HIPAA, Integrity, Code of Ethics
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
38 Terms
What does HIPAA stand for?
Health Insurance Portability and Accountability Act.
What is the primary purpose of HIPAA?
To protect patient privacy,
Ensure the security of health information, and
Enhance healthcare efficiency.
What are the three main principles of HIPAA?
Confidentiality,
Integrity,
Availability.
Why is patient confidentiality important?
It builds trust, is a legal and ethical obligation, and upholds patient rights.
What is considered PHI?
Any information that can identify a person
Including personal identifiers, medical information, and payment information.
What types of data need to be protected under HIPAA?
Written documentation, spoken information,
Electronic databases, photographs, audio, and video recordings.
What is a Tier 1 civil violation under HIPAA?
Unaware of the violation and exercised reasonable due diligence.
What is the penalty for Tier 4 civil violation of HIPAA?
Minimum $50,000 per violation, maximum $1.5 million per year.
What constitutes a criminal violation of HIPAA?
Deliberately obtaining and/or disclosing PHI without authorization.
What is the penalty for Tier 3 criminal violation of HIPAA?
Up to 10 years in jail and a $250,000 fine.
Is it a HIPAA violation to share patient information with an authorized technician in the elevator?
Yes, due to the lack of privacy in that setting.
What can result from a breach of HIPAA?
Reputation damage, trust erosion, and legal consequences.
Post Conference is held in the cafeteria. Is it a HIPAA violation?
Yes, if patient information is discussed in a public setting without ensuring privacy.
Scenario 1: A nurse shares patient information with a radiology technician who is authorized to receive the information.
No
Why? HIPAA allows the sharing of PHI (Protected Health Information) with other healthcare professionals who are directly involved in the patient's care. Since the radiology technician is authorized to receive the information, this does not constitute a violation.
Scenario 2: A nurse shares patient information with a radiology technician who is authorized to receive the information, but discussion takes place in the elevator?
Yes
Why? HIPAA requires confidential patient information to be discussed in private settings. An elevator is a public space, where unauthorized individuals may overhear sensitive information. This would be considered an inadvertent disclosure of PHI, violating HIPAA's Confidentiality Principle.

Scenario 3: Your patient’s family member is calling for an update. A HIPAA violation?
Yes, unless proper consent is obtained.
Why? A nurse cannot share a patient’s PHI with anyone (including family) unless the patient has provided explicit permission. HIPAA protects patient privacy, and information should only be disclosed if the patient has authorized their family members to receive updates.
You mistakenly brought home a document from a patient that contains PHI. A HIPAA violation?
Yes
Why? Taking patient records, reports, or any documentation containing PHI outside the healthcare facility violates HIPAA regulations. Even if unintentional, losing or exposing that information could compromise patient confidentiality. All PHI should be securely stored and disposed of according to facility policy.
The nurse is charting. A code blue is called, and the nurse runs to help. A HIPAA violation?
No, in emergencies patient care takes precedence. HIPAA allows for necessary disclosures to provide immediate medical assistance.

How many Tiers are listed to categorize the level of criminal violations & penalties?
