Topic 5 - Kidney
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
43 Terms
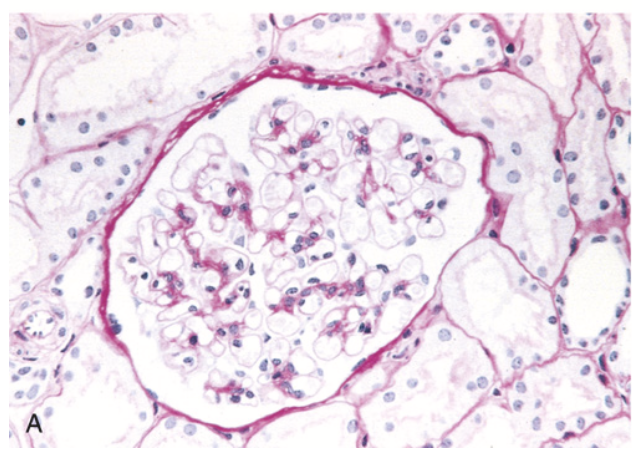
Minimal change disease. (A) Glomerulus showing normal basement membranes and absence of proliferation (PAS stain, which highlights polysaccharides and glycoproteins).
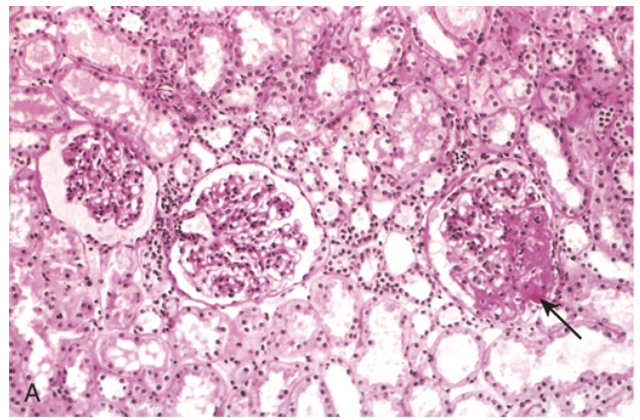
Focal segmental glomerulosclerosis (FSGS). (A) Low-power view showing focal sclerosis involving one of three glomeruli (arrow).
Focal segmental glomerulosclerosis (FSGS). (B) Involvement of a segment of a glomerulus, with sclerosis and hyaline deposit (arrow).
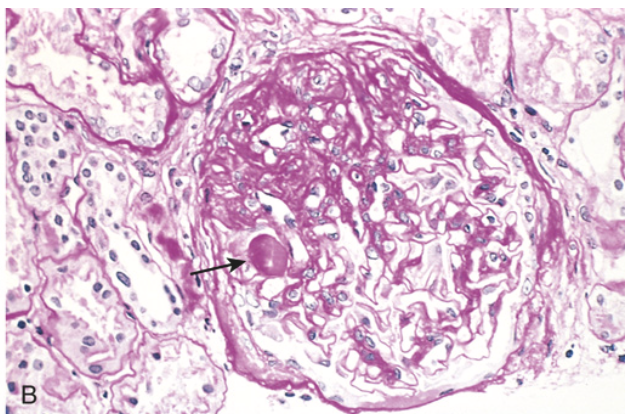
Membranous nephropathy. (A) Diffuse thickening of the glomerular basement membrane without proliferation of cells or inflammation (silver stain, which highlights proteins in the GBM).
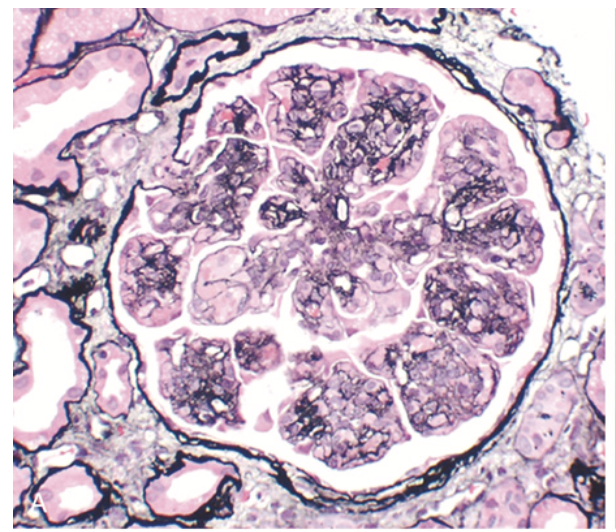
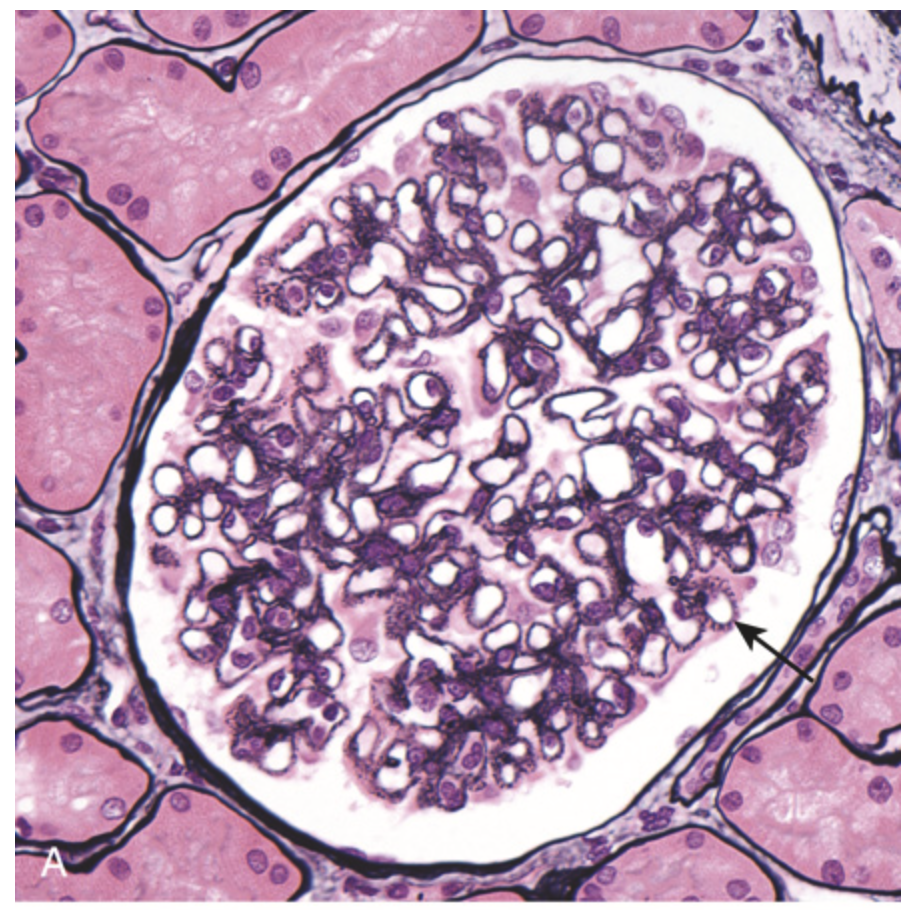
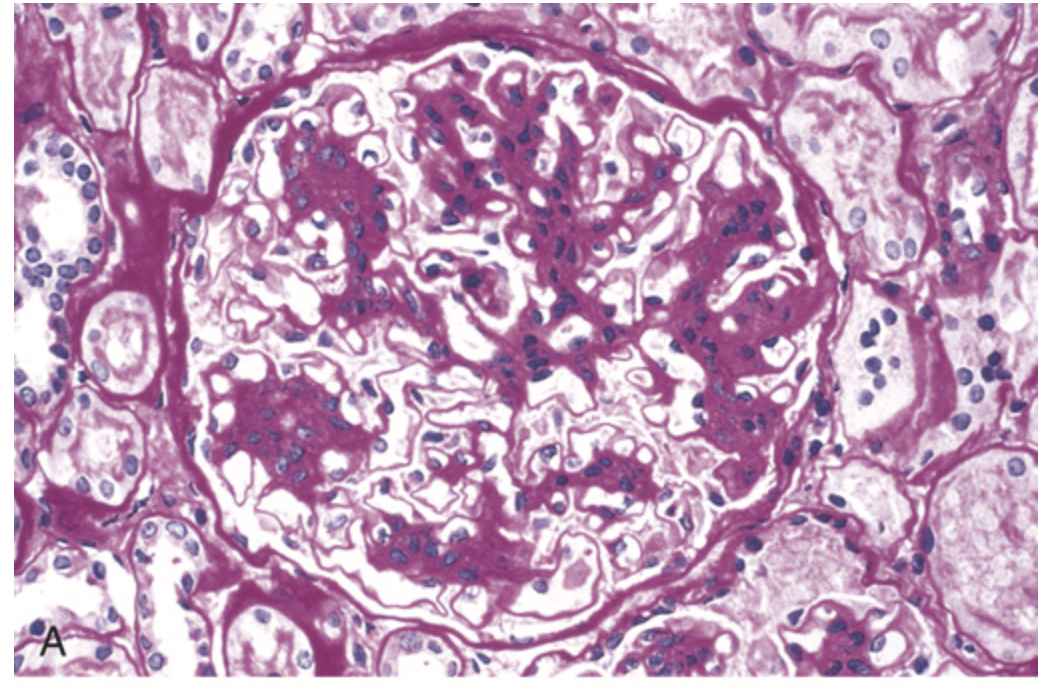
Membranoproliferative glomerulonephritis (MPGN). (A) Mesangial cell proliferation, increased mesangial matrix (staining black with silver stain), basement membrane thickening with segmental