Medical Imaging Techniques: Ultrasound, X-ray, MRI, and Image Processing | Quizlet
1/148
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
149 Terms
What is image acquisition in medical imaging?
The creation of a digitally encoded representation of the visual characteristics of an object.
What frequency range defines ultrasound?
Sound with frequency greater than approximately 20 kHz.
What is the purpose of medical ultrasound?
To create images of internal body structures to find disease sources or exclude pathology.
What is interference in wave phenomena?
The combination of two or more electromagnetic waveforms to form a resultant wave.
Define diffraction in wave behavior.
The bending of waves around obstacles or through apertures.
What are acoustical waves?
Pressure waves that propagate through matter via compression and expansion.
What factors affect sound wave propagation velocity?
The density and elasticity of the medium.
How is acoustic impedance calculated?
By the formula Z = ρ * c, where ρ is density and c is the speed of sound.
What does attenuation refer to in ultrasound?
The loss of wave amplitude due to absorption and scattering.
How is attenuation expressed mathematically?
Attenuation = -10 * log(Az/A0), where Az is the measured amplitude and A0 is the source amplitude.
What occurs during the reflection of sound waves?
Sound waves reflect at boundaries where two media with different acoustic impedances meet.
What is the reflection coefficient?
The fraction of incoming wave energy that is reflected at a boundary.
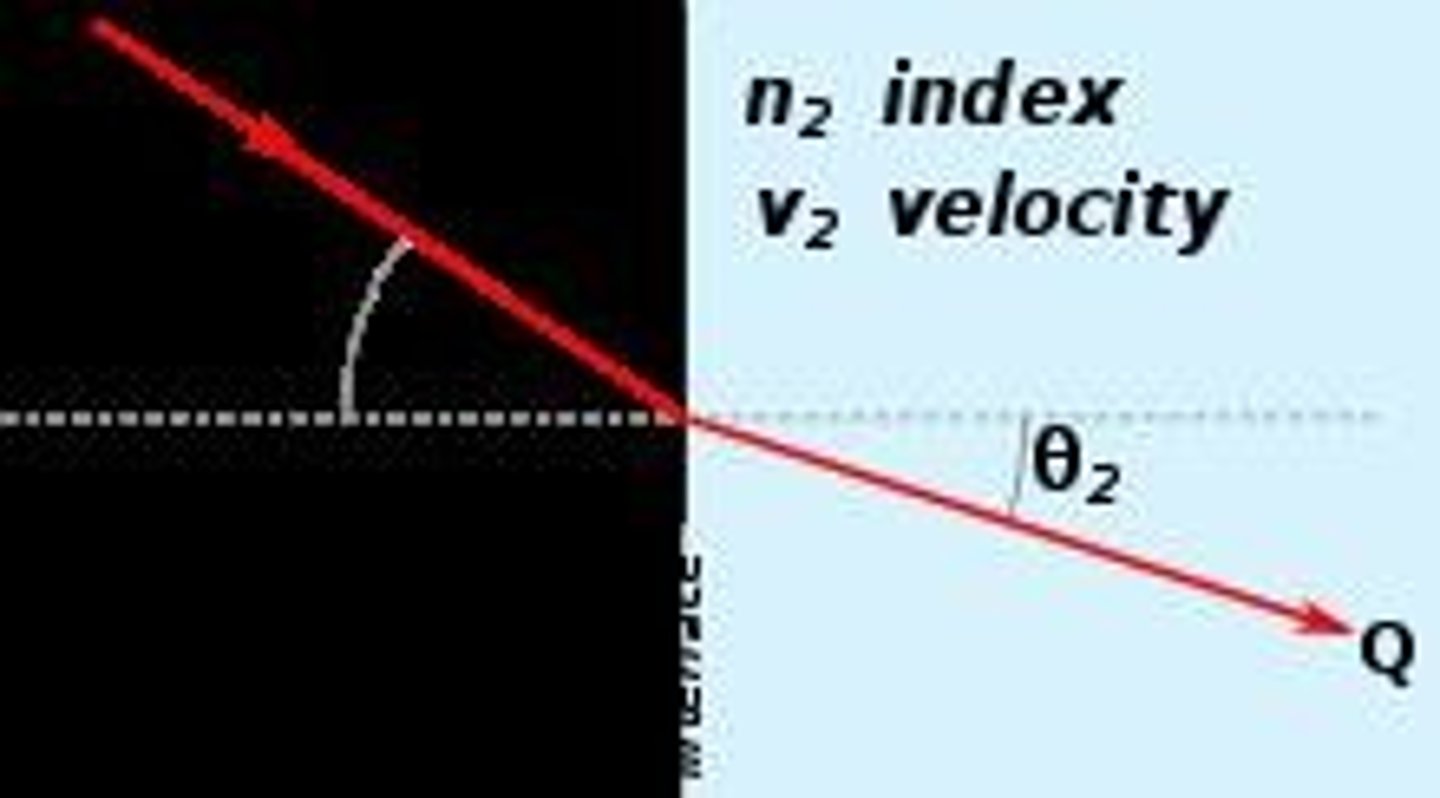
What is refraction in wave propagation?
The change in direction of a wave as it passes from one medium to another.
