LAM: Exam 1
1/64
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
65 Terms
Immunization protocols in horses
What
Core: Tetanus, EEE, WEE, WNV, Rabies
tetanus toxoid and killed virus vaccines: alum adjuvant
Risk-based: E. influenza, herpesvirus, strangles, EVA, VEE, botulism, rotavirus, Potomac, anthrax & more
When
Mares: re-immunized during 3rd trimester
Foals: colostral Ab, then vax 4-6, 7, 12m
Adults: priming series then annual boosters
2-3 injections at 1m intervals
Rxn: purpura hemorrhagica (Strep equi), clostridial myonecrosis (bad technique)
Record lot/serial # + report to USDA/manufacturer
Considerations for control of animal contact & movement
Outbreaks of equine infectious dzs typically occur via
Comingling
Introduction of comingled &/or new animals onto individual
premises
Prevention
Separation
Entry requirements
Isolation and quarantine protocols
Regulatory surveillance, including veterinary inspections & travel requirements
Immunization terms
Active immunization: stimulates an individual's immune system
Toxoid: bacterial toxin that has been chemically altered or inactivated
Adjuvant: added to boost and enhance the immune response
Antiserum: blood serum containing specific antibodies
GI Parasite Control in Horses
Major Types: 4 types: ascarids (foals), SM/LG strongyles (adults), tapeworms
Small strongyles (cyathostomins) - most common
Large strongyles (“blood worms”)
Tx: Use Fecal Egg Count & treat high-shedder adults, don't treat resistant individuals, pasture management, manure removal - tailored to each indv. farm!
Nematodes: Benzimidazoles, ivermectin, moxidectin, pyrante → applied / single dose / oral drench
Adults: Treat all yearly w/ macrocyclic lactone for S. vulgaris!! (LG strongyles)
Foals: benzimadazoles q 60 d for first 1y for ascarids
Larvicidal deworming: high-dose benzimidazoles x multiple days!!
Tapeworm: Praziquantel & pyrantel
Fluid Loss in Horses
MOA: water is drawn into intravascular space leading to hypovolemic shock
Normal: urine, respiration, skin evaporation
Pathologic: enteritis/colitis, hemorrhage, gradual reduced intake, effusions, sweating, rapid
Cs: dry MM, concentrated/decreased urine, low GFR, tachycardia, vasoconstriction, poor perfusion, organ failure/death
Tx: IV or Oral fluids
Adult: 50 ml/kg/d **
25 L/day for 500 kg horse = 1 L/hr for a average horse **
Minor fluid deficits: w/out loss can be corrected w/ 5-20L of fluid/per 500 kg horse
Neonate: 100 ml/kg/d
5 L/day for 50 kg foal = 200 mL/hr
Shock: 40L/500kg horse
Ongoing: 60-120 L/day
Oral fluids in Horses
Use: Minor fluid loss
Equipt: NG tube
gravity safer than pump
Rx: plain water, hypotonic electrolyte solution (Lg amounts)
Dose: 5 L/500kg
IV fluid use in Horses
Dose: fluid challenge principle (give ¼ deficit rapidly, reassess, repeat as needed)
Isotonic crystalloid fluids: 280-320 mOsm/L
Balanced Electrolyte Sol (BES) (#1): alkalinizing, added Na, Ca, Cl, K, organic anions
Normal Saline NaCl (0 9%): acidifying, use for hyperkalemia/Na depletion
addeditives: Ca, K, Mg, dextrose, Sodium bicarb
5% dextrose - hypoglycemia
Sodium Bicarb - met. acidosis
Hypertonic saline - cerebral edema
Colloids:
Hetastarch: rapid expansion, oncotic support, follow w/ isotonic crystalloids, limits edema, retained in IV space
FF Plasma: Ig, albumin, clotting factors, antitoxins, FPT, Hypoproteinemia
Whole blood: acute severe anemia (transfuse if PCV <20% in acute, <12% chronic; 6-8 L from Qa neg, un-sensitized gelding)
Monitor for HS Type I rxn!!!