splitting, accentuation of lobular architecture, swelling of cells lining peripheral capillaries, and influx of leukocytes (endocapillary proliferation) (silver stain).
C3 glomerulopathy. (A) Glomerulus showing hypercellularity and increased mesangial matrix.
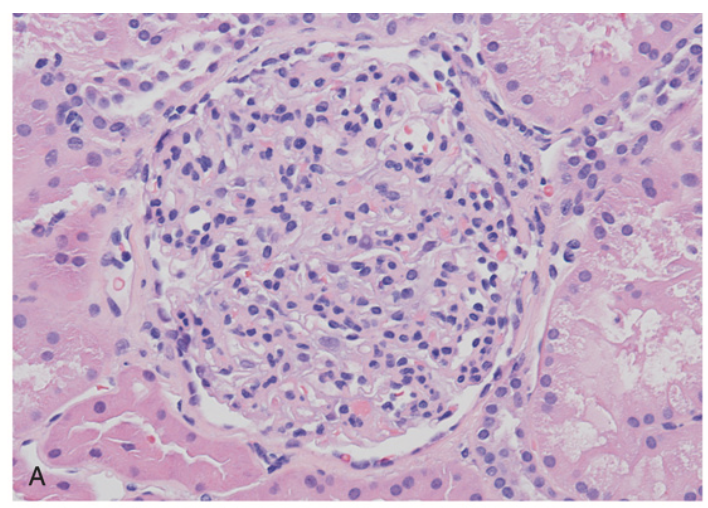
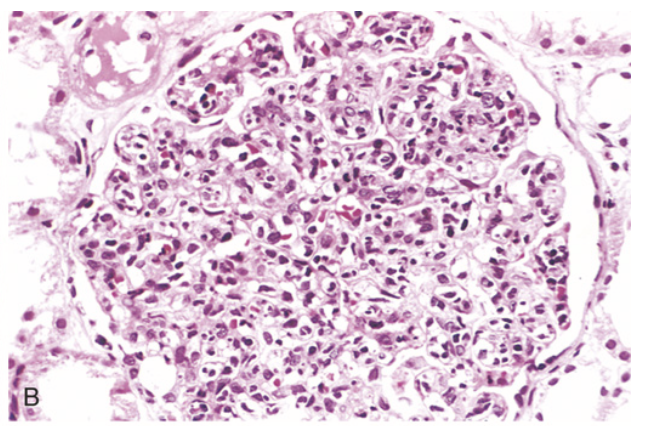
Acute poststreptococcal glomerulonephritis. (A) Glomerular hypercellularity due to intracapillary leukocytes and possibly proliferation of intrinsic glomerular cells.
Crescentic glomerulonephritis (A) Compressed glomerular tufts and crescent-shaped mass of proliferating epithelial cells and leukocytes within the Bowman capsule (PAS stain).
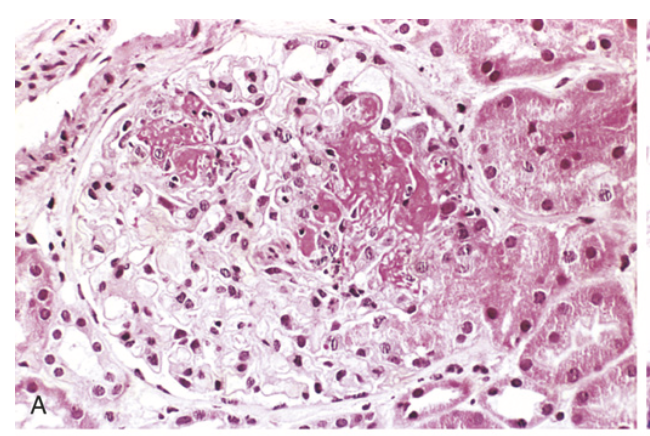
Lupus nephritis. (A) Focal proliferative glomerulonephritis, with two focal necrotizing lesions at the 11 o’clock and 2 o’clock positions (H&E stain). Extracapillary proliferation is not prominent in this case.
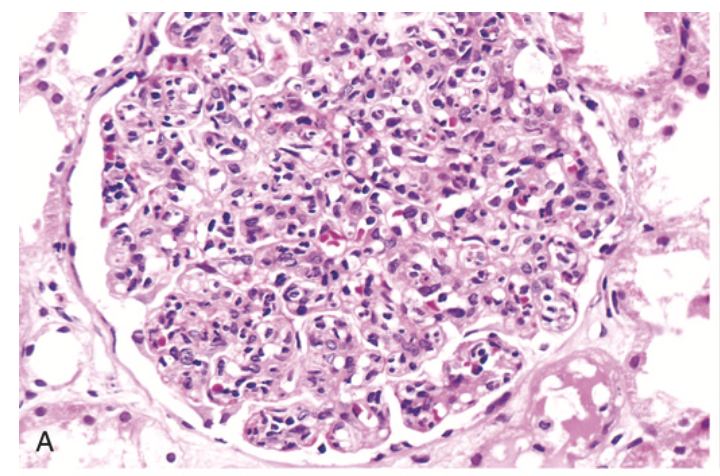
Lupus nephritis. (B) Diffuse proliferative glomerulonephritis. Note the marked increase in cellularity throughout the glomerulus (H&E stain).