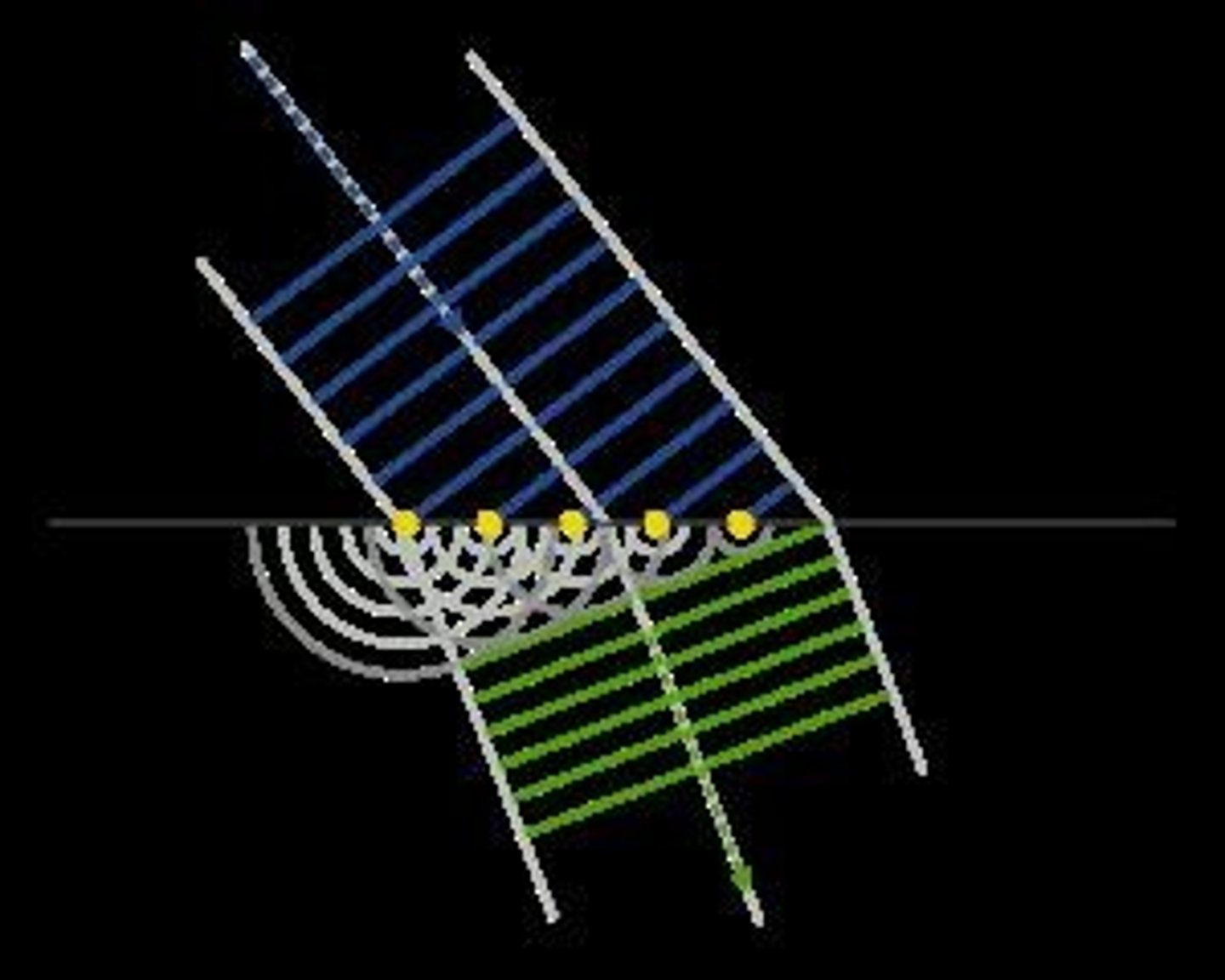
What is the Huygens-Fresnel principle?
A method of analysis for wave propagation stating that every point on a wave front is a source of spherical wavelets.
How is ultrasound pulse generated?
By applying a high-voltage pulse to a piezo-ceramic crystal, causing it to expand and create an ultrasound pressure wave.
What is the focal zone in ultrasound imaging?
The region where the ultrasound intensity is maximal, located between the Fresnel and Fraunhofer zones.
What is A-mode in ultrasound imaging?
Amplitude mode where a single transducer scans a line through the body, plotting echoes as a function of depth.
What is B-mode in ultrasound imaging?
Brightness mode where a linear array of transducers scans a plane through the body, producing a 2D image.
What is the effect of using a curved ultrasound transducer?
It narrows the focal zone for higher resolution but causes wider divergence of the beam before and after the focal zone.
What is the Doppler Effect?
The change in frequency of a wave in relation to an observer moving relative to the wave source.