Must follow colloids with isotonic crystalloids
IV Catheters in Horses
Site: Jugular, lateral thoracic & cephalic v
Transverse facial artery: palpate arterial pulse, arterial blood gas collection
Material: 14g, 5”
Short-term: Teflon, rigid, thrombogenic, crack
Long-term: polyurethane, pliable
Rxn: phlebitis, thrombophlebitis, cellulitis
Sedative-analgesic drugs in Horses
Purposes of: Chemical restraint, Pain management & Pre-anesthesia → IV, IM, CRI
Alpha-2 agonists
Xylazine: short-acting, brief restraint, pre-anesthetic, first-line for colic - abd. pain
Detomidine: more potent, long acting, CRI or oral gel, good for standing procedures
Butorphanol: Opioid of choice in horses, used w/ alpha-2s
Acepromazine: Tranquilizer, prolonged sedation,“drop penis” (risk of priapism in stallions)
Pain Management in Horses
Colic pain: xylazine, butorphanol, flunixin
MSK pain: NSAIDs (phenylbutazone)
Peri-op pain:
CRI: alpha-2, butorphanol, lidocaine, ketamine
Epidurals: lidocaine, alpha-2, morphine
NSAIDs in Horses
MOA: inhibit COX → block prostaglandins/thromboxanes
Rx:
Flunixin meglumine: general, common
Phenylbutazone: ortho pain, cheap
Firocoxib (Equioxx): less ulcer risk
Rxn: GI ulcers, Renal crest necrosis/interstitial nephritis, clostridial myonecrosis/injection rxn
Corticosteroids in Horses
MOA: inhibit phospholipase A2 → shut down arachidonic acid cascade
Uses: equine asthma, allergic skin dz, pemphigus foliaceus, uveitis, purpura hemorrhagica, IM polymyositis, IMHA, IBD, osteoarthritis (intra-articular)
Anti-inflam + immunosuppression
Rx: prednisolone (oral), dexamethasone (oral/injectable), beclomethasone (inhaled), fluticasone (inhaled), triamcinolone (intra-articular)
Rxn: laminitis, infection, impaired wound healing, cartilage degeneration, adrenal suppression
Avoid long acting types, use short acting
Empiric Guidelines for Antibiotic use in Horses
Culture before use
Strep: penicillin, 1st-gen cephalosporins, ceftiofur
S equi equi/zooepidemicus
Anaerobes(stink): penicillin (G+ &G-)
if resistant → oral metronidazole
G - aerobic: gentamicyn
Rhodococcus equi: macrolide + rifampin (foals)
causes colitis in adults
Clostridia: penicillin G, metronidazole
Ehrlichial: Tetracyclines
Potentiated sulfas: EPM, practical for alot
Oral: potentiated sulfas, doxycycline
Special combos: rifampin + sulfa/doxy
chronic abscesses, off-label
Bloodwork on feed/water restriction
polycythemia
pre-renal azotemia
hypocalcemia
Hypokalemia
decreased Bilirubin - fasting
increased PCV & total proteins (TP)
Increased CK
Misc PE in Horses
Upper Airway Exam: Nasal passages, Paranasal sinuses, Pharynx, Larynx, Guttural pouches & Trachea
Upper: obstruction, resp. distress, noise, cough, nasal discharge, facial swelling, air flow, LN swelling, fever
Dt: endoscopy
Misc: alnar for increased airflow
Lower: Vital signs, Auscultation, Re-breathing, Percussion
faired nostrils, wheezing, nasal discharge, resp. effort, tracheal exudate, abnorm. lung sounds
Thoracic inlet: lower airway sounds auscultation
Normal Airway Cytology
Macrophages 40-70%
Lymphocytes 30-60%
Neutrophils <5%
Cardiac Exam
Valve areas: left ICSs 3,4,5; right ICS 4
HR: 28-44 BPM
high vagal tone
Resting 2nd degree AV block is normal
Equine Herpes Viruses
Et: EHV1-4, ubiquitous, latency
Types:
Rhinopneumonitis: resp dz in weanlings/yearlings 2-5y (adults immune)
Cs: fever, malaise, serous nasal discharge, dry cough, lymphadenopathy
EHV-1 abortion: “abortion storms” at 7-11m (3rd trimester)
Cs: placental/fetal vasculitis, none pre-abortion or to mare
EHV-1 neuro
Cs: acute ataxia, tetraparesis, sacral signs, spinal vasculitis
Dt: bld/nasal PCR/VI, fetal lesions, IHC post mortem
Tx: rest, shelter, NSAIDs, antivirals, quarantine, report, vax (reduces shedding)
Equine Influenza
Et: contagious, Type A H3N8, no carrier state
Invades resp epithelium, short incubation (1-3d)
