40. Fractures. Aetiology, symptoms. Biological, physical and clinical assessment of the fracture. Methods of therapy. Cerclage. Intramedullary pinning. Bone plate. External fixation of the bone fractures.
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
58 Terms
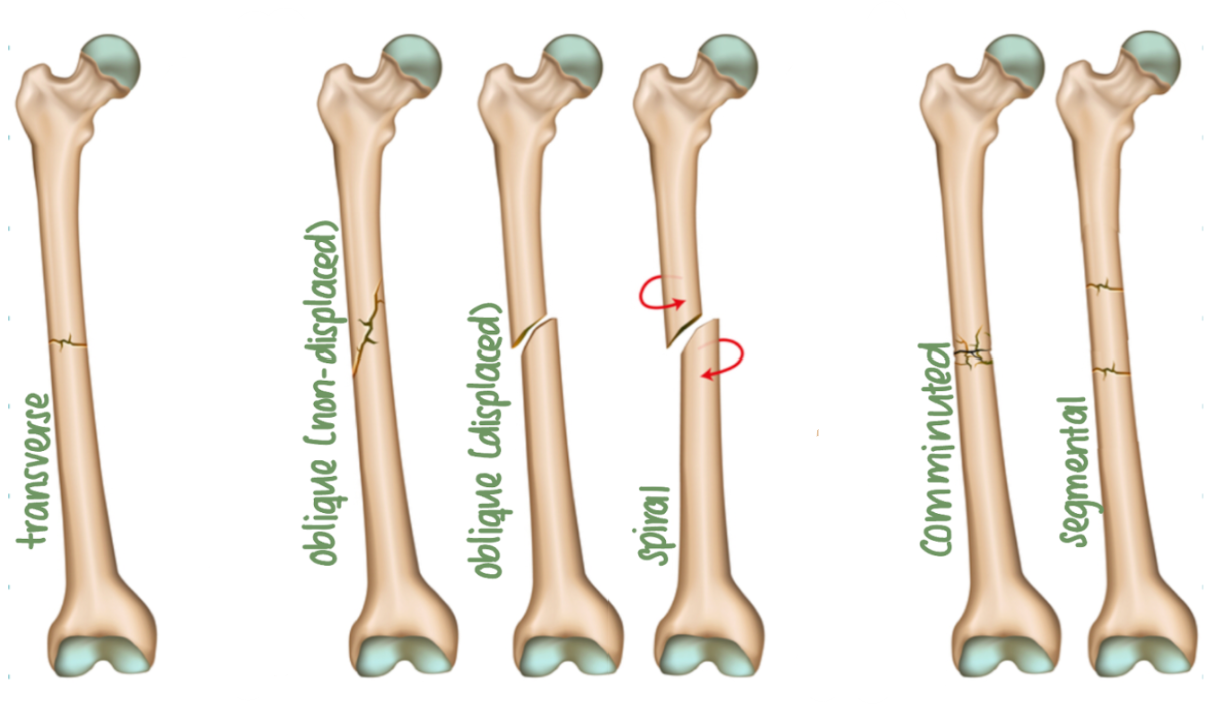
What are examples of complete fractures?