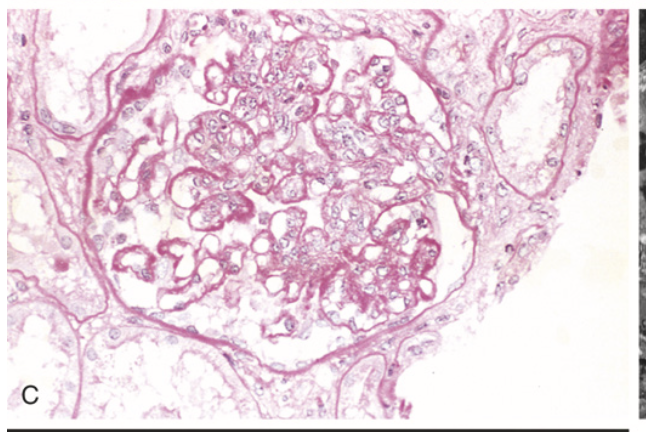
Lupus nephritis. (C) Lupus nephritis showing a glomerulus with several “wire-loop” lesions representing extensive subendothelial deposits of immune complexes (PAS stain).
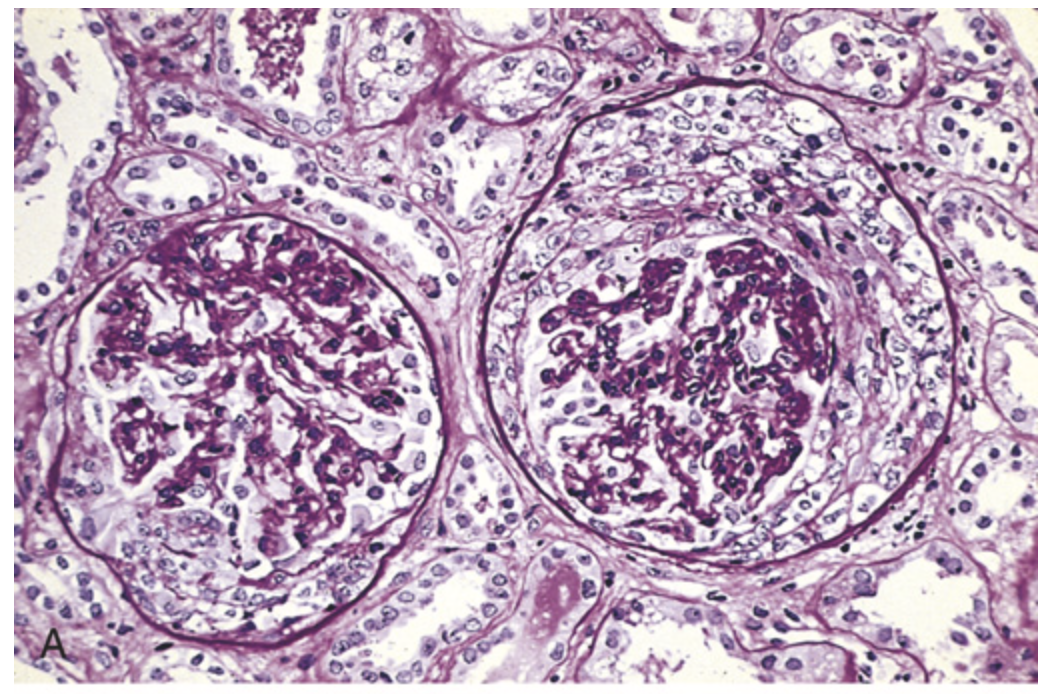
IgA nephropathy. (A) Light microscopy showing mesangial proliferation and matrix increase.
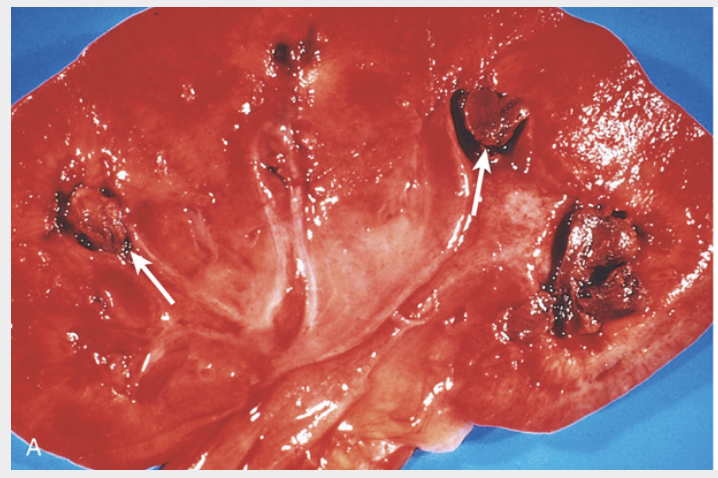
Papillary necrosis. (A) Areas of hemorrhagic necrosis involve the papillae (arrows).
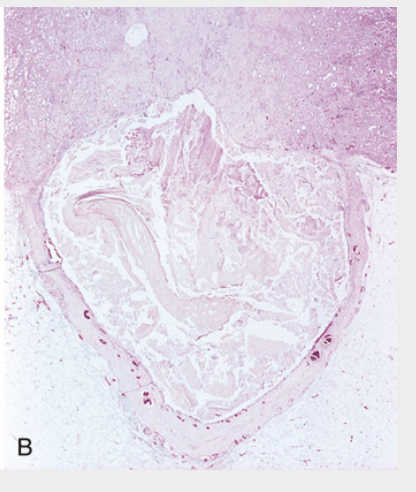
Papillary necrosis. (B) The tissue is necrotic and seen as fragmented debris
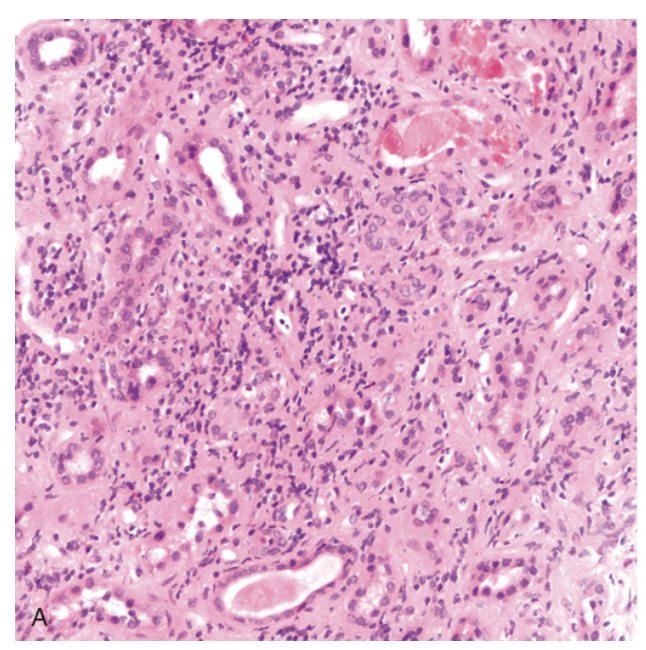
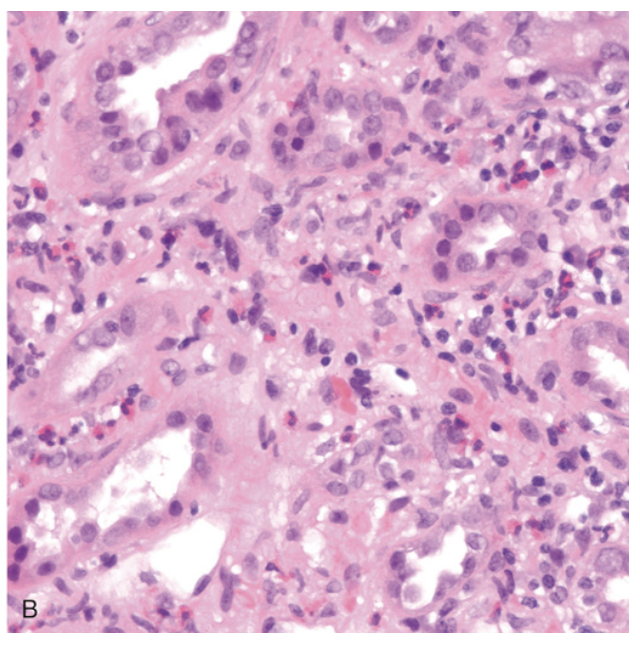
Acute pyelonephritis. (A) The cortical surface shows grayish white areas of inflammation and abscess formation.