Cs: malaise, high fever, cough, serous nasal discharge, pneumonia, myocarditis, pericarditis, myositis, vasculitis, death
Dt: PCR (#1), ELISA, VI, paired serology
Tx: Rest >21d, NSAIDs, good enviro, encourage feed/water intake, IM killed vax or MLV nasla vax
High-risk horses vax biannually
Streptococcus equi subsp zooepidemicus
Et: Opportunistic - Nasopharynx flora
gram positive beta-hemolytic strep, infection requires a compromised host
common second-degree invader in resp dx and other body systems
Cs: rhinitis, pharyngitis, sinusitis, pneumonia, peritonitis, abscesses, endometritis, keratitis, wound infectionsTx: penicillin
Streptococcus equi subsp equi (Strangles)
Et: Incubation 3-14d, M-protein (SeM) inhibits lysosomes, host adapted, Gram-positive, beta hemolytic
Cs: purulent lymphadenitis of head & neck, airway obstruction, guttural pouch empyema, abscess, systemic metastasis, purpura hemorrhagica, fever, depression, anorexia, mucoid nasal discharge, vasculitis
submandibular, medial retropharyngeal LN
Dt: neutrophilia w/ L shift, high fibrinogen, PCR/culture (swabs, guttural pouch wash, pus), imaging (US/scope/Rads)
Evaluate guttural pouches
Tx: warm compresses, drainage, NSAIDs, Penicillin, quarantine, M-protein subunit/ Mod-live IN vax
Risk of purpura hemorrhagica post-vax, immunity not permanent
Nasal & Paranasal Disorders in Horses
Epidermal inclusion cyst: nasal diverticulum, cosmetic; sx removal curative
Redundant alar folds:“floppy nostrils,” stertor, obstruction on inspiration; Dt mattress suture test; elective resection
Nasal septum deformities: congenital, trauma, rare, amyloidosis; may need resection
Choanal atresia: dev failure of nasopharyngeal perforation; neonatal resp distress
Wry nose: lateral maxillary deviation, malocclusion, nasal occlusion; sx correction
Progressive ethmoidal hematoma: benign mass, mild intermittent epistaxis; Dt w/ CT; Tx w/ sx bone flap, endoscopic laser ablation, formalin injection
Sinus Disorders in Horses
Sinusitis
Et:
Primary: bacti, viral, fungal
Secondary: dental disease (M1 tooth root abscess), trauma, ethmoidal hematoma, cysts, neoplasia
Cs: unilateral mucopurulent discharge, malodor ( w/ tooth root infection), swelling/facial distortion
Dt: endoscopy (nasomaxillary drainage), rads (fluid lines), CT, culture, cytology
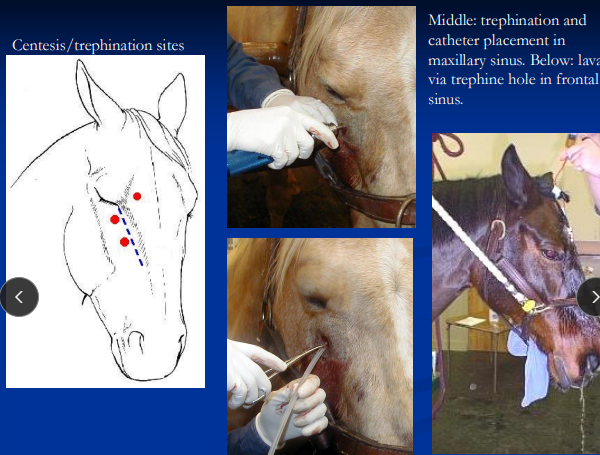
Tx: drainage via trephination/lavage, antibiotics, tooth extraction, bone flap sx
Paranasal sinus cyst
Et: Lg, multiloculated, congenital, slow-growing
Cs: facial deformity, mild discharge
Dt: rads(cyst cavity), mucinous fluid on centesis
Tx: sx removal via bone flap


Pharynx & Larynx Developmental Conditions in Horses
Cleft palate: milk in nostrils from birth; aspiration pneumonia; Dt w/ endoscopy; Tx w/ Sx
Pharyngeal cysts: congenital; obstructive noise/choke; Tx w/ Sx removal
Hypoplastic/flaccid epiglottis: congenital or neuropathic; recurrent DDSP, resp nosise, epiglottis entrapment; Tx w/ epiglottic augmentation via Teflon injection
4th branchial arch defect: rare; resp noise, poor performance, cough, aspiration; Dt: “rostral displacement of palatopharyngeal arch”; No Tx


Dynamic Airway Obstruction in Horses
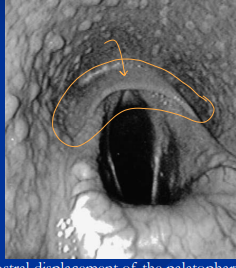
Dynamic DDSP (soft palate)
Sig: 2-3y racehorses
Cs: acute obstruction + “choking down ” at speed,
Dt: treadmill/overground endoscopy
Tx: fitness, tongue tie, myotenectomy, partial staphylectomy
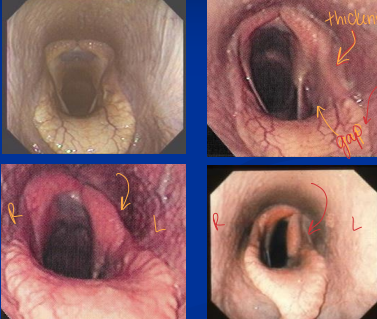
Left laryngeal hemiplegia (“roaring”)
Et: left recurrent laryngeal nerve failure, QHs/Tbs/Drafts
Cs: inspiratory noise + exercise intolerance
Dt: Endoscopy
Tx: prosthetic laryngoplasty “tieback” (Good return to full performance)
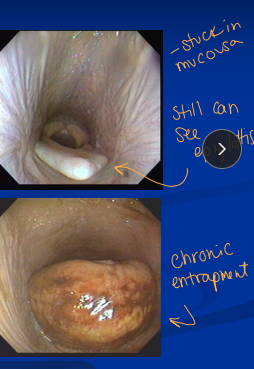
Epiglottic entrapment
Et: Epiglottis enveloped by aryepiglottic fold
Cs: poor performance, noise, cough, DDSP, inflamed mucosa
Dt: endoscopy
Tx: sx axial division of fold, anti-inflam sprays