Transverse fracture: at a right angle to bone's long axis
Oblique fracture: diagonal to bone's long axis
Spiral fracture: at least one part of bone has been twisted
Comminuted fracture: bone has broken into several pieces
Segmental fracture: bone has broken in at least two places
Avulsion fracture: bone has been broken off by lig/tendon
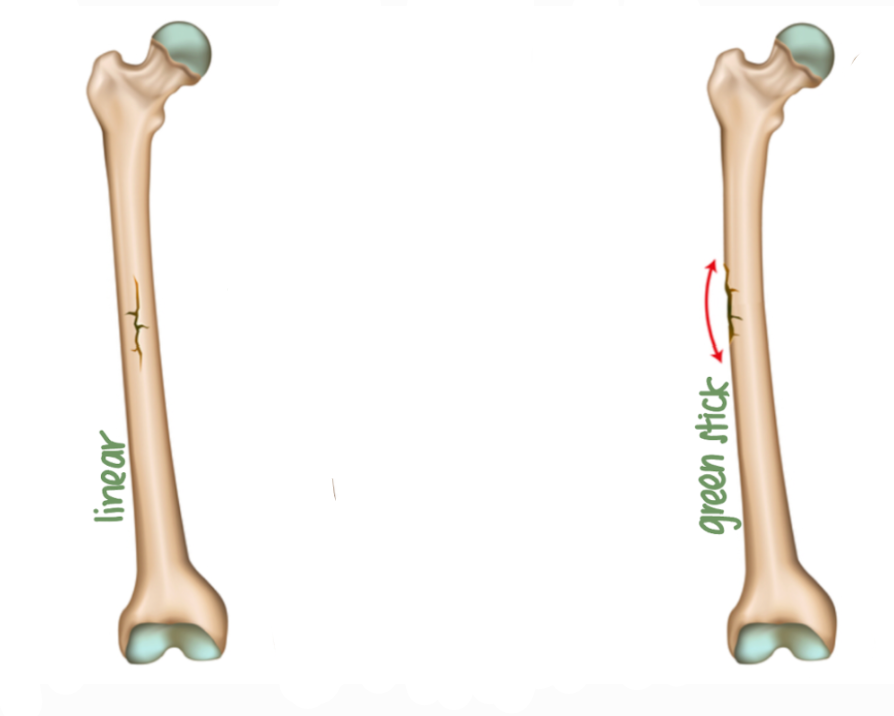
What are examples of incomplete fractures?
Greenstick
Linear
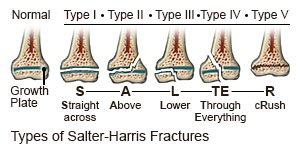
Type 1: Through physis (Straight across)
Type 2: Through physis and metaphysis (Above)
Type 3: Through physis and epiphysis (Lower)
Type 4: Through epiphysis, physis, and metaphysis (Through Everything)
Type 5: Crush injury to physis. (CRush)
X-ray (minimum two views: ML, CrCa).
Haematoma and inflammation
Fibrous callus
Cartilaginous callus
Osseous callus
Bone remodelling
A method to evaluate fracture healing potential. Mostly used for long bones (diaphyseal fractures)
What is each factor of the FAS scored out of?
1 to 10. A higher score means faster healing and lower risk of implant failure.
What types of factors are assessed in the FAS?
Biological (affect how fast bone will heal)
Mechanical (affect how stable the fracture is & weight loading)
Clinical (relating to the patient and their care)
What are examples of biological factors of the FAS?
Age: paediatric patients exhibit significantly faster bone healing than adults or geriatric patients
Soft tissue injury: compromise blood supply to bone, decreasing healing potential
Region of bone affected: bones of distal extremities (radius & tibia) are surrounded by a smaller volume of muscle & soft tissue, thus exhibit an increased rate of delayed fracture union
Health: heal faster than one with health issues.
What are examples of mechanical factors of the FAS?
Fracture configuration: Comminuted, non-reconstructable fractures have lower assessment score
Patient size: larger dogs exert larger forces on fracture, thus have lower assessment score
Presence of single limb versus multiple limb injury.
What are examples of clinical factors of the FAS?
Post-op patient cooperation: active patients are poor candidates for external fixators.
Patient comfort: presence of an external fixator may inhibit normal limb use for some dogs
Owner compliance: owners who are unable or unwilling to perform post operative management for casts are better off having their pet’s fracture managed with internal fixation
How does the FAS help guide treatment decisions?
High: simpler methods (like casts or external fixators) might be enough
Low: more robust methods (like plates or rods) are needed to ensure healing and prevent complications like implant failure
Reposition and stabilise fragments
Promote healing
Restore function
Achieve cosmetic appearance.
External stabilisation
Internal stabilisation
When fracture can be reduced with minimal displacement. Usually incomplete fractures of young, healthy animals
Conservative: Casts, splints, bandage
Surgical: external skeleton fixation
What is external skeleton fixation?
Stainless steel/titanium pins are placed transcutaneous & attached to external pin-gripping clamps & connecting bar
What are indications for external skeleton fixation?
Open fractures (radius, ulna) or across joints. Contraindicated when fracture is unstable
What are some benefits and disadvantages to external skeleton fixation?
Advantage: infections are uncommon, less expensive, wide usage
Disadvantage: Bulky for animals
What are the types of frames used in external skeleton fixation?
