LCD 207 Test 4 (Julianne's copy)
1/94
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
95 Terms
Larynx
Musco-cartilaginous structure
Attached superiorly to the hyoid bone, inferiorly to the trachea.
Composed of 3 paired and 3 unpaired cartilages bound by ligaments and lined with a mucous membrane. Larger are unpaired, smaller are paired.
Functions: airway protection & phonation.
Anterior to the spinal column at C4-6.
Innervated via X Vagus nerve: recurrent laryngeal branch.
Moves up and forward during swallowing.
Epiglottis
Prevents food & liquids from entering the trachea (airway protector).
Stays elevated during phonation, closes during swallowing.
Unpaired.
Sides join with arytenoid cartilages via aryepiglottic folds.
Attached to the base of the tongue.
Pointy section connects to inside of thyroid cartilage below the thyroid notch.
Innervated via X Vagus nerve: superior laryngeal branch.
Thyroid cartilage
Largest laryngeal cartilage.
Unpaired.
Allows for pitch change.
Laminae (thyroid cartilage)
Plates that make up the anterior surface of the thyroid cartilage
Thyroid angle
Midline where laminae plates meet
Thyroid notch
Superior-most point of the thyroid angle
Oblique line
Site for muscle attachment on thyroid cartilage
Laryngeal prominence
Adam’s apple.
Where the laminae meet at the inferior part of the thyroid notch.
Superior cornu
Horns of the thyroid cartilage.
Projects superiorly to articulate with the greater cornu of hyoid bone via tissue.
Not a joint.
Inferior cornu
Horns of the thyroid cartilage.
Projects downward to articulate with cricoid cartilage, forming the cricothyroid joint.
Cricoid cartilage
Most inferior unpaired cartilage (forms base of larynx).
Sits above the uppermost tracheal ring.
Unpaired.
Laminae (cricoid cartilage)
Makes up the posterior surface of the cricoid cartilage.
Facets
Points of articulation for the inferior horns of thyroid cartilage & arytenoid cartilages
Cuneiform cartilages
Paired cartilages.
Embedded within the aryepiglottic folds.
Superior & anterior to corniculate cartilages.
Provide stiffness/support to keep folds open.
Arytenoid cartilages
Paired cartilages.
Reside on posterolateral surface of cricoid cartilage.
Provide mechanical structure that allows onset/offset of voicing.
Involved in voicing & airway opening.
Each has 2 processes & 4 surfaces.
Apex (arytenoids)
Superior portion of the arytenoids.
Where corniculate cartilage is positioned.
Base (arytenoids)
Inferior surface of the arytenoids.
Concave surface is point of articulation with cricoid cartilage.
Vocal process
Medial attachment for posterior portion of vocal folds.
Project anteriorly toward thyroid notch.
Part of arytenoids.
Muscular process
Lateral attachment for muscles that help abduct/adduct vocal folds.
Part of arytenoids.
3 movements of the arytenoids
Rocking forward & backward.
Coming together medially (kissing).
Twisting/turning.
Rocking motion of arytenoids
Motion of arytenoids.
Tenses VFs, changing pitch.
Kissing/medial motion of arytenoids
Motion of arytenoids.
Adduction.
Twisting/turning motion of arytenoids
Motion of arytenoids.
Pulls vocal & muscular processes together or apart.
Corniculate cartilages
Paired cartilages.
Located on superior surface (apex) of each arytenoid.
Cricothyroid joint
Formed by articulation between cricoid + thyroid cartilages.
Allows for pitch change.
Rocking forward = pitch goes up.
Cricoarytenoid joint
Formed by articulation between cricoid + arytenoid cartilages.
Involved in vocal fold movement (abduction & adduction).
Supraglottic / laryngeal vestibule
Laryngeal cavity.
Superior to true vocal folds.
Innervated by superior laryngeal nerve.
Glottis
Laryngeal cavity.
Location of the vocal folds.
Subglottic
Laryngeal cavity.
Inferior to the vocal folds.
Innervated by the recurrent laryngeal nerve.
Superior margin = vocal folds; inferior margin = cricoid cartilage.
Aditus
The entrance to a cavity, “rim of jar”
Edge of the laryngeal vestibule.
