NPB 101: Cardiac Physiology
1/142
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
143 Terms
three principle components of the circulatory system are...
heart, blood, blood vessels
Functions of the circulatory system
1. Transport
2. Protection
3. Regulation
- supply oxygen, remove wastes, temperature regulation, distribution of hormones, and immune-vigilance
functions of the circulatory system are impacted by...
- endocrine and nervous systems
- kidneys (salt and water balance)
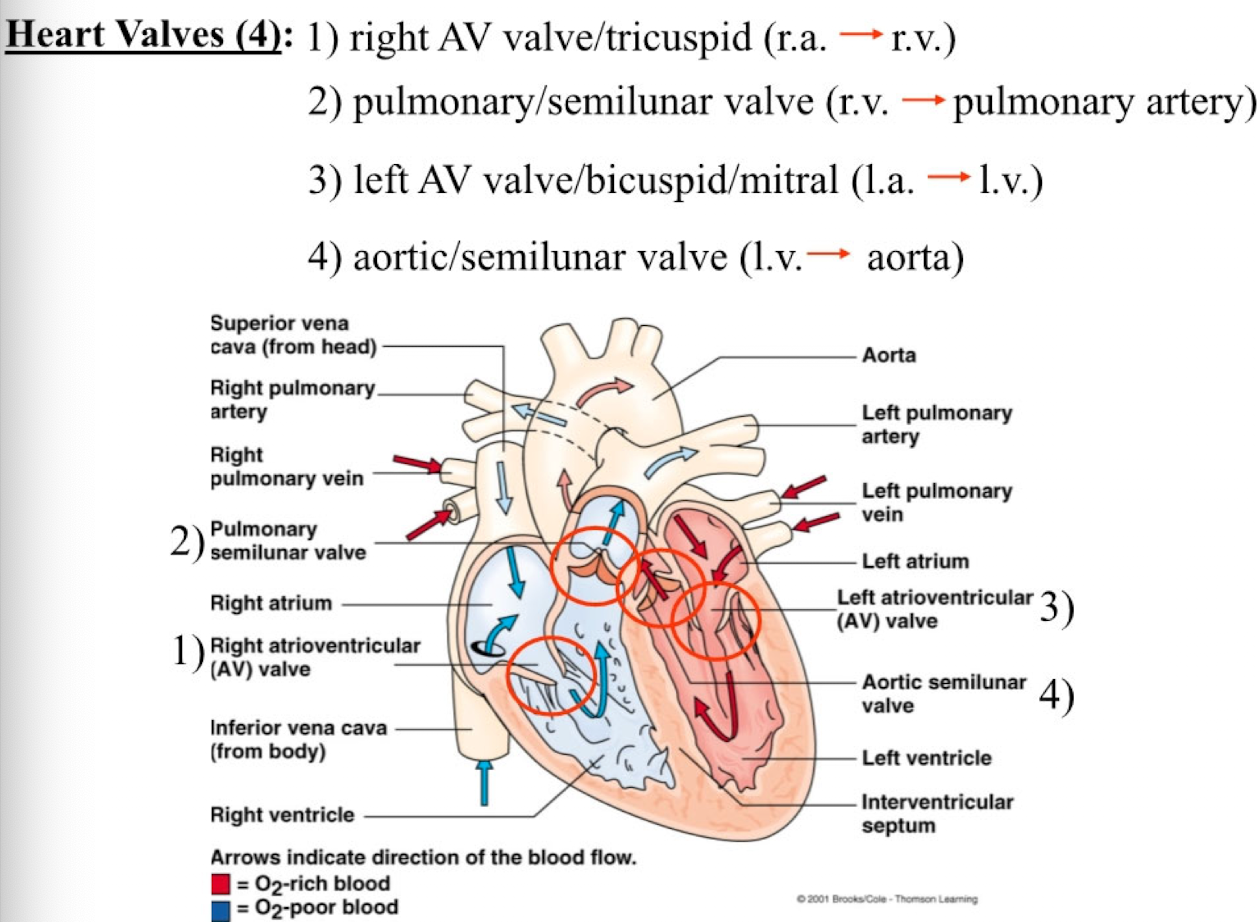
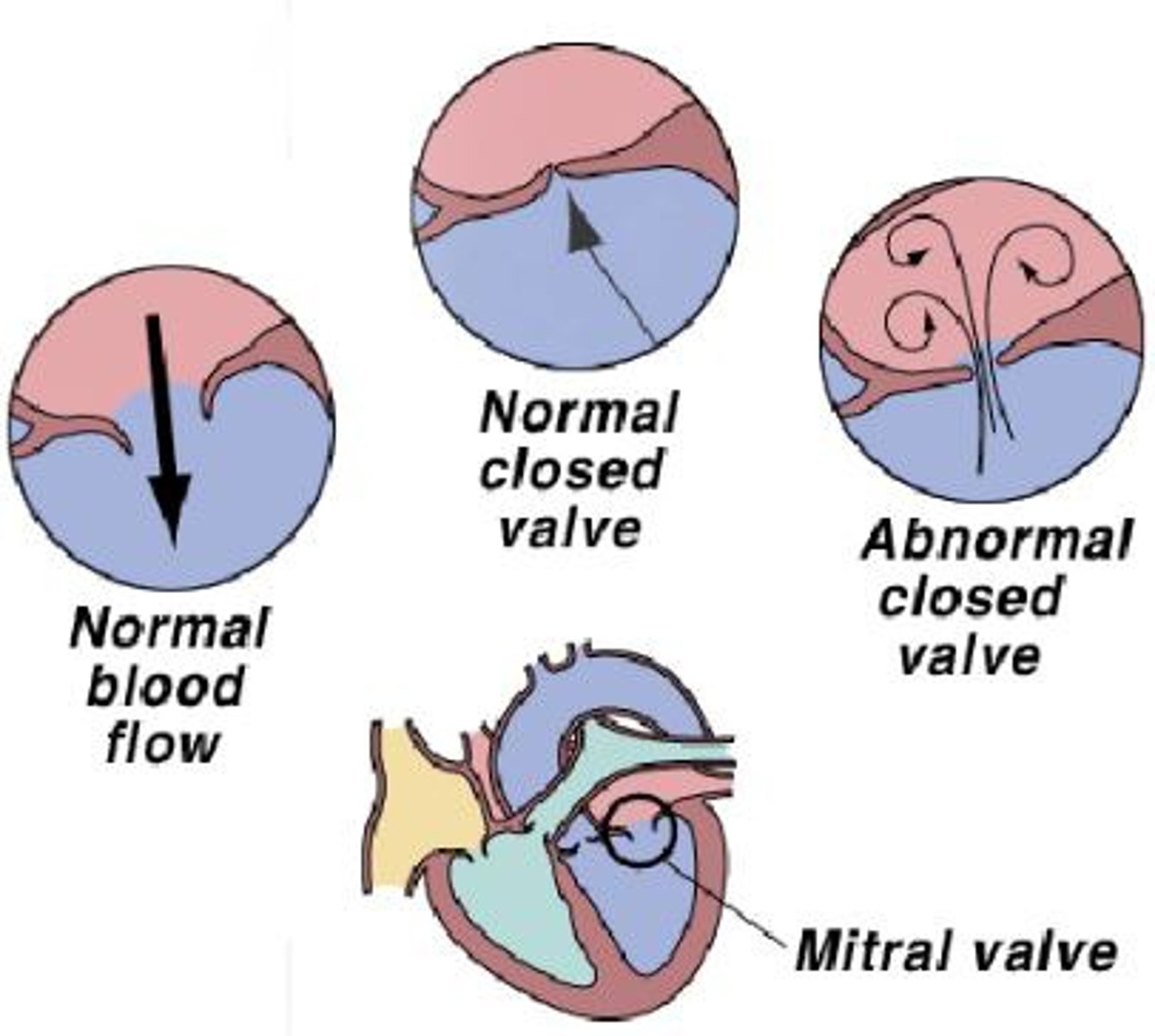
How many heart valves are there?
4
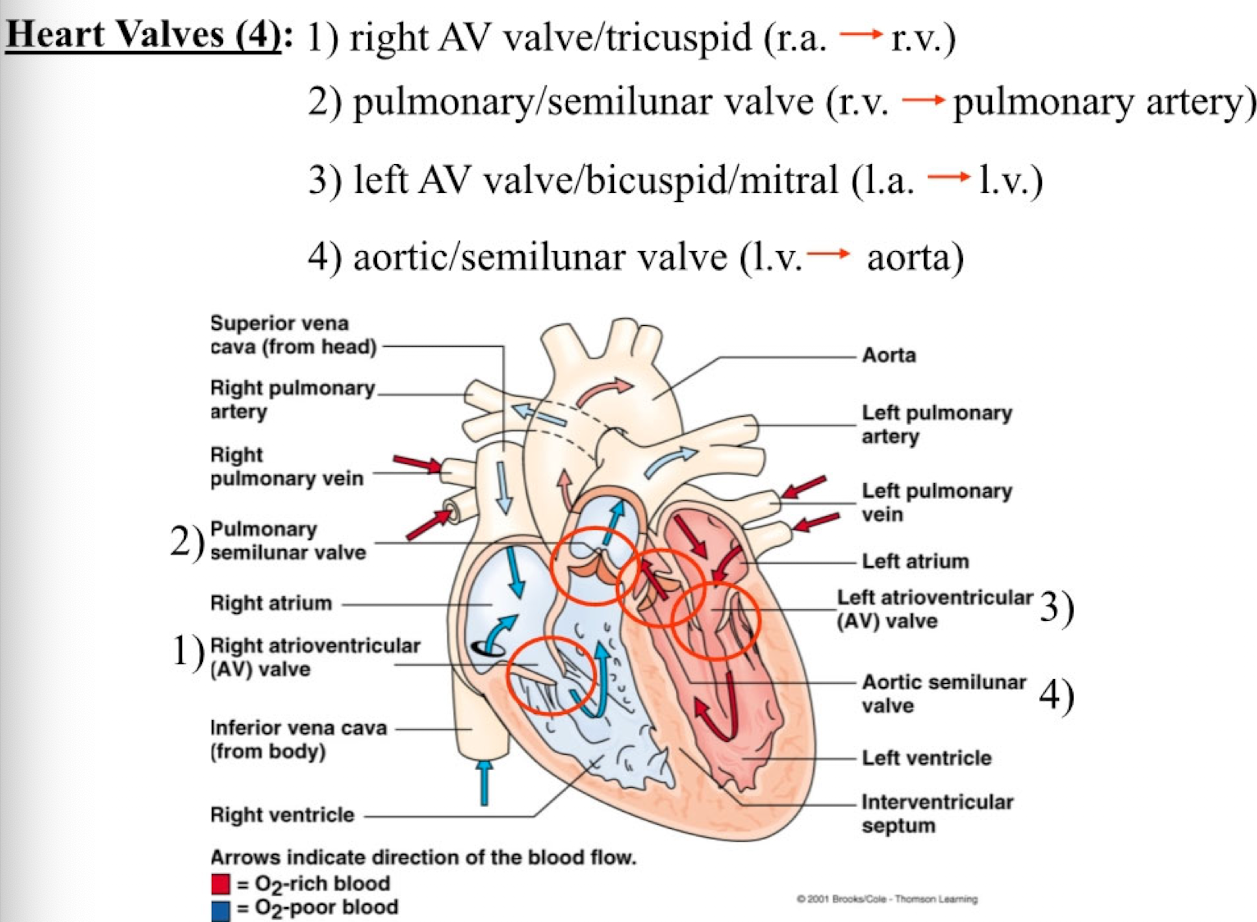
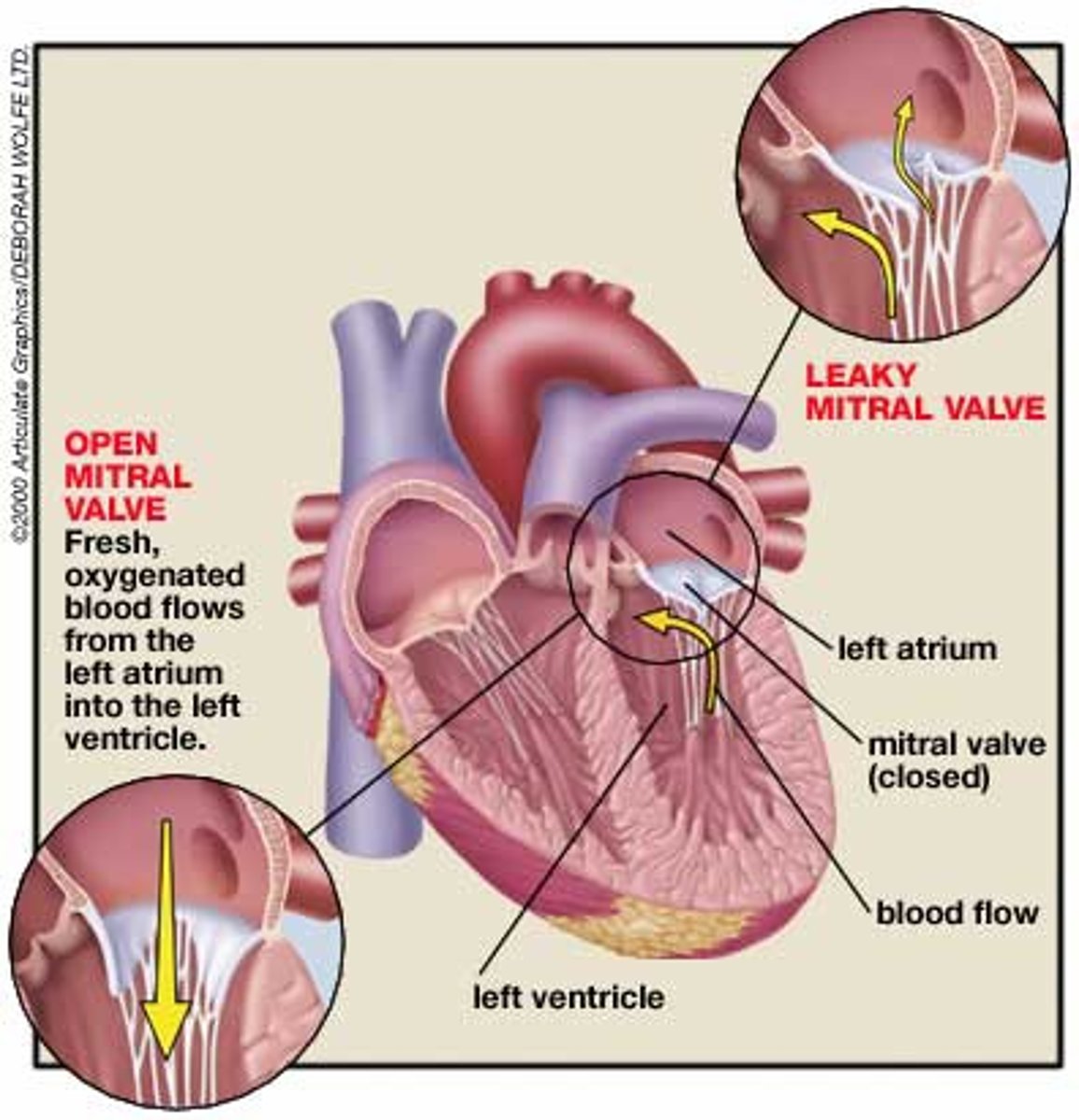
AV valves
right AV valve / tricuspid: (r.a. → r.v.)
pulmonary/semilunar valve (r.v. pulmonary artery)
left AV valve / mitral/ bicuspid: (l.a. → l.v.)