Half-pin splintage
Full-pin splintage
Combination
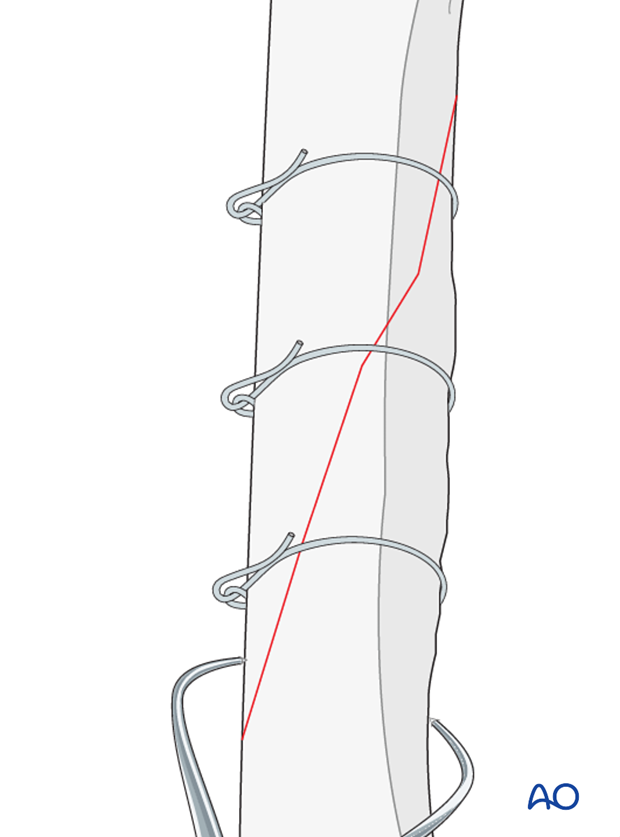
Cerclage wire
Intramedullary (IM) pins
Bone plates and screws.
Spiral or oblique fractures, combined with IM pin or fixator (Not strong enough to be used as the sole means of repair of diaphyseal long bone fractures)
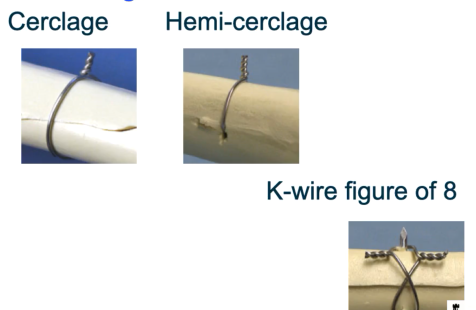
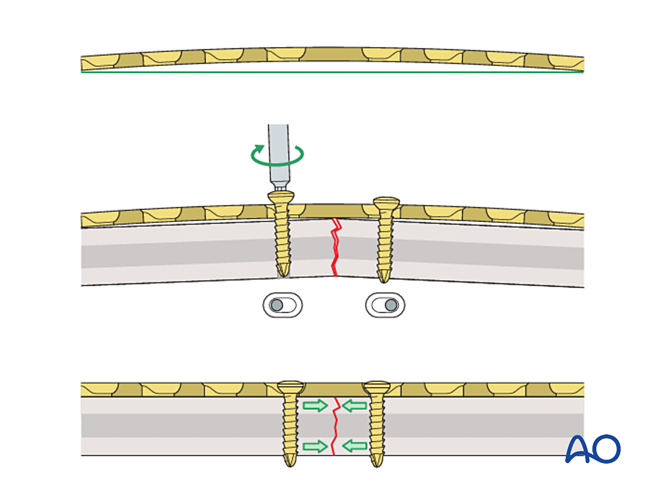
What is full cerclage wire?
Utilises 360° circumferential wire placed around bone at a fracture site. This use is generally restricted to diaphyseal segments of long bones.
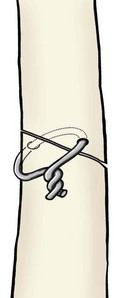
What is hemicirclage wire?