Laryngeal ventricle
Area between the false vocal folds (ventricular folds) and true vocal folds.
Develops tension if the larynx is tense.
True vocal folds
Used for phonation.
Abduct & adduct.
Pearly white d/t tissue.
Can close through reflex actions (coughing, throat clearing).
False vocal folds / ventricular folds
Tissue that overhands the true vocal folds
Vocal ligament
Medial boundary of VFs.
End point of conus elasticus.
Embedded within lamina propriae.
Squamous epitheloum
Outermost layer of the vocal folds (white part) where blisters can occur
Lamina propria
Has gelatinous material, allowing layers to float on each other.
Located on top of true VFs.
Composed of 3 layers: superficial, intermediate, deep.
Superficial lamina propria
Lamina propria layer.
Provides flexibility.
Cushions VFs.
Intermediate lamina propria
Lamina propria layer.
Provides elasticity.
Deep lamina propria
Lamina propria layer.
Provides strength.
Pyriform sinuses
Recesses that flatten when the larynx elevates and moves forward.
Disappear during swallowing.
Conus elasticus
Membrane that stabilizes laryngeal cartilages.
Extends from the trachea to the vocal ligament.
Quadrangular membrane
Part of the pyriform sinus complex.
Provides structure for larynx.
Contributes to formation of false vocal folds.
Anterior commissure
The point where the two vocal folds meet at the front of the larynx, attaching to the thyroid cartilage
Hyoid bone
Only floating bone in the body.
Superior to the larynx, inferior to the mandible.
Greater cornu direct posteriorly, lesser cornu direct superiorly.
Serves as an attachment point for various muscles associated with the larynx:
Hyoepiglottic ligament
Ligament that connects the hyoid bone to the epiglottis
Thyrohyoid membrane
Connects the thyroid cartilage of the larynx to the hyoid bone
Upper esophageal sphincter (UES)
Adjacent to the cricoid cartilage.
Located near C7.
Control the passage of food/liquids from the pharynx into the esophagus.
Prevents the backflow of esophageal contents into the throat.
Intrinsic muscles
Responsible for controlling the movement of the vocal folds.
Contract to shorten, moving the vocal folds. The vocal folds themselves do not move; rather, they are moved by these muscles.
Categorized by functions: adductors, abductors, tensors, & relaxors.
Attach to cartilaginous structures within the larynx.
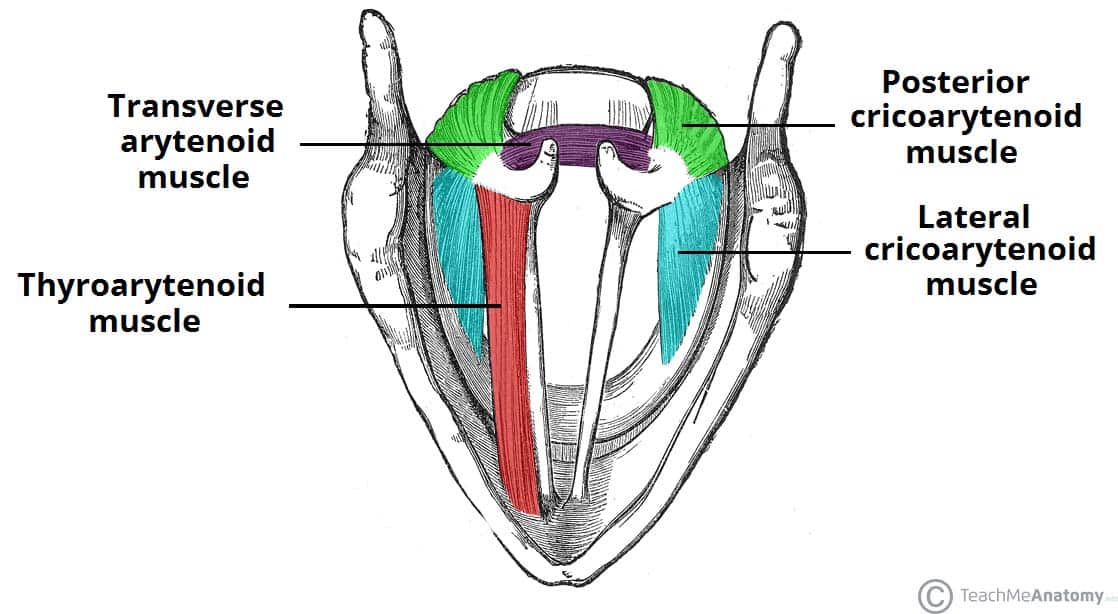
Lateral cricoarytenoid (LCA)
Intrinsic muscle — primary VF adductor.