aortic/semilunar valve (l.v. → aorta)
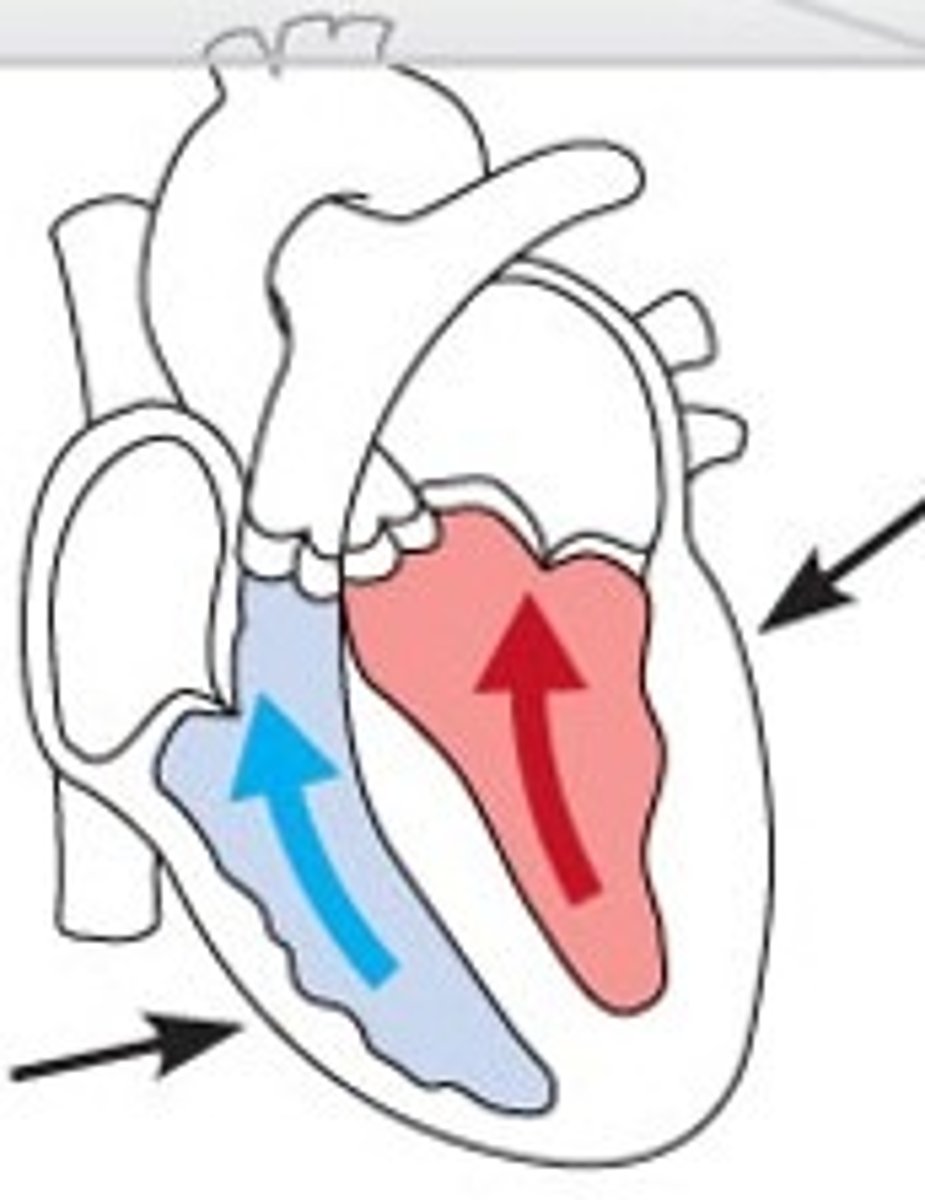
Systemic vs Pulmonary Arteries
Systemic arteries carry oxygenated (oxygen-rich) blood to the body from the heart
Pulmonary arteries carry deoxygenated (oxygen-poor) blood to the lungs from the heart
Systemic and pulmonary veins
systemic veins carry deoxygenated blood from the body to the heart
pulmonary veins carry oxygenated blood from the lungs to the heart
flow of blood starting from the lungs
lungs --> pulmonary veins --> LA --> biscuspid valve --> LV --> aortic valve --> aorta --> systemic circulation (O2-rich blood) --> vena cava --> RA --> tricuspid valve --> RV --> pulmonary artery --> lungs → repeat
when pressure is higher BEHIND a valve...
it opens
when pressure is higher in FRONT of a valve...
it closes
Heart valves
flap of tissue in the heart and large veins that prevents blood from flowing backwards (ensure a one-way flow of blood)
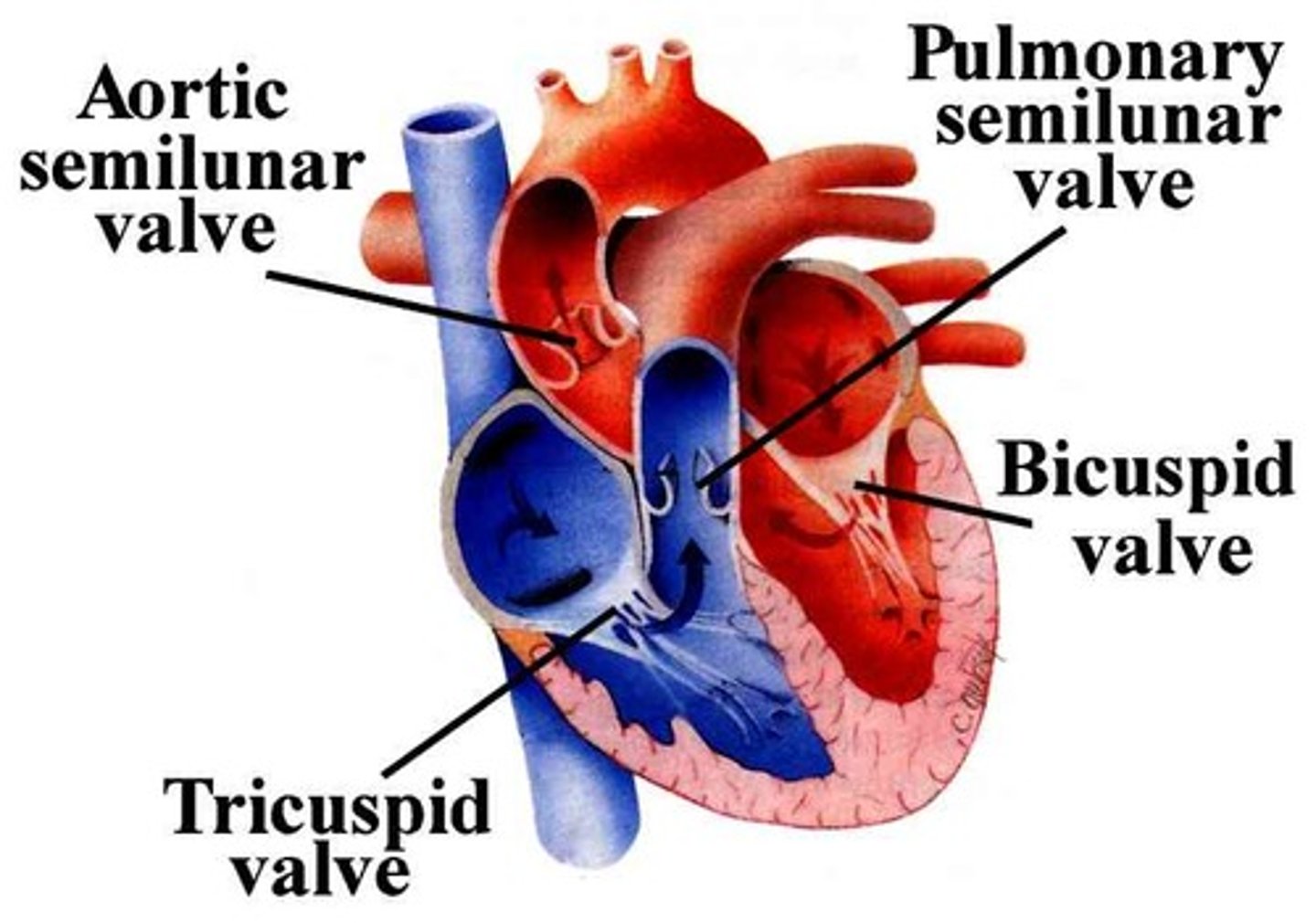
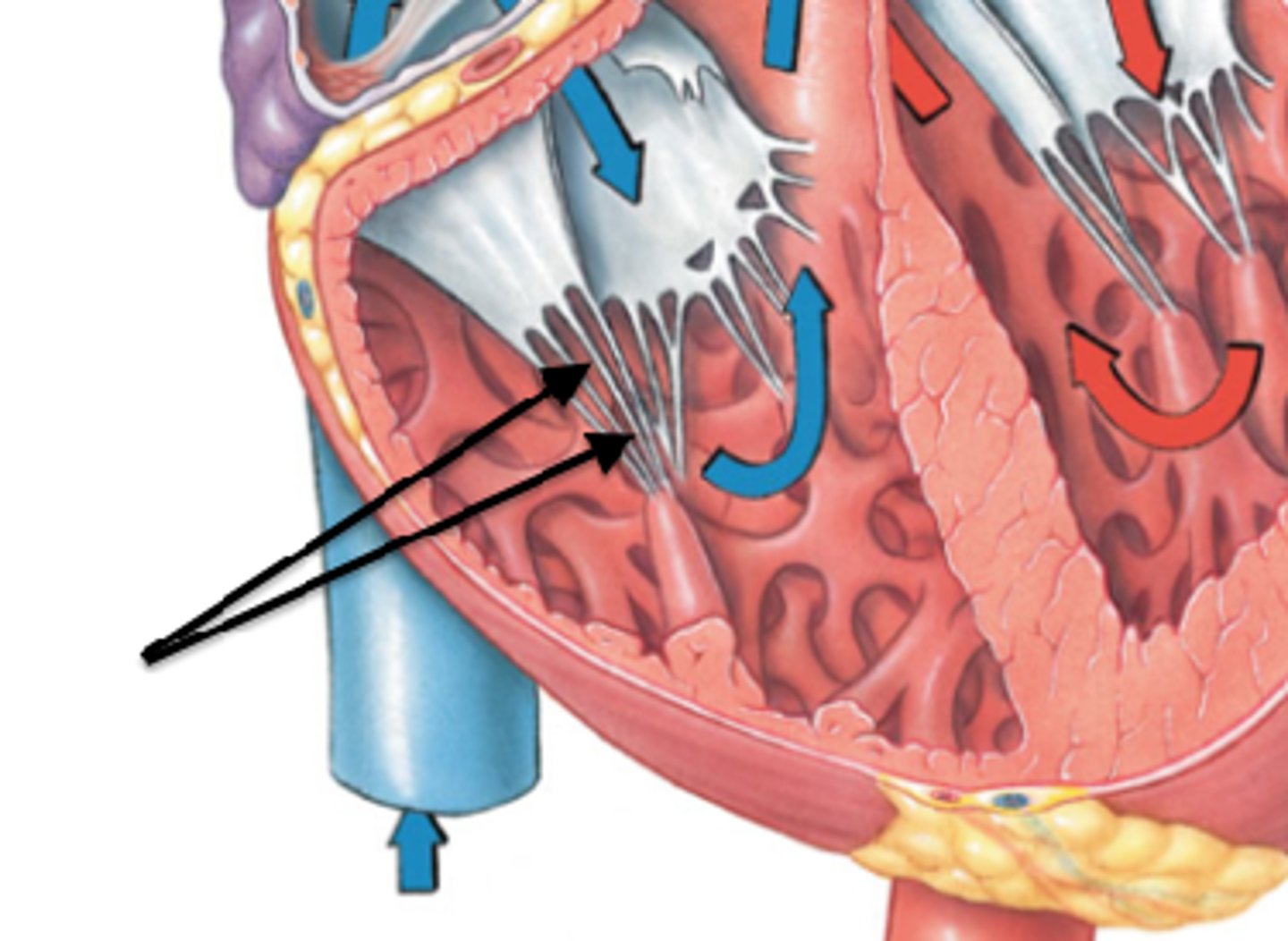
chordae tendineae
"heart strings" are tiny white collagenic cords that anchor the cusps to the ventricular walls.
They originate from the papillary muscles.
prevents valves from everting
causes of heart valve disease
product of age-related changes, infection (mouth), or other cardiovascular problems
- NOT only in those born with heart valve defects
connective tissue
separates atria and ventricles
- provides a rigid base for attaching heart valves to cardiac muscle
- prevents communication of electrical impulses with other muscles
- allows for localization and sequential flow of electrical impulses
thickest in the LV
ring of dense fibrous connective tissue surrounds each valve
3 layers of the heart wall
1. Epicardium (outer)
2. Myocardium
3. Endocardium/endothelium (inner)
endocardium
thin endothelial tissue lining interior of each chamber (atria and ventricles)
myocardium
- middle layer of the heart wall
- composed of cardiac muscle
- intercalated discs connect cardiac muscle cells together (desmosomes and gap junctions)
Desmosomes in myocardium
mechanism that holds cells together
- stronger than gap junctions and important for structure
gap junctions in myocardium
paths of low R for elec current flow between muscle cells
- allows for the formation of a functional syncytium
(atria and ventricles are separate functional syncytiums as the atria contract together before the ventricles contract together)
autorhythmic cells of the heart
depolarize to threshold "spontaneously"
-->Due to slow Na+ Channel inflow
SA node, AV node, Bundle of His, Purkinje Fibers
- does not require innervation
- only 1% of cardiac cells
pacemaker cells of the heart
are cardiac myocytes
- spontaneously depolarize at regular intervals
- grouped together into specific regions (nodes) that together control rate and coordination of cardiac contractions
contractile cardiac cells
-bulk of heart muscle
-contractions are initiated by action potentials (innervation required)
- 99% of all cardiac cells
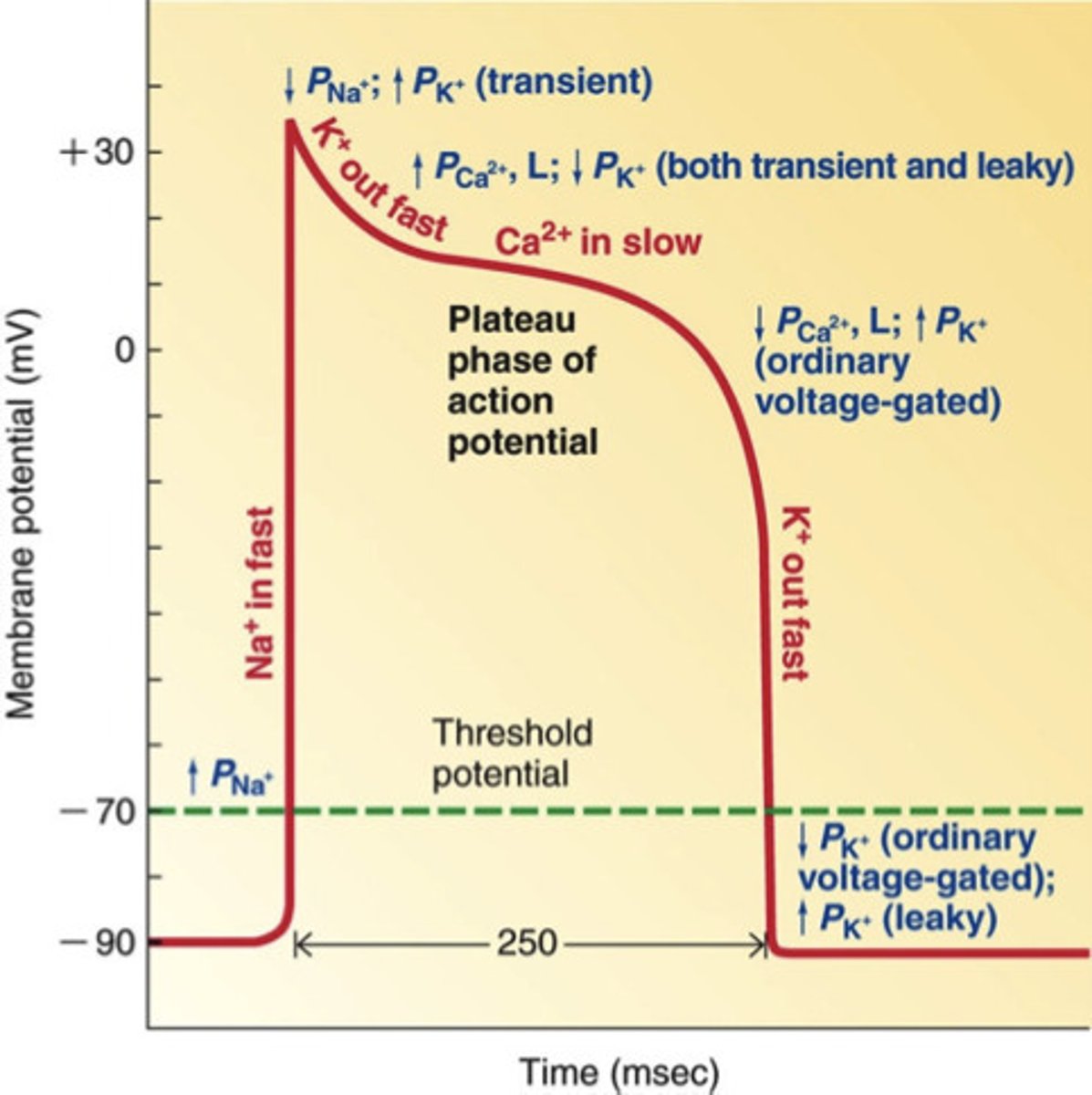
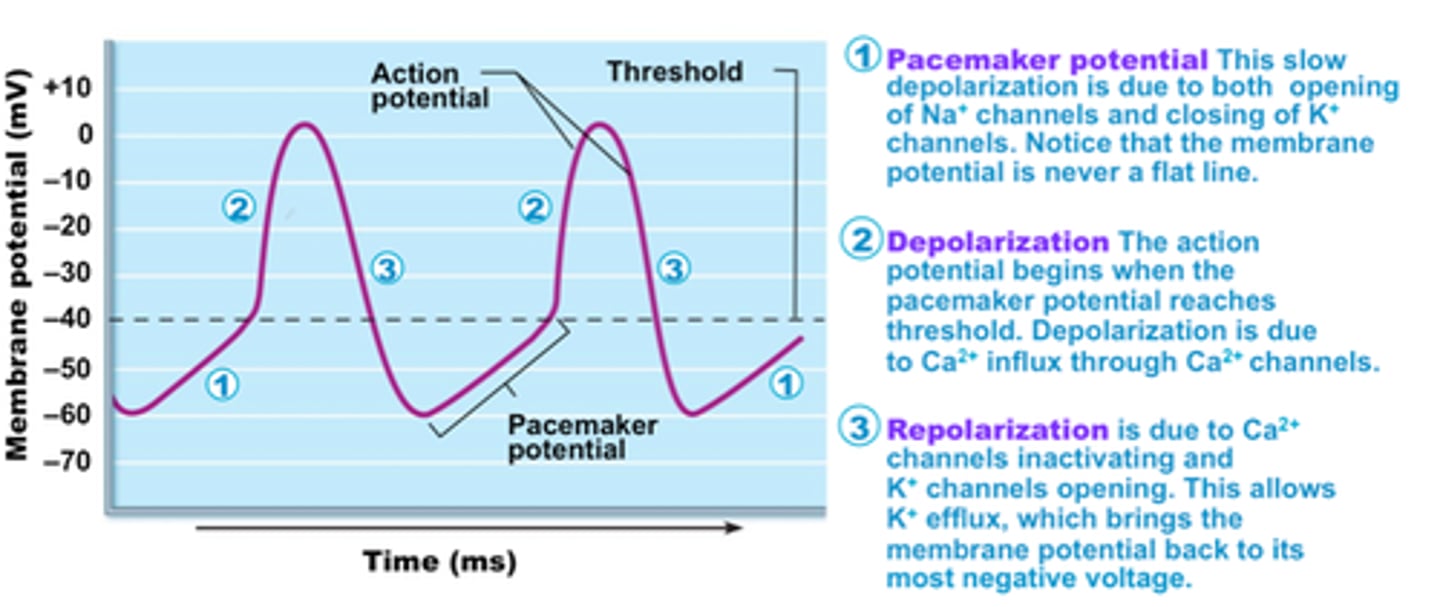
pacemaker activity of cardiac autorhythmic cells
The first half of the pacemaker potential is the result of simultaneous opening of unique funny channels, which permits inward Na+ current, and closure of K+ channels, which reduces outward K+ current (enables cell to become more +)
The second half of the pacemaker potential is the result of opening of T-type Ca2+ channels (which enables reaching threshold).
