HP LEC 12: Adrenal Glands/ Tyroid and Parathyroid Glands/Pancreas & Other Endocrine glands
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
52 Terms
Structure/location of Adrenal glands
located above the kidneys
consist of an outer adrenal cortex and an inner adrenal medulla that functions as seperate glands
Adrenal Medulla
is neuroendocrine tissue and secretes epinephrine & norepinephrine in response to sympathetic neural stimulation
outer
Adrenal cortex
is glandular epithelium and secretes steriod hormones (cortisol, aldosterone, etc…) in response mostly to ACTH (released by the anterior pituitary gland) or other hormones
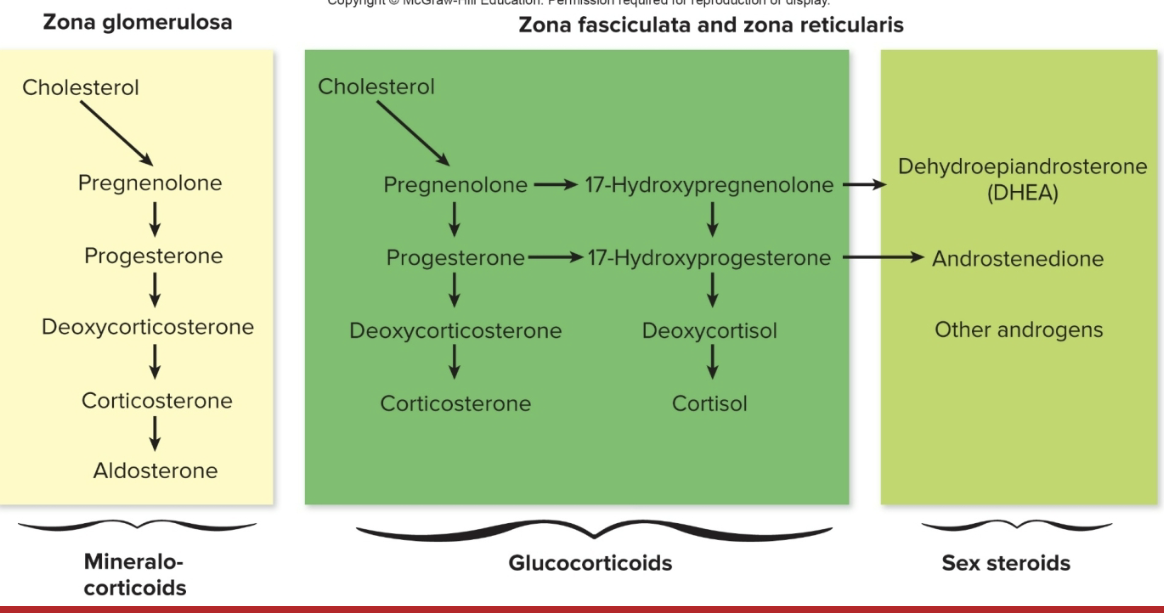
3 Layers:
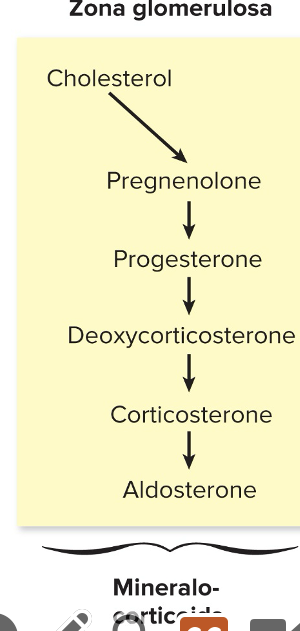
a) Zona Glomerulosa
b) Zona fasciculata
c) Zona Reticularis
Functions of the Adrenal Cortex
secretes hormones made from cholesterol; called corticosteriods or corticoids
3 Categories of corticosteroids
a) Mineralocorticoids
b) glucocorticoids
c) adrenal androgens
Mineralocorticoids
from the zona glomerulosa
regulate Na+ and K+ balance
ex: aldosterone
Glucocorticoids
from the zona fasciculata
systemic fuel metabolism
the immune system and the stress response
ex: cortisol
Adrenal Androgens
from the zona reticularis
are “weak” sex hormones that supplement those made in gonads
ex: DHEA
Functions of the Adrenal Cortex: Aldosterone
1) aldosterone is one of the most potent of the mineralcorticoids
2) plays a central role in the regulation of blood pressure mainly by acting on organs such as the kidney and the colon to INCREASE the amt of salt reabsorbed into the bloodstream and to increase the amt of K+ excreted in the urine
Aldosterone Hormone- what does aldosterone cause?