There are three (3) tiers: Tier 1, Tier 2, & Tier 3
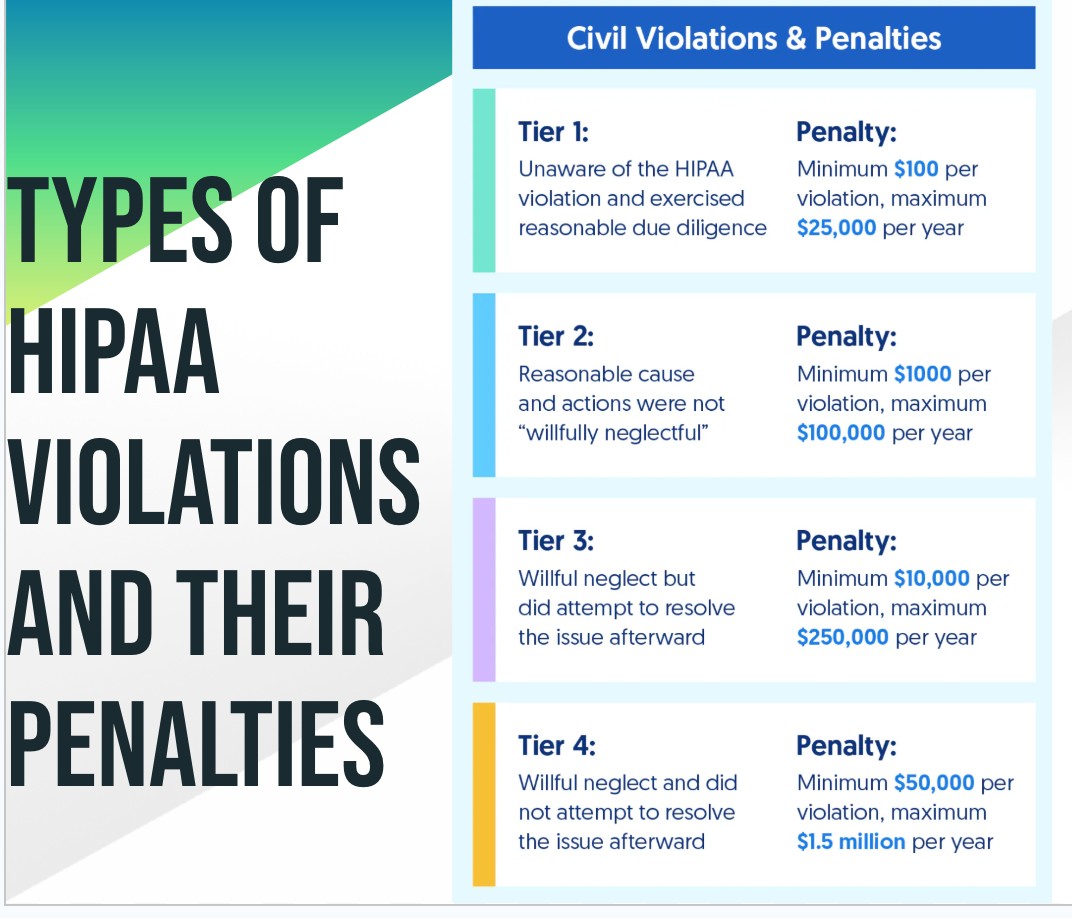
How many type of HIPAA Tier civil violations & penalties?
Four tiers: Tier 1, Tier 2, Tier 3, and Tier 4.
When can PHI be shared with a third party?
✅ Treatment – Sharing PHI for patient care coordination
✅ Payment – Billing, claims processing, verifying insurance coverage
✅ Healthcare Operations – Quality assessment, audits, business management
Which of the following actions should a nurse take after witnessing a breach of a client's confidentiality in a provider's office?
Complete a health information privacy complaint form.
Rationale:
It is the nurse's responsibility to submit complaints to the proper agency regarding a breach of client confidentiality.
When reporting a HIPAA violation, the nurse must remember that any reporting must be?
The complaint should be signed by the person originating it. HIPAA prohibits retaliatory action being taken against an employee who files a complaint.
When a HIPAA violation has occurred, who is responsible for notifying the agency of a breach?
The nurse or covered entity should notify the agency of a breach.
It is not the client's responsibility to notify the agency of a breach.
However, the covered entity should notify a client when there is suspicion that their information has been compromised.
A nurse in the emergency department is caring for a client following a motor-vehicle crash. The client is unresponsive and the client's spouse is not present at the facility. Which of the following actions should the nurse take to assist with obtaining consent for the client's surgery?
The nurse should attempt to contact the spouse or another legally authorized representative to obtain consent.
If unable to reach them, the nurse may proceed with surgery under implied consent due to the client's medical emergency.