Attached superiorly to the arytenoid muscular process and inferiorly to the lateral side of the cricoid.
Arytenoids move medially when contracted through turning motion.
X vagus, recurrent laryngeal nerve.
Transverse arytenoid
Intrinsic muscle — VF adductor.
Runs posteriorly across both arytenoids.Unpaired.
Moves arytenoids closer together during contraction.
X vagus, recurrent laryngeal nerve.
Oblique arytenoid
Intrinsic muscle — VF adductor.
Crosses over the transverse arytenoid.
Paired.
Pulls down on the epiglottis and pushes the arytenoids together (medially) during contraction.
X vagus, recurrent laryngeal nerve.
Posterior cricoarytenoid (PCA)
Intrinsic muscle — VF abductor.
Located over the lamina of the cricoid cartilage.
Attaches to the muscular process of the arytenoid.
Opens vocal folds laterally by turning the muscular process in the opposite direction of the LCA.
Loss of nerve function can prevent airway opening.
X vagus, recurrent laryngeal nerve.
Cricothyroid
Intrinsic muscle — glottal tensor.
Contracts to rock the thyroid cartilage forward, stretching and tensing the vocal folds, which increases pitch.
Composed of 2 parts:
Pars recta - inside belly.
Pars oblique - outside belly.
X vagus, superior laryngeal nerve.
Thyrovocalis
Intrinsic muscle — glottal tensor.
Part of medial thyroarytenoid *.
Attached to the arytenoid vocal process.
X vagus, recurrent laryngeal nerve.
Thyromuscularis
Intrinsic muscle — VF relaxor.
Part of the lateral thyroarytenoid *.
Attached to the arytenoid muscular process.
X vagus, recurrent laryngeal nerve.
Thyroarytenoid
Represents the true vocal folds as a whole (body).
Attaches to the arytenoids (vocal and muscular processes) and thyroid cartilage.
Composed of two parts: muscularis and vocalis.
Extrinsic muscles
Categorized into two groups based on their location relative to the hyoid bone:
Suprahyoid / hyolaryngeal elevators
Infrahyoid / hyolaryngeal depressors
Digastricus
Extrinsic muscle — suprahyoid.
Elevate hyoid bone & larynx.
Anterior belly - located in the floor of the mouth; elevates and moves larynx forward; V trigeminal nerve.
Posterior belly - elevates and moves larynx back; VII facial nerve.
Stylohyoid
Extrinsic muscle — suprahyoid.
Elevate hyoid bone & larynx.
Originates from styloid process of temporal bone.
VII facial nerve.
Mylohyoid
Extrinsic muscle — suprahyoid.
Elevate hyoid bone & larynx.
Forms the floor of the mouth.
V trigeminal.
Geniohyoid
Extrinsic muscle — suprahyoid.
Elevate hyoid bone & larynx.
Located above the mylohyoid.
XII hypoglossal & C1.
Hyoglossus & genioglossus
Extrinsic muscle — suprahyoid.
Tongue muscles that can affect laryngeal elevation, primarily in severe cases.
XII hypoglossal.
Thyropharyngeus
Extrinsic muscle — suprahyoid.
Part of the hypopharynx that attaches to the thyroid cartilage.
X vagus pharyngeal branch & IX glossopharyngeal pharyngeal branch.
Sternothyroid
Extrinsic muscle — infrahyoid.
Depresses hyoid bone & larynx.
Extends from manubrium of sternum to hyoid cartilage.
Does not attach to hyoid bone.
Located beneath the sternocleidomastoid.
C1 - C3.
Omohyoid
Extrinsic muscle — infrahyoid.
Depresses hyoid bone & larynx.
Positioned behind the sternohyoid.