Dynamic pharyngeal collapse
Et: High insp neg pressures, narrow pharynx, neuropathy, fatigue, lymphoid hyperplasia, laryngeal hemiplegia, nasal obx

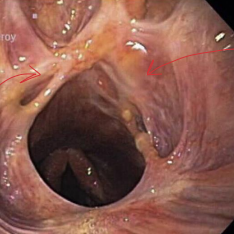
Inflammatory Pharynx & Larynx Conditions in Horses
Pharyngeal lymphoid hyperplasia
Et: Normal in young horses, associated w/ immune dev
Cs: sore throat/cough, DDSP
Tx: rest, soft feeds, NSAIDs/steroids, throat sprays
Laryngitis/chondritis
Et: Persistent inflam, high-speed work, hemiplegia, epiglottic entrapment, coarse feeds
Cs: obx, insp noise, dysphagia, aspiration, stenosis, DDSP
Tx: rest, NSAIDs, antibiotics, partial arytenoidectomy, tracheostomy
Poor prognosis for performance
Pharyngeal cicatrix: Idiopathic inflam scarring, Texas pasture horses
Pharyngeal neuropathies: GP disease (mycosis), trauma, EPM, encephalopathy, toxins (lead, botulism), myopathies (HYPP, white muscle dz)
Guttural Pouch Disorders
Tympany
Et: Air distension, foals, congenital or acquired
Cs: soft swelling throatlatch, resp distress
Dt: endoscopy, rads
Tx: Sx fenestration of septum (unilateral), resection, decompression
Good prognosis
Mycosis
Et: Aspergillus, plaques near arteries/nerves
Cs: aneurysm, rupture, epistaxis (fatal), neuropathy, aspiration, cough, dysphagia, Horners
Tx: stabilize hemorrhage, sx arterial occlusion (balloon/coil), antifungals
Empyema
Et: strangle, carrier state
Cs: Purulent exudate, nasal discharge, fever, depression, airway obx
Dt: endoscopy, culture/PCR
Tx: lavage, antibiotics, Sx removal, Modified Whitehouse procedure (ventral drainage)
Trauma/stylohyoid disease
Et: Avulsion of longus capitis/rectus capitis ventralis, fracture, Temporohyoid osteoarthropathy
Cs: hemorrhage, neuro signs, vestibular dx, facial paralysis
Conditions of the Trachea in Horses
Et: infectious (EHV, strangles), trauma, stenosis, granulomas, FB, collapse (old ponies), neoplasia (SCC, melanoma)
Tx: Tracheotomy
Incision: junction of upper 1/3 and lower 2/3 of neck, above sternomandibularis split
Initial ventral midline incision
Horizontal incision of <50% annular ligament
DO NOT Cut cartilage rings = chondroma/stenosis risk
Healing: second intention
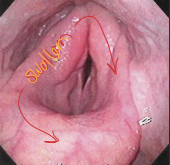
Bacterial Pneumonia
Et: Strep zooepidemicus (#1), Staph, E coli, Klebsiella, Pasteurella, Actinobacillus, Pseudomonas, Bacteroides, Clostridium, Fusobacterium
Sig: performance horses, travel
Cs: Fever, depression, anorexia, toxemia, dehydration, ventral lung sounds, shallow breathing, stilted gait, pain on percussion, purulent exudate, consolidation, necrosis
Dt: Inflam leukogram (↑ fibrinogen), US/rads w/ ventral consolidation, endoscopy/tracheal wash, thoracocentesis
Tx: penicillin + gentamicin, metronidazole, NSAIDs, O₂, fluids, dust-free enviro, thoracotomy, chest tubes ± lavage
Aggressive, early intervention - uncomplicated pneumonia
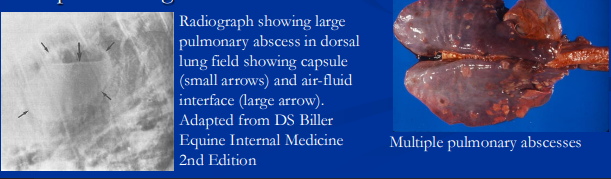
Rhodococcus equi
Et: G+ facutive intracellular, fecal/resp transmission, soil, vapA causes resistance
Sig: foals 1-5m
Cs: Hilar lymphadenitis, suppurative bronchopneumonia, intestinal signs, pulmonary parenchymal abscessation, synovial distention, septic arthritis
Dt: high fibrinogen/neutrophils/globulins), tracheal wash, culture
Tx: O₂, fluids, dust-free enviro, Azithromycin + rifampin, hyperimmune plasma
Aggressive, early intervention
Fungal Pneumonia in Horses
Et: antibiotic tx, Neutropenia, steroid tx
Opportunists: Aspergillus, Candida, Fusarium, Pneumocystis
Primary: Histoplasma, Blastomyces, Coccidioides, Cryptococcus, Conidiobolus
Cs: Fever, depression, anorexia, toxemia, dehydration, abnormal/reduced lung sounds ventrally, shallow breathing, reluctance to walk, stilted gait, pain on percussion
Dt: airway cytology, culture, biopsy; rads w/ patchy multifocal infiltrates, peripheral granulomas
Tx: amphotericin B, azoles, iodides
guarded prognosis
Aspiration Pneumonia in Horses
