CH 8
1/96
Earn XP
Description and Tags
Vocabulary flashcards related to joints, their structure, classification, and common conditions.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
97 Terms
Joints (Articulations)
Locations where two or more bones meet; points at which movements of bones can occur.
Synarthrosis
Functional joint classification; no movement allowed and extremely strong.
Amphiarthrosis
Functional joint classification; little movement allowed, stronger than diarthrosis, connected by collagen fibers or cartilage.
Diarthrosis
Functional joint classification; freely movable.
Fibrous: Suture
Structural joint classification; synarthrotic joint connected by dense fibrous connective tissue, located between bones of the skull.
Fibrous: Gomphosis
Structural joint classification; synarthrotic joint binding teeth to bony sockets in maxillae and mandible.
Fibrous: Syndesmosis
Structural joint classification; amphiarthrotic joint with bones connected by a ligament (e.g., distal joint between tibia and fibula).
Cartilaginous: Synchondrosis
Structural joint classification; synarthrotic joint formed by a rigid, cartilaginous bridge between two articulating bones (e.g., between ends of the first pair of ribs and the sternum).
Cartilaginous: Symphysis
Structural joint classification; amphiarthrotic joint where articulating bones are separated by a pad of fibrocartilage (e.g., joint between the two pubic bones).
Bony: Synostosis
Structural joint classification; synarthrotic, totally rigid, immovable joint formed when bones fuse (e.g., frontal suture and epiphyseal lines).
Synovial
Structural joint classification; diarthrotic joints permitting a wider range of motion, located at the ends of long bones.
Articular cartilage
Covers bones at joints like hyaline cartilage but with more water and no perichondrium.
Joint capsule (Articular capsule)
Sac enclosing the articular ends of bones in a joint, reinforced with tendons and ligaments.
Synovial membrane
Lines the interior of the joint capsule and secretes synovial fluid.
Synovial fluid
Clear, straw-colored, viscous fluid that lubricates, provides nutrients and takes out waste, shock absorption. cushions, and prevents abrasion in a joint.
Bursa
Small, thin, fluid-filled pocket filled with synovial fluid and lined by synovial membrane, reduces friction and acts as a shock absorber.
Fat pads
Localized masses of adipose tissue covered by a layer of synovial membrane, protect articular cartilage, and fill spaces created as the joint moves.
Meniscus (Articular disc)
Pad of fibrocartilage between opposing bones in a synovial joint, may subdivide a synovial cavity and channel synovial fluid flow.
Capsular ligaments / Intrinsic ligaments
Localized thickenings of the joint capsule.
Extrinsic ligaments
Ligaments separate from the joint capsule, either outside (extracapsular) or inside (intracapsular).
Dislocation (Luxation)
Movement beyond the normal range of motion; articulating surfaces forced out of position.
Gliding
Linear motion, permits sliding motion in any direction on a relatively flat surface.
Angular motion
Movement along two axes in one plane, involves a change in angle.
Circumduction
Complex angular movement where the proximal end of bone remains fixed while the distal end moves in a circular path.
Rotation
Movement around the longitudinal axis.
Monoaxial
Around one axis
Biaxial
Around two axes
Triaxial
Around three axes
Flexion
Decreases the angle of the joint.
Extension
Increases the angle of the joint.
Hyperextension
Extension past the anatomical position.
Lateral flexion
Bending the vertebral column to the side, most pronounced in cervical and thoracic regions.
Dorsiflexion
Upward movement of the foot or toes.
Plantar flexion
Movement extending the ankle, as in standing on tiptoe.
Abduction
Movement away from the longitudinal axis in the frontal plane.
Adduction
Movement toward the longitudinal axis in the frontal plane.
Circumduction
Moving a body part such that the distal end traces a circle while the proximal end stays in one position.
Medial rotation
Anterior surface of a limb turns toward the long axis of the trunk.
Lateral rotation
Anterior surface of a limb turns away from the long axis of the trunk.
Pronation
Distal epiphysis of radius rolls across the anterior surface of the ulna, turning the wrist and hand from palm facing front to palm facing back.
Supination
Opposing movement to pronation; palm is turned anteriorly.
Opposition
Movement of the thumb toward the surface of the palm or pads of other fingers.
Inversion
Twisting motion turning the sole inward.
Eversion
Opposing motion to inversion; turning the sole outward.
Protraction
Moving a part of the body anteriorly in the horizontal plane.
Retraction
Reverse of protraction; returning the body part to normal position.
Depression
Moving a body part inferiorly (as in opening your jaw).
Elevation
Moving a body part superiorly (as in closing your jaw).
Atlanto-occipital joint
Articulation between the occipital bone and atlas
Atlanto-axial joint
Articulation between C1 and C2
Sternoclavicular joint
Articulation between the axial skeleton and pectoral girdle and upper limb
Sacro-iliac joint
Attaches the sacrum of axial skeleton to the pelvic girdle.
Syndesmoses of vertebral column
Fibrous joints including vertebral ligaments.
Synchondroses of vertebral column
Intervertebral joints, forming intervertebral discs.
Vertebral synovial joints
Joints between bony processes.
Anulus fibrosus
Tough outer ring of fibrocartilage in an intervertebral disc, collagen fiber attach to adjacent vertebrae
Nucleus pulposus
Soft, elastic, gelatinous core of an intervertebral disc. Gives disc resilience and shock absorption ability
Ligamentum flavum
Connects laminae of adjacent vertebrae.
Posterior longitudinal ligament
Connects posterior surfaces of adjacent vertebral bodies.
Interspinous ligament
Connects spinous processes of adjacent vertebrae.