Acute pyelonephritis. (B) Neutrophilic exudates within tubules and interstitium.
Chronic pyelonephritis. (A) Shrunken kidney with irregular, coarse scars.
Chronic pyelonephritis. (B) Focus of chronic inflammation with tubular atrophy and interstitial fibrosis (left part of micrograph)
Drug-induced tubulointerstitial nephritis. (A) Chronic inflammatory infiltrate in the interstitium with tubular injury.
Drug-induced tubulointerstitial nephritis. (B) Prominent eosinophilic infiltrate.
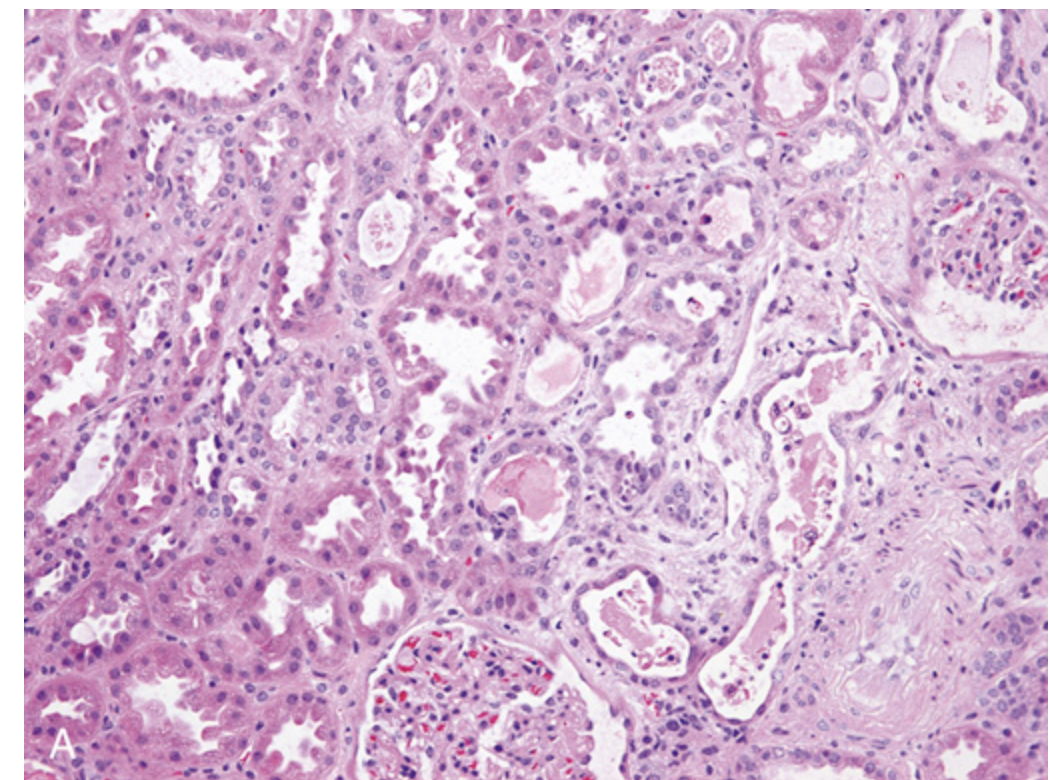
Acute tubular injury. (A) Detachment of tubular epithelial cells from their underlying basement membranes, and granular casts.
Acute tubular injury. (B) Necrotic tubular epithelial cells and cellular debris in tubular lumens. Congestion of peritubular capillaries is prominent
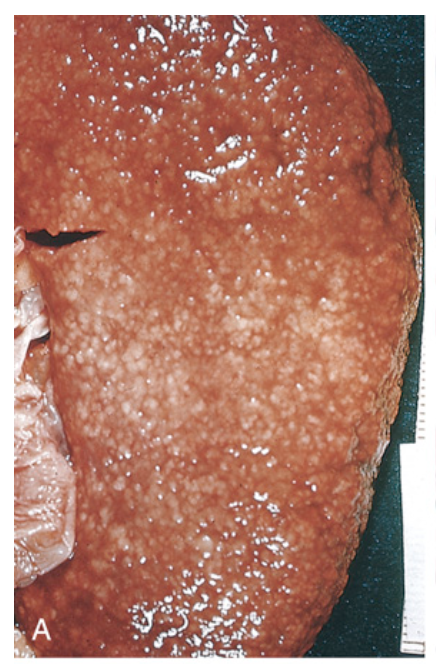
Benign nephrosclerosis. (A) The external surface is finely granular because of scarring.
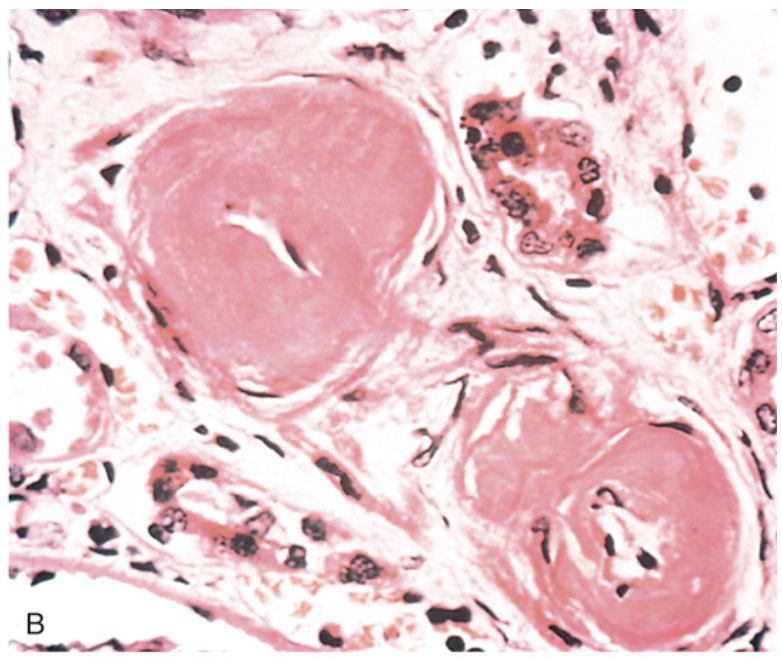
Benign nephrosclerosis. (B) Two arterioles with hyaline deposition, marked thickening of the walls, and a narrowed lumen.