Et: inhalation of saliva, feed, milk, oral meds (oil), choke, pharyngeal paresis, URT obstruction, cleft palate, bottle-fed neonates
Cs: Fever, depression, anorexia, toxemia, ventral lung sounds, shallow breathing, stilted gait, pain on percussion
Dt: Inflam leukogram, US/rads w/ ventral consolidation, endoscopy/tracheal wash w/ suppurative tracheal exudate, thoracocentesis
Tx: penicillin + gentamicin, metronidazole, NSAIDs, O₂, fluids, dust-free enviro, chest tubes ± lavage
Aggressive, early intervention
Equine Asthma Spectrum
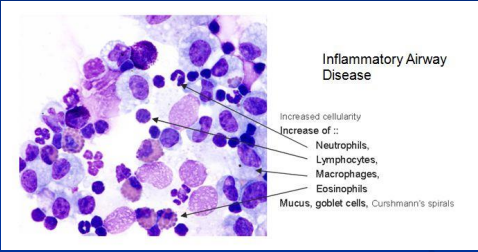
Inflammatory Airway Disease
Et: dust, particulates, endotoxins, ammonia, air pollution, post-infectious inflam
Cs: no resp distress at rest, poor performance, exercise intolerance, cough, mild discharge
Dt: performance issues, normal CBC, BAL, neutrophilic inflam
Tx: envirol control, steroids, bronchodialators
Recurrent Airway Obstruction (ROA)(“Heaves”)
Et: Summer pasture, allergens, genetics
Sig: Older horses
Cs: cough, exercise intolerance, abnormal lung sounds, acute attacks, mucopurulent discharge, flared nostrils, expiratory effort (“heave line”)
Dt: normal temp/BW, BAL w/ non-septic neutrophilia, mucus plugs (Curschmann’s spirals), allergy testing
Tx: enviro control, steroids, bronchodialators

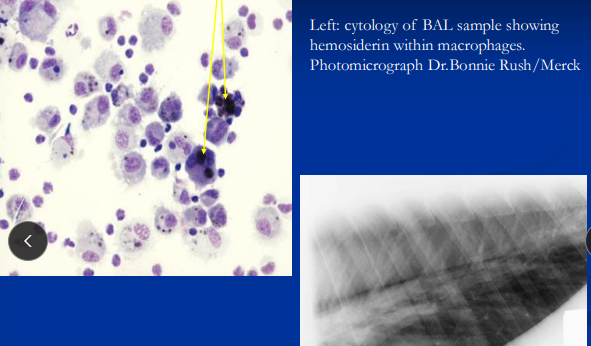
Exercise-Induced Pulmonary Hemorrhage
Et: hemorrhage from dorsal lungs during max exertion
Sig: racehorses
Dt: Endoscopy w/in 45 min post-exertion, BAL cytology w/ hemosiderin-laden macrophages
Tx: furosemide, nosebands
Normal Cardio
Valve areas left ICSs 3,4,5; right ICS 4 (PAM-T)
Rate 28-44 BPM due to high vagal tone
Resting 2nd degree AV block is normal
Normal to hear all 4 heart sounds
Physiologic/flow murmurs common
Heart Failure in horses
Et: poor myocardial ventricular pumping efficiency
Myocardial injury/myopathy, Volume overload (valvular insufficiency, High afterload (pulmonary/systemic hypertension), Acute tachyarrhythmias (AF, VT)
Types:
Left: pulmonary hypertension/edema, poor systemic arterial circulation
Cs: weakness, exercise intolerance, cough, dyspnea, tachycardia, weak pulses
Right: systemic venous backup
Cs: jugular distention, edema
Dt: murmurs, prerenal azotemia, high hepatic enzymes, high CVP, echo w/ chamber enlargement + poor function, rad w/ cardiomegaly + pulmonary edema
Tx: Furosemide (diuretic), Digoxin (positive inotrope), Benazepril (ACE inhibitor)
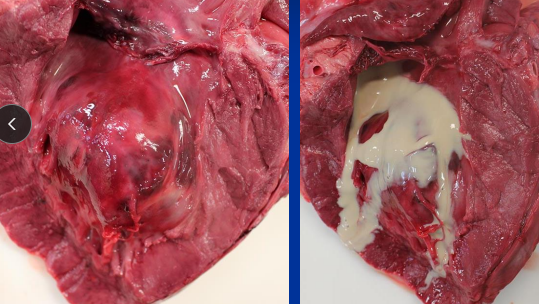
Myocarditis in Horses
inflammation and damage to a horse's heart muscle
Et: Influenza, bacti, parasitic, toxins #1 (Ionophores, venom, plants), IM, thromboembolic
Cs: weakness, exercise intolerance, cough, dyspnea, tachycardia, weak pulses, fever
Dt: High CK, high cardiac troponin, echo w/ poor contractility or abnormal motion, Stomach contents exam
Tx: Rest, furosemide, digoxin, benazepril, lidocaine, MgSO4, antibiotics, lavage, charcoal, mineral oil, smectite, Antivenom, Corticosteroids
Prognosis guarded
Cardiomyopathies in horses
Adults: no primary cardiomyopathies; most secondary to myocarditis/valvular disease
Foals: selenium deficiency (white muscle disease)
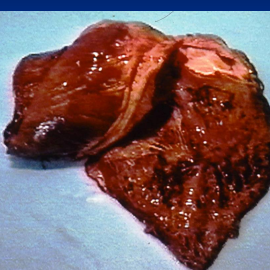
Acquired Valvular Disease in horses
Et: degenerative change (#1), bacti endocarditis, ruptured chordae tendineae
Leads to regurgitation → volume overload → chamber enlargement → CHF
Mitral & aortic insufficiencies (#1)
Sig: performance horses
Cs: #1 cause of pathologic murmurs, benign murmur, afib
AV valve insufficiency → systolic murmur
Aortic insufficiency → diastolic murmur
Dt: echo (valve function, high L arterial pressure, chamber size, Doppler)
Tx: retire from work
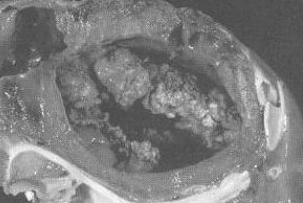
Bacterial Endocarditis in horses
Et: bacti adhere to valves, rare
aortic > mitral > tricuspid > pulmonic
Strep equi zoo, Actinobacillus equuli
Cs: intermittit fever, weight loss, murmur, inflam leukogram