1) adrenocorticotropic hormone (ACTH) can stimulate aldosterone secretion acutely and transiently under normal conditions, but to a lesser extent that the reninangiotensin- aldosterone system
2) aldosterone causes an INCREASE in salt & water reabsorption into the bloodstream from the kidney thereby increasing the blood volume, restoring salt levels & blood pressure
Too Much Aldosterone?
causes high blood pressure
low blood levels of potassium
abnormal increase in blood volume
Not enough aldosterone
causes Addison’s disease
in addisons diease there is a general loss of adrenal function resulting in LOW blood pressure, lethargy, and in increase in postassium levels in the blood
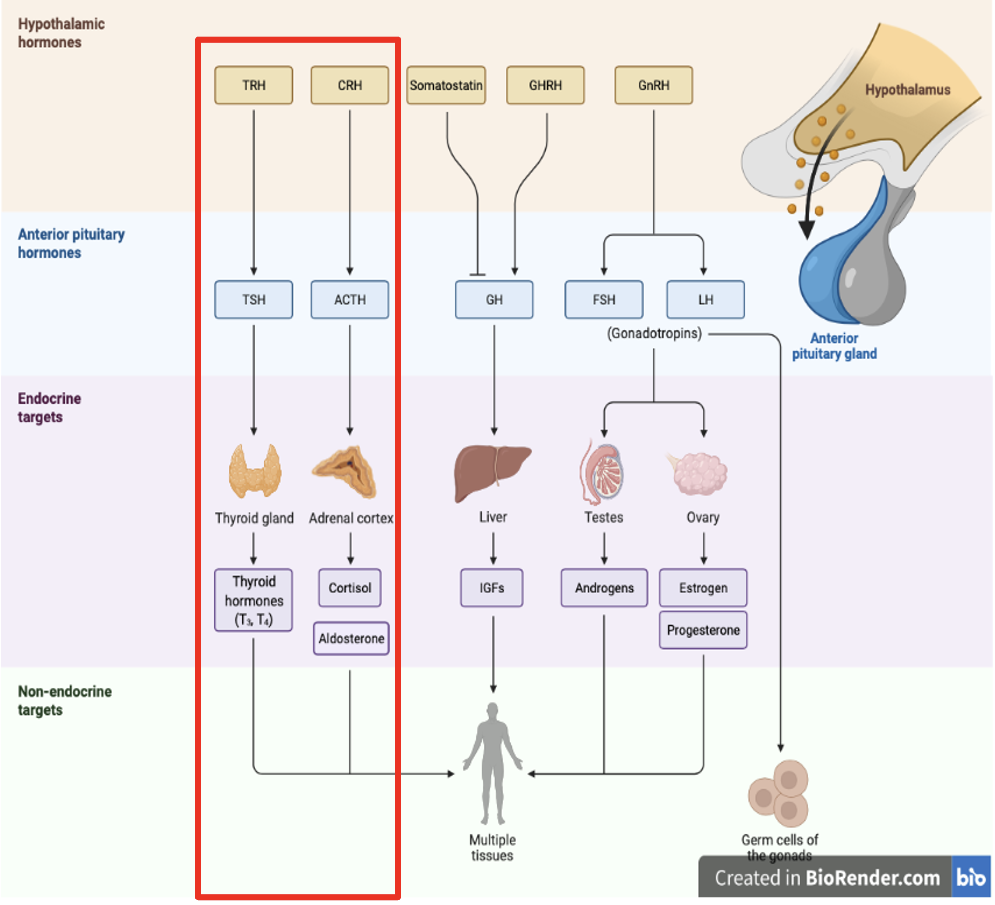
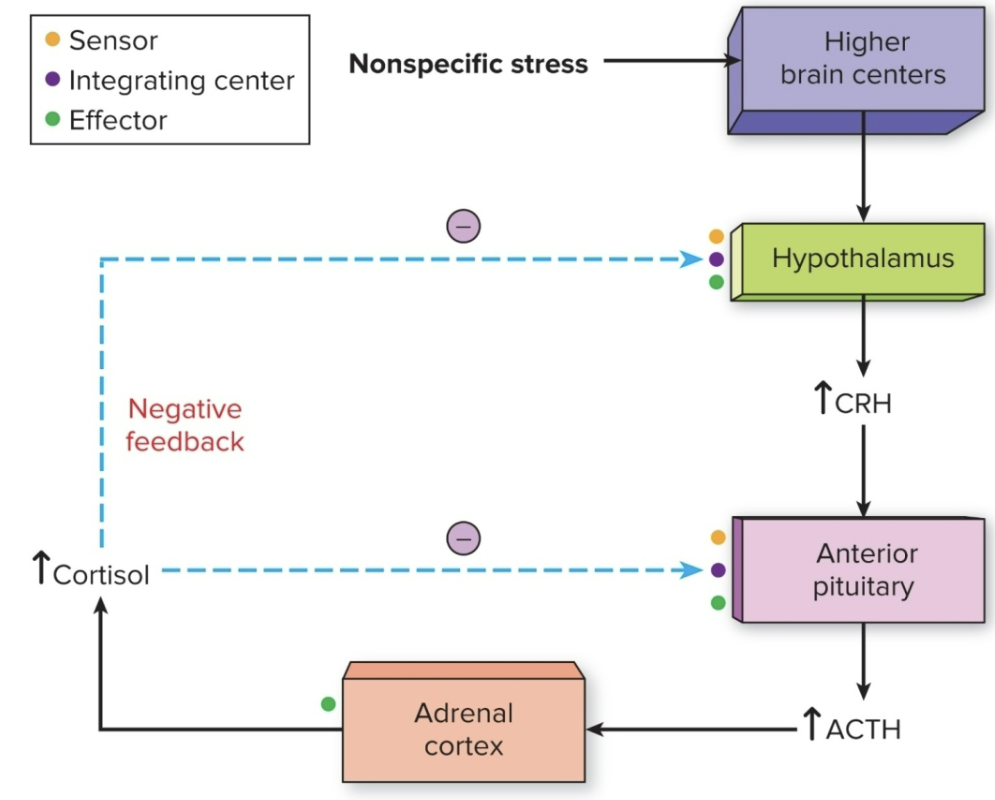
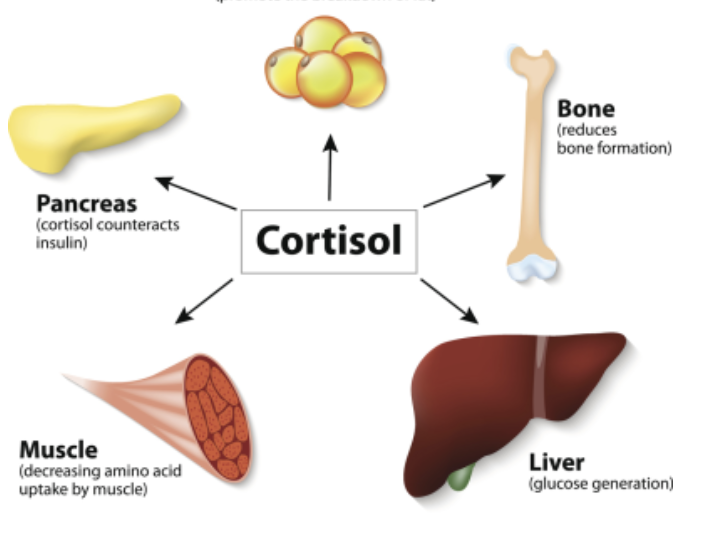
Functions of the Adrenal Cortex: Cortisol
cortisol production is regulated by hypothalamus & pituitary gland (hypothalamic pituitary-adrenal axis)
a) corticotropin releasing hormone (CRH)
b) adrenocorticotropic releasing hormone (ACTH)
Cortisol actions (7)
almost every cell contains receptors for cortisol, so it can have lots of different actions depending on which cell its acting upon
controlling the body blood sugar levels
regulating metabolism
acting as an anti-inflammatory
influencing memory formation
controlling salt & water balance
influencing blood pressure
helping development of the fetus
What are exogenous glucocorticoids used for?
exogenous glucocorticoids are used medically to suppress immune response & inhibit inflammation; can have many negative side effects
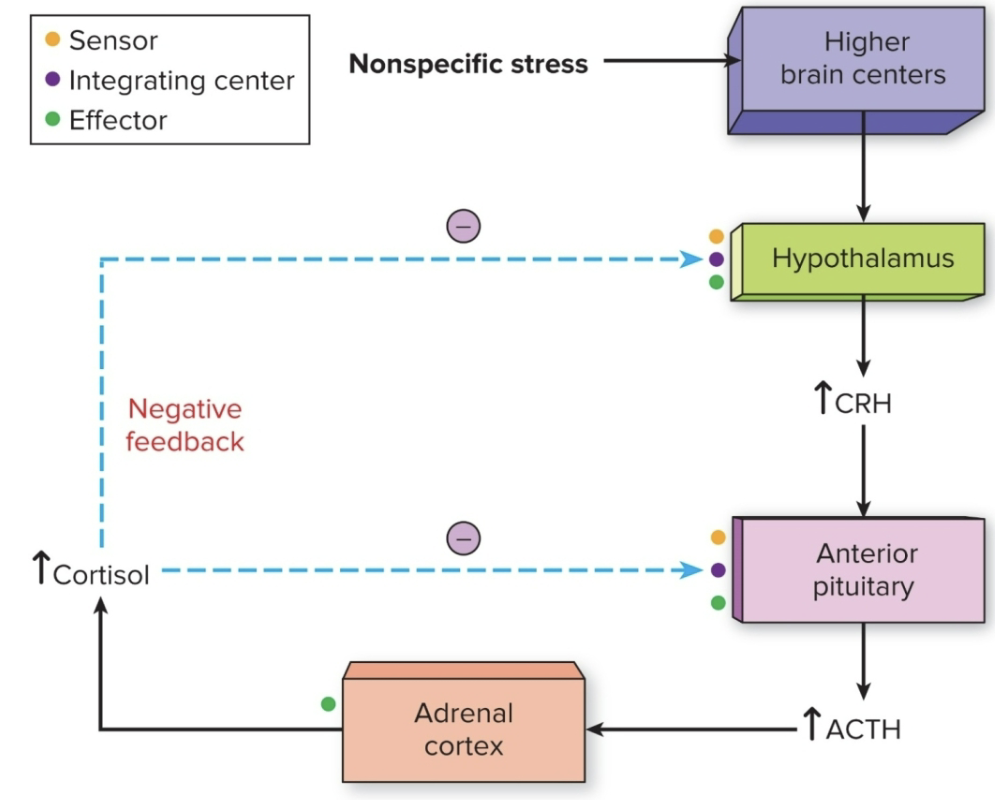
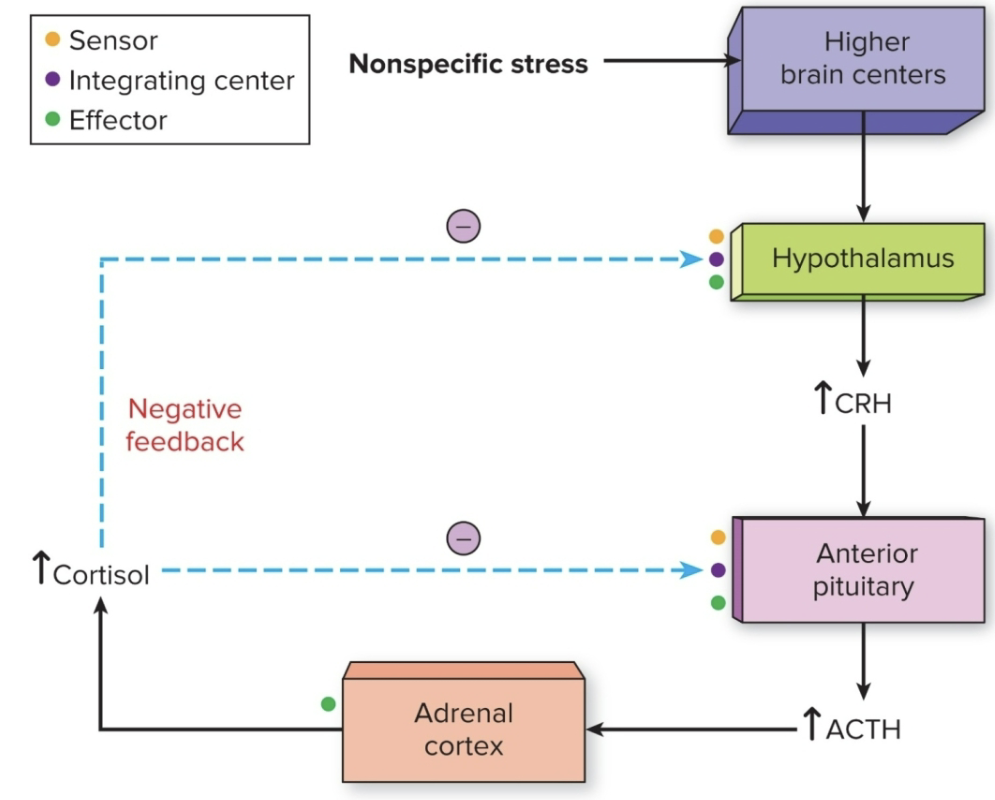
Stress & the Adrenal Gland (how does the body respond to stress?)