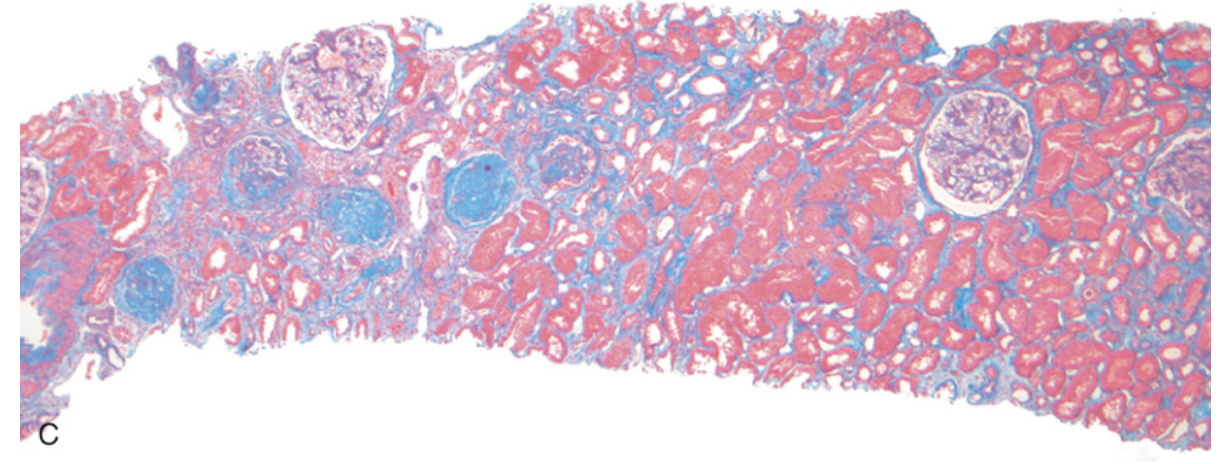
Benign nephrosclerosis. (C) Tubular atrophy resulting from vascular narrowing, and interstitial fibrosis (stained blue).
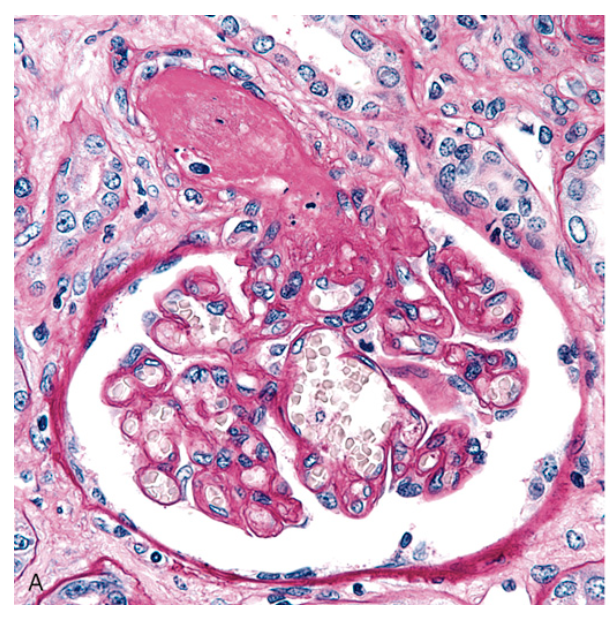
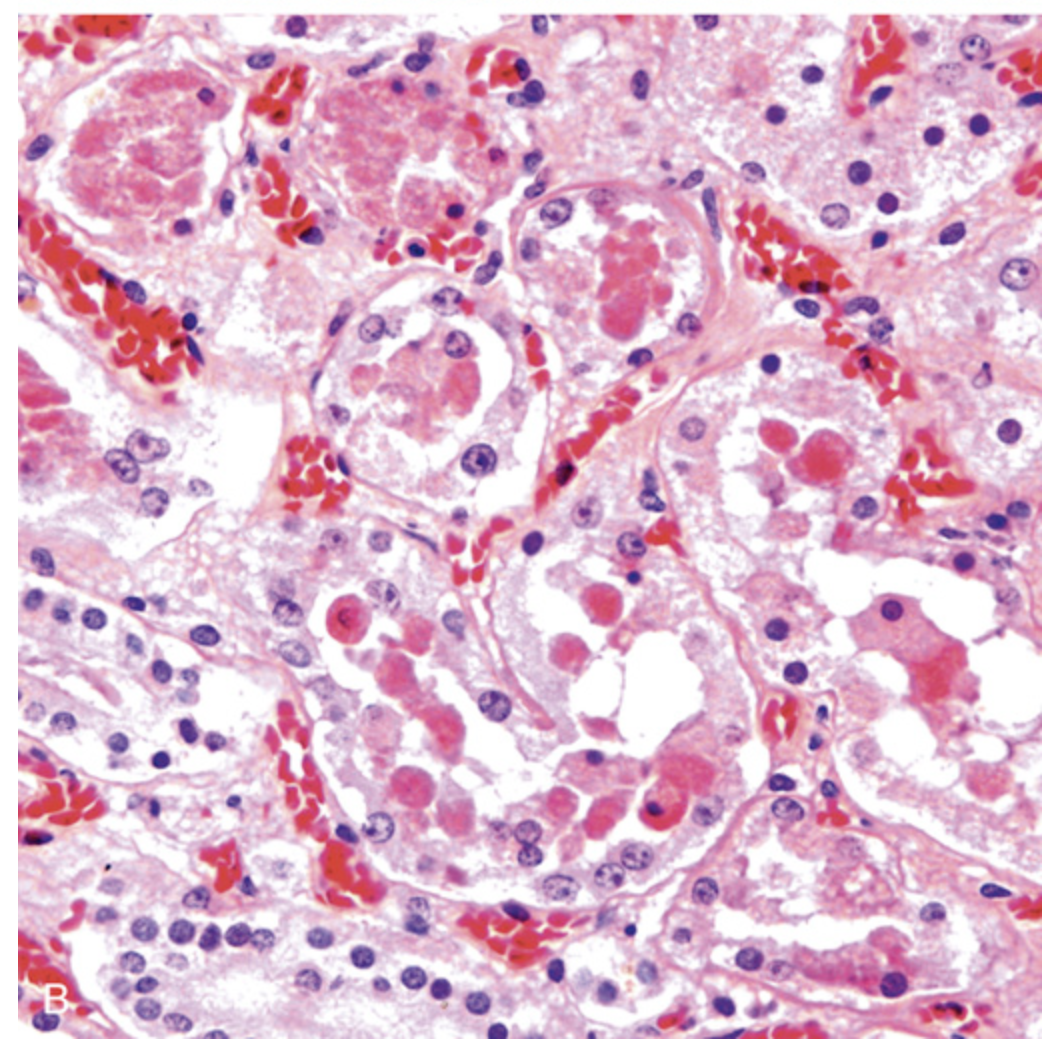
Malignant hypertension. (A) Fibrinoid necrosis of afferent arteriole.
