Conjunctiva
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
16 Terms
Red Eye Overview History
Discharge (profuse/severe – gonorrhea conj)
What color (yellow green – bacterial, white – allergic)?
Both eyes (allergic or viral)? Started in one eye then delayed response other eye (Bacterial or EKC)
Unilateral (trauma or bacterial bleph on side of pillow)?
Recent Trauma (Traumatic iritis)?
Itchy (allergic, if intense then VKC or AKC atopic)?
Flu-like symptoms or fever (viral)? Watery (allergy)?
Eyelids stuck upon waking (bacterial)?
Objective General
- Lymph node swelling – EKC, Chlamydia, HSV, Gonorrhea, Parinauds, pthisis
- Follicles: CHAT – Chlamydia, herpes, Adenovirus (EKC), toxic including pediculosis and molluscum
Trachoma chlamydia (follicles superior)
A Chel (follicles below
- Papillae – pABillae – allergy/atopy, bacterial, gonorrhea
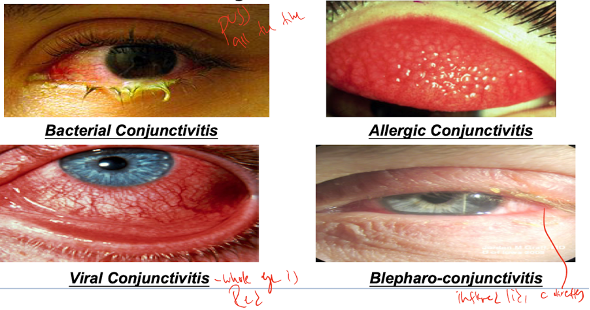
Painful red eye, photophobia, swelling, yellowish-green discharge, tearing, blurred vision
Bacterial infection causing inflammation of the white part of the eye.
Objective: Mild purulent white-yellow discharge. Papillae, chemosis and NO tender lymph nodes.
Plan: Moxifloxacin 0.5% (Vigamox) TID for 7-10 days (Polytrim for children q3h)
RTC 2-3 days then 5-7 days until stable. Consider swabbing the conjunctiva if the infection doesn’t get better.
Itching, burning, photophobia, FB sensation, blurred vision
Acute Allergic Conjunctivitis seasonal and perennial
Symptoms: itching, burning, photophobia, FB sensation, blurred vision
Objective: chemosis, watery discharge
Plan: 0.2% pataday BID. Follow up in 4 weeks
Chronic Allergic conjunctivitis
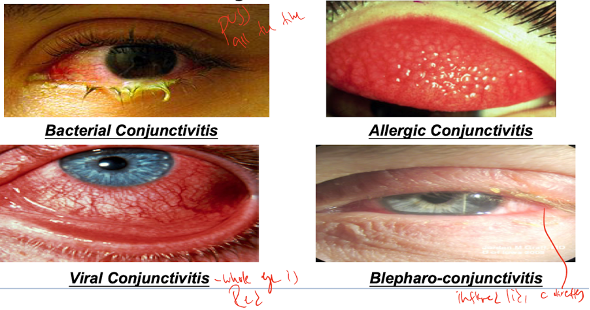
Vernal: intense itching in young males
Objective: cobblestone papillae (upper lid) + trantas dots at limbus. Can have shield ulcer in severe case

Plan: Loteprednol 0.2% QID and 0.2% pataday BID. Follow up in 1-2 week.
If shield ulcer present in VKC: pred forte 1% 4-6x per day, Polytrim QID, cyclo 1% TID, cool compress. RTC 1-3 weeks for IOP and cornea check.
Atopic: associated with atopic condition (eczema, asthma, atopic dermatitis) in children and young adults. Papillae mostly on lower lid.
Plan: Tacrolimus ointment twice a day for 1-2 weeks
GPC: hypersensitivity rxn caused by contact lens.
Plan: Loteprednol 0.2% QID and 0.2% pataday BID. Follow up in 1-2 week.
Fever + red eye + FBS
Viral Conjunctivitis
Pharyngoconjunctival fever (PCF): fever, pharyngitis, and acute follicular conjunctivitis, more common in children spread by respiratory secretions.
Objective: preauricular lymph node enlargement
Plan: Educated patient on infectious nature, so avoid spread. No treatment is needed at this time. It usually lasts 4 days to 2 weeks
Palliative: NSAID, cool compress, ATs
Epidemic Keratoconjunctivitis (EKC)
Symptoms: consisting of fever, malaise, and myalgias followed by a red eye, eyelid edema, excessive tearing, irritation, foreign body sensation, and photophobia
Objective findings: Objective Findings: follicular response (in viral, toxic or chlamydia), pseudo membranes in severe cases, gritty sensation, watery discharge, sticky in mornings, chemosis, injection, CORNEAL INVOLVEMENT - SPK, Sub epithelial infiltrates possible, positive lymph nodes, subconj hemes
Rule of 8s: serotype 8. symptoms occur 8 days after exposure. SEIs develop 8 days after onset of symptoms and at that point it's not contagious.