stress INcreases secretion of ACTH, which results in increased cortisol release
the stress hormone are glucocorticoids, but also norepinephrine & epinephrine (fight or flight)
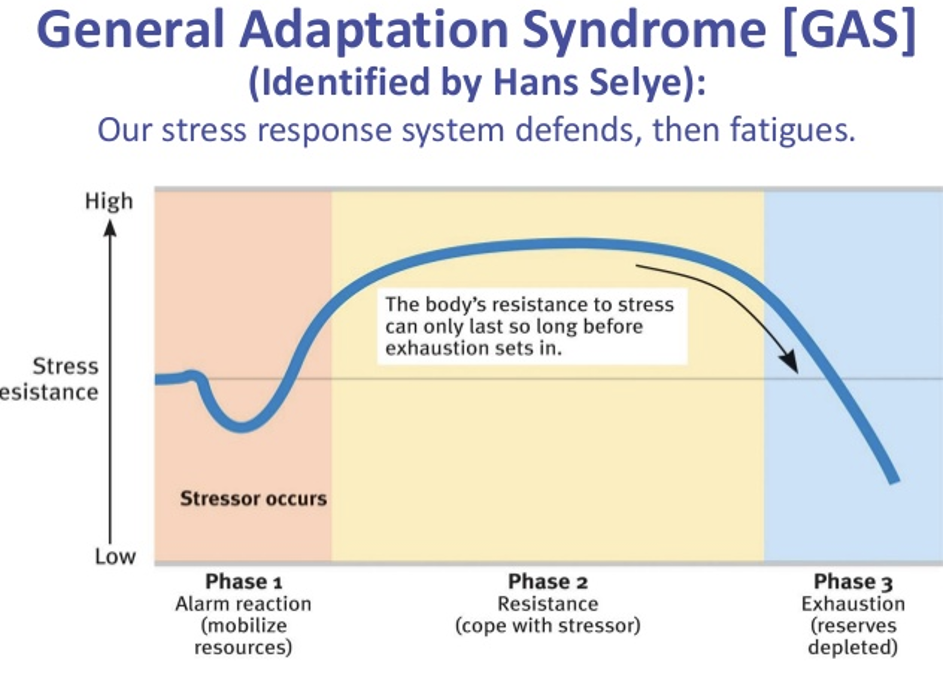
Body responds to stress by the general adaptation syndrome (GAS)
Stages of GAS (general adaptation syndrome)
Alarm Reaction
Stage of Resistance
Stage of Exhaustion
Stages of Gas: Alarm Rxn
1) Alarm Rxn: activates the adrenal glands- this natural rxn prepares you to either flee or protect yourself in dangerous situations
heart rate increases
adrenal medulla releases cortisol, you receive a boost of adrenaline (released by adrenal cortex)- increases energy
fight or flight response occurs in the alarm rxn stage
Stages of Gas: Stage of Resistance
2) readjustments in response
body begins to repair itself
it releases a lower amt of cortisol
heart rate and blood pressure begin to normalize
However, some stressful situations continue for extended periods of time, your body remains on high alert, it eventually adapts and learns how to live with a higher stress level
Stages of Gas: Stage of Exhaustion
3) stage of exhaustion:
may lead to sickness or death
this stage is the result of prolonged or chronic stress
Stress & the adrenal gland- (what does Chronic Stress lead to? what can cortisol act on?)
Chronic stress leads to an INcreased risk of illness
cortisol may act on higher brain regions, contributing to depression, anxiety, memory
By stimulating the liver to release glucose, insulin receptors may become resistant, making it harder to treat people with diabetes
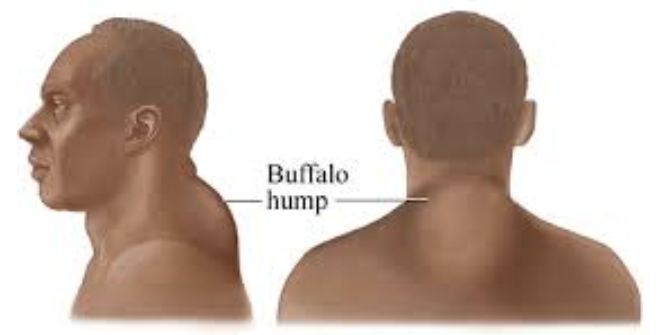
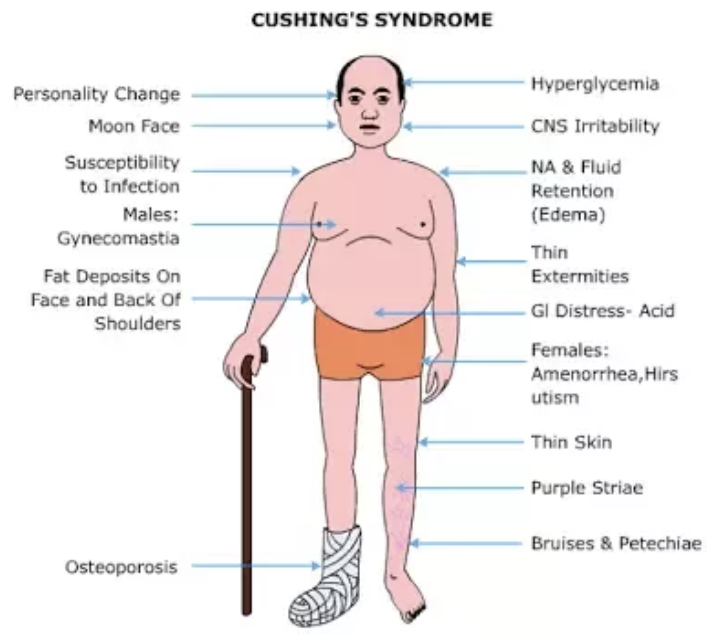