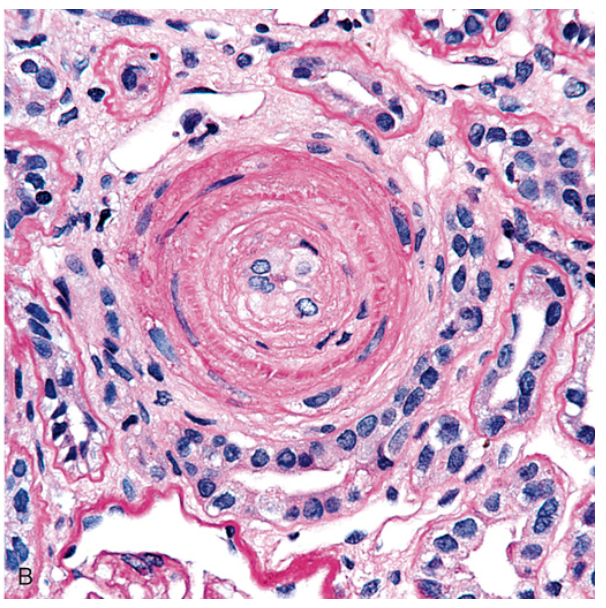
Malignant hypertension. (B) Hyperplastic arteriolosclerosis (onion-skin lesion), typically seen in cases with long-standing hypertension
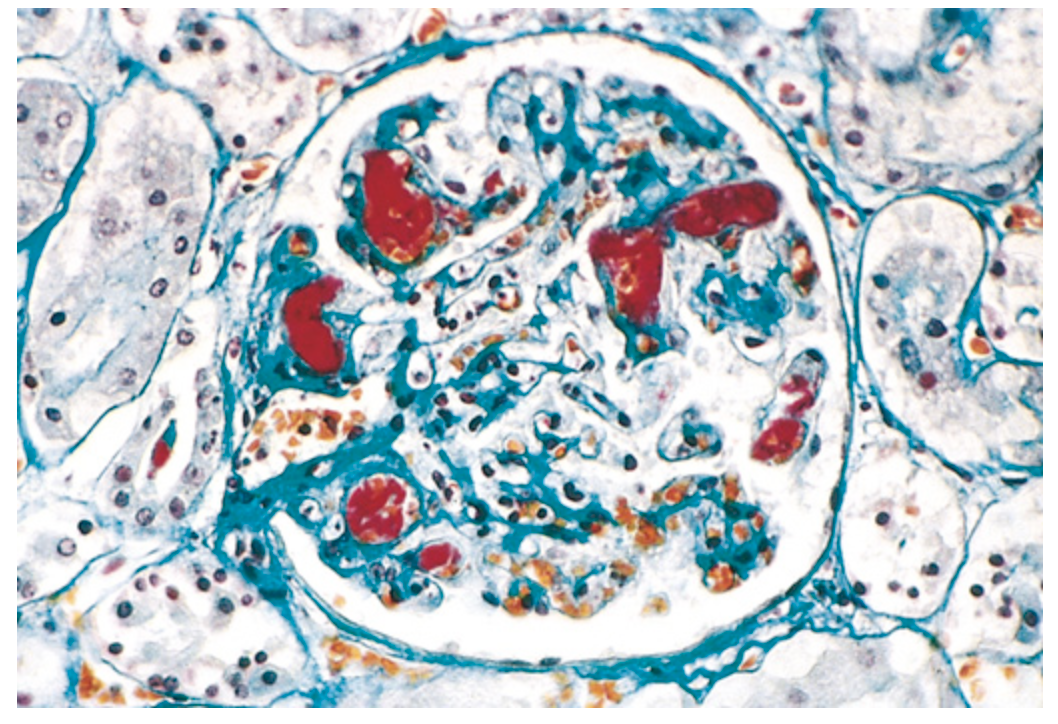
Thrombotic microangiopathy. Fibrin stain showing thrombi (red) in the glomerular capillaries.
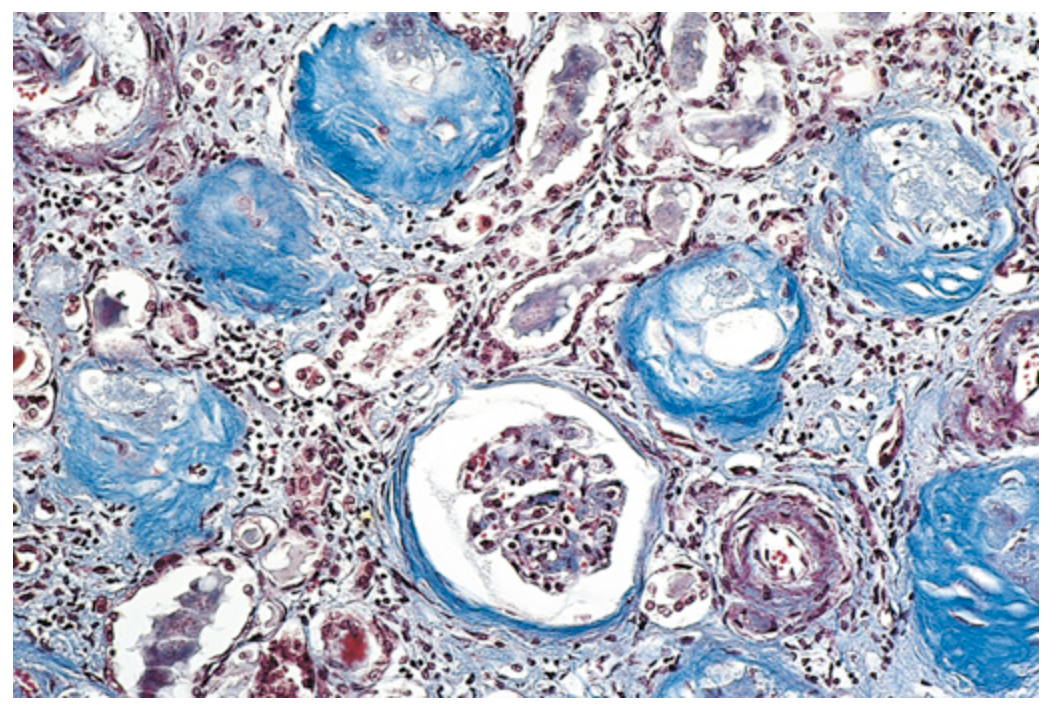
Chronic kidney disease. Replacement of virtually all glomeruli by collagen (stained blue in this trichrome stain), with tubular atrophy and interstitial fibrosis.