Rationale:Because the client is not cognitively or physically able to provide consent, it is within HIPAA guidelines to discuss the client's condition with a spouse, close relative, or friend. Informed consent guidelines mandate obtaining consent from the client's closest adult relative in an emergency situation because it is deemed in the best interest of the client.
A group of nurses on a clinical unit are planning to research the incidence of falls among clients following joint replacement surgery. Which of the following actions should the nurses take to ensure the study complies with the HIPAA Privacy Rule?
Submit their proposal to the institutional review board for review and describe how they will de-identify client information.
Rationale:
Research using client records can be done if client information is de-identified. It is the responsibility of institutional review boards to determine if a study meets this criterion.
A newly hired nurse is reviewing information about the HIPAA Privacy Rule during facility orientation. Which of the following statements by the nurse indicates an understanding of the Privacy Rule?
"I can give information about a client over the phone if the client gives permission."
Rationale:
Information about a client can be given over the phone if the client has granted permission for that person to receive information. Many facilities have implemented an access code system that requires the person asking for information to provide the code.
Are patients allowed to read their charts?
Yes! patients have the right to read their medical records.
However, facility policies can govern how this is carried out and what health care personnel must be in attendance.
Why should client admitting diagnoses NOT be posted on the unit floor you work at?
Posting client admitting diagnoses in a public location is a breach of confidentiality.
This information should be made available only to health care providers, either electronically or on paper in a secure area.
A client tells a nurse that they feel their privacy has been violated and wants to file a formal complaint with someone other than the medical facility. Through which of the following agencies should the nurse instruct the client to file the complaint?
Office for Civil Rights (OCR)
Rationale: The OCR investigates complaints by clients and other involved individuals related to the HIPAA Privacy Rule. If the client wants to file a complaint to someone in the medical facility, the nurse should arrange for the client to talk to the facility's Privacy Officer.
Which of the following methods of information exchange can occur without client authorization?
Walking rounds that involve two nurses discussing an assigned client at the client's bedside in a private room
Rationale:
This practice is acceptable if the two nurses are both assigned to this client and no one else is in the room. It is within the client's rights to hear information about their own care and treatment.
After a patient comes forward to complain about a privacy or HIPAA violation, who should the nurse report the incident to?
Privacy Officer is the first person to inform about the incident.
Reporting to the Privacy Officer ensures that the complaint is addressed according to facility protocols and HIPAA regulations.
If a breach of information occurs or is suspected, the covered entity must complete a breach notification to which governmental agency?
It must complete a breach notification form that is directed to the Secretary of the Department of Health and Human Services (HHS).
The Privacy Rule covers all medical records and other individually identifiable health information held or disclosed by a covered entity in any form, whether communicated electronically, on paper, or orally EXCEPT?
Psychotherapy notes (used only by a psychotherapist)
Held to a higher standard of protection because they
Not part of the medical record and are never intended to be shared with anyone else.