Dt: Neutrophilia, high fibrinogen, Echo (visualize lesion, regurg), Bld cultures
Tx: Long-term IV antibiotics
Prognosis poor
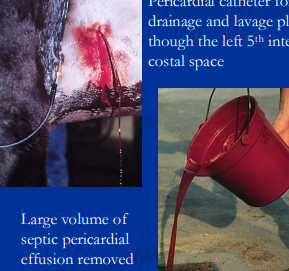
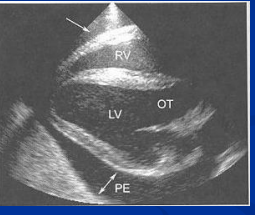
Pericarditis in horses
Et: Inflam of pericardium, Actinobacillus, Strep zoo, influenza, EVA, AHS
Fibrinous or Effusive
Cs: fever, depression, exercise intolerance, weakness, tachycardia, muffled heart sounds, weak pulses, circulatory collapse
Dt: Echo (effusion), Pericardial tap, ECG w/ Low QRS amp
Tx: Pericardial drainage + lavage, Antibiotics, Corticosteroids
Prognosis poor
Congenital Heart Disease in Horses
Et: VSD (#1), ASD, PDA, valve lesions, tetralogy of Fallot
Sig: Arabians, STB, QH
Cs: systolic murmur loudest on R, Growth stunting, lethargy, exercise intolerance, CHF, premature foal death
Dt: echo/Doppler
Tx: palliative only
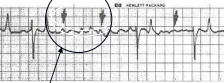
Cardiac Arrhythmias in Horses
Atrial fibrillation:
Et: #1 arrhythmia, high vagal tone, low K from GI dx, mitral insufficiency, atrial enlargement, CHF, low resting HR
Cs: exercise intolerance, poor performance, distress, collapse
asymptomatic at rest if benign
Dt: ECG w/ no P waves, irregular R-R
Tx: quinidine (oral), electrical cardioversion
Good prognosis
Ventricular tachycardia:
Et: systemic illness, endotoxemia, electrolyte disorders (↓ K+), myocarditis
Cs: syncope, resp distress, acute CHF, myocardial injury, HR >100 BPM
Tx: lidocaine (bolus + CRI), Mg sulfate
Hyperkolemia
Et: Depresses impulse conduction
renal failure, post-renal obstruction, uroperitoneum, acidosis, severe rhabdomyolysis or hemolysis, over-supplementation, IV fluids
Cs: atrial flutter, atrial standstill, asystole/cardia arrest
Dt: K >6 mEq/dL, broad flat P, wide QRS, tall T
Tx: dextrose, insulin, bicarbonate

Jugular thrombophlebitis in Horses
Et: venipuncture, injections, catheterization, sepsis, endotoxemia
Cs: thick vein, pain, swelling, venous congestion proximal, fever, facial swelling, pulmonary embolism, thrombophlebitis, occlusion
Dt: inflam leukogram, high fibrinogen, US, culture
Tx: remove catheter, warm compresses, anti-inflam, antibiotics, good catheter technique, asepsis, avoid bad veins, aspirin prophylaxis
Verminous arteritis
Et: S vulgaris L4 larvae migrates in cranial mesenteric artery
Cs: arteritis, stenosis, aneurysm, intestinal ischemia, infarction, colic, aortic root lesions, rupture, coronary artery migration, thrombophlebitis
Aneurysm/rupture in Horses
Et: mesenteric (hemoperitoneum), middle uterine artery (postpartum mares), internal carotid/maxillary (GP mycosis), aorta, sinus of Valsalva
Cs: hemoperitoneum, hemopericardium, death

Arterial thrombosis in Horses
Et: S vulgaris arteritis, idiopathic aorto-iliac thrombosis in athletes, sepsis, toxins
Cs: sudden pain/lameness, cool limb, absent pulse, ischemic lameness
Dt: rectal exam, US
Tx: thrombolytics (TPA, streptokinase)
Acute bronchointerstitial pneumonia of foals
Et: hot weather
Cs: high fever, respiratory distress, cyanosis, & high mortality
Sporadic
Dt: diffuse interstitial pattern, hypoxemia, hypercapnea
Tx: O2, steroids
emergency
White Blood Cells in Horses
Fibrinogen: coagulation/fibrin formation, acute phase reactant
High = active inflam, within 24h of infection, chronic bacti infections
Serum amyloid A: same as fibrinogen
Neutrophils:
Stress: mature neutrophilia (no bands) + lymphopenia
Acute: high levels + left shift, high fibrinogen
Chronic: mature neutrophilia + hyperfibrinogenemia
Neutropenia: LPS (endotoxemia), GI dx, G- sepsis; left shift + toxic changes
Caused by margination
Lymphocytes
Lymphopenia: Stress, steroids, acute infections
Lymphocytosis: Physiologic, lymphoid neoplasia
Lymphoblasts in peripheral blood = diagnostic
Monocytes: high in chronic infection/convalescence, rarely neoplasia
Eosinophils: Type HS, airway dz, parasites, eosinophilic enterocolitis, MEEDs