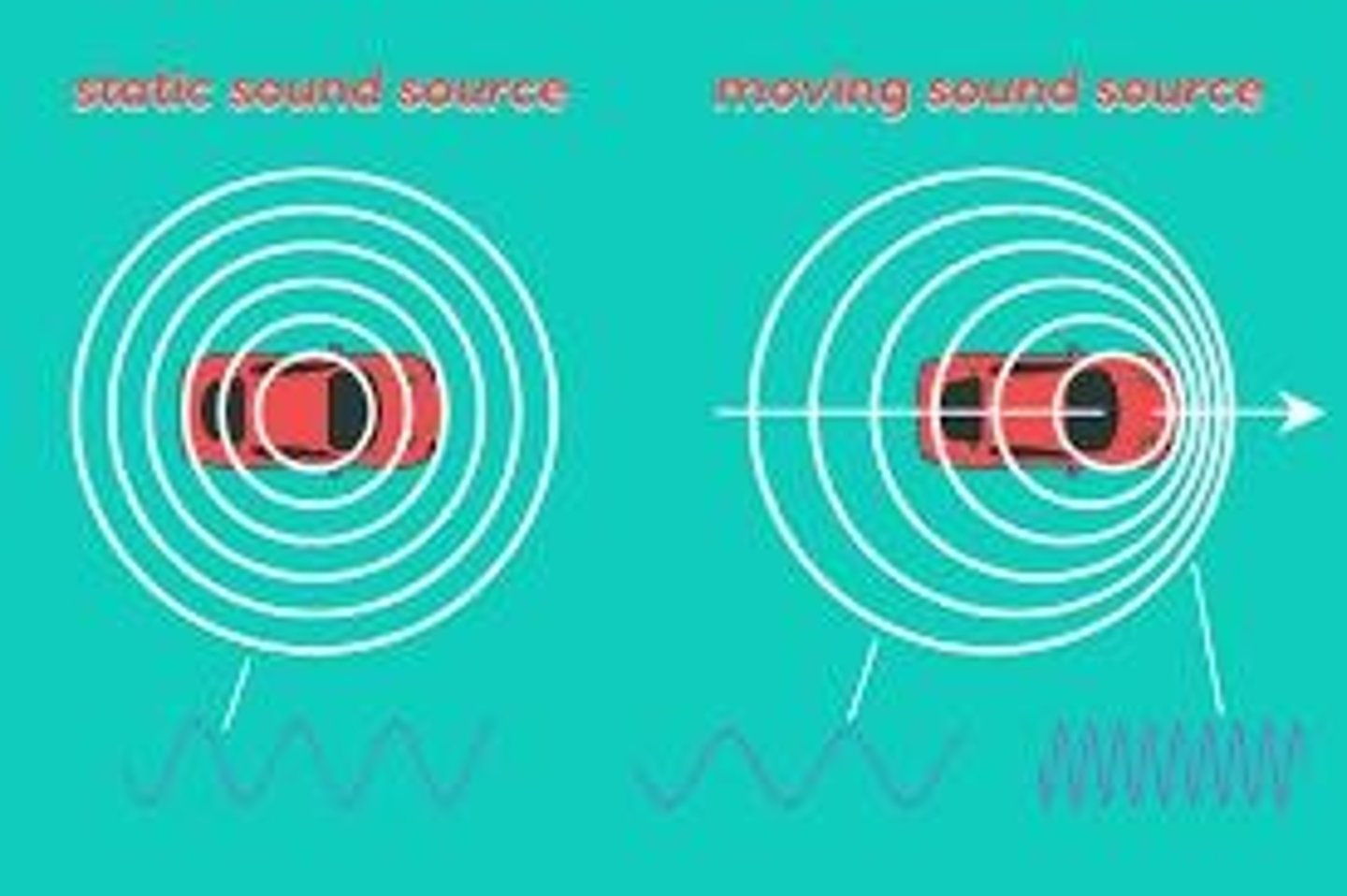
What equation computes the frequency change in the Doppler Effect?
Δf = 2v/c f cos(θ)
How does the sign of the Doppler shift change?
The sign changes when the source passes the observer, as cos(θ) changes sign.
What is a common application of the Doppler Effect in medicine?
Measuring the speed of blood particles to detect abnormalities in blood flow.
What are the advantages of ultrasound imaging?
No harmful side effects, real-time imaging, visibility of tissues without contrast agents, patient-friendly, quantification of blood velocity, and compact equipment.
What are the disadvantages of ultrasound imaging?
Limited depth range (approx. 25 cm), inability to scan bone or lung tissue, speckle interference, reverberation, acoustic shadowing, and refraction distortion.
What is the structure of an atom?
The nucleus consists of neutrons (no charge) and protons (positive charge), with electrons (negative charge) grouped in energy levels around the nucleus.
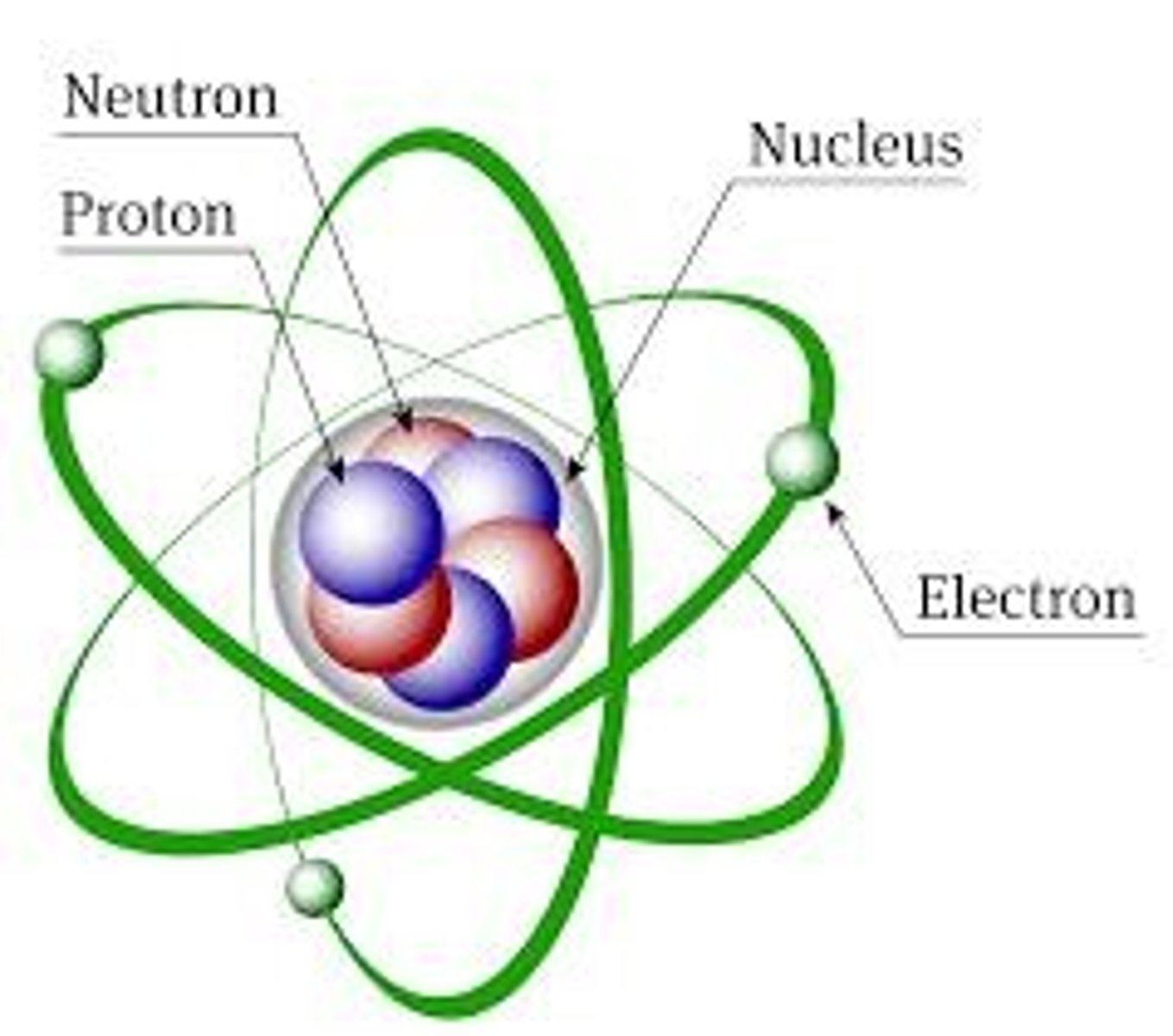
What determines the mass of an atom?