Cushing’s Syndrome (what does it result from? what does it cause?)
resulting from chronically HIGH levels of glucocorticoids (stress hormone)
it causes lipolysis & a redistribution of fat that can produce a “buffalo hump” (a fatty deposit between the shoulders and below the back of the neck), a '“moon face” (round) and other symptoms
When does Cushing’s Syndrome commonly occur?
commonly occurs when a person takes sustained high does of glucocorticoid medicine, but it can be produced by either:
1) a pituitary tumor that secretes excessive ACTH
2) a benign tumor of the adrenal that secretes excessive cortisol without requiring ACTH stimulation
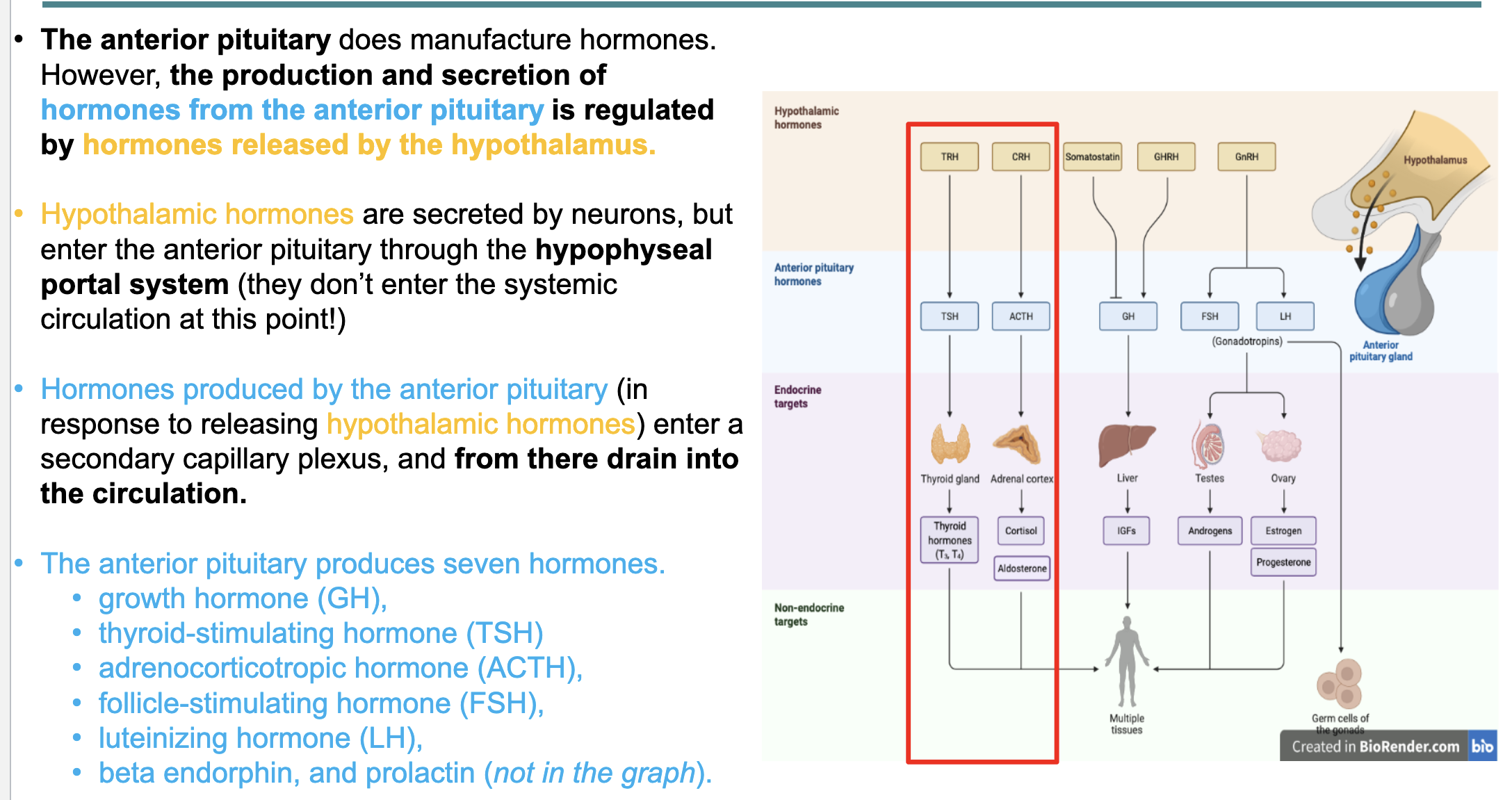
hypothalamus and anterior pituitary gland hormone review
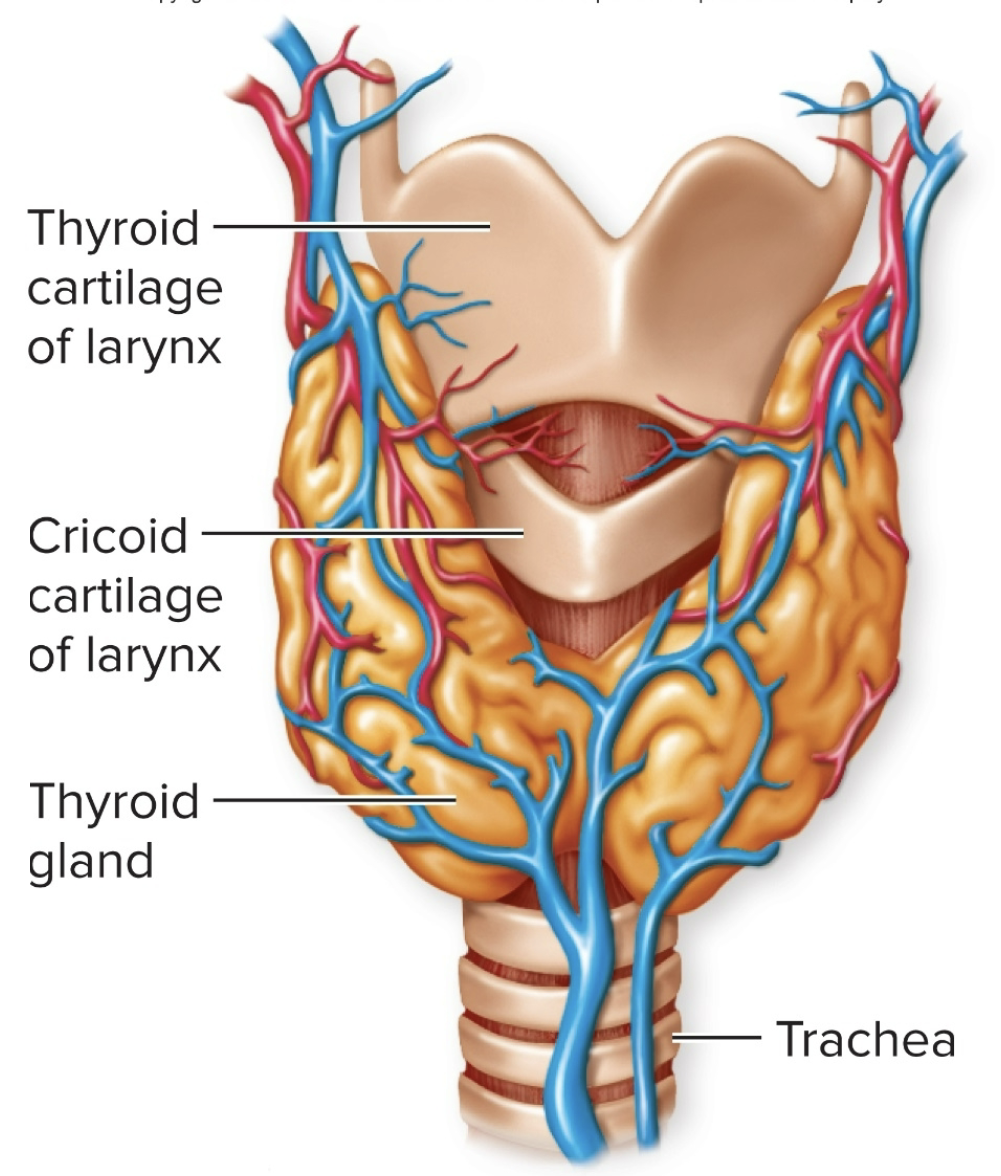
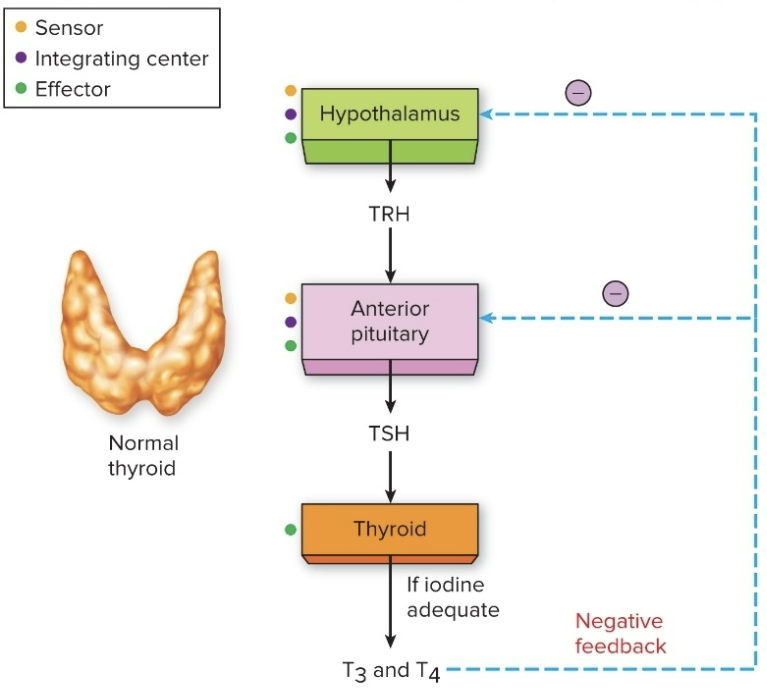
Thyroid Glands (location, structure)
located just below the larynx
has two lobes on either side of the trachea, connected by the isthmus
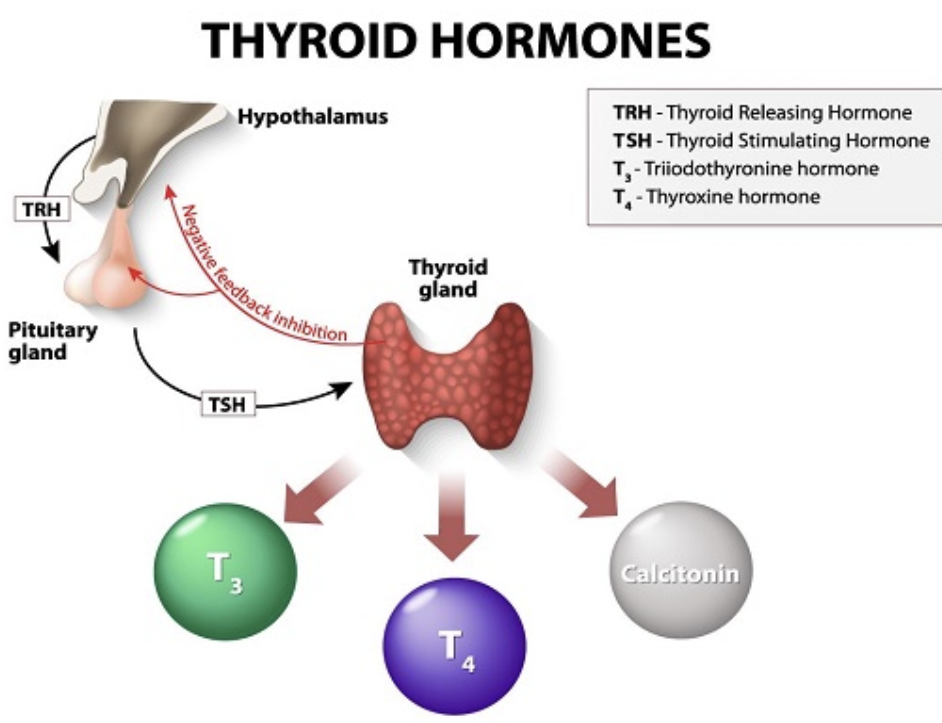
hypothalamus signals the pituitary glands which signals the thyroid glands
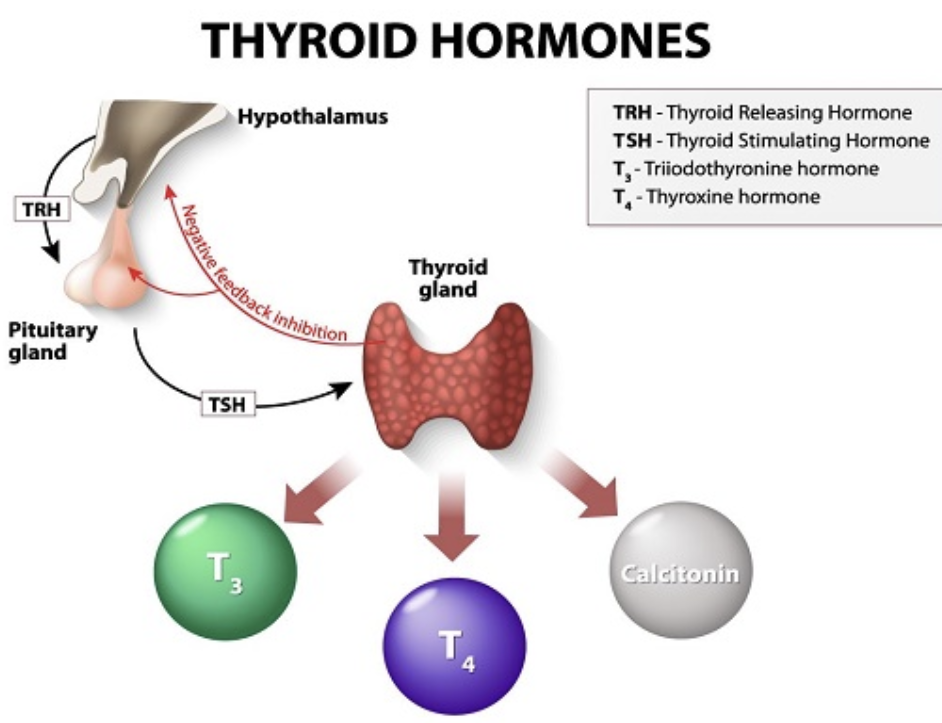
Thyroid Hormones (4)
TRH- thyroid releasing hormone
TSH- thyroid stimulating hormone
T3- Triiodothyronine hormone
T4- Thyroxine hormone
Thyroid Gland consists of: T3, T4, and calcitonin
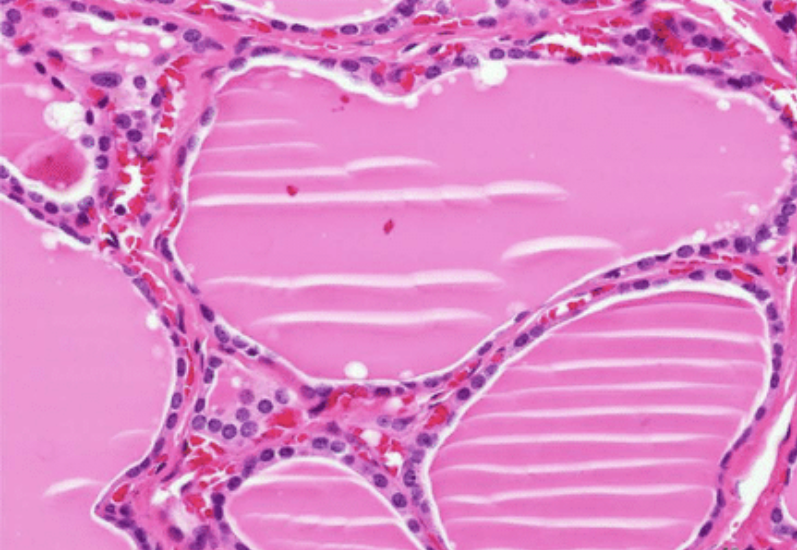
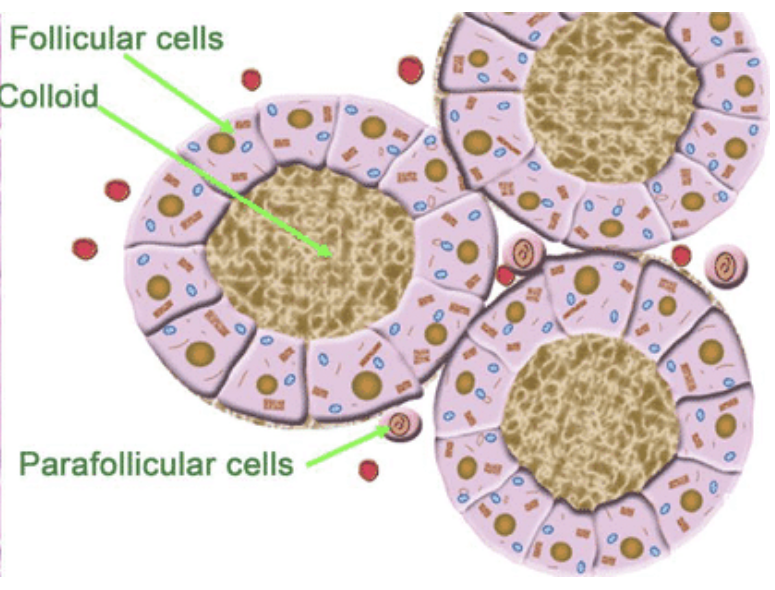
Photomicrograph of the Thyroid Gland
consists of hollow spaces called thyroid follicles lined with simple cuboidal epithelium composed of follicular cells that produce thyroxine (T4) and Triiodothyronine (T3)
outside of the follicles are parafollicular cells that secrete calcitonin