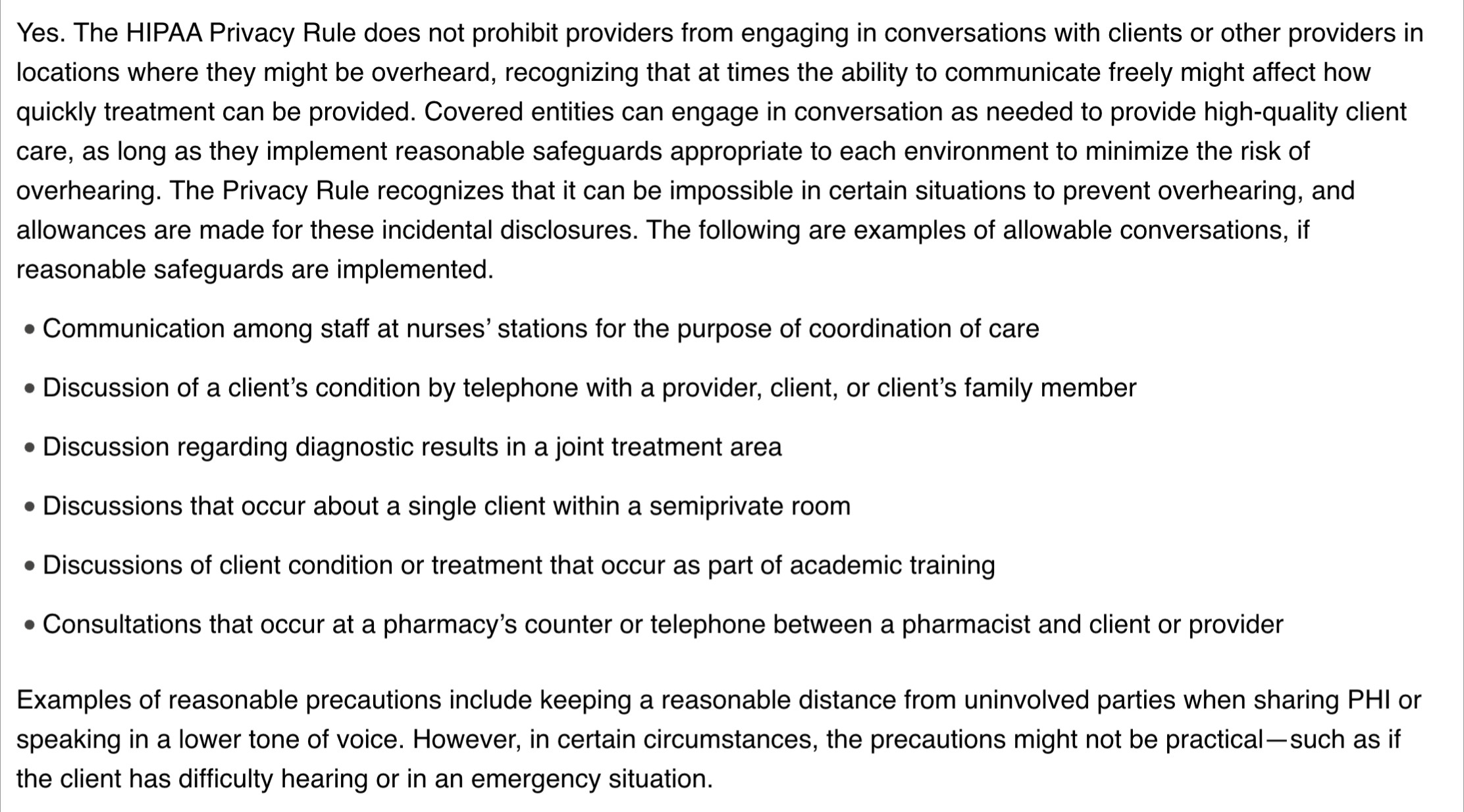
Does the HIPAA Privacy Rule require hospitals and provider offices to be retrofitted with private rooms and soundproof walls to avoid any possibility of overhearing a conversation?
No, the HIPAA Privacy Rule does not mandate specific architectural changes like retrofitting with private rooms or soundproof walls.
However, it does require covered entities to implement reasonable safeguards to protect patient privacy and confidentiality.
Can health care providers engage in confidential conversations in environments where there is the possibility of being overheard?
Yes, health care providers can engage in confidential conversations in such environments, but they must take reasonable steps to minimize the risk of being overheard.
Are medical and nursing students, medical residents, and other medical trainees prohibited from accessing clients’ PHI in the course of their training?
No, they are not prohibited from accessing PHI as long as it is necessary for their training and they are under appropriate supervision and adhere to confidentiality rules.
Does the HIPAA Privacy Rule prohibit obtaining information from client’s via telephone, such as to gather preoperative information, prior to the client obtaining or acknowledging the covered entity’s privacy notice?
No, the HIPAA Privacy Rule does not prohibit obtaining information via telephone as long as the covered entity provides the privacy notice in a timely manner and ensures the client's understanding and consent.