The number of nucleons, which is the sum of protons and neutrons.
What is electromagnetic radiation?
Waves of the electromagnetic field that propagate through space, carrying electromagnetic energy, including radio waves, microwaves, infrared, light, ultraviolet, X-rays, and gamma rays.
What is Planck's constant?
A fundamental constant used to calculate the energy of a photon, approximately 6.6 x 10^-34 Js.
How is the energy of a photon calculated?
Using the formula ε = h f = h c/λ.
Why can X-rays penetrate the body?
Because X-rays have a wavelength that is 10^6 times smaller than that of visible light.
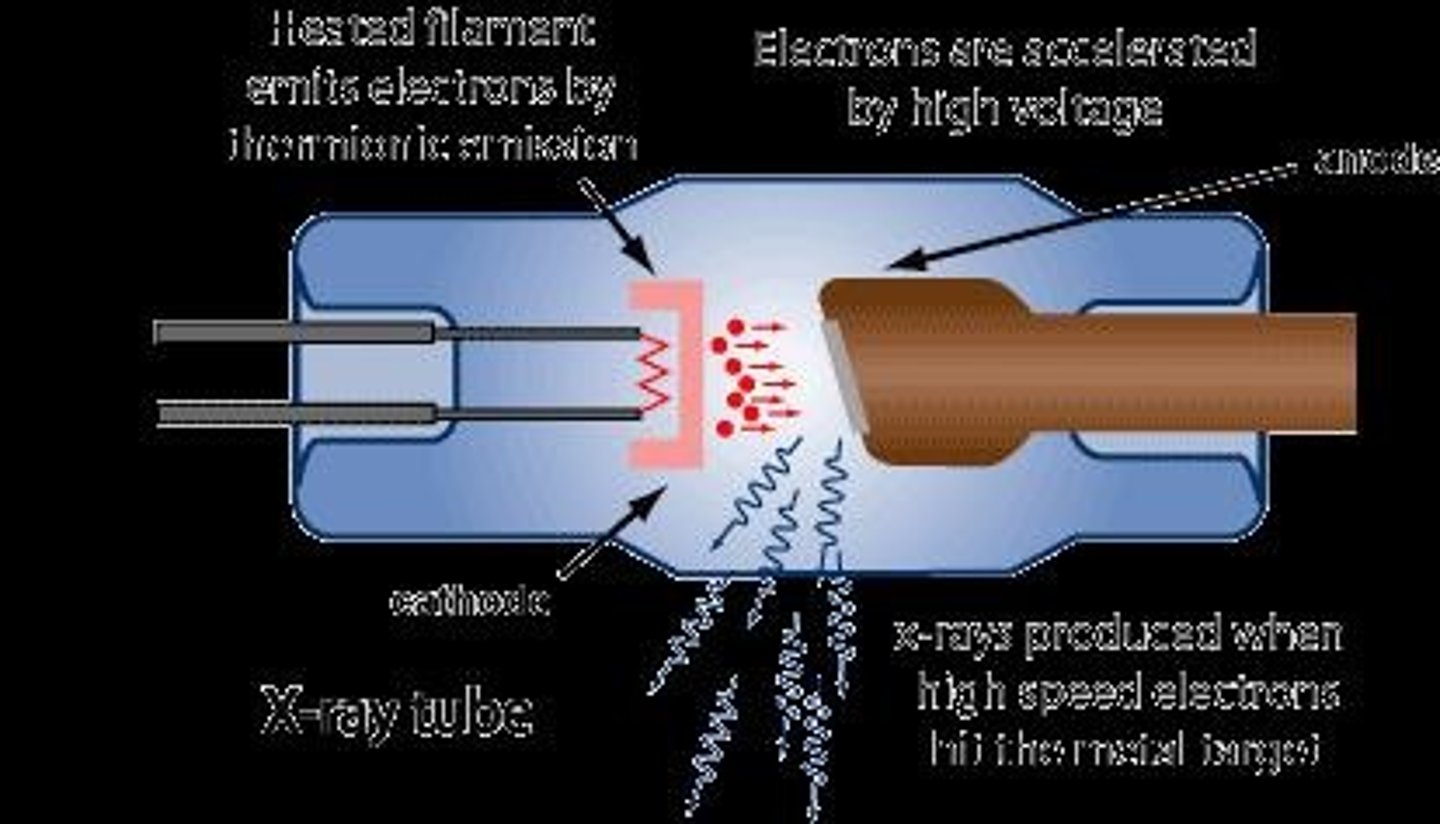
What is the function of an X-ray tube?