Wire is placed through (not around) main fragments of bone. Other components of fracture are then enclosed in wire to hold them firmly to main fragment
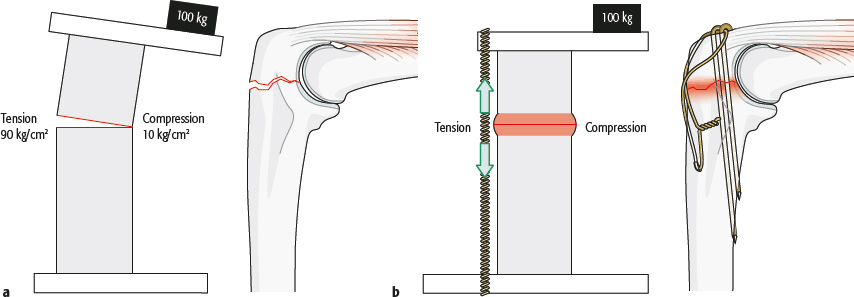
What is tension band wiring?
A specialised form of hemi cerclage. Use 2 K-wires
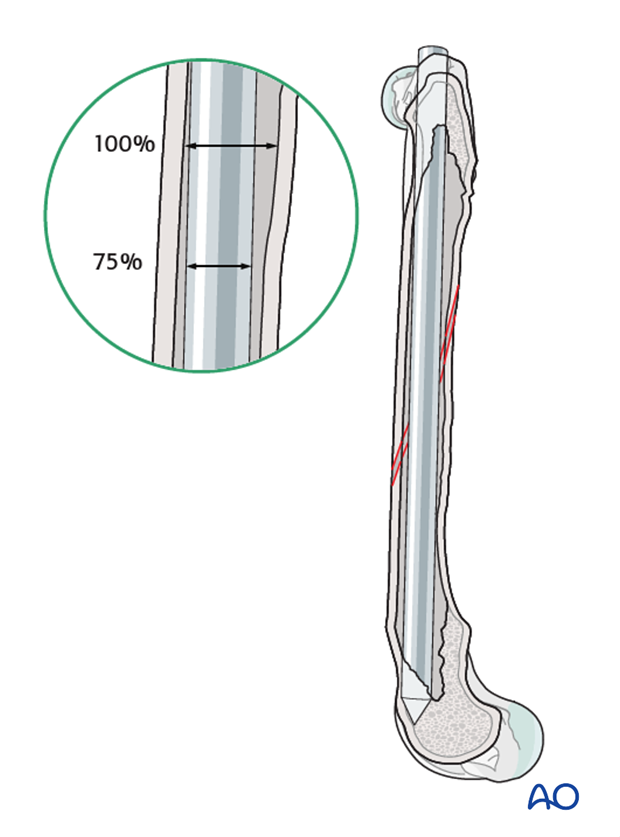
What is the principle of intramedullary pins?
Internal fixation in which pins are inserted into medullary cavity of bone & left in for 6-8 weeks. IM pin must fulfil 75% of IM cavity.
IM pins function to resist bending forces placed on fracture site, however an IM pin alone cannot resist rotational forces. Therefore, any fracture is rarely suitable for IM pinning alone, unless fracture interdigitates after reduction
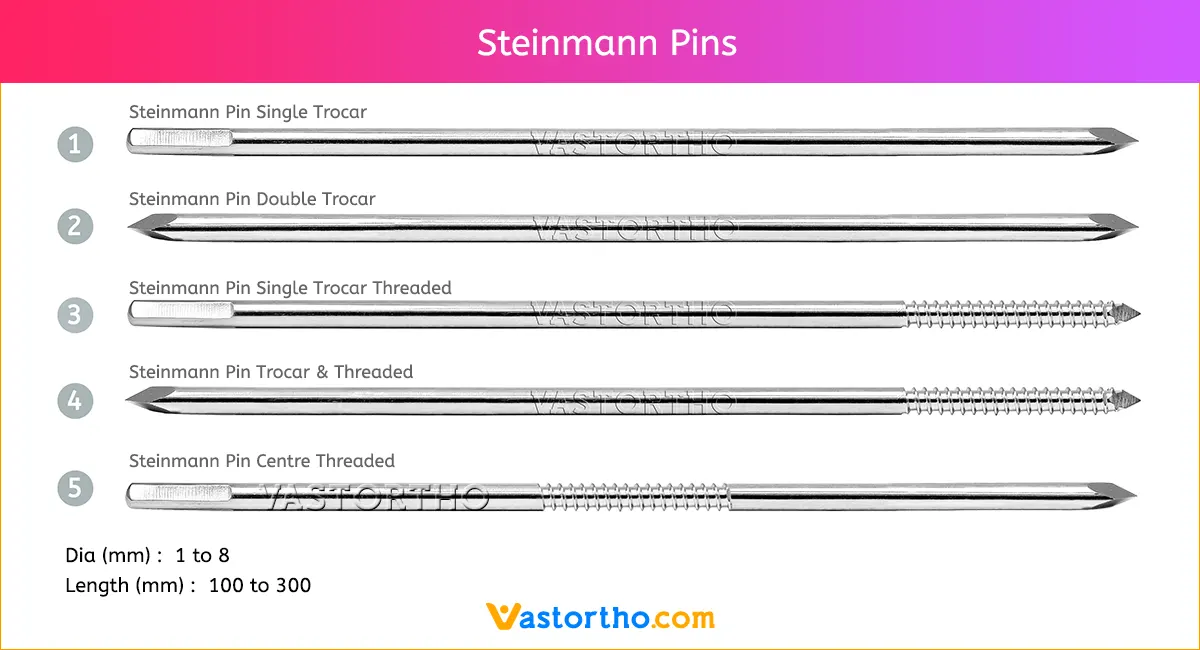
Steinmann pin
Kirschner wire
Rush pin
Kuntscher nail
Normograde: drill through both sections at once. From unaffected bone to the fracture site to other side. Preferred over retrograde - minimally invasive.
Retrograde: drill from fracture site into bone. Then down into other half of the bone. Performed when normograde cannot be performed likely due to risk of damaging joint.
Adding wires
External fixator
Multiple pins
Plate and screw fixation.
What type of material is used for bone plates/screws?
Titanium (biocompatible)
What types of fractures can bone plates and screws be used for?
Versatile & can be used for most types & locations of fractures
What is the function of bone plates?
Plates neutralise forces (bending, rotation, compression, tension) placed on bone. Plates can be used w/ IM pins for extra support.