Superior head - C1 innervation.
Inferior belly - C2 + C3 innervation.
Sternohyoid
Extrinsic muscle — infrahyoid.
Depresses hyoid bone & larynx.
Connects hyoid bone to the sternum.
Does not attach to the thyroid cartilage or larynx.
C1 - C3.
Thyrohyoid
Extrinsic muscle — infrahyoid.
Depresses hyoid bone & larynx.
Extends from the hyoid bone to the thyroid cartilage, without further attachment.
XII hypoglossal.
Phonation
The production of voice through action of the vocal folds in relation to the air stream. 3 stages:
Onset
Sustained phonation
Offset
Abdominal fixation
VF closure provides additional strength to the thorax during activities such as pushing and heavy weightlifting
Myoelastic-aerodynamic theory
Describes how the elastic properties of the vocal folds interact with airflow to produce sound & sustain vibration
Bernoulli effect
When air flows through a constriction, there is a decrease in pressure perpendicular to the flow and an increase in flow velocity (given a constant volume flow).
As air is sent upward and encounters closed VFs, subglottic pressure builds until it overcomes the pressure keeping the VFs closed.
This pressure explosion creates an opening, allowing air to escape and achieve atmospheric pressure.
The change in velocity creates a negative pressure gradient at the glottis, which helps to close it again.
Constriction = increased velocity; increased velocity = pressure drop.
Pitch
Perceptual counterpart of frequency.
Measured in Hertz (Hz).
# of open/close cycles per second.
Intensity
Loudness is the perceptual counterpart.
Measured in decibels (dB).
Optimal dB level is 60 - 70.
Dependent on the amplitude of VF abduction
Amplitude
The width to which the VFs are blown apart during vibration.
Affects intensity, and is dependent on subglottic pressure.
Louder sounds require more air and higher subglottic pressure, resulting in greater ______.
Quality
Whether the VFs are vibrating in sync with the same stiffness.
Conditions like laryngitis affect quality d/t inflammation and swelling, which prevents the VFs from vibrating at the same frequency.
Hoarseness
Occurs when VFs do not vibrate with the same quality, potentially resulting in a decreased pitch.
Can occur with or without infection (ex: paralyzed vocal fold).
Resonance
The tendency for a body to vibrate at a specific frequency, based upon physical characteristics of it
Spasticity
Excessive tone or stiffness, which can be associated with conditions like dystonia (abnormal tone) or upper motor neuron issues
Flaccidity
Lack of tone; associated with lower motor neuron issues
Upper motor neurons
Send signals from the brain to the spinal cord to control movement.
Damage = stiff muscles or exaggerated reflexes.
Lower motor neurons
Send signals from the spinal cord to the muscles to make them move.
Damage = muscle weakness, wasting, & twitching.
Sustained pitch
The ability to maintain a pitch over time
Habitual pitch
The pitch at which a person typically speaks
Modal/optimal pitch
Fundamental frequency (F0) that is optimal for speech
Falsetto
Upper vocal register.
VFs are stretched thin.
Pulse / glottal fry
Lower vocal register.
VFs vibrate with minimal stiffness and subglottic pressure, resulting in less air passing through the airway.
Whistle register
Pitch produced by turbulence as air is forced through a constriction
Attack
When vocal folds come together for phonation (adduct).
Facilitated by the action of laryngeal adductor muscles.
Innervated by the recurrent laryngeal nerve.
Hard glottal attack
Forceful closure of the VFs, may lead to nodules
Breathy attack
Involves air passing through the vocal folds as they close, resulting in decreased volume.
Perturbation / jitter
Quantifies cycle-by-cycle differences in vibration of the vocal folds. High perturbation is often associated with a hoarse voice
Shimmer
Examines cycle-by-cycle differences in intensity
Vocal nodules
Typically form at the midpoint of the anterior & posterior VFs.
Caused by intense collision.
Add mass & stiffness to the VFs.
Result in lower pitch & issues with full closure.
Polyps
Blister-like growths that occur after vocal abuse.
Add mass and stiffness to the vocal folds.
Two types:
Pedunculated
Sessile
Stroboscopy
A strobe light is used to visualize the opening and closure of the vocal folds