Once threshold is reached, the rising phase of the action potential is the result of opening of L-type Ca2+ channels, whereas the falling phase is the result of opening of K+ channels and inactivation of Ca++ channels.
resting membrane potential of cardiac pacemaker cells vs cardiac contractile cells
cardiac pacemaker cells - higher Vm at -60 mV
- would be harder to reach threshold (-40mV) with a more negative Vm
cardiac contractile cells - lower Vm/ more negative at -90mV
- due to innervation, threshold (-70mV) can still be reached
nodes
specialized cardiac muscle cells capable of pacemaker activity
- grouped together to form nodes (SA and AV)
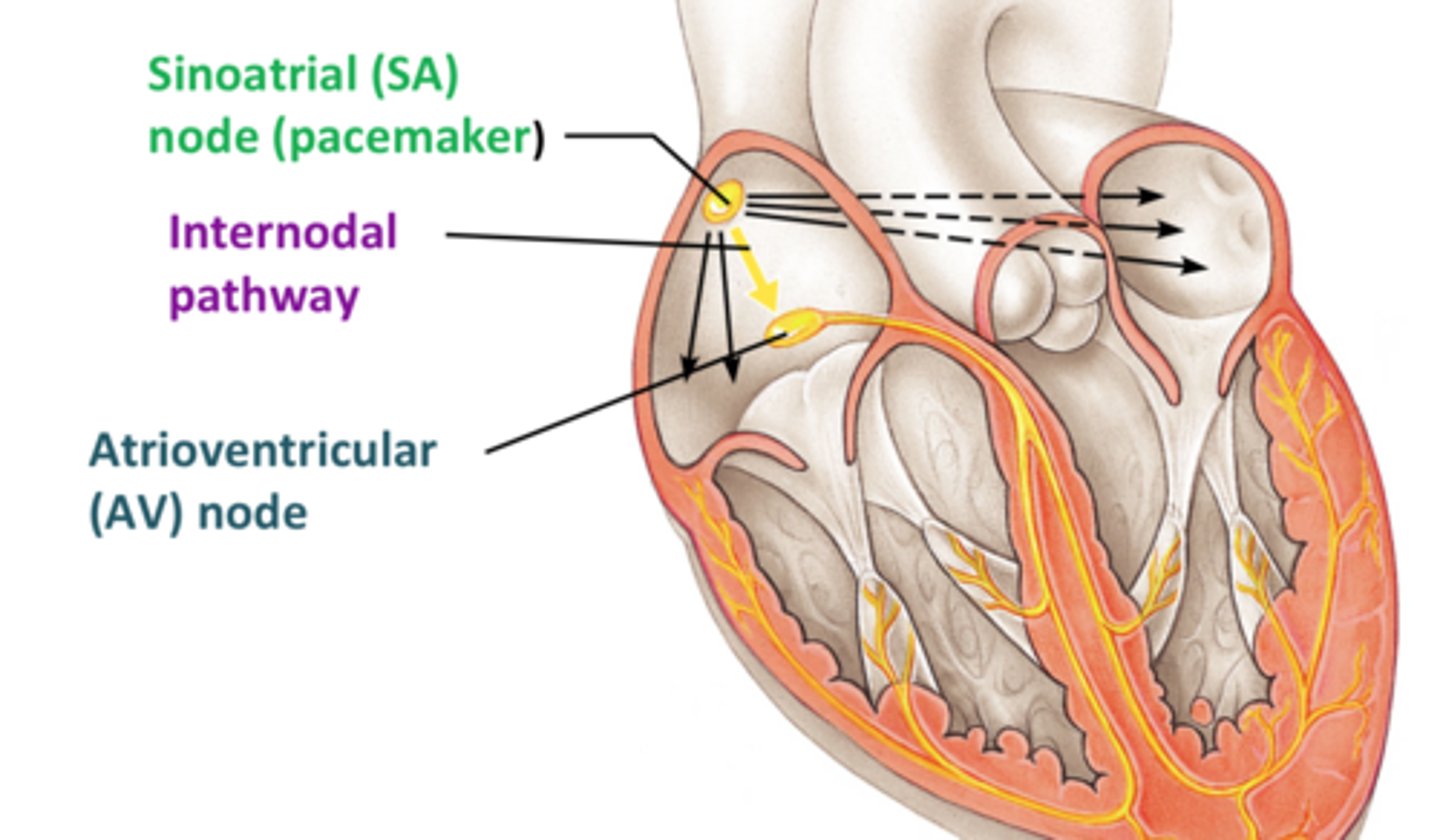
SA node (sinoatrial node)
-pacemaker of the heart
-sets the heartbeat rate (leads all other PM cells of the heart)
-located in the right atrium
-causes atria to contract
- 70 APs/ min
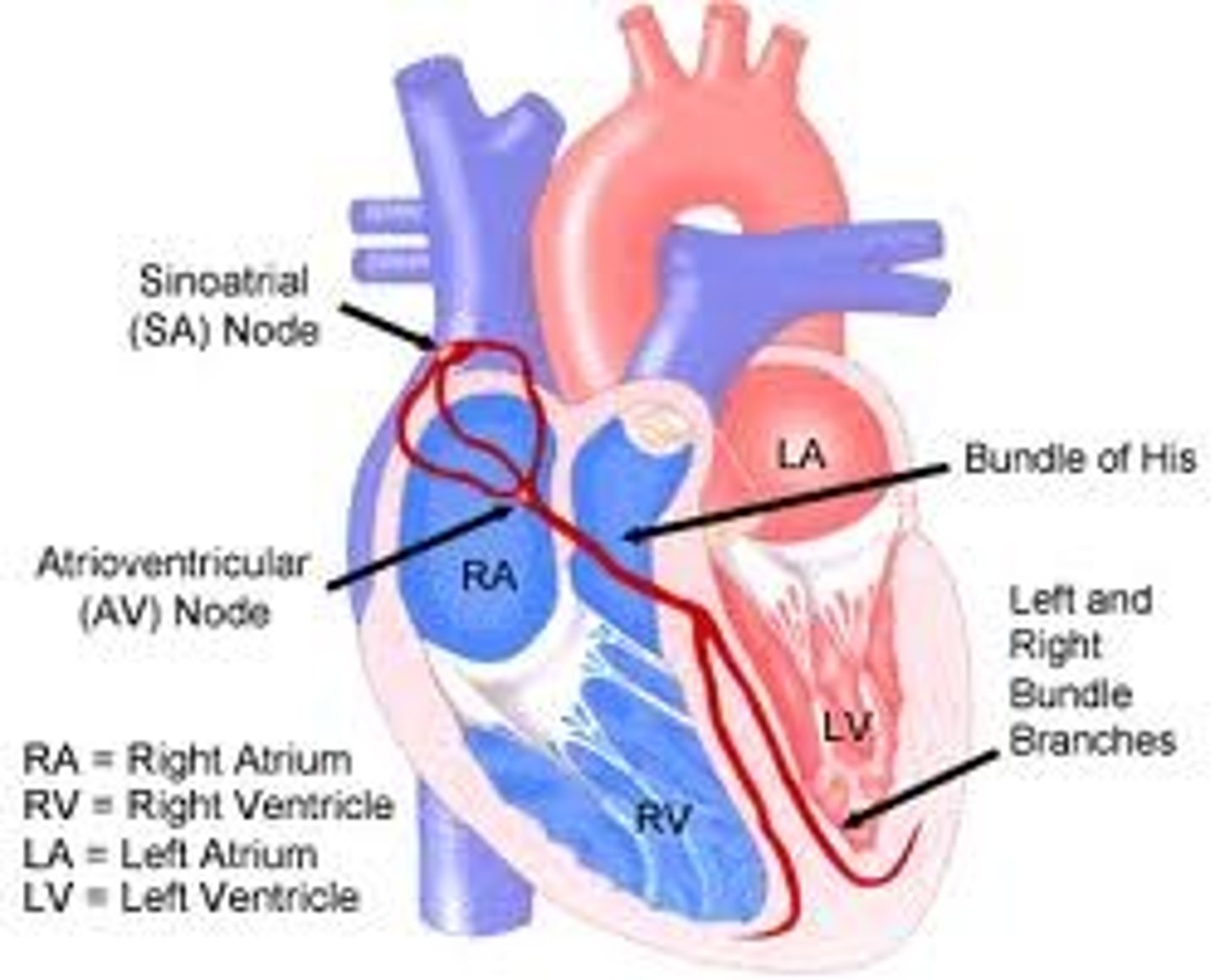
AV node (atrioventricular node)
- on base of RA
- Receives impulse from SA node and slowly passes the signal to the AV bundle (Bundle of His)
- 50 APs/ min
- if SA node is damaged, leads other PM cells and sets the heartbeat
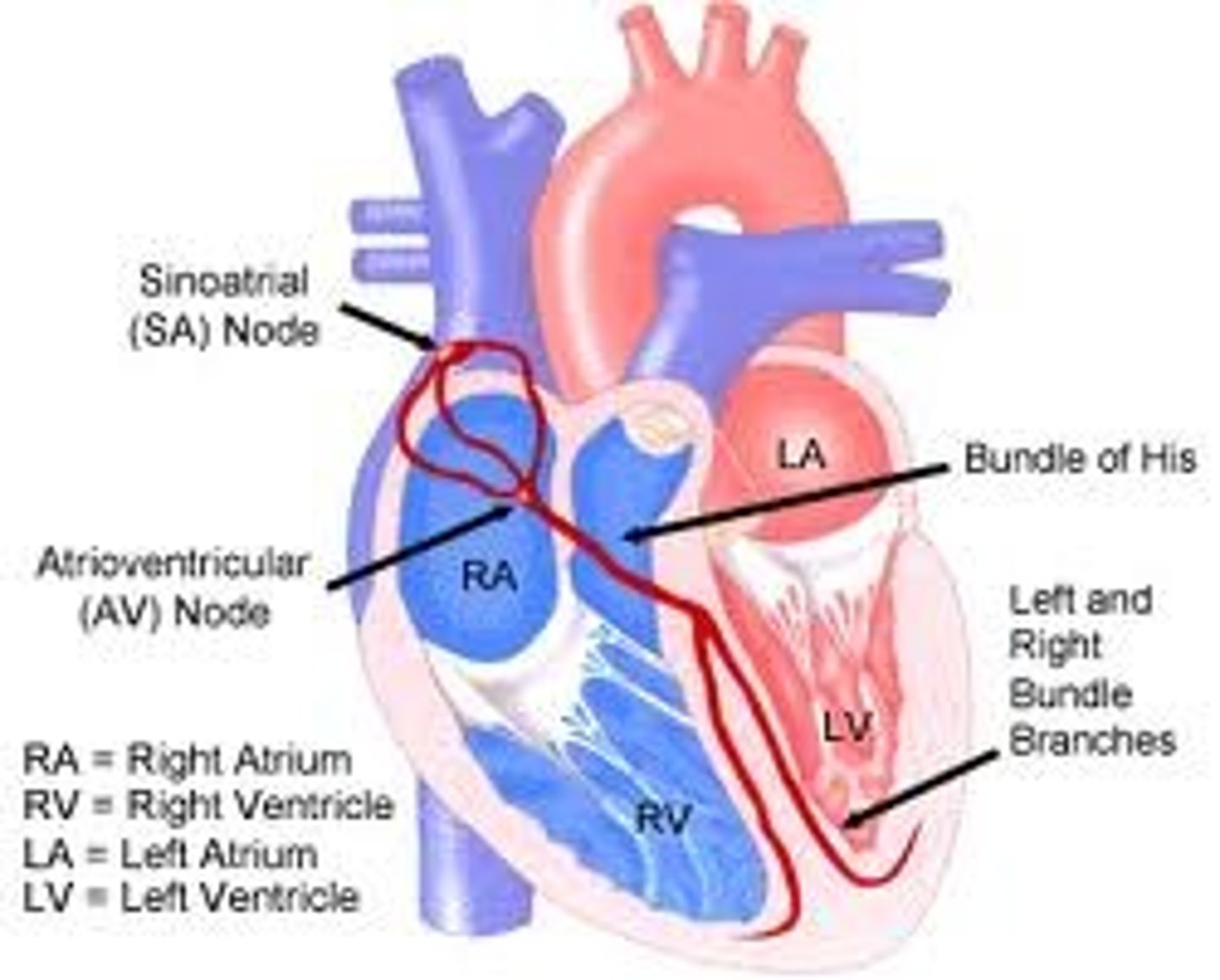
Bundle of His (AV bundle)
Conducts electrical impulses from the atria to the ventricles via bundle branches.