Supraspinous ligament
Connects tips of spinous processes from the sacrum to C7; Ligamentum nuchae extends from C7 to base of the skull.
Anterior longitudinal ligament
Connects anterior surfaces of adjacent vertebral bodies.
Bulging disc
Caused by weakened posterior longitudinal ligaments, allows compression of nucleus pulposus and distortion of anulus fibrosus. Tough, outer layer of cartilage bulges laterally.
Herniated disc
Nucleus pulposus breaks through anulus fibrosus and protrudes into the vertebral canal, compressing spinal nerves.
Osteopenia
Inadequate ossification leading to loss of bone mass.
Osteoporosis
Bone loss sufficient to affect normal function.
Shoulder joint (Glenohumoral joint)
Articulation between the head of the humerus and the glenoid cavity of the scapula.
Glenoid labrum
Fibrocartilage rim that increases the area of the glenoid cavity.
Acetabular labrum
Rim of fibrocartilage that increases the depth of the joint cavity and helps to seal in synovial fluid
Elbow joint
Complex hinge joint involving humerus, radius, and ulna.
Humeroradial joint
Capitulum of humerus articulates with head of radius.
Humero-ulnar joint
Largest and strongest articulation of elbow; trochlea of humerus articulates with the trochlear notch of the ulna.
Nursemaid’s elbow
Partial dislocation of the radial head from annular ligament.
Radial collateral ligament
Stabilizes the lateral surface of the elbow joint.
Annular ligament
Binds the head of the radius to the ulna.
Ulnar collateral ligament
Stabilizes the medial surface of the elbow joint.
Medial and lateral menisci
Pair of fibrocartilage pads between femoral and tibial surfaces.
Rheumatism
General term indicating pain and stiffness in the bones and/or muscles.
Arthritis
All rheumatic diseases that affect synovial joints; always involves damage to the articular cartilage.
Osteoarthritis
Most common form of arthritis, generally affects individuals age 60 or older; caused by wear and tear on joints and genetic factors.
Arthroscope
Narrow, flexible fiberoptic tube with tiny camera used to explore a joint without major surgery.
Accessory structures supporting the knee are
Bursa, Fat pads, Meniscus, Ligaments, Tendons
Hip joint reinforcing ligaments
include the Iliofemoral, Ischiofemoral, and Pubofemoral ligaments, which provide stability and support to the hip joint.
Transverse acetabular ligament
Crosses the acetabular notch, filling gap in the inferior border of the acetabulum
Ligamentum teres /ligament of the femoral head
Originates along the transverse acetabular ligament • Attaches to the fovea capitis
Why is the elbow joint stable
The bony surfaces of the humerus and ulna interlock
2. A single, thick articular capsule surrounds both the humero-ulnar and proximal radio-ulnar joints
3. Strong ligaments reinforce the articular capsule
proximal radio-ulnar joint
not part of the elbow joints, capsule and ligaments help hold the humerus, ulna and radius in position
Knee joint
contains 3 seperate articulations that permit flexion, extension and very limited rotation
Two articulations of the knee joint between the femur and tibia
Medial condyle of tibia to medial condyle of femur
Lateral condyle of tibia to lateral condyle of femur
Is fibula part of the knee joint?
NO
Quadriceps tendon (knee joint)
continues as patellar ligament to anterior tibial surface
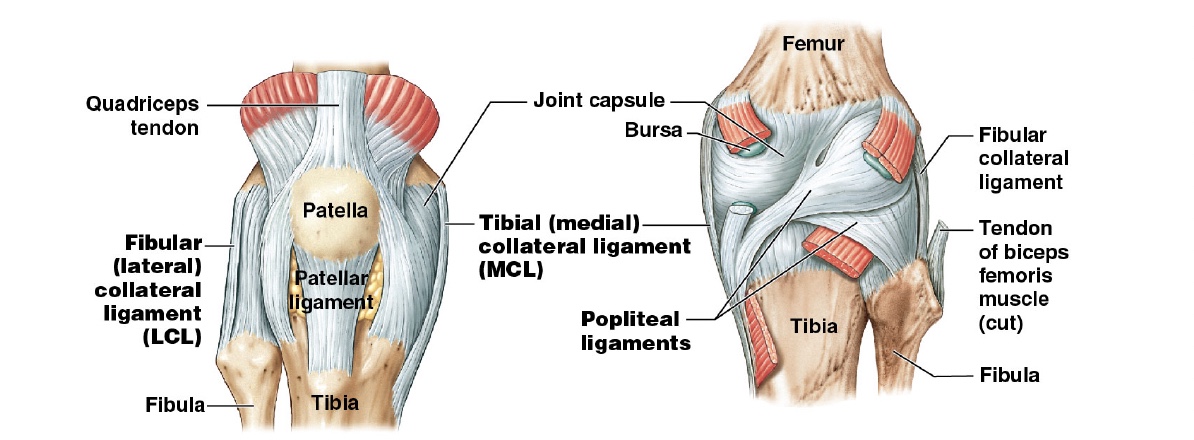
Fibular collateral ligament (knee joint)
provides lateral support
Tibial collateral ligament/ medial collateral ligament (knee joint)
provides medial support
popliteal ligament
run between femur and heads of the tibia and fibula
Medial and lateral menisci (hip joint)
pair of fibrocartilage pads, located between a femoral and tibial surfaces, acts as cushion and provide lateral stability
Anterior cruciate ligament (ACL) (hip joint)
At full extension, slight lateral rotation of tibia tightens ACL and forces lateral meniscus between tibia and femur • This “locks” knee in extended position • Opposite motion is required to “unlock”
PCL (Hip joint)
Posterior cruciate ligament (PCL)