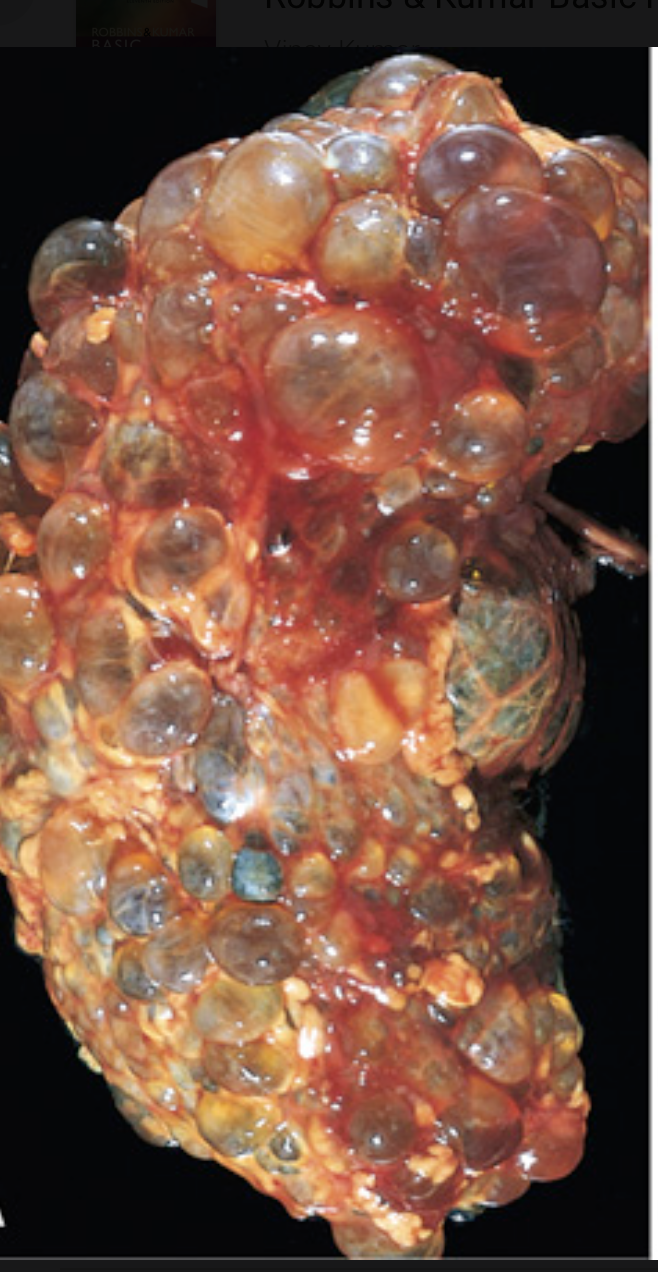
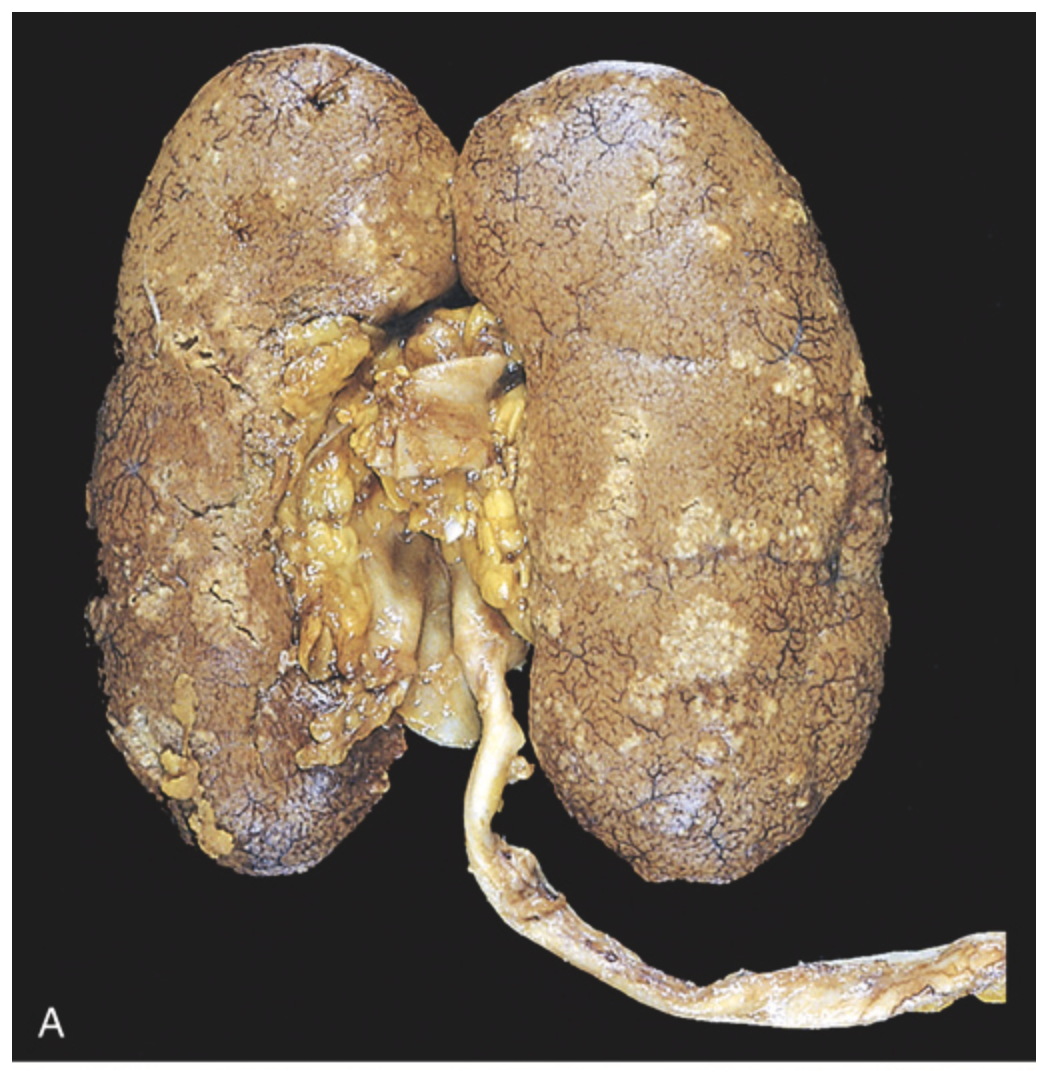
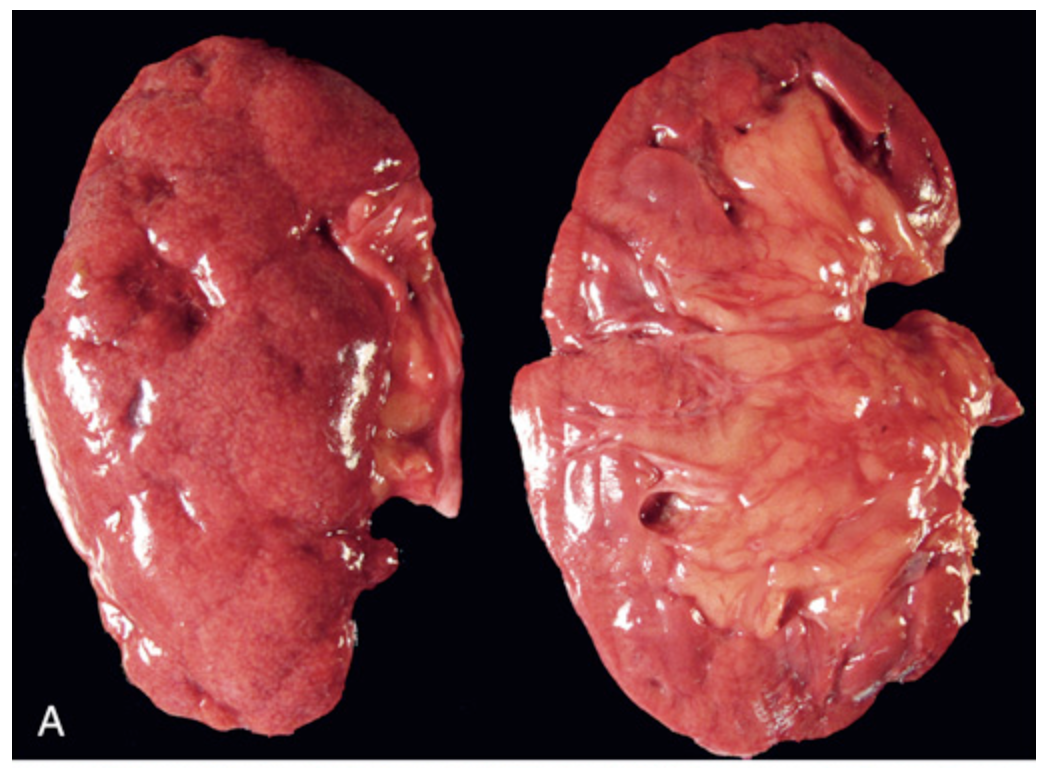
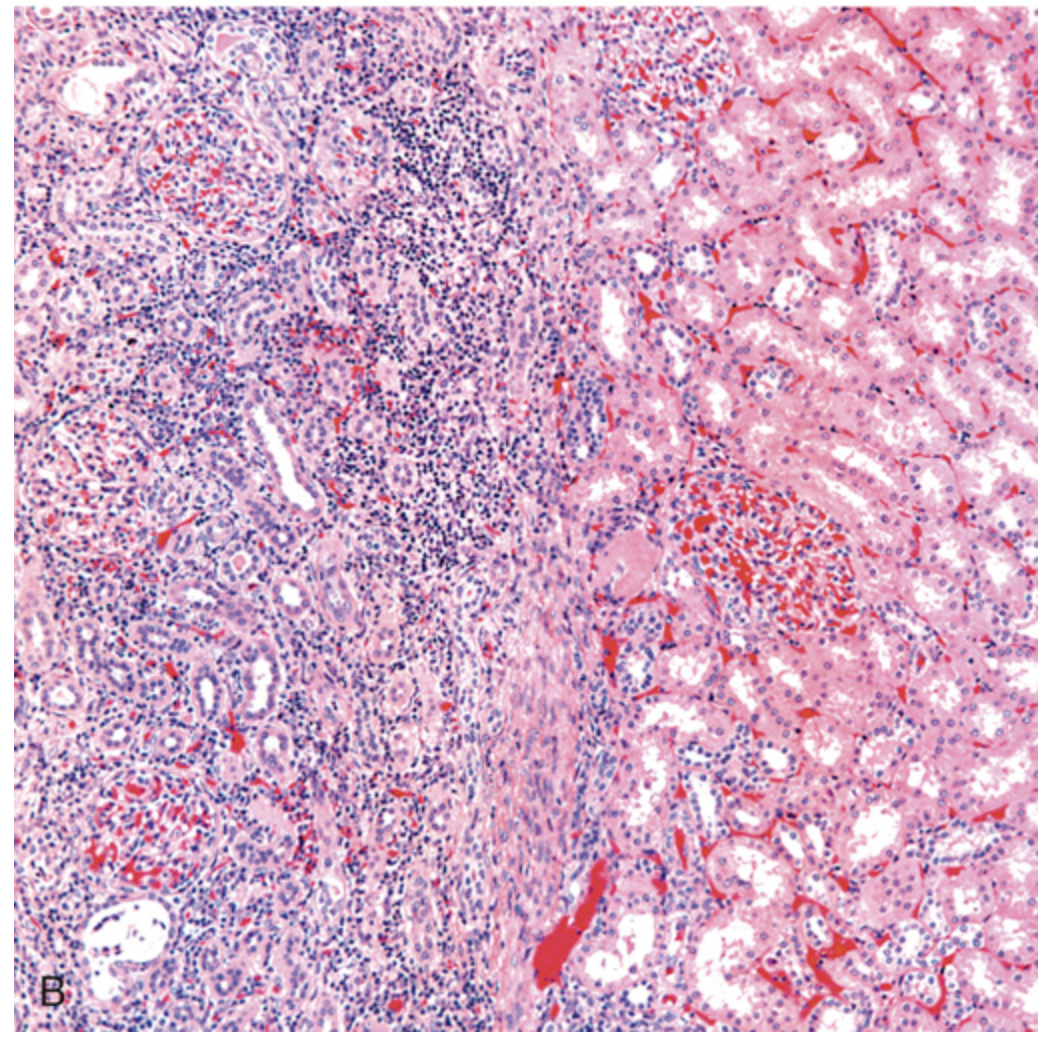
Polycystic kidney disease. (A and B) Autosomal dominant adult polycystic kidney disease (ADPKD) viewed from the external surface and bisected. The kidney