- located in the middle of the heart
- branches into the right and left bundle branches
- heart rate of 30-40 bpm (or 30-40 APs/min)
Purkinje fibers
specialized conductive fibers located within the walls of the ventricles
fibers in the ventricles that transmit impulses to the right and left ventricles, causing them to contract
- heart rate of 30-40 bpm (or 30-40 APs/min)
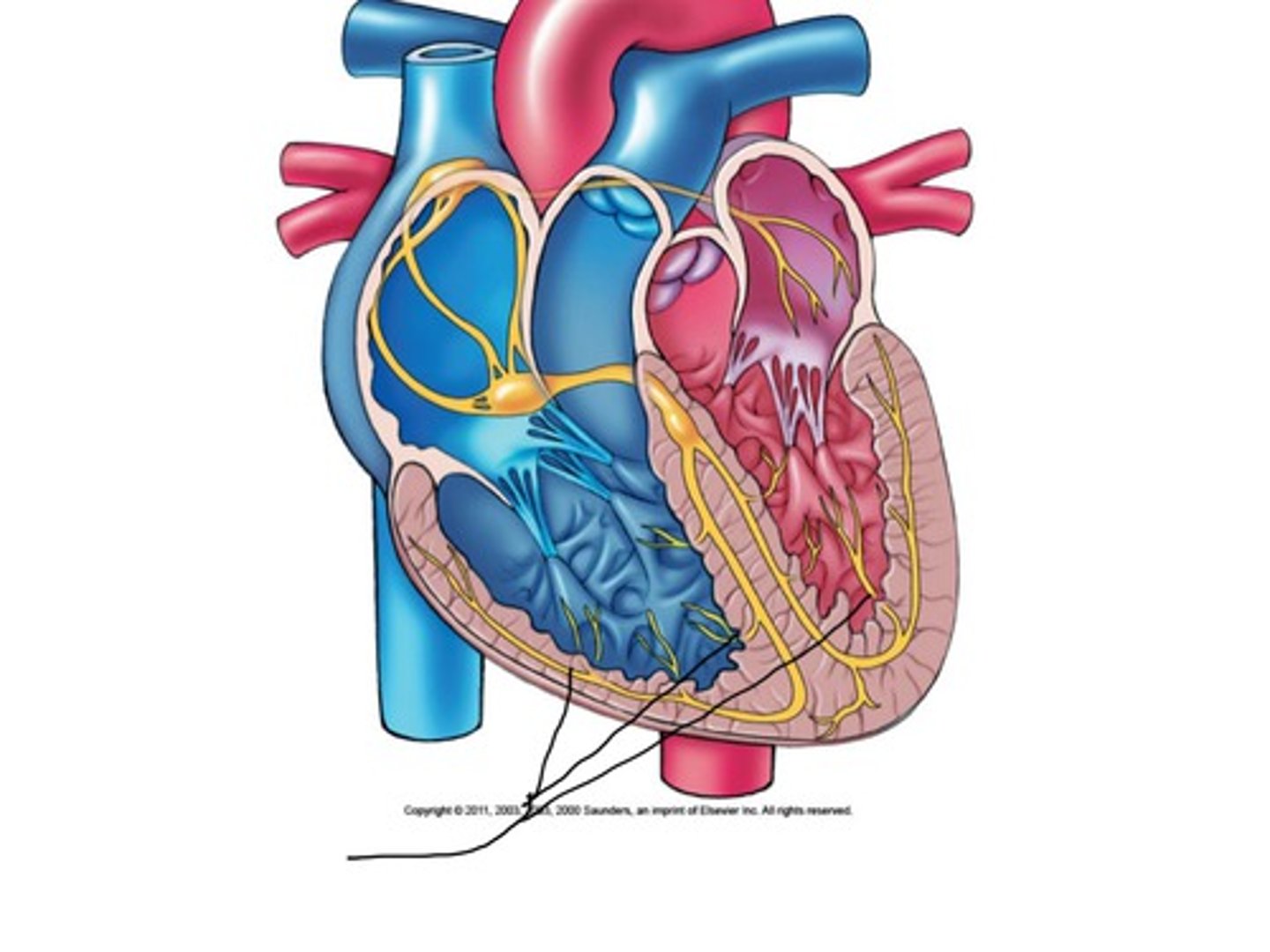
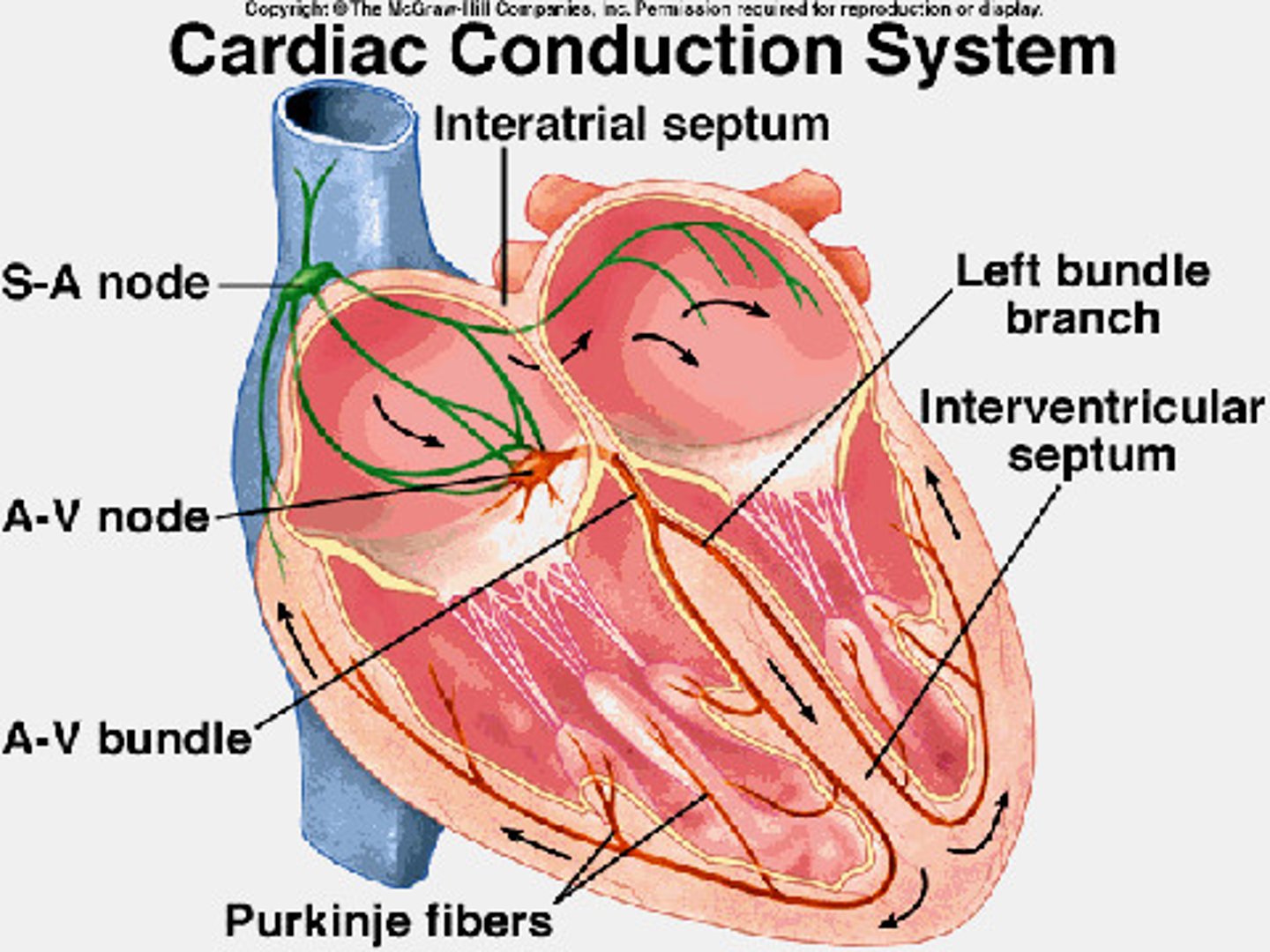
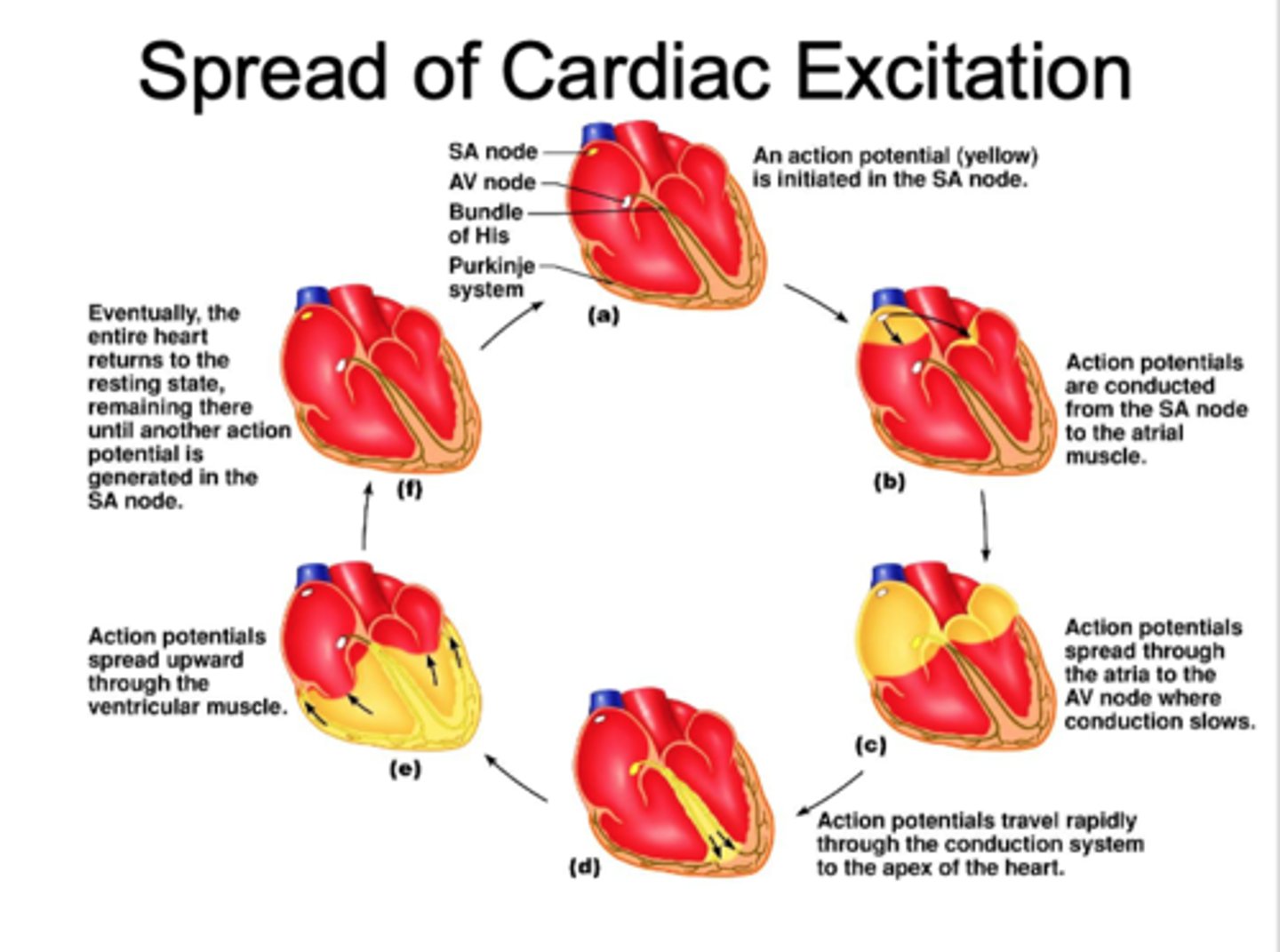
spread of cardiac excitation
1) Cardiac impulse originates at SA node
2) Action potential spreads throughout right and left atria via interatrial pathway
3) Impulse passes from atria into ventricles through AV node
4) AV node delay - 100 ms or 0.1s - (ensures atrial contraction precedes ventricular contraction to allow complete ventricular filling)
5) Impulse travels rapidly down interventricular septum by means of bundle of His
6) Impulse rapidly disperses throughout myocardium by means of Purkinje fibers (into ventricles)
7) Rest of ventricular cells activated by cell-to-cell spread of impulse through gap junctions
interatrial pathway
SA node ---> right atrium ---> left atrium
Rapid
Simultaneous contraction right and left atria
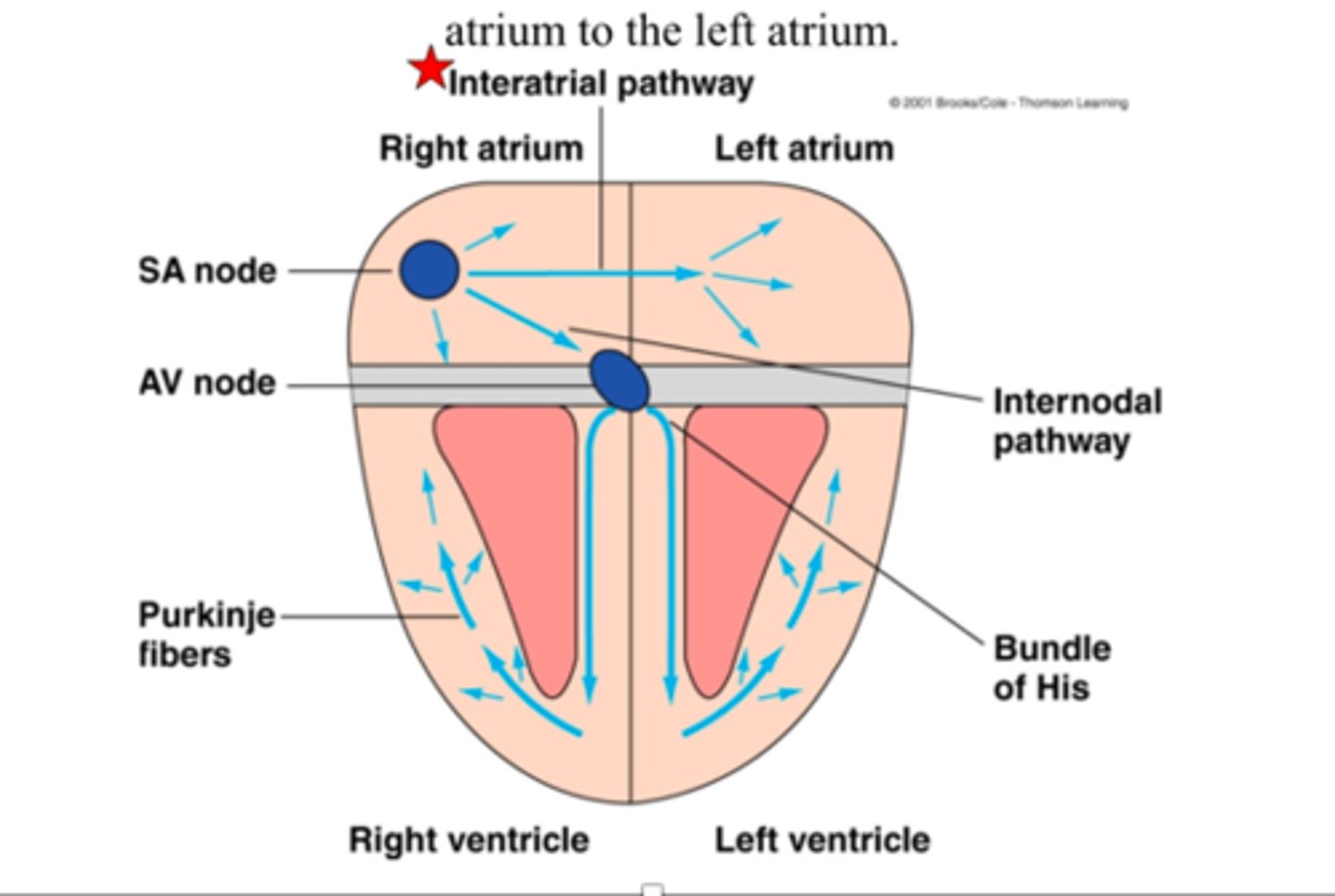
internodal pathway
conduction pathway from the SA node to the AV node
AV nodal delay
The delay in impulse transmission between the atria and ventricles at the AV node
which allows enough time for the atria to become completely depolarized and contract
atria empty their contents into the ventricles before ventricular depolarization and contraction occur
100 ms / 0.1s
PR segment
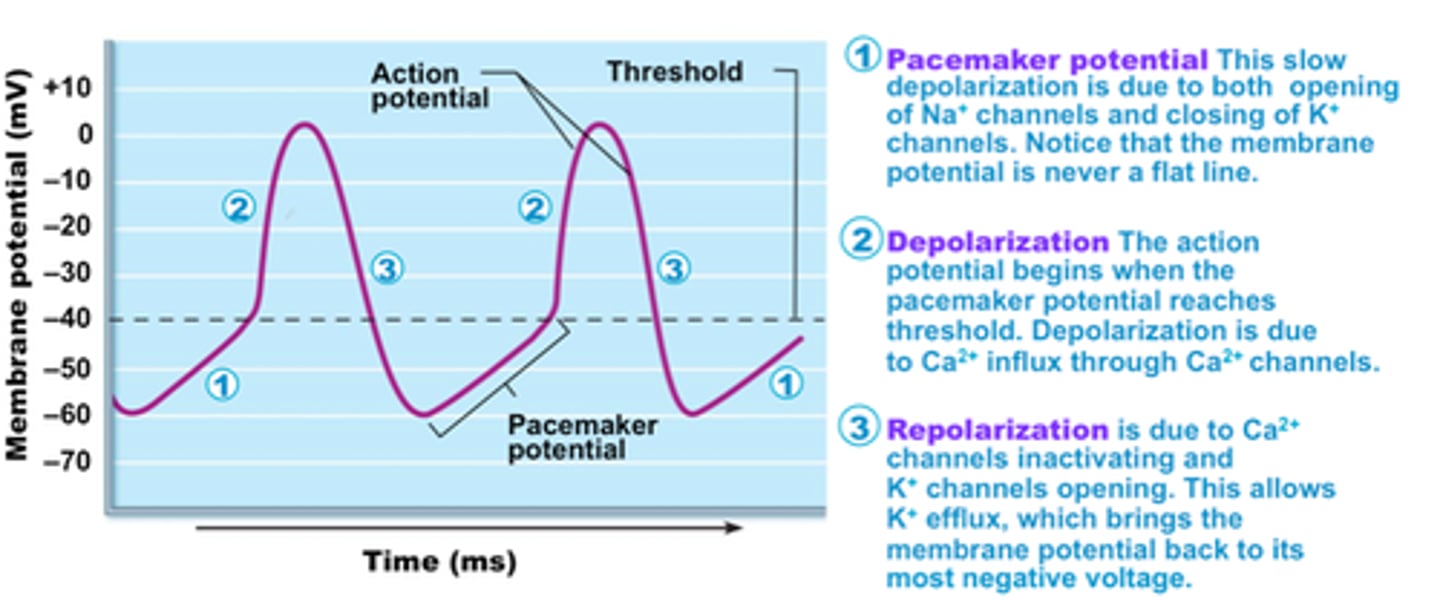
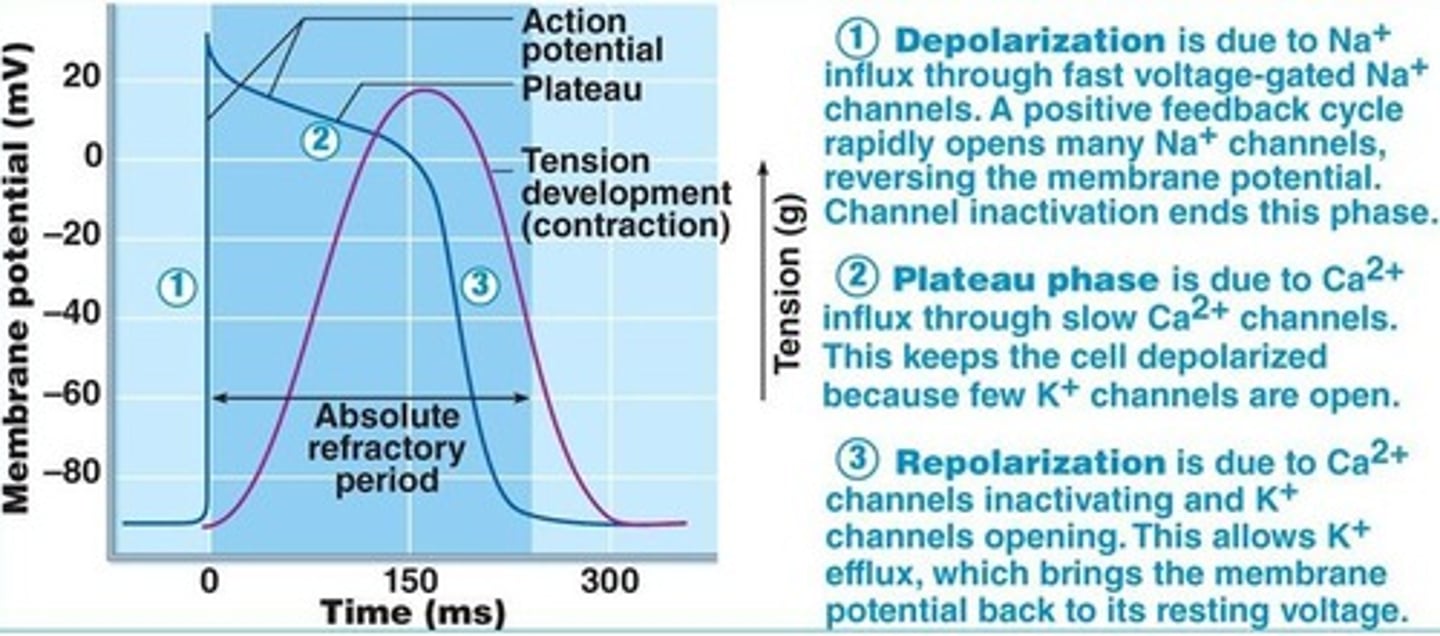
AP in cardiac contractile muscle
resting membrane potential = -90 mV
- rapid rising phase --> result of Na+ entry on opening of fast Na+ channels at threshold
- early, brief repolarization --> after peak, limited K+ efflux (transient channels open) with inactivation of Na+ channels
- plateau phase --> slow Ca++ entry (via L-type Ca++ channels) and less K+ efflux on closing of many K+ channels (leaky and transient)
- rapid falling phase --> efflux of K+ through opening of voltage-gated K+ channels
how is the resting potential maintained in contractile cardiac muscle cells?