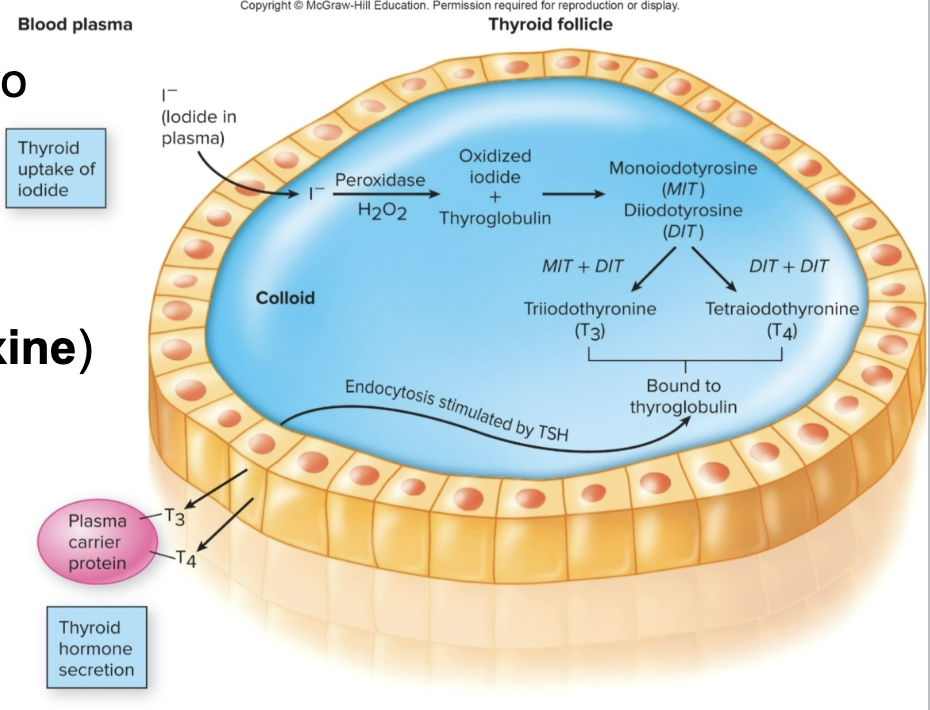
Production & Action of Thyroid Hormone- pt 1
1) Thyroglobulin (precursor of T3 & T4) is made by the follicular cells
a) thyroid follicles- actively accumulate iodide (I-) and secrete it into the colloid; the enzyme thyroid peroxidase catalyzes the oxidation of iodide ions to molecular iodine (I2 oxidized iodide)
Production & Action of Thyroid Hormone- pt 2
b) the iodine is attached to tyrosine within the thyroglobulin
1) one iodine produces monoidotyrosine (MIT)
2) two iodine produces diiodotyrosine (DIT)
enzymes within the colloid attach MIT & DIT together
DIT +DIT= T4 (tetraiodothyronine/ thyroxine)
DIT +MIT= T3 (triiodothyronine)
Production & Action of Thyroid Hormone- pt 3
c) these are still bound to thyroglobulin
they dissociate from thyroglobulin when the thyroid gland is stimulated by TSH & secreted into the blood
Action of Thyroid Hormone (4)
stimulates protein synthesis
promotes maturation of the nervous system
increases rates of cellular respiration
elevates basal metabolic rate
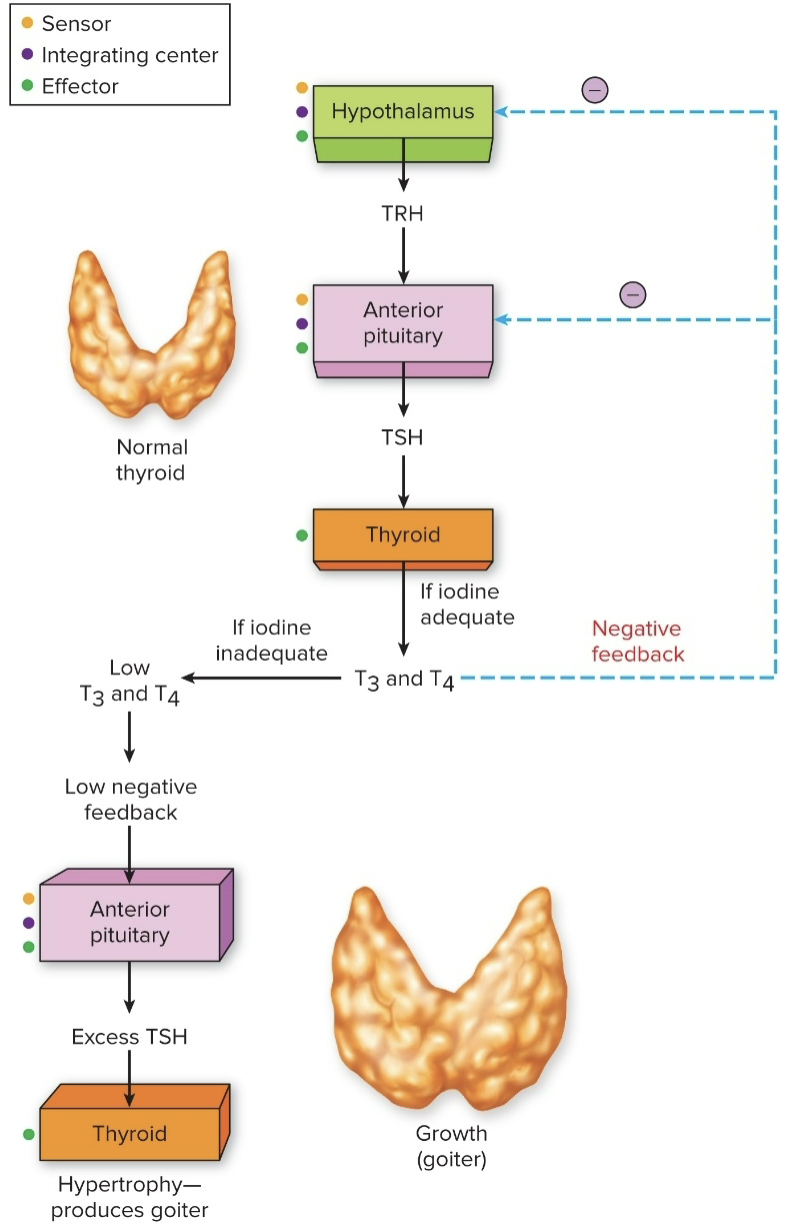
How Iodine Deficiency Causes a Goiter (enlargement of the thyroid gland in the neck)- what can it lead too
1) iodine deficiency (low) leads to overstimulation of the thyroid gland (no negative feedback on pituitary gland) and growth of a goiter (endemic goiter)
2) can also lead to hypothyroidsm: LOW metabolic rates, weight gain, lethargy, poor adaptation to cold stress, & myxedema (accumulation of fluids in subcutaneous connective tissues)
Other causes of hypothyroidism (4)
Pituitary disorder
Pregnancy
Autoimmune diease (hasimoto)
Medication (lithium)
What disease does hypothyroidism cause?
