Clin chem exam review
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
52 Terms
List the 2 types of disorders of the liver
excretory
synthetic
list 5 things the liver synthesizes
Bile
Proteins
Carbohydrates
Lipids
clotting factors
explain the secretory function of the liver
define cholestasis
stoppage of bile (obstruction)
within hepatocytes (intra-hepatic) or bile duct (extra-hepatic)
what are 3 categories of testing for the liver
functional capacity
serum activity of liver enzyme tests
supplemental diagnostic (liver biopsy etc)
list 4 of the more common functional capacity tests for the liver
BSP or ICG
clearance or retention
BUN & ammonia (NH3)
tests livers ability to convert ammonia to urea
Albumin
exclusively produced by hepatocytes
hypoproteinemia almost always do to albumin loss
Coagulation
many clotting factors synthesized by the liver
how is the liver related to ammonia
liver convert ammonia to urea
why are ammonia levels important
with liver dysfunction , what would ammonia and urea levels be in the serum
when would ammonia tolerance test NOT be a good option
with relation to the liver , why might albumin levels decrease
renal or intestinal disease
nutritional problems
what are three globulin groups
Alpha
Beta
Gamma ( not produced in the liver, produced by immune system)
why is fibrinogen important
needed for clotting
two tests
refractometer
heat precipitation test
why should you not use the jugular for venipuncture on a suspected liver dysfunction
severe bleeding disorders are common with hepatic injury
so taking blood from the major blood vessel is not smart
why should serum and urine samples be protected from light if doing a liver profile
light exposure falsely lowers bilirubin levels, b/c bilirubin breaks down when light exposed
misleading liver profile
why is bilirubin a test for liver function ? how is it related to the liver?
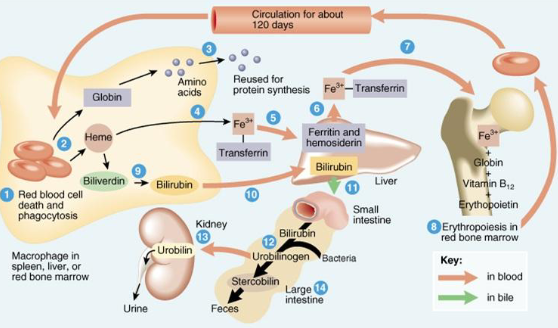
explain start to finish normal bilirubin circuit
RBC breakdown
Hemoglobin breakdown (iron, globin, bilirubin) –in spleen
Bilirubin (unconjugated) binds to albumin to travel to liver*
Liver turns unconjugated into conjugated (“conjugates it”)
Most conjugated travels via bile ducts to duodenum for excretion
and small amount reabsorbed back into circulation (which can be
filtered by normal kidney)
In intestine: bacterial fermentation to urobilinogen/stercobilinogen
Oxidized to stercobilin and excreted in feces. Some urobilinogen
reabsorbed into circulation, or oxidized to urobilin and excreted in
urine
The oxidation creates urochrome that gives colour to urine and feces
what is jaundice
discolouration of body tissues
due to Increased amount of circulating bilirubin in plasma
conjugated or unconjugated
Symptom not disease
typically where can you find unconjugated vs conjugated bilirubin
Unconjugated:
in circulation (blood) bounce to albumin
Conjugated
in circulation (blood) from reabsorption from the intestines
in urine , after reabsorption ( can pass through glomerulus and be filtered out by kidney)
what is the cause for pre-hepatic jaundice, what is the result for bilirubin
due to increased RBC destruction
increase in both unconjugated and conjugated bilirubin
what is the cause for hepatic jaundice, what is the bilirubin result
directly related to liver function
Usually from hepato-cellular damage
Primary defect
Secondary to virus, toxins, hepatic lipidosis
Depending on CAUSE, 2 different results:
1. low conjugating ability = high unconjugated bilirubin
2. high conjugated bilirubin due to leakage from cell damage
what is the cause for post-hepatic jaundice
in ability to excrete bilirubin into the duodenum
often due to biliary obstruction
Conjugated bilirubin is reabsorbed, therefore no reduction in intestines:
o ↓ urobilin in urine
o ↓ stercobilin in feces
Chalky coloured stool*
how are bile acids related to liver function
what serum enzymes indicate liver cell damage , what does it mean if they are elevated
What serum enzymes indicate impaired bile flow? Why would they NOT elevate if there is only primary cell damage
what is phenobarbital
Why is it important to monitor liver function and enzymes while a patient is on phenobarbital
What specifically should you monitor at least every 6-12 months while on the drug
Why are older patients more at risk during anesthesia?
List 3 specific organ related changes with geriatrics
What are some signs of cardiovascular disease?
Which enzyme can be evaluated to determine if there is cardiovascular damage? Why can it be used?
What are some reasons for this enzyme to be falsely elevated?
How is the anion gap calculated
Why is a normal anion gap higher than zero?
What happens to serum bicarbonate levels during metabolic acidosis
. What are the reasons bicarbonate levels may decrease during metabolic acidosis
What are clinical signs of metabolic acidosis?
What happens to serum bicarbonate levels during metabolic alkalosis?
How are albumin and a decreased anion gap related?
What are clinical signs of metabolic alkalosis?
What are signs of hypothyroidism
What serum value would be evaluated to help make this diagnosis
What other tests can be done
In what species is hyperthyroidism more prevalent? What are the signs
What is the parathyroid gland, what does it do, what condition primarily affects it, and what bone result can this cause in the patient
What is Cushing’s?
How do pituitary and primary adrenal Cushing’s disease differ
What are some clinical signs of Cushing’s
What is Addison’s disease
How does the pituitary/adrenal gland/ACTH/cortisol negative feedback loop work? (understand all parts of the loop and the diagrams from the PowerPoint presentation
Which test confirms Addison’s? What would the results be?
Which test differentiates between pituitary and adrenal Cushing’s (not just a screen)? What would the results be?