To convert electrical input power into X-rays, enabling radiography and other applications.
What happens when electrons hit the anode in an X-ray tube?
Kinetic energy is converted into X-rays through breaking radiation and characteristic radiation.
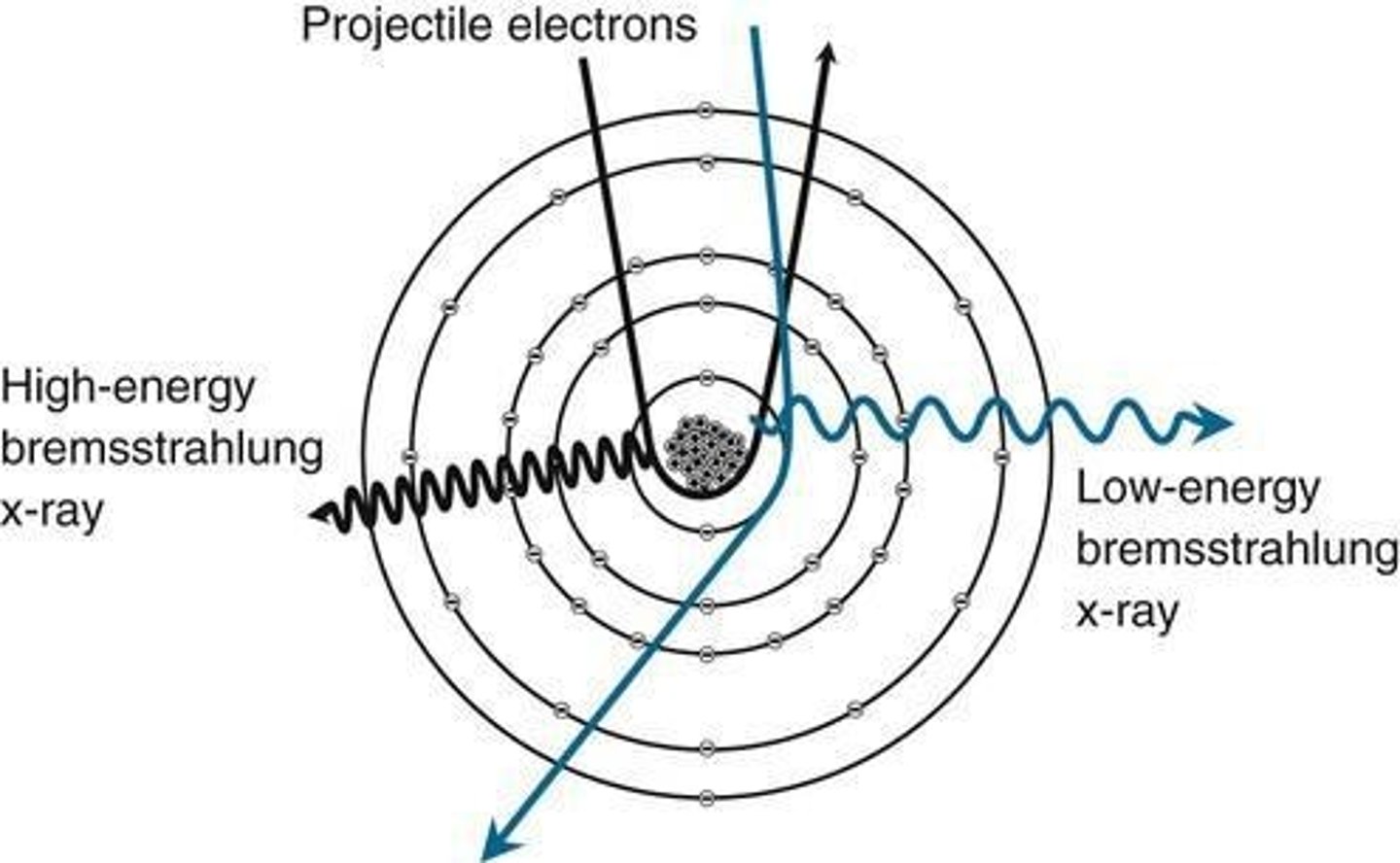
What is bremsstrahlung radiation?
Radiation produced when an incoming electron interacts with a nucleus, causing it to bend and lose energy as an electromagnetic photon.