Graves disease is an autoimmune disorder which autoantibodies bind to the receptors for TSH on thyroid gland follicular cells
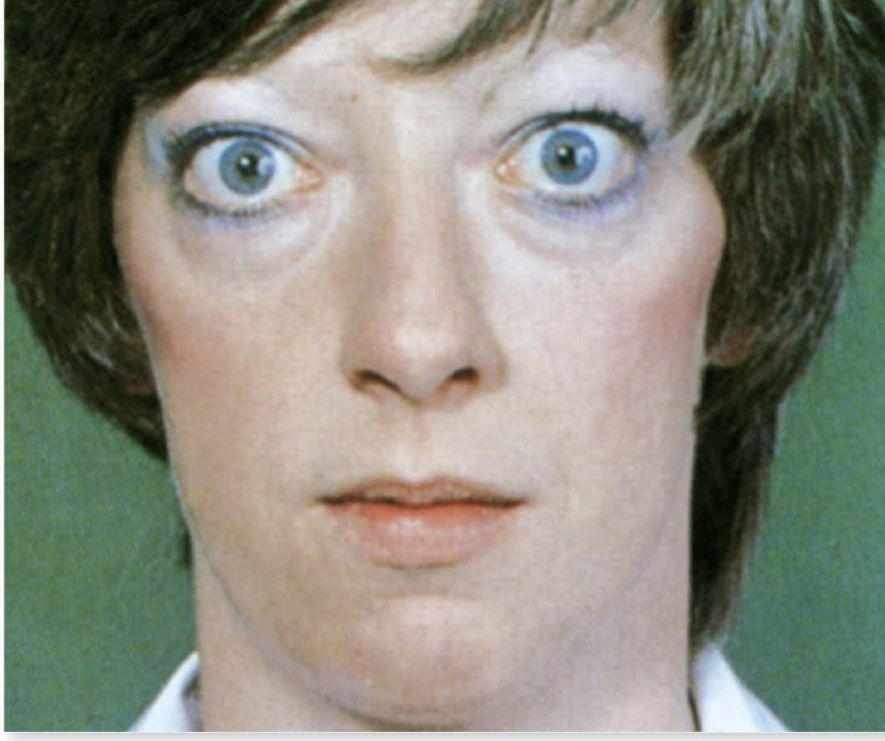
What does graves disease cause
a) this causes growth of the thyroid ( a goiter) and stimulates the excessive secretion of thyroid hormones
b) although TSH levels are very low bc of negative feedback, the thyroid continues to be stimulated by the thryotropin receptor antibodes to grow & secrete thyroxine
c) the hyperthyroidism produces symptoms such as sensitivity to heat, palpitations and others
d) graves disease is the most common cause of hyperthyroidism and is 5 to 10 times more common in women than men
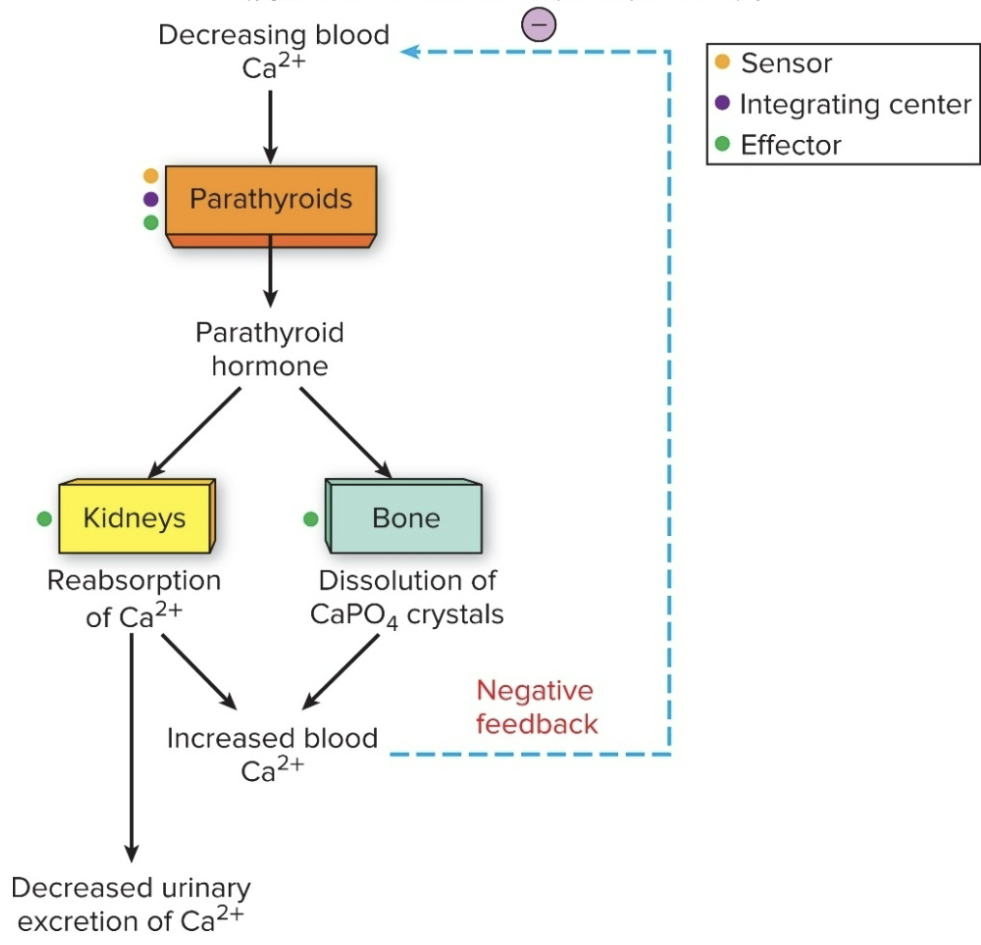
Parathyroid Glands (what is it, location?)