by opening of leaky K+ channels, Vm is maintained at -90 mV
components of APs in PM vs cardiac contractile cells
PACEMAKER CELLS: slow depolarization, no plateau, increase heart rate in newborn/ infants; autorhythmic
CONTRACTILE CELLS: rapid rising phase, plateau, rapid falling phase; nervous stimulus
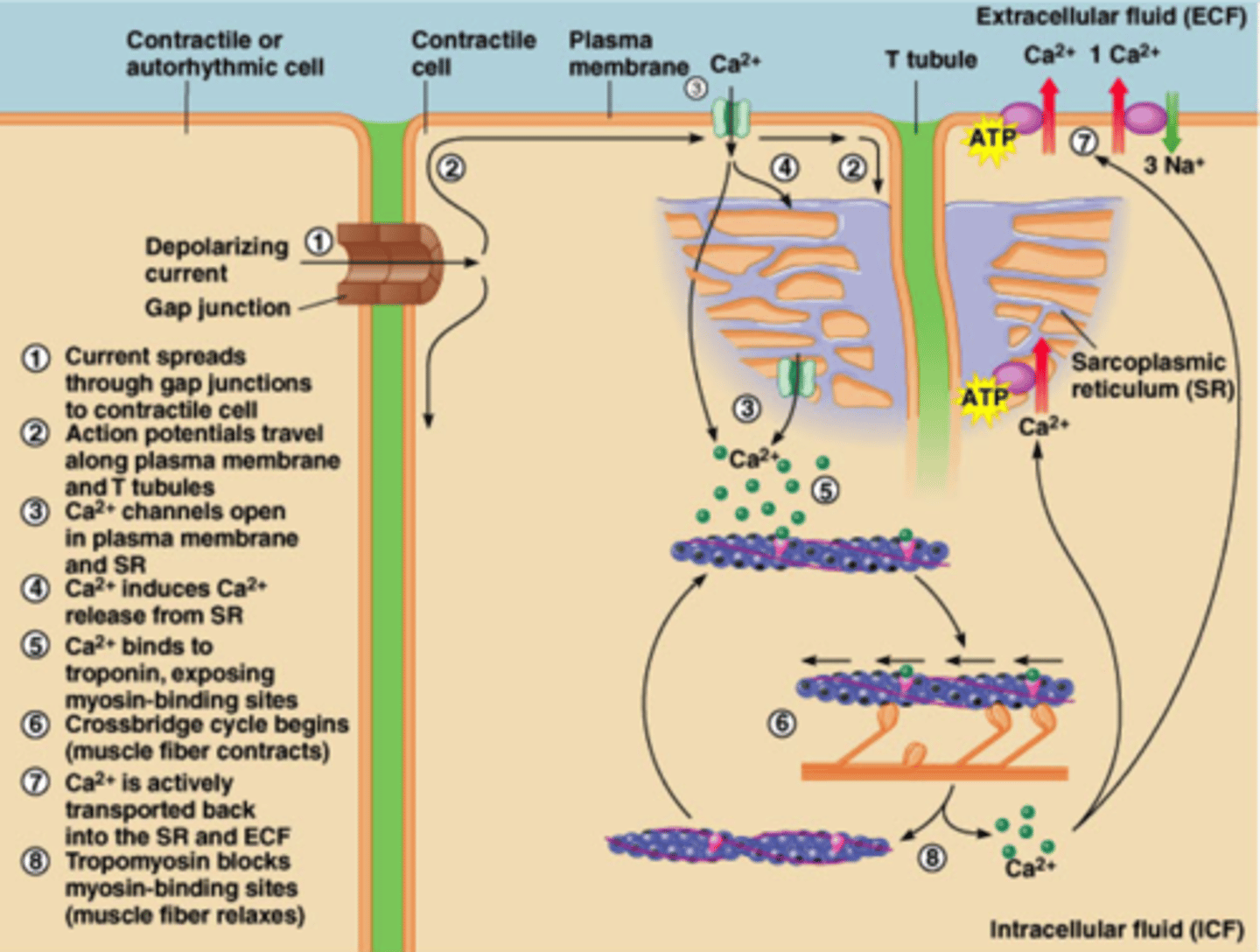
excitation-contraction coupling in cardiac muscle
-components of both skeletal and smooth muscle
-gap junctions located in intercalated discs
1.) Action potential on sarcolemma travels on T-tubule and activates L-type Ca2+ channels (DHPRs - not bound to foot proteins - stimulate voltage-gated Ca++ channels, leading to tubule opening and Ca2+ influx from the cell into the cytosol)
2.) Increased intracellular Ca2+ activates ryanodine receptors on the sarcoplasmic reticulum, which release intracellular Ca2+ stores (calcium-induced calcium release)
3.) Ca2+ binds to troponin C, tropomyosin is moved off of binding sites, and actin-myosin crossbridge formation can occur --> contraction
Cross-bridge cycling continues as long as intracellular Ca2+ concentration remains high enough to occupy the Ca2+ binding sites on troponin C
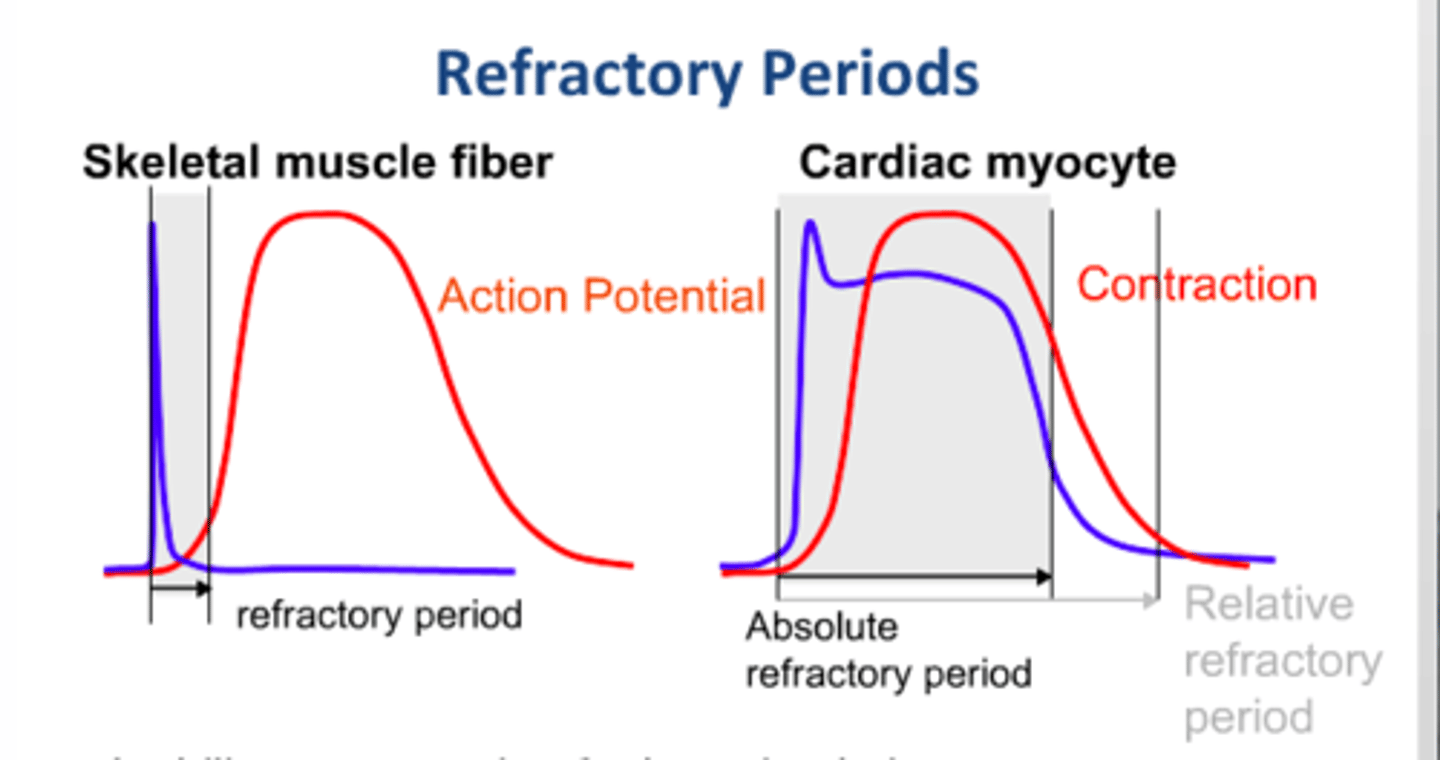
Refractory period of cardiac muscle
Lasts almost as long as the contraction period and is much longer than the refractory period in skeletal muscle.