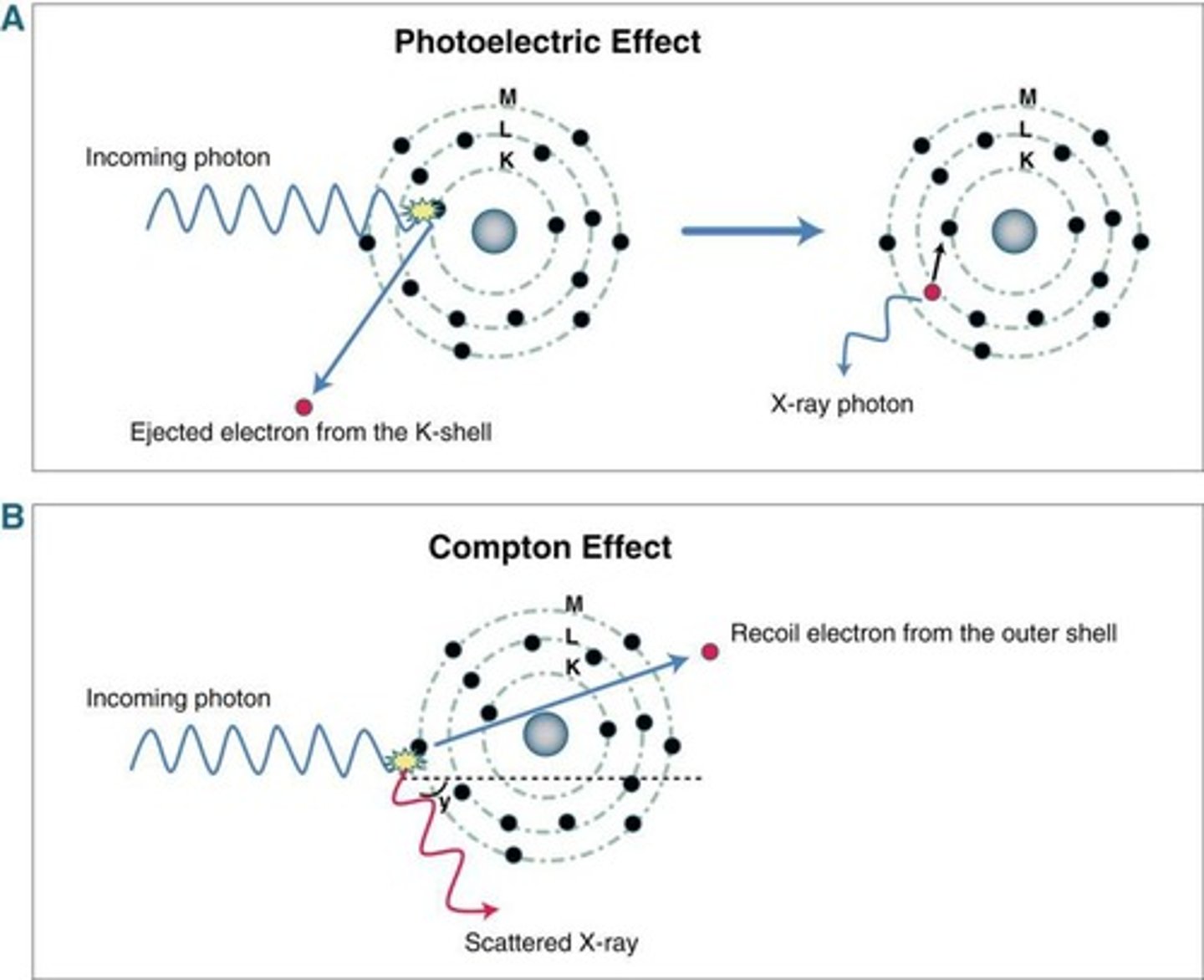
What is characteristic radiation?
Radiation generated when an incoming electron collides with a bound electron, freeing it and creating an X-ray photon from the energy difference.
What is the X-ray spectrum?
The spectrum of emitted X-rays obtained by dispersion with a crystal grating or ruled grating.
How does the X-ray spectrum change with tube voltage?
The spectrum shifts to the right with a higher X-ray tube voltage.
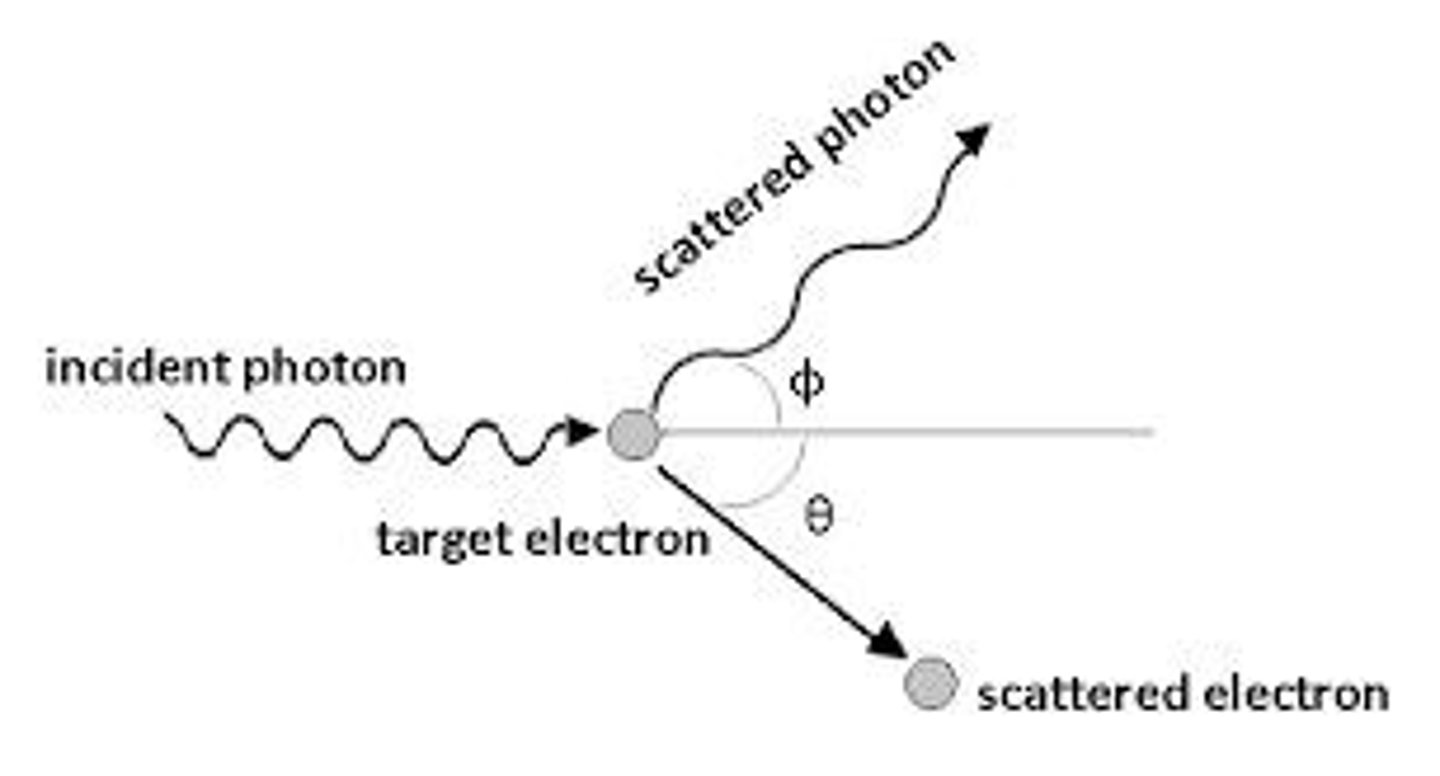
What is Compton scattering?