generally 4 glands embedded in the BACK of the thyroid gland
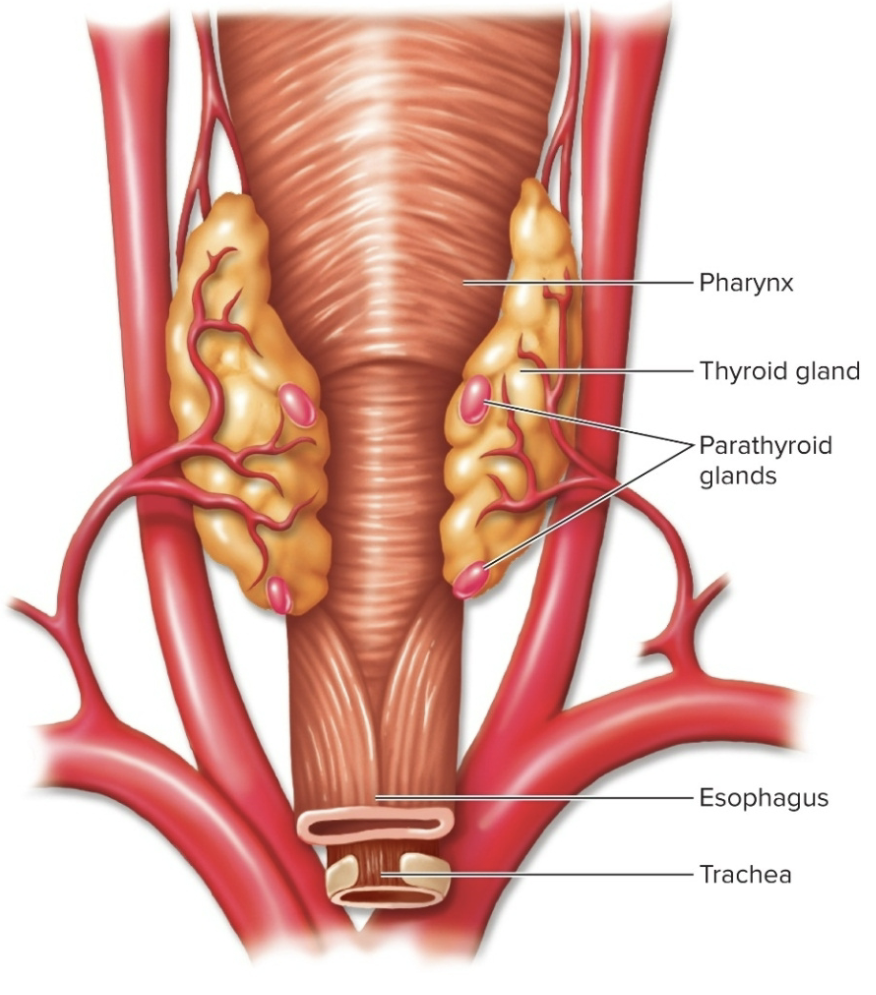
Parathyroid Glands (function)
secretes parathyroid hormone (PTH)
PTH promotes a RISE in blood calcium by acting on bones, kidneys, and intestine
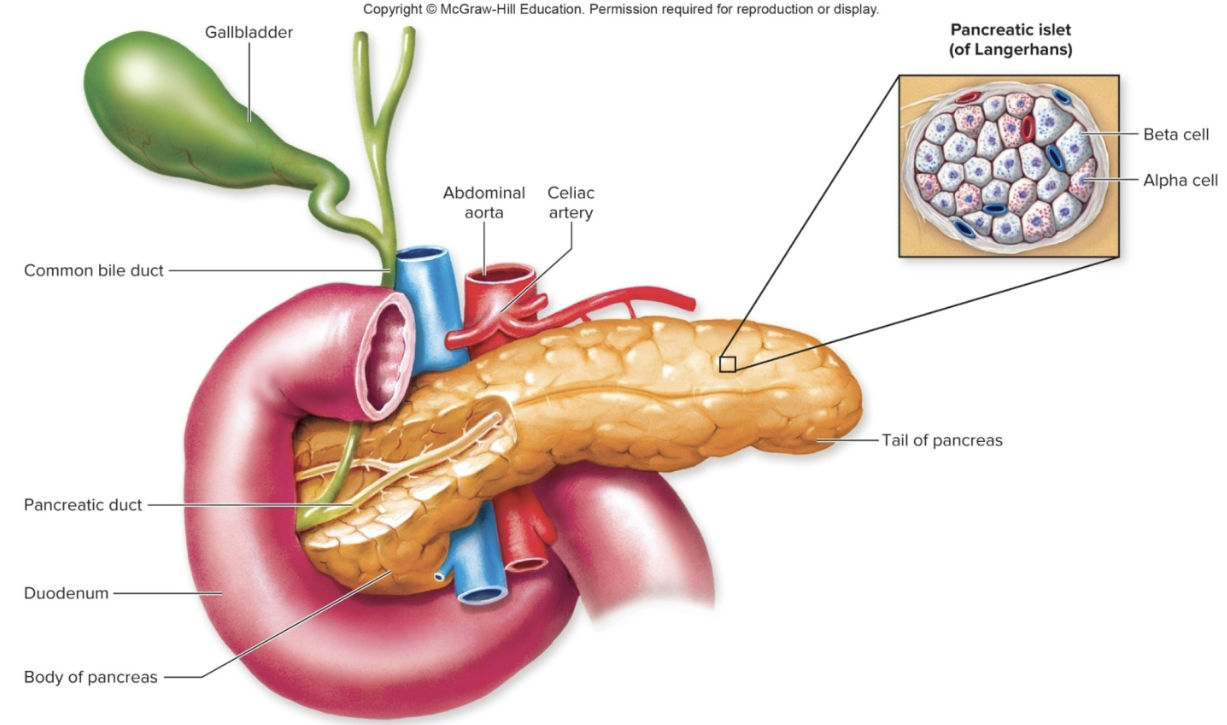
Pancreas (what is it? location?)
1) the pancreas is both an ENdocrine and an EXocrine gland
2) ENdocrine cells are located in pancreatic islets (islets of Langerhans)
Alpha cells: release glucagon
Beta Cells: release insulin
Pancreas: Insulin (what is it? what is it secreted by? its purpose?
1) Insulin is a primary hormone regulating plasma glucose concentration
2) insulin is secreted by beta cells when blood glucose levels rise after a sugary or carbohydrate meal
3) its purpose is to lower blood glucose levels to the “normal” range
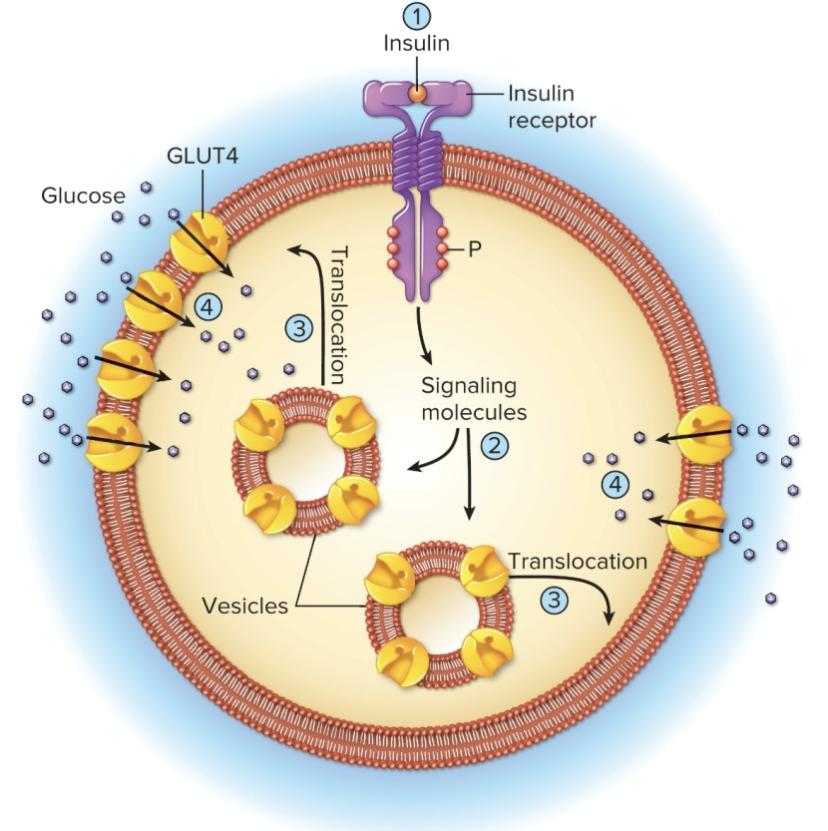
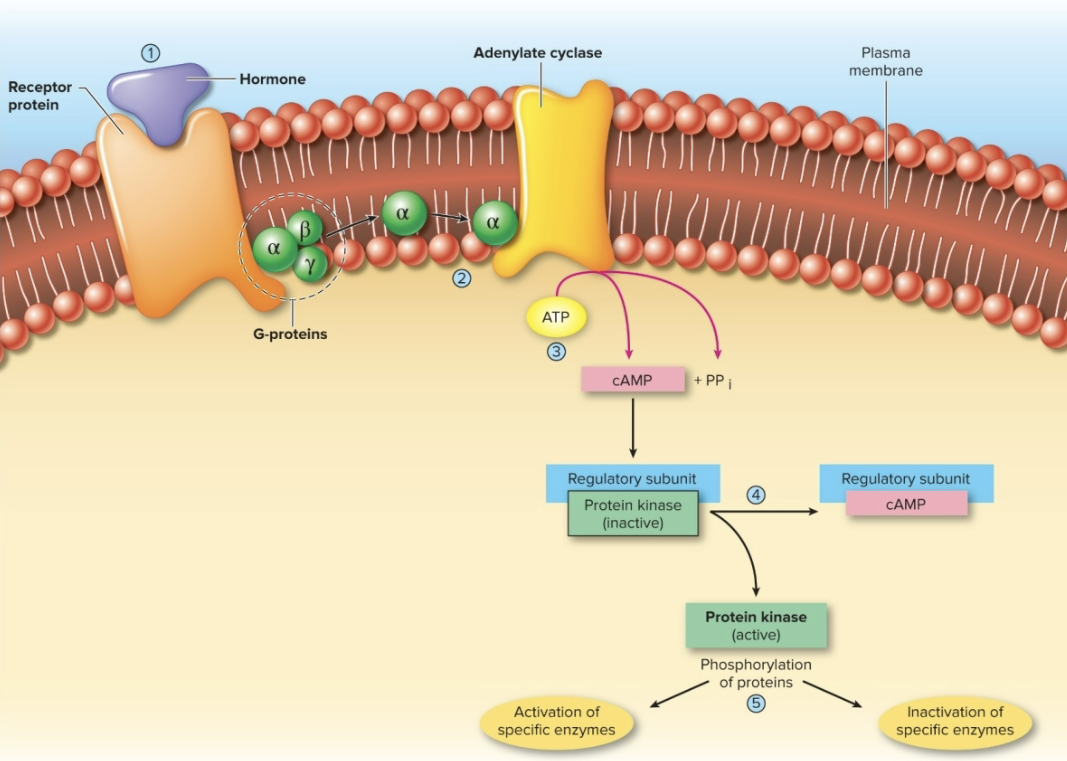
Action of Insulin
1) Insulin binds to receptors on target cells
vesicles with GLUT4 carrier proteins bind to membrane
glucose diffuses through GLUT4 channels by facilitated diffusion
occurs mostly in adipose tissue, skeletal muscle, and the liver
2) INdirectly stimulates the enzyme glycogen synthase in liver and skeletal muscles to promote sugar storage
3) Stimulates adipose tissue to store fat
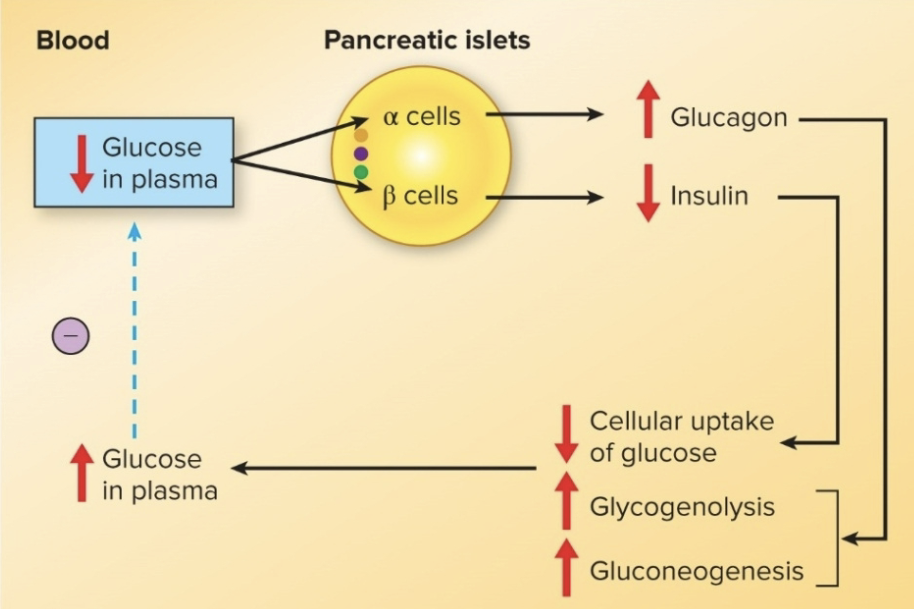
Pancreas: glucagon (what is it, secreted by, purpose?)
1) antagonistic (opposite to insulin)
2) secreted b alpha cells when blood glucose levels are LOW
3) purpose is to raise blood glucose levels to a “normal” range
Action of Glucagon
1) stimulates liver to hydrolyze glycogen into glucose & release it into the blood
2) stimulates gluconeogenesis conversion of noncarbohydrates (amino acids, lactate) into glucose
3) stimulates lipolysis in adipose tissue so fat is released and used as a fuel source instead of glucose
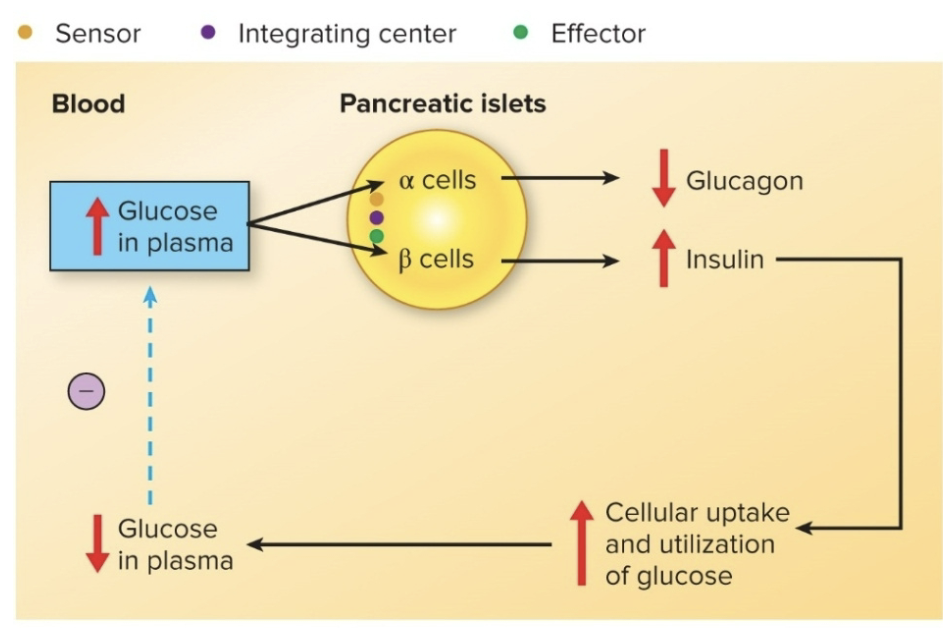
Glucose homeostasis
Diabetes Mellitus (what is it characterized by, two major forms?)
Diabetes mellitus is characterized by fasting hyperglycemina and the presence of glucose in the urine
Two major forms of this disease:
Type 1 diabetes