What are considerations for removal or leaving bone plates in place?
Most plates are left in place, though some may be removed.
If the animal is growing then remove plates once fracture is healed to avoid bone complications. If older patient - just leave it. Removing plate can be deemed unnecessary surgery.
What are examples of bone screws?
Cortical screws: Designed for dense bone.
Cancellous screws: For spongy bone.
Self-tapping and non-self-tapping screws.
Locking screws: Lock into the plate for additional stability
What types of holes can be drilled into the bone fragments to prepare for bone screws?
Gliding hole: Matches screw diameter. Screws glide and don’t hold proximal segment. Without a gliding hole, the screw threads will engage in both the proximal and distal segments, preventing compression.
Threaded hole: Smaller diameter (equal to or less than diameter of the core), drawing the distal bone segment towards the proximal segment with the gliding hole, facilitating compression
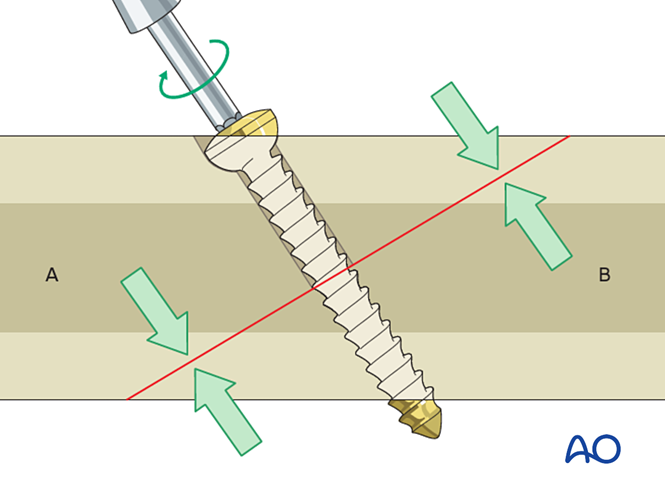
At what angle to the fracture should holes be drilled?
90 (perpendicular)
What are the main types of bone plates?
Classic plates: Screws fix the plate to the bone.
Locking plates: Screws lock into the plate itself, maintaining stability, often used in bridging techniques for complex fractures.
Dynamic Compression Plates (DCP): Sloped holes allow the screw to compress bone fragments as it's tightened.
What are the main concepts of bone plates?
Protection (neutralisation)
Compression
Bridging
Buttress (antiglide)
Plates with sloped holes that compress bone fragments when screws are tightened.