The interaction of an X-ray photon with an outer shell electron, resulting in energy loss and a change in direction of the photon.
What is the photoelectric effect?
The interaction of an X-ray photon with a bound electron, causing the ejection of the bound electron from its shell.
What formula computes the intensity of radiation?
I = I0 e^(-Σμi zi) or I = I0 e^(-∫μ(z) dz).
What factors influence attenuation by Compton scattering?
It is independent of atom number (Z) and X-ray energy (E), but proportional to density (ρ).
What is the relationship between tube current and X-ray production?
A larger tube current induces more X-ray photons.
What is the significance of the linear attenuation coefficient?
It quantifies how much the intensity of radiation decreases as it passes through a material.
What is attenuation by Compton scattering independent of?
Atom number (Z) and X-ray energy (E)
What is the relationship between attenuation and density in Compton scattering?
Attenuation is proportional to density (ρ).
How does the photoelectric effect relate to biological effects of ionizing radiation?
Ejected electrons can contribute to detrimental biological effects, such as cancer.
At what energy levels does the photoelectric effect become more significant?
At low energies, accentuating differences in atomic composition.
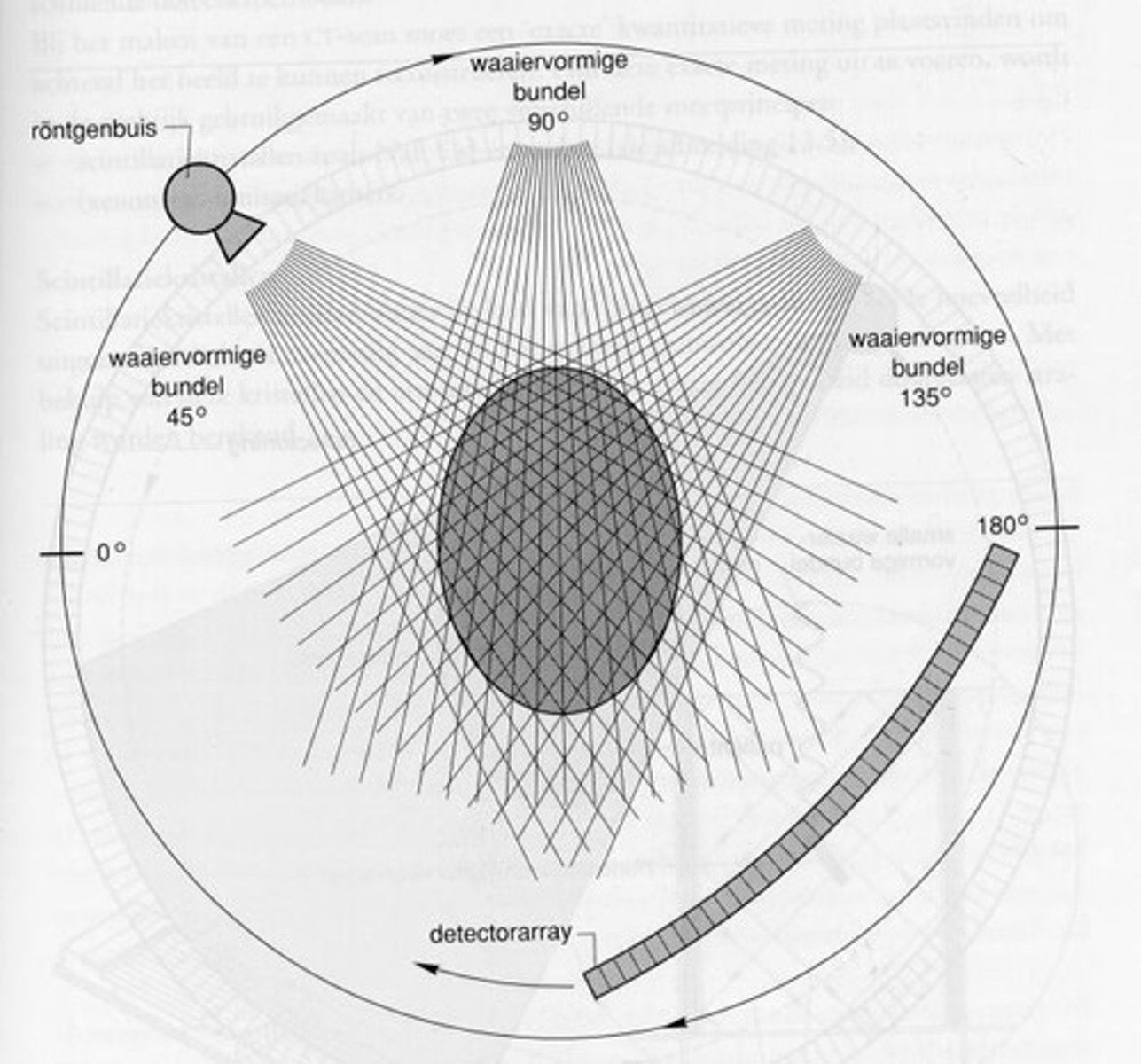
What does a CT image represent?
A cross-sectional image created by recording the attenuation of X-rays as the tube revolves around a body.
What does a high CT number indicate in a CT image?
White areas correspond to high CT numbers.
What is the equation for calculating the CT number?
CT Number = 1000 * (μ_pixel - μ_water) / μ_water
What are the three image reconstruction techniques discussed in CT imaging?