myocardial cells have a long plateau phase before depolarization
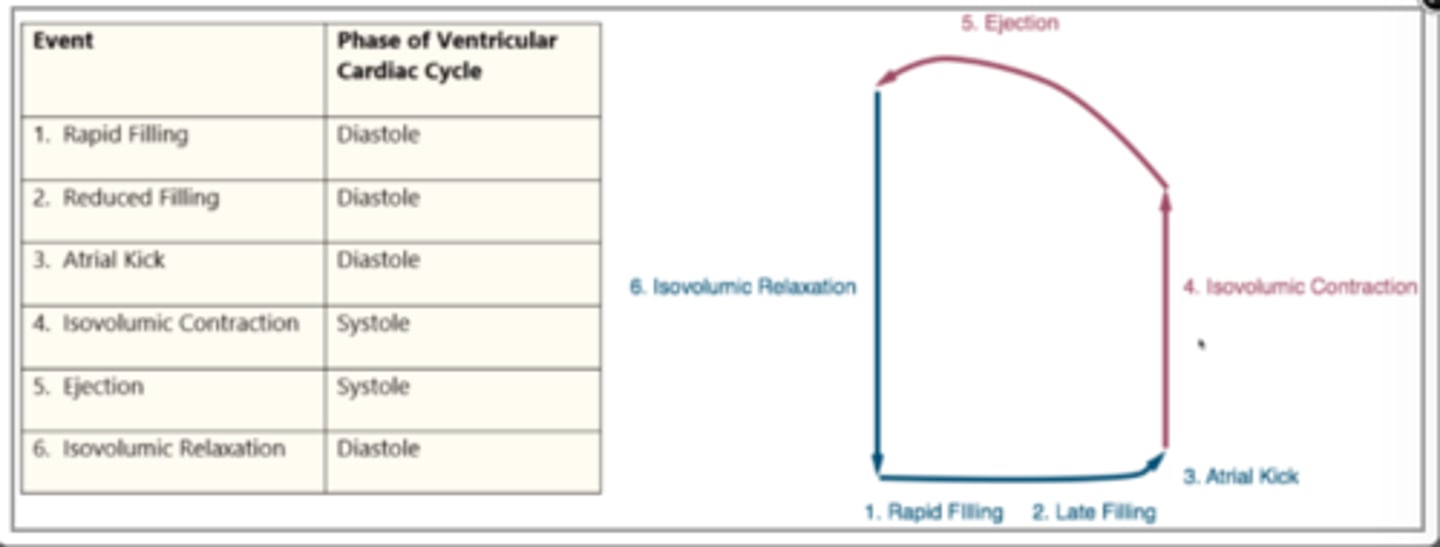
components of the cardiac cycle
- movement of impulse from the SA node to all regions of the heart
- closing and opening of heart valves during each heart beat
- changes in potential gradients in all heart chambers
- changes in blood volume in all chambers of the heart
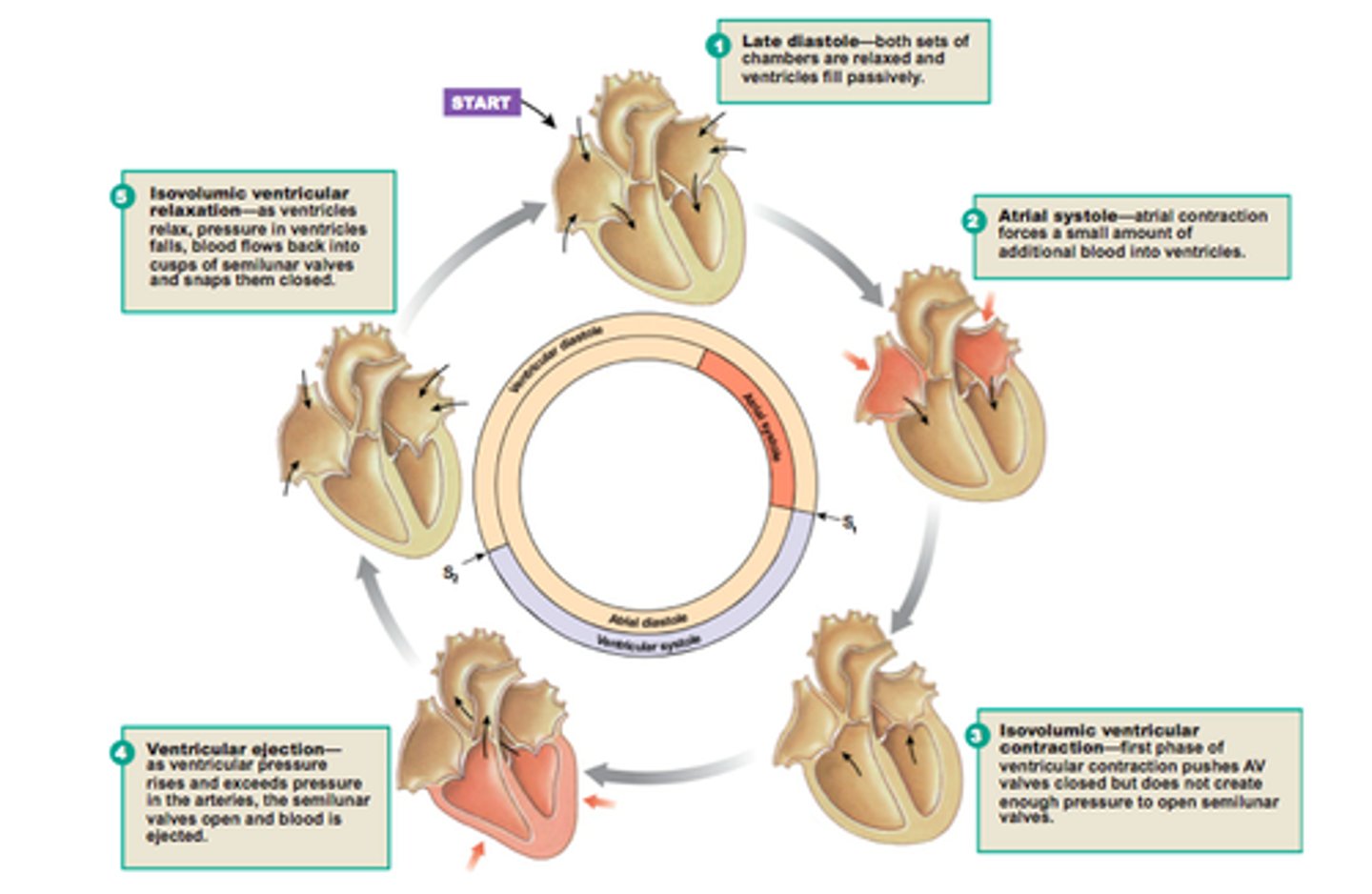
3 Phases of Cardiac Cycle
1. Ventricular filling: mid-to-late diastole
- atrial contraction occurs to eject remaining amount of blood from atria into the ventricles prior to ventricular contraction
- occurs through opening of the AV valves after 80% of blood went to ventricle via passive flow
- remaining 20% ejected via atrial contraction
2. Ventricular systole
- actual ventricular contraction and ejection of blood to aorta and systemic circulation/ body
3. Isovolumetric relaxation: early diastole
- period of passive filling of the heart after ventricular contraction
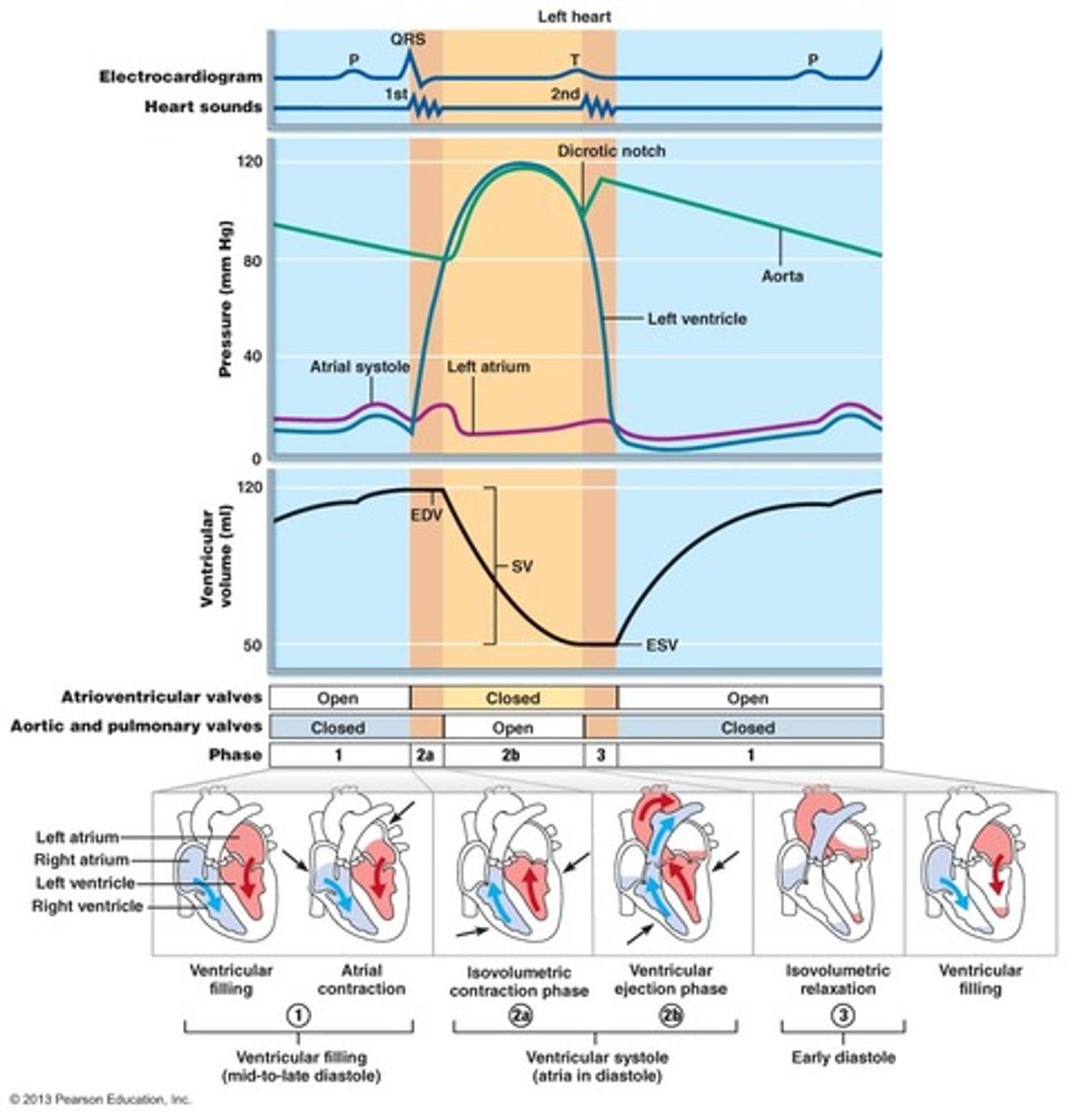
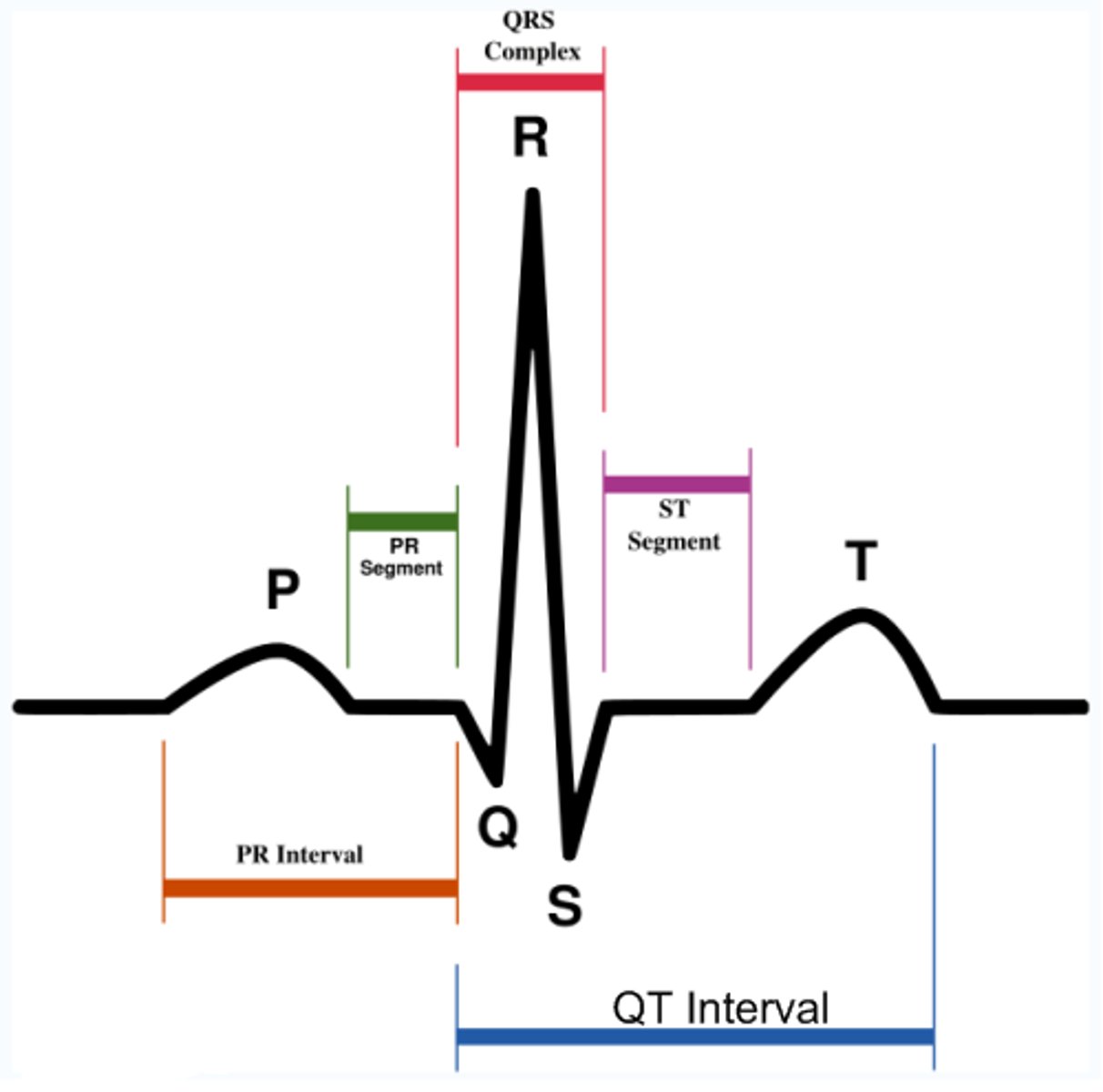
Electrocardiogram (ECG)
electric currents generated by coordinated APs of heart muscle can reach surface of the body and be detected as voltage differences between two points on body surface
- record of volume changes --> ECG
- disturbances in heart function can be detected on an ECG
record of the overall spread of electrical activity through the heart
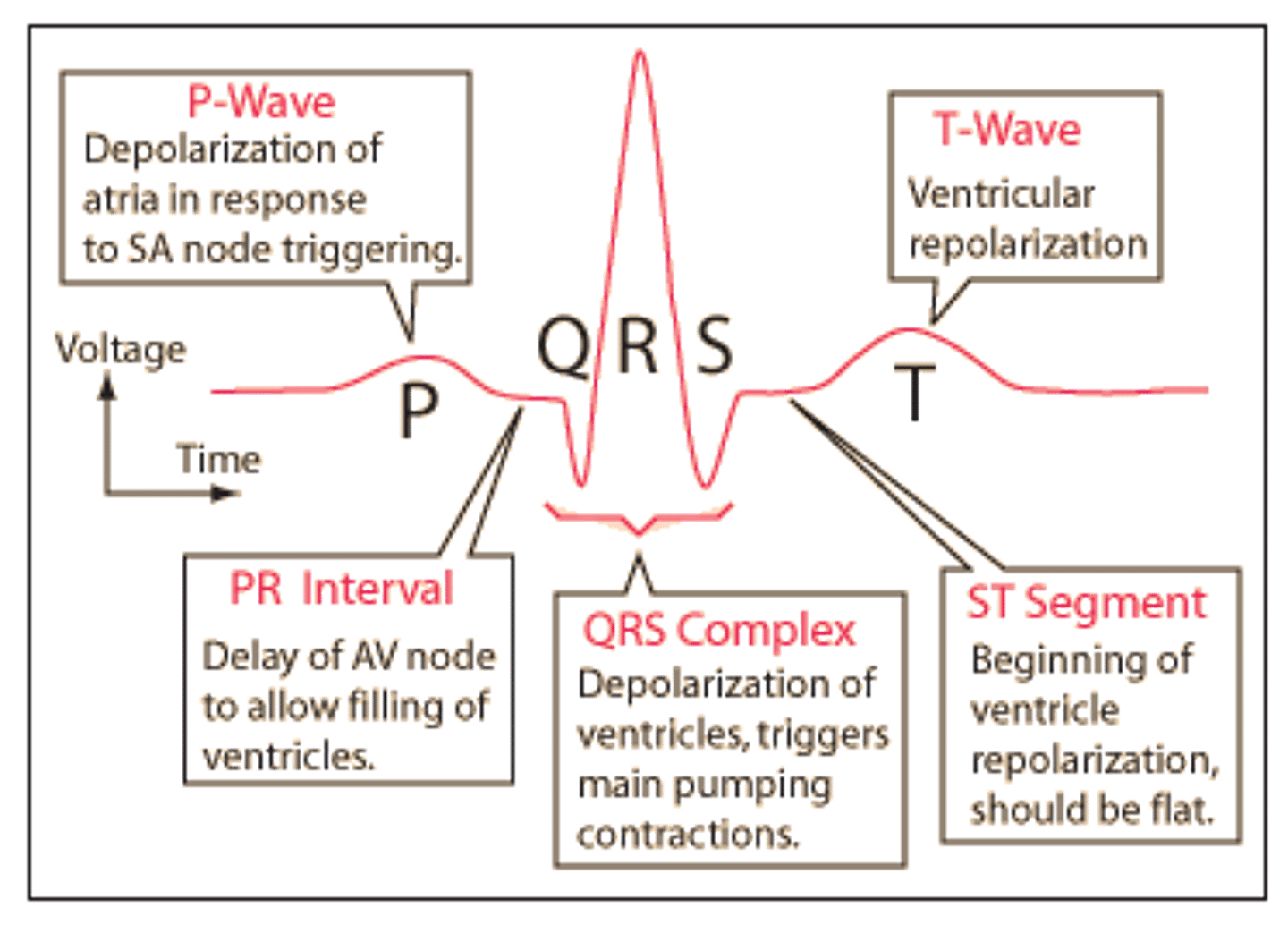
ECG waveforms
P wave: atria contraction/depolarization
PR segment: Following P wave, pause due to AV node (to fill ventricles -- ensuring atria contract before the ventricles)
QRS complex: ventricular contraction/depolarization (atrial relaxation/repolarization occurs during this time but is obscured by ventricular activity)
ST segment: time during which ventricles are contracting/ emptying
T wave: ventricular relaxation/repolarization
TP interval: time where ventricles are relaxing/ filling
depolarization = contractions
atria contract before the ventricles
repolarization = relaxation
atria repolarize before ventricles
summary of cardiac contractile cells APs and RF period
- AP of cardiac contractile cells show plateau phase --> due primarily to activity of slow L-type Ca++ channels
- ensure adequate ejection time
- long RP occurs in conjuction with plateau phase and prevents cardiac muscle cell summation and tetanus -- which would lead to fatigue (unfavored in the heart)
mechanical events of the cardiac cycle
-Ventricular filling=passive filling, AV valve is open
-Atrial contraction=Atrium contracts to squeeze a little more blood into the ventricle
-isovolumic contraction=ventricle contracts, closes the AV valve, however it is not strong enough to open the pulmonary valve,
-ventricular ejection=the pressure in the ventricle is finally higher than the pulmonary, thus the semilunar valve opens and blood is ejected out
-isovolumetric relaxation=as the ventricle relaxes, the semilunar valve closes, but the ventricle is still higher than that of the atrium, thus the AV valve is closed as well
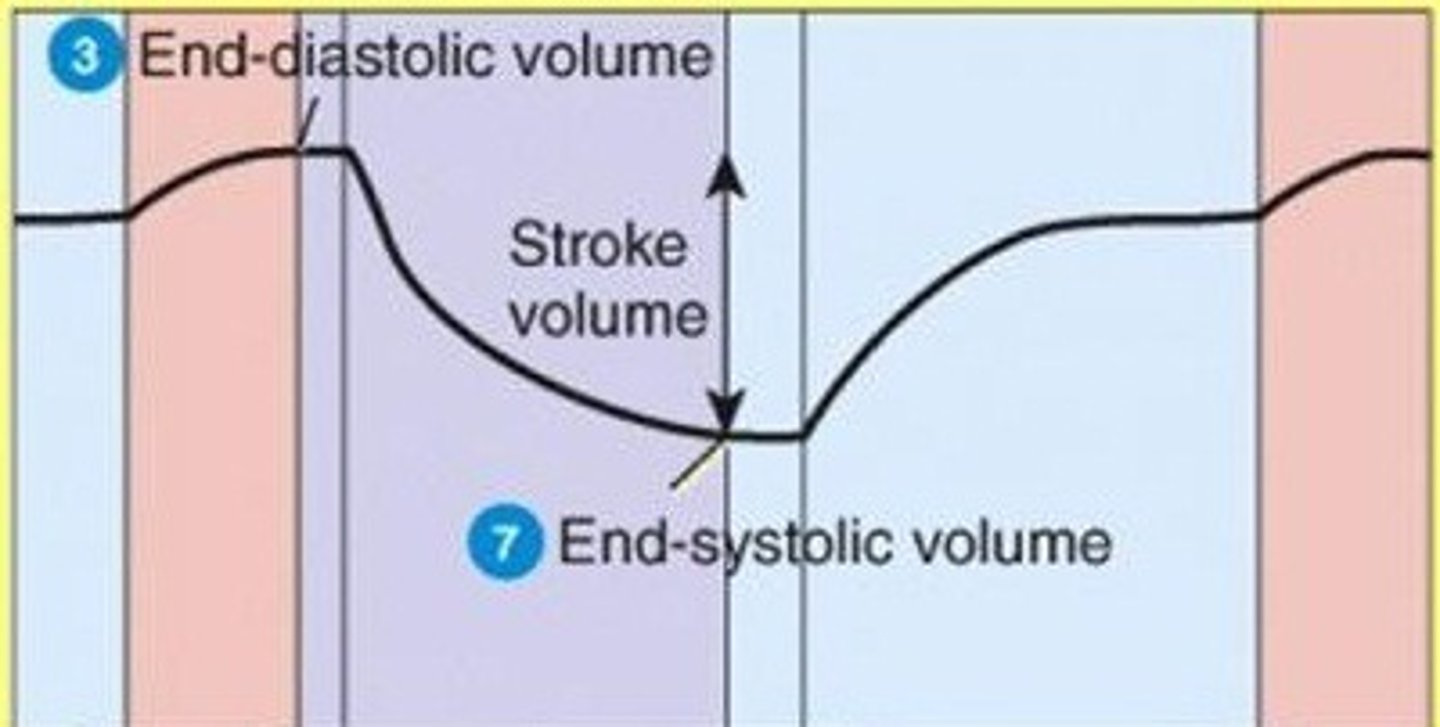
End Diastolic Volume (EDV)
Volume of blood in the ventricles at the end of diastole ("preload")
isovolumetric ventricular contraction
first phase of ventricular contraction pushes AV valves closed but does not create enough pressure to open semilunar valves
- volume does not change in the ventricle
End Systolic Volume (ESV)
Amount of blood remaining in each ventricle at the end of systole (contraction).