Basophils: high w/ allergic dx
Leukogram Patterns
Stress: mature neutrophilia + lymphopenia, normal fibrinogen, no bands
Physiologic: mature neutrophilia + lymphocytosis, no left shift
Inflam: Left shift, high fibrinogen
Lymphosarcoma
Et: Malignant lymphoid neoplasia
Generalized, intestinal, mediastinal & cutaneous forms
Cs: malabsorption, diarrhea, colic, organ dysfunction, fever, pleural effusion, resp issues, masses, anemia, inflam leukogram, atypical lymphoblasts, pancytopenia,
LN enlargement not typical
Dt: Blasts on bld smear (#1), LN aspirates, biopsy, BM aspirate
Tx: Steroids, chemo, excision of cutaneous nodes
Grave prognosis, Cutaneous better prognosis
Myeloproliferative Diseases in Horses
Et: BM infiltrated w/ neoplastic granulocytic/monocytic cells, atypical cells in blood, leukemia, myelophthisis, pancytopenia
Sig: young (~5 y)
Cs: depression, fever, lymphadenopathy, splenomegaly, edema, mucosal hemorrhage
Dt: CBC, BM aspirate
Prognosis is poor
Polycythemia
Et: high PCV, RBC count, Hb
Types:
Relative: fluid deficit or splenic contraction
Absolute: uncommon
Primary = polycythemia vera (rare, idiopathic, normal PO2, ↓ EPO)
Secondary appropriate = chronic hypoxia
COPD, heart dx, high altitude
Secondary inappropriate = rare
hepatic, renal, endocrine neoplasia
Red Blood Cells in Equines
Unstable PCV: Lg splenic reserve
Rouleaux formation: normal, must differentiate from autoagglutination
Regeneration: not apparent on smear, need BM
Howell-Jolly bodies: normal in sm #
Mild plasma icterus: normal
Acute Hemorrhage in Horses
Et: trauma, organ/artery rupture, coagulopathies, lung laceration, rib fracture, diaphragmatic tear, GP mycosis
Cs: Pallor, tachycardia, tachypnea, hypovolemic shock, trembling, sweating, distress, white MM (>1/3 blood loss)
Dt: low RBCs and plasma protein, US
Tx: pressure bandage, nasal packing, suture/ligate, tie off vessels, crystalloid fluids, transfusions (PCV <20% w/i 12h or <12% 1-2d), autotransfussion
Stop hemorrhage and volume expansion
Chronic Hemorrhage in Horses
Et: GI bleeding, NSAID ulcers, platelet disorders, tumors, external parasites, urinary tract bleeding, clotting disorders
Cs: animal stable unless stressed, adapted to hypoxemia
Dt: CBC, clotting studies, fecal occult blood, parasitology
Tx: feed quality forage, avoid iron dextrans
Hemolytic Diseases in Horses
Types:
Intravascular: Free hemoglobin; Rapid; Schistocytes on smear
Extravascular: No gross hemoglobinemia/uria, gradual PCV drop
Immune-mediated hemolytic anemia (IMHA)
Et:
Primary: rare; idiopathic autoimmune
Secondary: most common; infection, drugs lymphosarcoma, Alloimmune (neonatal isoerythrolysis, bad transfusions)
Cs: fever, jaundice, hemoglobinemia/uria, hyperbilirubinemia
Dt: Acute anemia, normal TP, slide agglutination, Coombs, flow cytometry,
Tx: Oxygen, transfusions, steroids (dex)
Oxidative hemolysis (Heinz body anemia)
Et: oxidative injury, dry red maple, onions, Brassica, phenothiazine, pistaia trees
Cs: brown plasma, pigment nephropathy, heinz bodies, intravascular hemolysis, methemoglobinemia, Tachypnea, tachycardia, weakness
Tx: aggressive fluids, transfusion, supportive care
Prognosis is guarded
Neonatal Isoerythrolysis
Et: Secondary IMHA, colostral Ab against foal’s RBC antigens
Sig: Foals <1w, multiparous mare, mules
Cs: weakness, lethargy, pallor, tachypnea, tachycardia, anemia, jaundice, dehydration, metabolic acidosis, hypoglycemia, hyperbilirubinemia
Dt: Acute anemia, normal TP, jaundice foal agg, Coombs, flow cytometry, test mares for Aa/Qa, mare serum vs stallion RBCs, colostrum screen
Tx: Rest, correct fluids/electrolytes/glucose, transfusion, donor colostrum
Coagulation disorders in horses
Thrombocytopenia
Et: blood loss, destruction, decreased production, high consumption
Idiopath, BM suppression, potentiated sulfas, IMTP, hemmorage
Cs: petechiae, epistaxis, GI bleeding, mucosal hemorrhage