Algebraic image reconstruction, Filtered backprojection, Fourier based reconstruction.
What is the advantage of algebraic image reconstruction?
It allows for the incorporation of prior knowledge into the reconstruction process.
What is backprojection in CT imaging?
The equal redistribution of measured attenuation over the ray measurement.
What is the effect of applying a high pass filter before backprojection?
It enhances high frequencies, resulting in a sharper image.
What is the role of Fourier transforms in Fourier based reconstruction?
They reconstruct the image by approximating the Fourier transform of the CT image using attenuation profiles.
What is a sinogram?
A collection of all the attenuation profiles measured during CT imaging.
What is absorbed dose measured in?
Joules per kilogram, equivalent to Gray (Gy).
What does effective dose account for in radiation protection?
Differences in radiation sensitivity among various organs.
What are deterministic effects of radiation?
Effects that cause cell death and have a threshold dose below which no effects are observed.
What are stochastic effects of radiation?
Effects such as cancer induction and genetic effects, which have no threshold dose and increase in probability with dose.
What is magnetic resonance imaging (MRI)?
A medical imaging technique that uses strong magnetic fields and radio waves to generate images without ionizing radiation.
What is the significance of spin in NMR?
Spin is an intrinsic form of angular momentum that affects how particles behave in a magnetic field.
What is the Larmor frequency?
The precession frequency of a particle in a magnetic field, dependent on the gyromagnetic ratio and applied field.
What happens to net magnetization at equilibrium in MRI?
It aligns in the direction of the main magnetic field.
What occurs when a radiofrequency wave is applied at Larmor frequency?
It alters the alignment of the spin, allowing energy absorption by protons.
What is the Larmor frequency's effect on net magnetization?
It causes the net magnetization to rotate away from the Z-axis.
What are the two independent effects observable in MRI?
T1 relaxation (longitudinal magnetization recovery) and T2 relaxation (transverse magnetization decay).
What does T1 relaxation describe?
The process by which net magnetization (M) returns to its initial maximum value (Mo) parallel to Bo.
What is the equation for longitudinal magnetization recovery during T1 relaxation?
Mz = M0(1 - e^(-t/T1)).
At what time does M reach approximately 63% of its maximum value (Mo) during T1 relaxation?
At t = T1.
How does T1 relaxation time change with magnetic field strength?
T1 constant increases with magnetic field strength.
What does T2 relaxation describe?
The decay or dephasing of transverse components of magnetization (Mxy).
What is the equation for the decay of transverse magnetization during T2 relaxation?
Mxy = M0 * e^(-t/T2).
What is the time required for transverse magnetization to fall to approximately 37% of its initial value?
This time is known as T2 relaxation time.
What are the main causes of T2* relaxation?
Molecular interaction and dephasing spins due to field inhomogeneities.
What is the purpose of a spin echo sequence in MRI?
To compensate for inhomogeneities in magnetization and to measure T2 accurately.
What is the role of TR (repetition time) and TE (echo time) in MRI?
They control image contrast and the weighting of the MR image.
What combination of TR and TE values results in T1-weighted imaging?
Short TR/Short TE.
What combination of TR and TE values results in T2-weighted imaging?
Long TR/Long TE.
What happens to T1 effects when TR is long compared to T1?
T1 effects disappear as tissues have time to recover from the excitation pulse.
What is the significance of using a long TE compared to T2 in T2-weighting?
It increases the importance of the exponential weighting term, highlighting differences in tissue signal decay.
What is proton density contrast in MRI?
It is the contrast based on the initial magnetization (Mz) of tissues, influenced by their proton density.
What is the effect of long TR and short TE on MR imaging?
It gives proton density weighting.
What is the relationship between TR, TE, and T2 weighting?
Long TR and intermediate TE gives T2 weighting.
What is the relationship between TR, TE, and T1 weighting?
Intermediate TR and short TE gives T1 weighting.
What is the significance of the echo time (TE) in MRI?
It is the time between the initial excitation and the echo.
What is the significance of the repetition time (TR) in MRI?
It is the time between two consecutive excitations.
What does a spin echo sequence compensate for?
Inhomogeneities in magnetization, but not for dephasing due to pure T2 decay.
What is the main difference between T1 and T2 relaxation processes?
T1 involves recovery of longitudinal magnetization, while T2 involves decay of transverse magnetization.
What is the typical range for T1 values in biological materials?
From a few tenths of a second to several seconds.
What effect does shortening Te have on T2 influence?
Shortening Te reduces T2 influence.
What is a gradient in MRI?
A gradient is a progression in the magnetic field, defined as change in field (ΔB) divided by change in frequency (Δf).
What is slice selection in MRI?
Slice selection localizes the signal by using an RF pulse to activate a specific slice, flipping the magnetic vector of its nuclei to the transverse plane.
How does RF pulse frequency affect slice selection?
Changing the RF pulse frequency moves the selected slice up and down the z-axis.
What is the relationship between gradient strength and image slice size?
A larger gradient results in a smaller image slice, while a smaller gradient results in a larger image slice.
What is K-space in MRI?
K-space is an array of numbers representing spatial frequencies in the MR image, sampled each time an echo is acquired.
How is frequency encoding achieved in MRI?
Frequency encoding is achieved by switching on a magnetic field gradient while the echo is sampled, causing spins to precess with location-dependent Larmor frequencies.
What is phase encoding in MRI?
Phase encoding involves briefly switching on a gradient before the echo is sampled, resulting in location-dependent phase shifts among spins.
What is a disadvantage of MRI compared to CT imaging?
MRI scans are noisier, take longer, may cause claustrophobia, and are costlier than CT scans.
In what scenario is a CT scan preferred over an MRI?
CT is preferred for abdominal pain as it is more readily available and accurate in emergency situations.