DBS - FA length, wrist neutral and MCPS at 50 degrees flexion; new protocol calls for slight wrist ext
Synergistic Exercise Orthosis: Hinged wrist at 30 degrees extension block at wrist, MCPs at 60 degrees, IPs free with dorsal block in full extension
Weeks 0-4 Full time DBS use
Hourly HEP and tenodesis orthosis
15 reps of passive flex/ext to PIP jt
15 reps of passive flex/ext to DIP jt.
15 reps of passive composite flex/ext
Synergistic exercise orthosis 25x with place and hold in wrist extension with composite finger flexion
Week 4
D/c synergistic orthosis
Continue DBS
Synergistic or tenodesis to wrist every two hours
Light active finger flexion and extension
Week 5
Add FDP glide (hook fist) and FDS glide (straight fist)
Week 6
D/c DBS
Joint blocking ***do not use on SF FDP***
Week 8
Add in passive ext
Add in light resistance
Week 14
return to normal tasks and activity level as tolerated
Modified Duran Protocol
Orthotic: DBS with wrist at 20 degrees flexion and MCPs at 40-50 deg flexion; palmar pan for nocturnal use; fingers strapped into DBS at night and between exercises
Weeks 0-3 Controlled PROM
Palmer pan for nocturnal use
Differential passive tendon gliding
PIP PROM with DIP in flexion
DIP PROM with PIP in flexion
Week 4:
Synergistic wrist tenodesis begun in clinic only
Week 5:
Gentle active joint blocking AROM
FDS glides
Full fist
One handed training techniques in dressing
Week 6:
D/C DBS
Dynamic or static progressive splinting as needed
Weeks 7-8
light resistance training
return to work training and work hardening
Original duran use rubberband 4x/day weeks 0-4; tenodesis motion 4+ weeks with rubberband traction for passive flex, active ext; week 5 differential tendon gliding; 6+ weeks light active strengthening
St. John’s Flexor Tendon Protocol
Orthoses
Casting days 1-5
Day 2 - Week 2: FA based DBS
Weeks 2-6: Hand Based DBS
Week 6: D/C
Day 4 - 2 Weeks Controlled AROM (move it, don’t use it)
PROM flexion full fist
AROM composite flexion to 1/3rd fist
Active extension of IPs and MCPs within confines of orthotic
Weeks 2-4
Modify FA DBS to hand based Manchester Orthotic
Begin tenodesis within hand based orthotic
Progress active flexion to ½ to 2/3rd fist
45 degrees active wrist extension
work toward full fist by week 6
Weeks 4-8
D/C hand based orthosis and start light strengthening at week 6
Static progressive or yoke as needed
work hardening and prepare for return to work
Return to full duty work at week 8
Gail Groth Pyramid of Progressive Forces
Specifically for Zone 2, but applies to a lot of other zones
Order of pyramid progression:
Protected passive ext
place and holds
active composite fist
hook fist and straight fist
isolated joint motion
D/C splint
resistive composite fist
resisted hook and straight fist
resisted isolated joint motion
Formula:
Current weeks active DIP flexion - Previous weeks active DIP flexion divided by previous week active DIP flexion X 100 = % of change
If less than 5 degree discrepancy between active and passive
If a discrepancy is noted, you want to start measuring with Groth formula
If less than 10% of change, patient needs to be advanced up pyramid
If change is 10% or greater, level of care being provided is appropriate
Strickland Total Active Motion (TAM)
PIP Flexion AROM + DIP Flexion AROM= ___________ - any ext lags at IPs divided by 175 X 100 = percentage of progress
Excellent = 85-100%
Good = 70-84%
Fair = 50-69%
Poor = <50%
Flexor tendon work of flexion
Keep intervention under 30 neutons of force within the 6 week mark
Ideal time to start therapy after flexor tendon repair:
p/o days 3-5
When is a 4 strand repair the weakest?
Week 1
Ideal time to start strengthening with no increase in risk of rupture
8 week ideally then d/c if not scarred down
Complete Passive Protocol
Weeks 0-3 or 4
DBS
Therapy (if allowed):
PROM flex of digits
wound care
Weeks 3-6
Orthotic modified to wrist in neutral position
Take orthotic off hourly:
PROM digit flex/ext
tendon glides
wrist tenodesis
Weeks 5-6
D/c orthosis
static progressive if needed
digit blocking
gentle resistance
Manchester Splint Pros
Significantly less flexion contractures
Improvement in DIP joint flexion as it prevents adherence of FDP
Gapping Complication
Can happen with place and holds when tendon gets stuck on A4 pulley and then gaps without fully rupturing
results in rupture or weak finger
Gapping above 3mm incompatible with good results
Lalonde recommends place and holds in short arc
Quadriga Effect
tightening or scarring of FDP resulting in flexion lag of adjacent digits due to tight FDP ***Jesus****
Lumbrical Plus Finger
Occurs from a lax FDP which results in tension to the lumbrical as lumbrical insert and attach to FDP - finger would extend instead of straighten
middle finger most often affected
Cannot be addressed in therapy- must be addressed in surgery; often a result of a long tendon graft
Which flexor tendon is likely to rupture?
FDP; stuck in scar in A1 pulley
Which tendon shares a common muscle belly for LF, RF and SF?
FDP - requires splinting of all fingers as opposed to just one
How much can the A2 pulley be vented for effective tendon gliding?
30%
A patient cut his FDS/FDP over 2 years ago and is unable to flex his PIP and DIP. What surgery would he typically undergo to regain motion of the PIP and DIP jt?
Hunter rod and then grafting
Vincula
promote blood supply in flexor tendons
Made of folds of mesotendon - connective tissue sheath attaching tendon to its fibrous sheath
Vincular system exits on the dorsal surface of the tendon
Flexor Tendon Repair Tensile Strength
Day 1 p/o
greater tensile strength days 3-5
Days 3-5 p/o
least tensile strength following repair secondary to softening tendon ends
Days 5-21 p/o
tensile strength increases slowly as collagen matures and cross linking continues
transverse retinacular ligament and lateral band migration
prevents dorsal migration of the lateral bands
originates from the volar capsule of the PIP joint and inserts on the volar border of the conjoined lateral bands at the middle phalanx
Triangular ligament and lateral band migration
prevents volar migration of lateral bands.