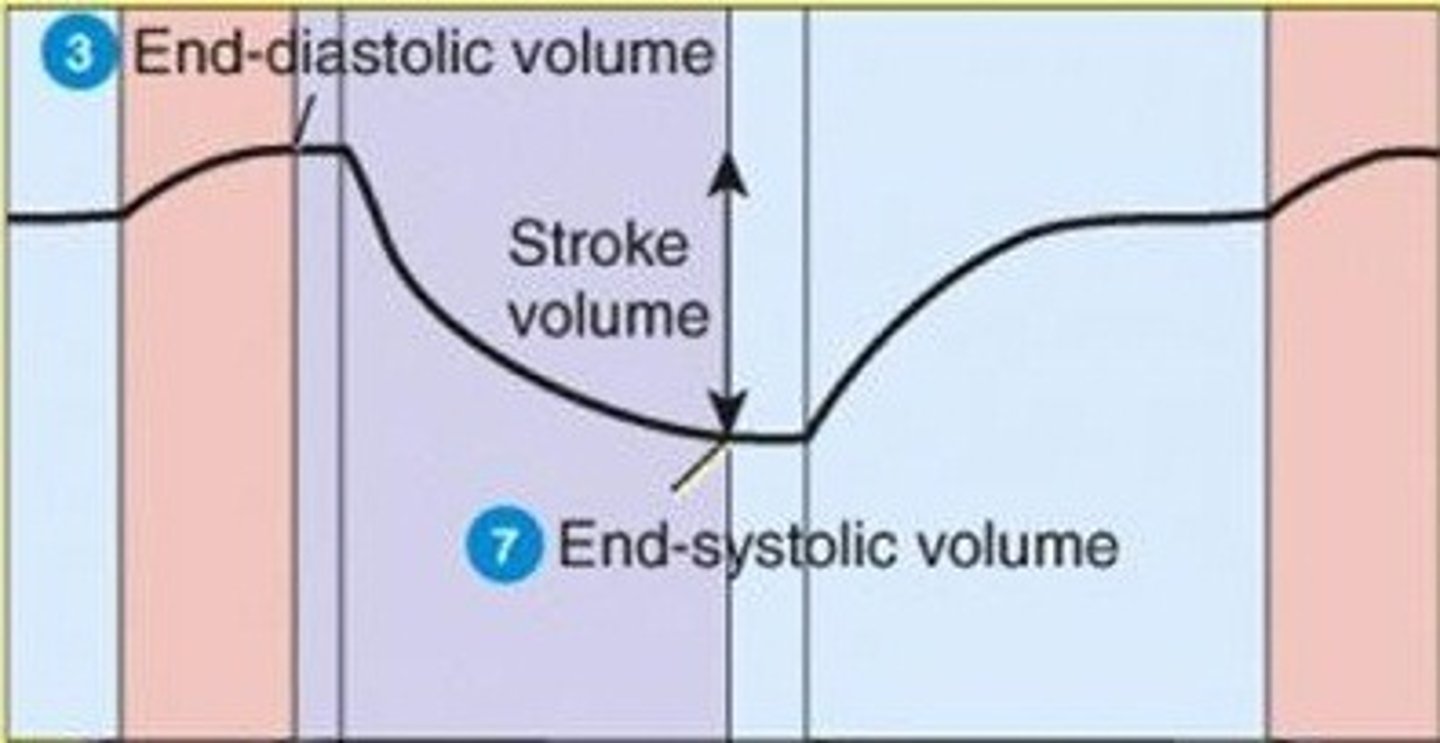
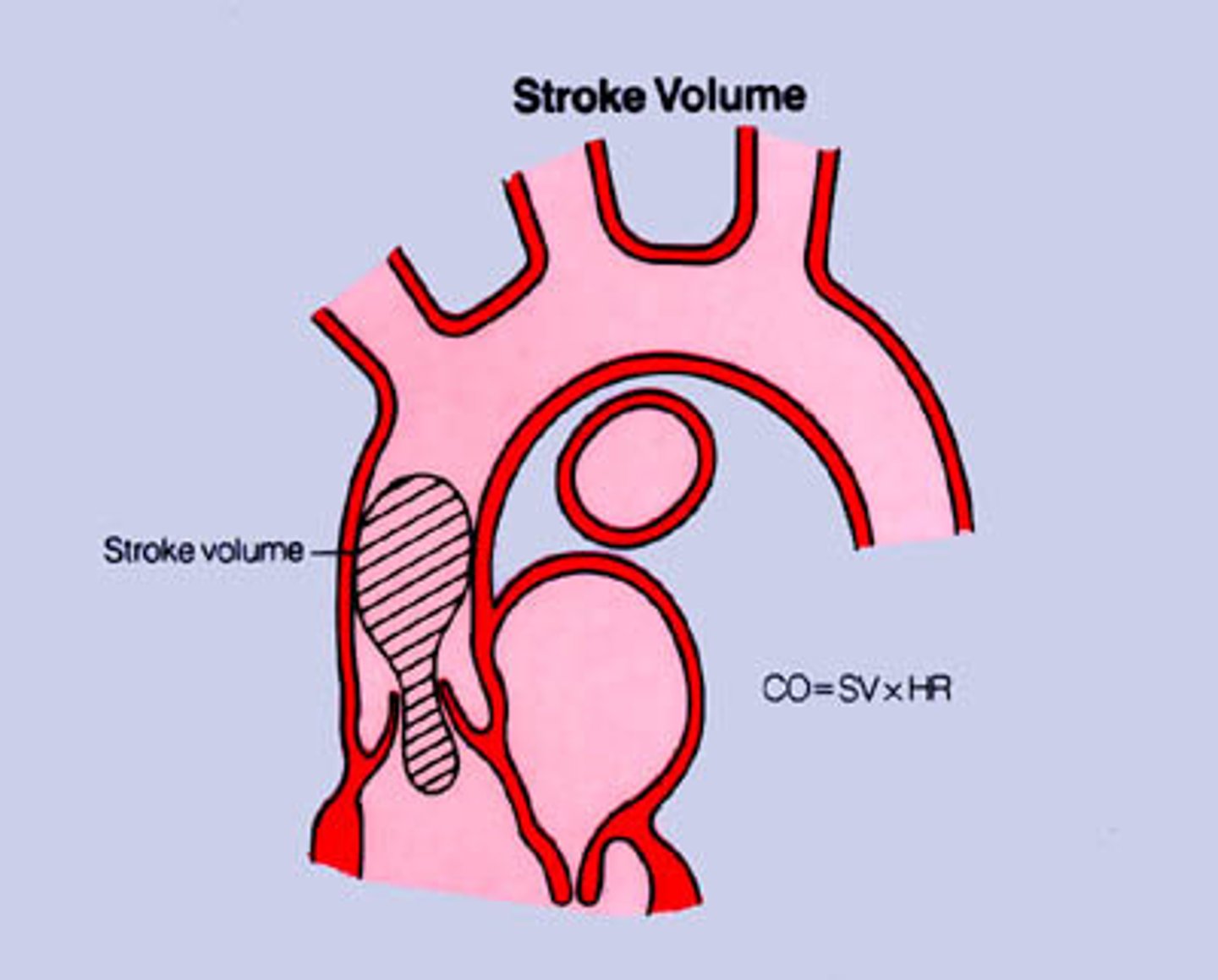
stroke volume
The volume of blood pumped from a ventricle of the heart in one beat
isovolumetric ventricular relaxation
Ventricle relaxes—decreases pressure
AV and semilunar valves closed
No blood entering or exiting ventricle
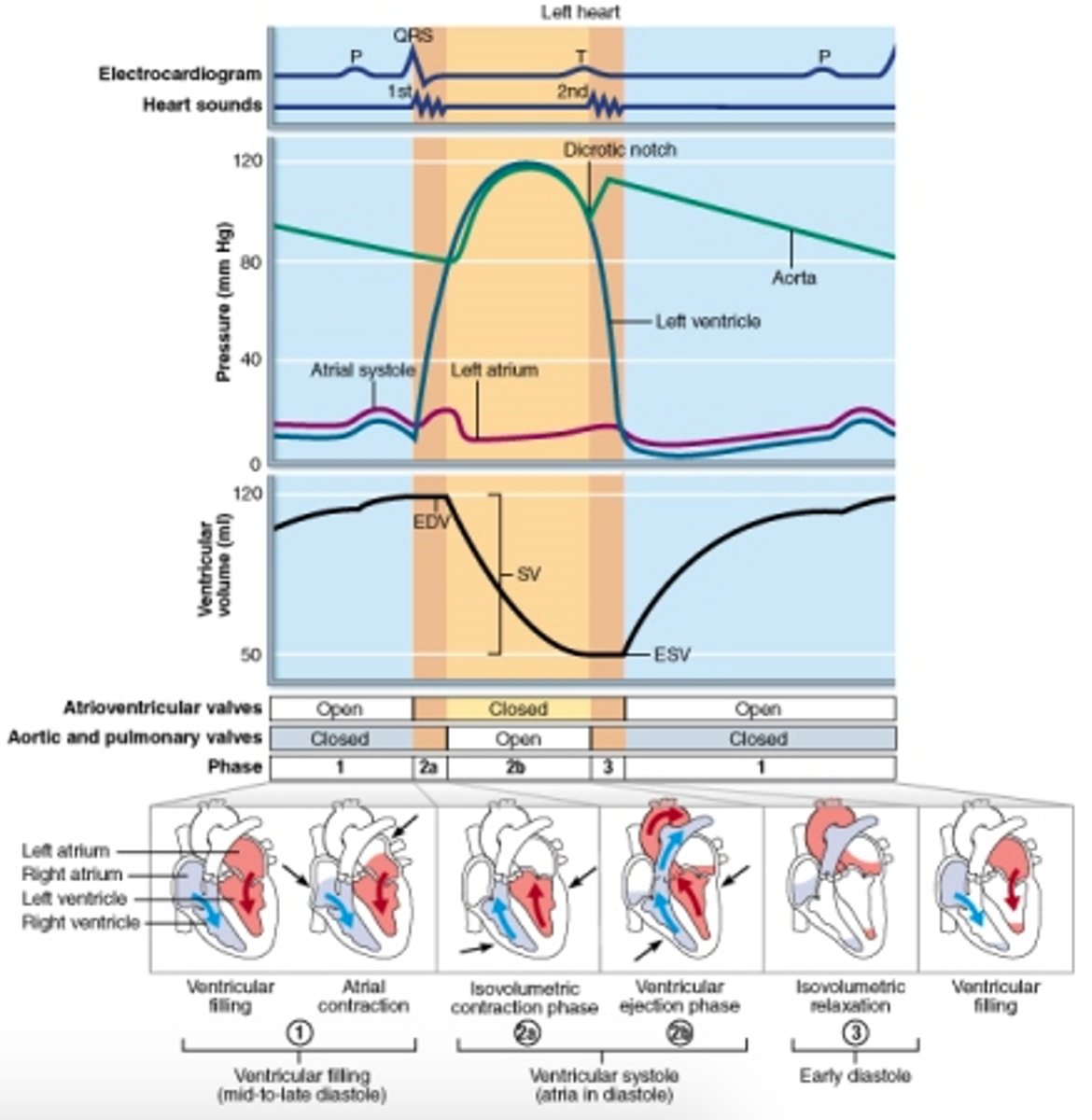
SV equation
SV = EDV - ESV
stages of the cardiac cycle
Blood arrives in the atria- atrial diastole
Rising pressure open AV valves
Ventricles fill with blood- ventricular diastole
SA node initiates impulse/ pacemaker
Impulse spreads across atria
Atria systole
AV node- delays impulse
Bundle of HIS
Purkinje fibres
Ventricular systole
Blood is ejected from the heart
heart sounds
lub - low-pitched, soft, long (closure of the AV valves)
dup - high-pitched, sharp, short (closure of the semilunar valves)
lub and dup refer to valves that are (closing/opening)
closing
4 types of heart sounds
- murmurs
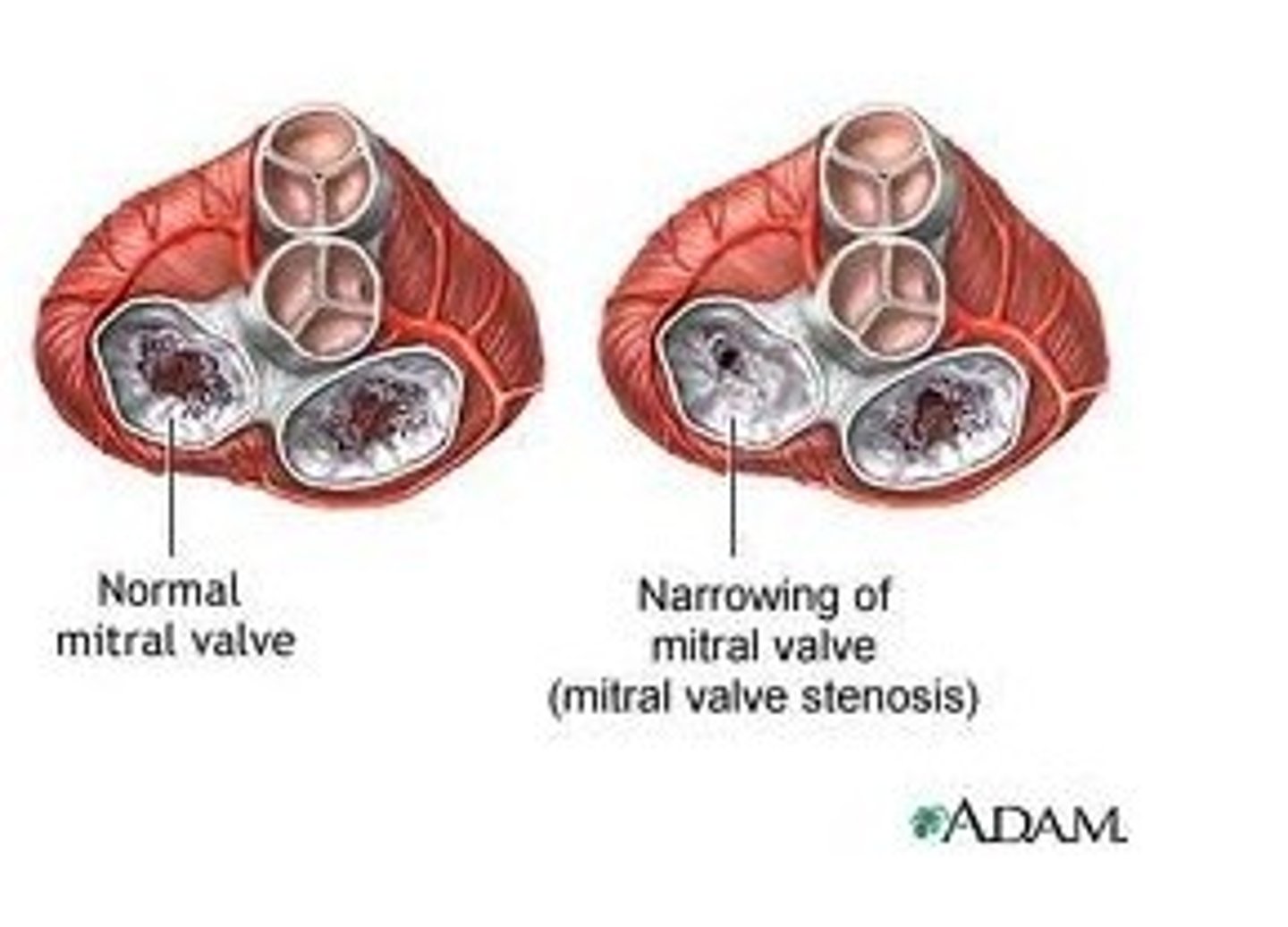
- stenotic valves
- insufficient valve
- rheumatic fever
murmurs
sounds created by abnormal, turbulent flow of blood in the heart
stenotic valve
- fails to open completely, restricting blood flow through valve
- Causes high-pitched sound or clicking as blood is forced through narrow valve
- whistling sound
does not open fully
insufficient valve
- structurally damaged valve that does not close properly,
- turbulence occurs when the blood flows backward through the valve and collides with blood moving in the opposite direction,
- produces an abnormal swishing sound
does not close fully
rheumatic fever
Streptococcus pyogenes is responsible for the infectious disease
- auto-immune disease triggered by a bacterial infection
- leads to vascular stenosis & insufficiency
- increased fever due to infection
lub-whistle-dup
stenotic semilunar valve
- semilunar valve does not open fully
- systolic
lub-dup-whistle
stenotic AV valve
- AV valve does not open fully
- diastolic
lub-swish-dup
insufficient AV valve
- AV valve does not fully close
- systolic
lub-dup-swish
insufficient semilunar valve
- diastolic
- semilunar valve does not close fully
diastole
relaxation/ filling of the heart
systole
Contraction and emptying of the heart
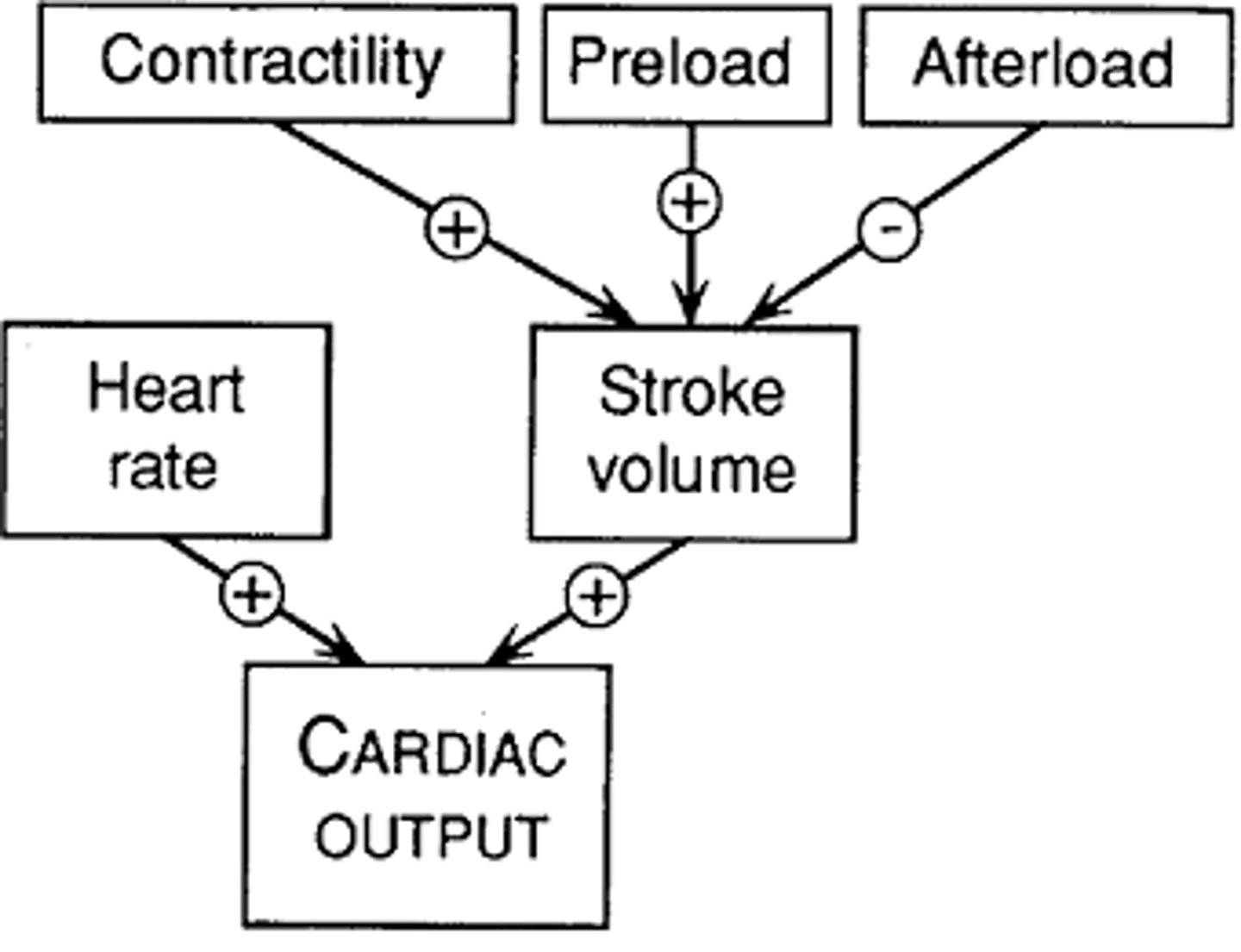
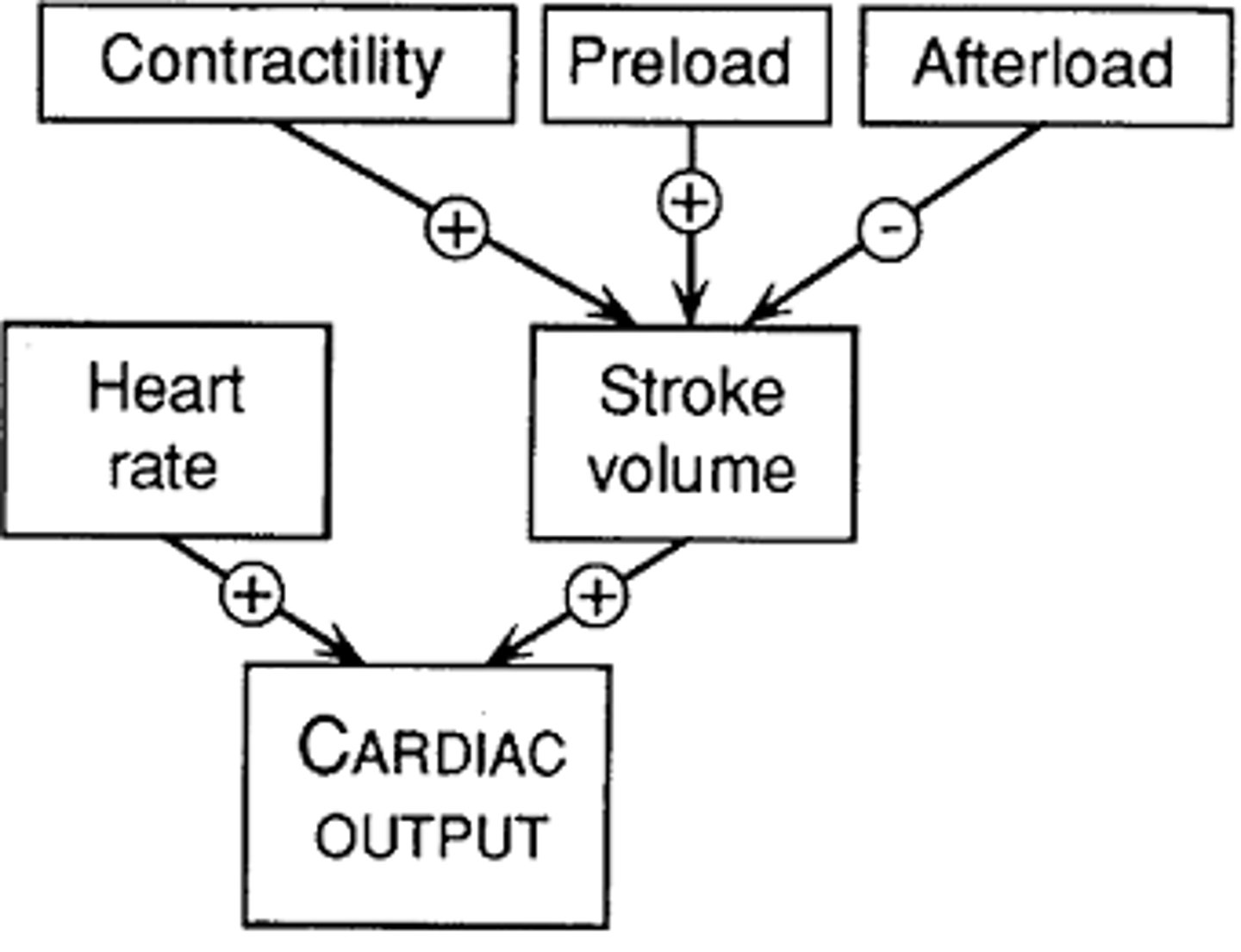
cardiac output
The volume of blood ejected from the left side of the heart in one minute.
CO = SV * HR
heart rate regulation (parasympathetic)
regulation by autonomic influences that control excitability of the SA node
(easier to control due to specific location)
- vagus nerve supplies parasympathetic innervation on SA node, AV node, and contractile cells of the atria
- little to no Parasym innervation of ventricles
- input mediated by NT ACh
- thru muscarinic receptors
ACh causes a decrease in heart rate
Effects of ACh on the SA node
- ACh increases permeability of SA nodal cells to K+
- more K+ efflux due to delaying of inactivation of K+ channels
- cell become hyperpolarized with greater K+ efflux
- decreases amount of APs
Effects of ACh on AV node
- increases K+ permeability of AV nodal cells
- more K+ efflux
- reduces excitability of AV node and delays response to input coming from the SA node
- slows down electrical conduction between nodes
Effects of ACh on atrial contractile cells
- ACh decreases duration of cardiac fiber APs
- reduces Ca++ permeability during plateau phase (less Ca++ comes in)
(amount of Ca++ is directly proportional to strength and rate of contraction)
sympathetic influences on heart rate
nerves supply atria (SA and AV nodes) and richly innervate ventricles
- NE = input
- beta-adrenergic Rs
- increase in heart rate
sympathetic influence on the SA node
NE decreases K+ permeability
- less K+ efflux
- K+ channels are rapidly closed
- less hyperpolarization and more (+) cell potential allowing for quicker depolarizations and more APs
sympathetic influence on the Av node
- increased conduction of velocity in AV nodal cells
- shorter time for AV nodal delay
- slow increase in Ca++ permeability during Ca++ phase of PM potential
- quicker reaching of threshold
sympathetic influence on Bundle of His and Purkinje Fibers
increased electrical conduction as that of AV nodes
sympathetic influence on atrial and ventricular contractile cells
NE increases contractile strength by increasing Ca++ permeability during plateau phase of AP
increased Ca++ in cell = increased strength of contraction
3 phases of the cardiac cycle for every heart beat
1) mid to late diastole (atrial contraction)
2) ventricular systole (contraction of ventricles)
3) early diastole (passive ventricular filling)