Workup: AdenoPlus
Plan:
Betadine 5% use within first 7 days to remove active virus
Lotemax QID OU if corneal involvement
F/U in 4 weeks or RTC prn

irritation, watery eyes, usually unilateral, mild pain/discomfort), younger paient, fast onset
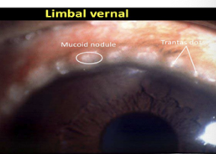
Episcleritis: self-limiting, recurring, idiopathic inflammation of the episcleral tissue that does not threaten vision. May be associated with connective tissue disease or autoimmune disease if recurrent. (nodular is more associated with systemic dx than simple - sectorial/diffuse)
Workup: phenylephrine (blanches episcleritis, no blanch if scleritis). if nodular, then moves with pressure(in scleritis, it doesn’t move)
Plan:
Mild case then AT and cold compress
mod/Severe or chronic: vasoconstrictors, topical NSAIDs (ketorolac QID) and steroid FML 0.1% qid. Ibuprofen 600 mg TID
Pt ed: self limiting and can recur, but not life threatening
RTC q2-4 weeks. if on steroid then every week. do systemic workup if more than 3 recurrences

Severe, boring pain that radiates to the face and wakes the patient at night. Pain on eye movement and touch. Slower onset, older patient
Scleritis: an inflammation of the sclera, the white outer layer of the eye. It is a rare but serious condition that can cause severe pain, redness, and vision loss.
Diffuse: most common (40-80%), least severe, painful, red eye without dec VA, associated with RA, HZV, gout (20% become necrotizing scleritis)
Nodular: tender, bilateral, severe pain
Necrotizing type WO inflammation: NO PAIN, bilateral, scleromalacia (usually from long standing Rheumatoid arthritis). 50% of patients die from systemic vascular event
Necrotizing with inflammation: EXTREMELY PAINFUL, has severe autoimmune dx and 33% die or lose vision
Plan for non necrotizing:
Oral NSAID naproxen 250mg twice daily
Escalate to predinsone 1mg/kg/day
RTC in 5 days or PRN if symptoms persists. Educate about possible reoccurence and to RTC for systemic testing.
Plan for necrotizing:
Oral prednione 40-60mg until resolution then taper.
refer to rheumotologist for management of autoimmune dx
Posterior Scleritis: UNILATERAL. 50% association with systemic disease (RA most common). Also associated Iritis, keratitis, glaucoma, and exudative Retinopathy -50% association with systemic dx
Symptoms: periocular pain, blurred vision, and headaches • Deep, dull, boring pain with HA • Wakes them up at night • Restricted EOMs, HA, diplopia, proptosis, ptosis • May not have any redness
Objective: chemosis, hyperemia (30%), AC rxn (25%), Subretinal granuloma/fundus mass, choroidal folds, mac edema, disc edema, serous RD
Workup: B- Scan (T sign). Blood work for underlying systemic diseases, such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), or ANCA-associated vasculitis.
Plan: predinsone 1mg/kg/day. Refer to rheumotologist for management of systemic condition.
Systemic aspirin, NSAID (Naproxen 250-500 mg BID), steroid, immunosuppression. Refer to retina.
Severe purulent HYPERACUTE discharge
Gonorrhea conjunctivitis: Sexually transmitted infection causing inflammatory rxn in eyes.
Objective: Papillae, chemosis, lid edema. Node involvement.
Workup: NAAT and Chocolate agar, Thayer Martin, Gram Gram stain will show diplococci.
Plan: IV ceftriaxone 1 gram and oral azithromycin 1 gram BID for 7 days (to treat chlamydia in case)
If corneal involvement, fluoroquinolone QID q1hour.
Need to report to local heath department and test and treat sexual partners
Treatment for nenoates – erythromycin ung and ethylsuccinate 50mg/kg/day for 14 days
Red eye, discharge, lids stuck in the morning, foreign body sensation
May mistaken for viral conjunctivitis (hasn’t gotten better)
Inclusion Chlamydia: Sexually transmitted infection causing inflammatory rxn in eyes. Inform sexual partners.
Objective: Inferior tarsal or bulbar conj follicles, superior pannus, sub-epi infiltrates, stringy mucous. Node involvement.
Systemic: Discharge from penis or vagina, burning on urination
Workup: NAAT and Chocolate agar, Thayer Martin, Gram Gram stain will show diplococci.