Type 2 diabetes
Type 1 Diabetes
caused by destruction of the BETA cells (production of insulin) and the resulting lack of insulin secretion
a) environmental factor: possibly a viral infection or a nutritional factor during childhood or early adulthood- causes the immune system to destroy the insulin- producing cells of the pancreases
b) genetic predisposition: makes some people more susceptible to an environmental factor
Type 2 Diabetes
caused largely by insulin resistance, or decreased tissue sensitivity to the effects of insulin
insulin resistance is when cells in muscles, body fat and liver, starts “resisting” or “ignoring” the signal that insulin is trying to send out- which is to grab glucose out of the bloodstream and put it into the cells
a) gestational diabetes occurs in about 4% of pregnancies due to insulin secretion that is inadequate to meet the increased demand imposed by the fetus and the anti-insulin effect of certain placental hormones
Other Endocrine Glands (3)
Gastrointestinal Tract
Gonads
Placenta
Endocrine Gland: Gastrointestinal Tract
several hormones are made in the stomach & small intestine to regulate digestive processes; includes gastrin, secretin, cholecystokinin
Endocrine Gland: Gonads
produce testosterone, estrogen, and progesterone to regulate production of gametes & secondary sexual characteristics
Endocrine Gland: Placenta
produces human chorionic gonadotropin (hCG) and samatomammotropin to regulate pregnancy
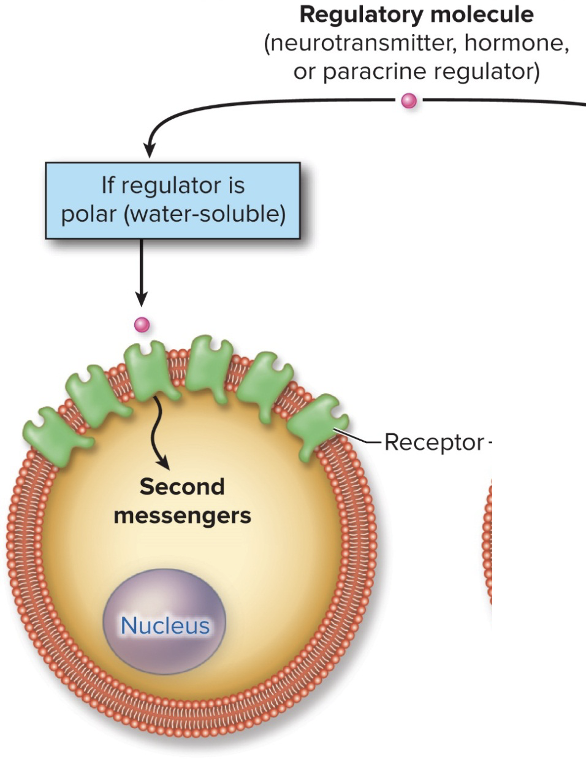
Autocrine Vs Paracrine Signals
1) both are involved in short-range signaling between neighboring cells within an organ
2) Autocrine signals: the sender & receiver are the same cell type( cell A to cell A)
3) Paracrine signals: the sender & receiver are different cell types/tissues (cell A to cell B)
Ex of Autocrine Regulation
1) many regulatory molecules are called cytokines or growth factors
cytokines regulate cells of the immune system
growth factors promote growth & cell division
given specific names depending on where they are found & what they do- for ex: lymphokines, neurotrophins
2) most control gene expression in the target cell