SV Regulation
preload, contractility, afterload
increase EDV, change arterial pressure, sympathetic NS
Intrinsically - increased venous return
Frank-Starling Law of the Heart
relationship between preload and stroke volume
the more the heart fills with blood during diastole, the greater the force of contraction during systole
the relatively longer the cardiac muscle fibers, the greater the force of contraction
length-tension relationship of the heart
Frank-Starling mechanism
Relationship between preload and contractility is relationship between length and tension
Preload results in increased sarcomere length, as preload increased, contractility (tension generated by cardiac myocytes) increases
Which direction does sympathetic stimulation shift the frank starling curve?
To the LEFT
- at a given EDV, increased Ca++ via sympathetic stimulation will increase contractile force and SV of the heart
Heart failure and frank starling curve
- inability of CO to meet demands of body
- due to damage to heart muscle or prolonged pumping against arterial blood => stenotic semilunar valve or chronic high BP
Leads to decreased contractility
Shifts FSC to the DOWN and RIGHT
compensations of heart failure
Kidney increases renin and aldosterone secretion (Vasoconstriction and workload)
SNS response increases heart rate
Chambers of heart dilate and cardiac muscle is hypertrophied
Which organs of the body use a lot of blood?
Brain, heart, and skeletal muscle
During rest, kidneys and digestive system, and still skeletal muscles that require a lot of blood
Basic organization of vessels
Arteries to arterioles to capillaries to venules to veins
Microcirculation
Name given to collection of arterioles, capillaries, and venules
Features of blood vessels
Greatest in number - capillaries
Greatest internal radius - aorta (high P)
Total cross sectional area - capillaries
Flow rate
The volume of fluid that moves through a system in a given period of time.
Determined by the pressure gradient and resistance to flow via friction and viscosity
F = change in P/ R
Pressure gradient
the amount of pressure change occurring over a given distance (beginning and end of vessel - change between 2 pts)
Resistance and the three factors it depends on
A material's opposition to the flow of electric current.
Blood Viscosity, vessel length, and radius of vessel
Blood viscosity
the thickness and stickiness of blood due to formed elements and plasma proteins
Increased viscosity = increased resistance
Vessel length
The farther liquid travels through a tube, the more cumulative friction it encounters
Pressure and flow decline with distance
Longer the vessel greater the resistance
Pressure and flow rate decline with longer distances
Vessel radius
most powerful influence over flow, only significant way of controlling peripheral resistance
r^4
Inversely proportional to the 4th power
Increased radius = increased flow rate = increased pressure = decreased resistance
Structure of arteries
Thick muscular walls (lots of smooth muscle)
Elastic and can recoil due to elastin - pressure reservoir
Structure of arterioles
-THICK MUSCLE LAYER= compared to arteries, to allow them to contract and restrict the flow of blood into the capillaries
-THIN ELASTIC LAYER= because the blood pressure is lower than in the arteries
No elastin = no recoil
Structure of capillaries
- capillary wall is one cell thick and has gaps (one layer of squamous endothelium)
- this allows for rapid diffusion between blood and tissues bc short diffusion pathway
- small lumen which gives time for exchange
- provide large SA = decreased resistance compared to arterioles
structure of large veins
Venous valves to prevent back flow
Less elastin - can't recoil - good blood reservoir
endothelium
the specialized epithelial tissue that lines the blood and lymph vessels, body cavities, glands, and organs
Found in all blood vessels
Capillaries are only one endothelium cell
Arteries
Blood vessels that carry blood away from the heart
Low resistance and high flow rate
Elasticity enables acting as a pressure reservoir
Even when heart relaxes, vessel are still pressurized
How can the arteries act as pressure reservoirs?
Due to high elasticity
Driving force during ventricular diastole
- arteries can expand and store pressure imparted by cardiac contractions
- during relaxation —> arterial walls recoil and maintain pressure
Pulse pressure
the difference between systolic and diastolic blood pressure
SP - DP
Mean arterial pressure
pressure forcing blood into tissues, averaged over cardiac cycle
diastolic pressure + 1/3 pulse pressure