Plan: Azithromycin 1 gram or doxy 100 mg BID for 7 days. Topical erythromycin ointment TID for 3 weeks.
RTC 2-3 weeks.
Trachoma Chlamydia: Trachoma is a chronic, infectious disease of the eye caused by certain strains of C. trachomatis. It's a leading cause of preventable blindness worldwide. Common in overcrowded area with poor hygiene and young ppl.
Objective: superior follicles, pannus, arlts sign and herbert pits, trichiasis, corneal opacification
Plan: doxycycline 100 mg PO bid x 7 days for systemic treatment + erythrmocyin ung TID for 6 weeks.
Need to report to local heath department and test and treat sexual partners
RTC 2-3 weeks
Red, irritated, and painful eye; fever; general lack of well-being; swelling of nearby lymph glands; increased tearing
Parinaud oculoglandular syndrome (POS) is an infection of the eyes caused by bacteria, a virus, fungus, or parasite. The most common causes are cat scratch disease (scratch or bite from cat) and tularemia (rabbit fever).
Objective: Granulomatous nodules on palpebral and bulbar conj. Ipsilat pre-auricular or submandibular nodes. Follicles, fever, rash
Workup: Cat scratch serology/skin test. CBC, RPR/VDRL, FTA-ABS, ACE, blood culture, PPD
Plan: Warm compress on nodes and tylenol or NSAID to reduce fever.
IF cat scratch then will spontaneously resolve in 6 weeks. Don't have to remove cat.
Treat underlying dx if present. Optional azithro or SMX-TMP, cipro. Antibiotic ointment.
RTC 1-2 week follow up
Bilateral red eye, middle aged
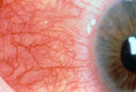
Ocular Rosacea: blood vessels in the eyes become dilated and fragile, leading to redness and flushing and have abnormal gland function leading to dry eyes. Triggers include
Objective: MGD, bleph, telangiectaisia, facial flush, papular/pustule skin lesion, thinopphyma, SPK, plyctenule, infiltrates
Plan: Avoid triggers, do warm compress BID, and lid hygeine.
Doxy 100mg twice daily for 1-2 weeks then taper to 20mg daily. Alt azithromycin
Rosacea escalation: Omega 3, cyclosporine or lifitegrast, topical steroids. Topical antibiotics if corneal ulcer. Treat chalazia
RTC?
Ocular cicatricial pemphigoid: autoiimmune disease that causes inflammation and scarring of the conjunctiva, the thin membrane that covers the white part of the eye
Objective: secondary conjunctivitis, SPK, corneal ulcer, dry eye syndrome, trichiasis, pannus, entropion, neo, keratinization, ankyloblepharon (pic above)
Workup: Slit lamp exam of fornices, gram stain and culture for infection, biopsy mucous membranes
Plan: AT, ung, autoglogous serum QID. Lid hygeine if bleph. Warm compress, erythromycin ung, orl doxycycline
Escalate: Moisture goggles, scleral lenses, punctal occlusion, topical steroid or oral steroid, immunosuppressant methotrexate
Surgery if indicated
RTC: 1-2 weeks during exacerbation, 1-6 months for remission
Contact dermatitis
Objective: Redness, Blisters, Edema, Intense itching, Peeling Orbital edema, erythema, vesicles, conj chemosis
Plan: Remove cause, cool compresses 4 times daily, artificial tears, topical antihistamine (ketotifen/Alaway). Tacrolimus ointment twice daily, FML 0.1% or loteprednol 0.5% twice daily, oral antihistamine.
Conj or corneal intraepithelial neoplasia: Most common conjunctival malignancy. (SCC precurser)
Plan: Refer for surgical excision and biopsy with Cryotherapy. Alt: mitomycin, 5F.U.
Primary acquired melanosis: Flat, brown pigment patch in the conj. Middle aged. Caucasian Risk of melanoma conversion.
Plan: Small: observe. Med: excision, biopsy, cryo.
DDx. Malignant melanoma on conj: Nodular brown vascularized mass, often feeder vessel. De novo, from nevus, or from primary acquired melanosis
Plan: DFE, TID, and ultrasound to look for ciliary body melanoma. Cryo and excision, biopsy lymph nodes for metastatic disease.
DDx. Malignant melanoma on iris. Unilat brown or translucent iris mass that grows slowly. Often inf half of iris. Caucasian. Assoc: Cortical cataract, ectropion, hyphema, darkening of iris, inc IOP
Plan: Exam every 3 months. Surgical resection if growing, blocking vision, causing glaucoma.
Ocular or oculodermal melanocytosis: congenital episcleral, not conjunctival, lesion. Will move if pushed with swab. unilateral, blue-gray, and often accompanied by a darker ipsilateral iris and choroid. Risk of uveal melanoma.