Spontaneous bleeding if platelets <30,000/µL
DIC:
Et: Triggered by endotoxemia, SIRS, G- sepsis, burns, trama, neoplasia
Generalized activation of the coagulation cascade
consumption of platelets, factors, fibrinogen
Cs: petechiae, ecchymoses, microvascular thrombosis, hemorrhagic diathesis
Dt: low platelets/fibrogen, high PT/APTT/FDPs
Hepatic failure:
Et: decreased clotting factors
Tx: frozen plasma
Rodentaside/sweetcover:
Et: decreased clotting factors
Cs: epistaxis, hematomas, hemarthroses, bleeding, hyphema, anemia
Dt: prolonged PT/APTT, normal platlet count, no FDP
Tx: Vit K
Genetic (rare): Hemophillia A (TB/QH/STB/Arab), vWB dx, Prekallikrein deficiency (draft/mini)
Production issues: chronic dx, BM suppression, sulfas, Erythropoietin deficiency, GI bleeding, iron seq
Vasculitis
Et: Inflam of sm vessels, immune mediated, infectious, Purpura Hemorrhagica
Vascular and hemostatic
Cs: pitting edema, mucosal hemorrhages, petechiation, serosal hemorrhages, jaundice, thrombocytopenia, anemia, fever
Tx: report if EVA/EIA/prioplasmosis
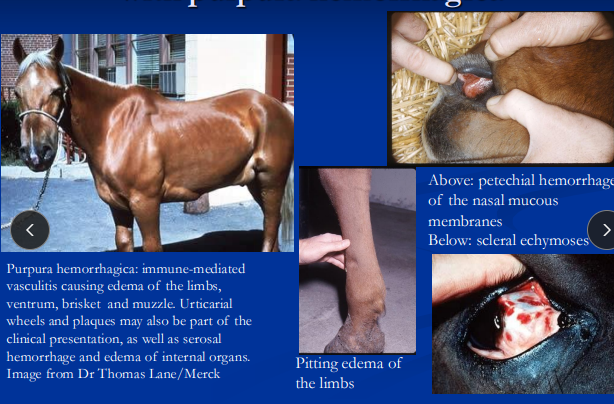
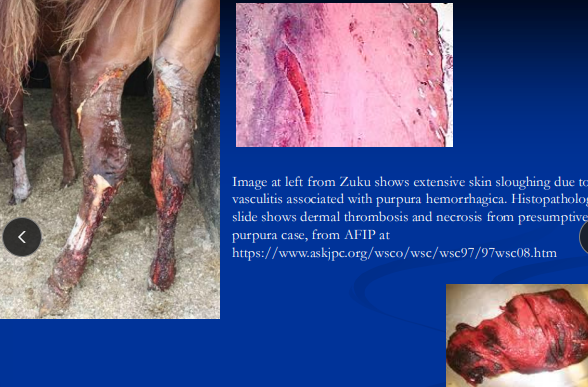
Purpura Hemorrhagica
Et: IM, post-Strep equi equi infection or vax
leukocytoclastic vasculitis, fibrinoid necrosis
Cs: limb/ventral/facial edema, petechiation, urticaria, fever, necrosis/sloughing, myocarditis, laminitis, infarctive myopathy
multisystem involvement
Dt: history of strangles/vax, high SeM titers for Strep, high globulins
Tx: drain abscesses, antibiotics, immune suppression, hydrotherapy, eliminate Ag, compression
Prognosis is fair-good; relapses possible
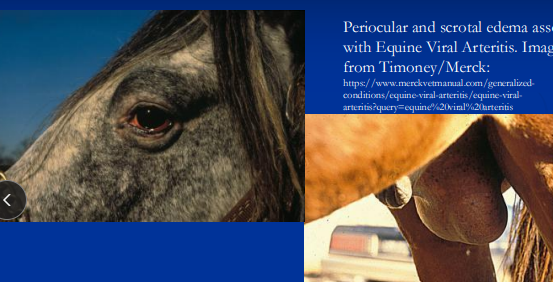
Equine Viral Arteritis
Et: RNA virus, resp & venereal (semen) transmission
Cell associated viremia, accessory sex glands, placenta
Cs: fever, edema, urticaria, resp dx, nasal discharge, lacrimation, icterus, leukopenia; abortions (3-10 m gestation), vasculitis
Subclinical common
Dt: PCR/virus isolation, serology (bld, nasal, fetal)
Tx: MLV vax (stallions before breeding, annual boosters), test semen, reportable
Equine Infectious Anemia (“Swamp Fever”)
Et: Retrovirus; transmitted by biting flies, iatrogenic, in utero, colostrum
Unregulated QH racing in North america
Cs:
Acute (30 d): fever, thrombocytopenia, lethargy, vasculitis, high viremia
Chronic: ill-thrift, recurrent fever, anemia, thrombocytopenia, jaundice, low viremia
Carrier (#1): lifelong infection, no signs
Dt: Coggin’s test (AGID gold standard), ELISA
Tx: permanent quarantine, test before travel, euthanasia, report, persistent infection
Equine Piroplasmosis
Et: Protozoal RBC parasites (Babesia caballi, Theileria equi), Dermacentor ticks
Endemic South america, europe, mediterranean
Unregulated QH racing in North america
Cs: hemolytic anemia, fever, icterus, edema
Permanent subclinical
Dt: blood smear (parasites in RBCs), cELISA/CF for carriers
Tx: imidocarb, report, quarantine
Equine Granulocytic Anaplasmosis
Et: Anaplasma phagocytophilum, tick-borne, Ixodes, North america
Cs: fever, depression, ataxia, edema, petechiation, icterus, anemia, thrombocytopenia, leukopenia, vasculitis
worse in adults
Dt: morulae in neutrophils on smear, PCR, serology
Tx: tetracyclines
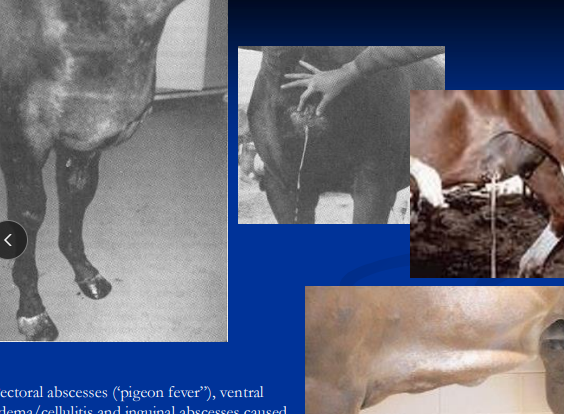
Corynebacterium pseudotuberculosis (Pigeon Fever)
Et: Gram+ facultative anaerobe, intracellular, soil organism, wounds, insects
Inhabits macrophages
Sig: arid N America, late summer/fall, post drought + rain
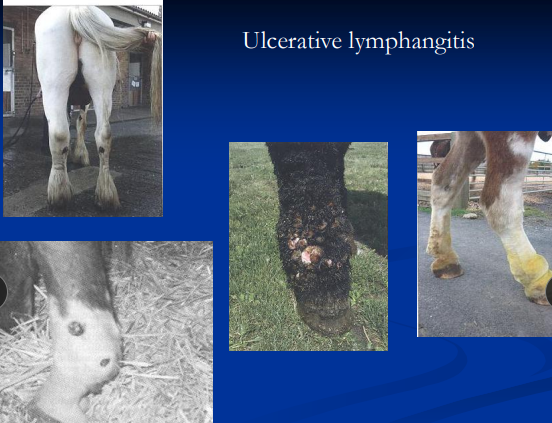
Cs: classic pectoral abscesses (#1), external/internal abscesses, ulcerative/purulent lymphangitis, cellulitis, severe limb swelling
3 forms: External/Internal abscesses Ulcerative lymphangitis
Dt: Culture, inflam leukogram, high fibrinogen/globulins, SHI titer, US
Tx: allow maturation, lance/drain, antibiotics, Sx
Antibiotics before drainage = delays healing
Internal worse prog than external