is markedly enlarged and contains numerous dilated cysts.

Polycystic kidney disease. (A and B) Autosomal dominant adult polycystic kidney disease (ADPKD) viewed from the external surface and bisected. The kidney is markedly enlarged and contains numerous dilated cysts.
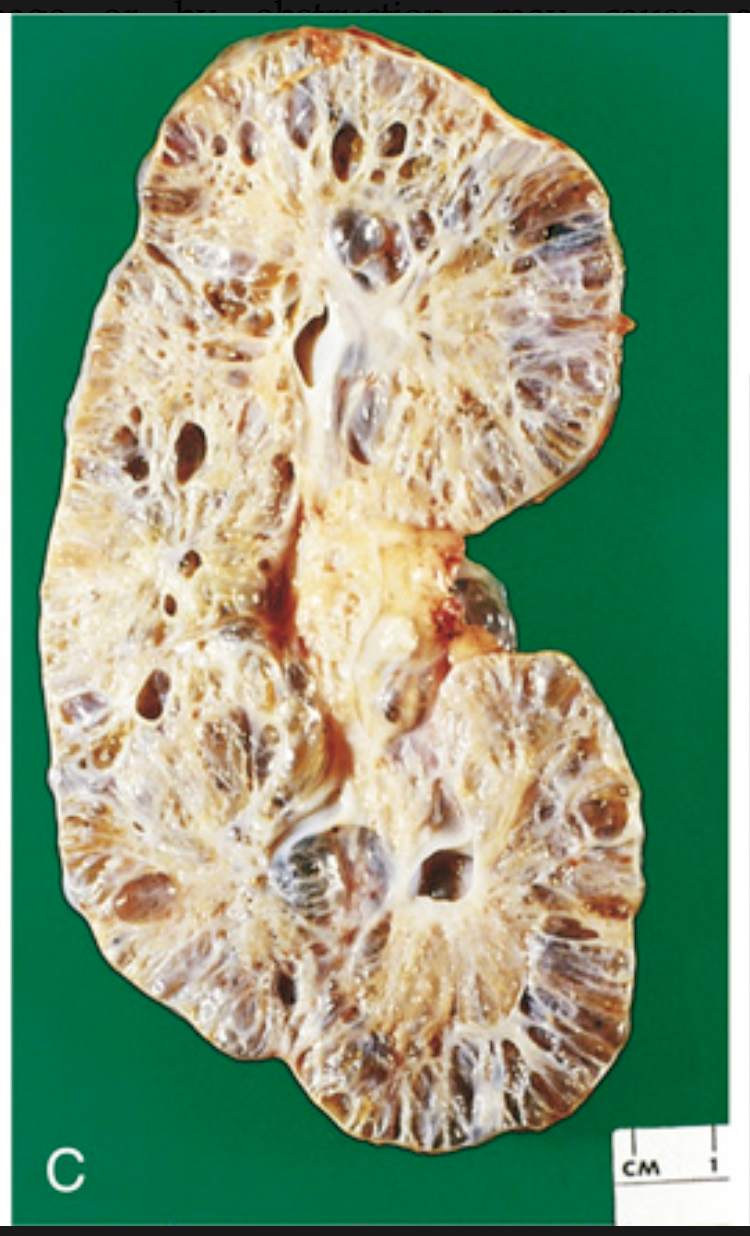
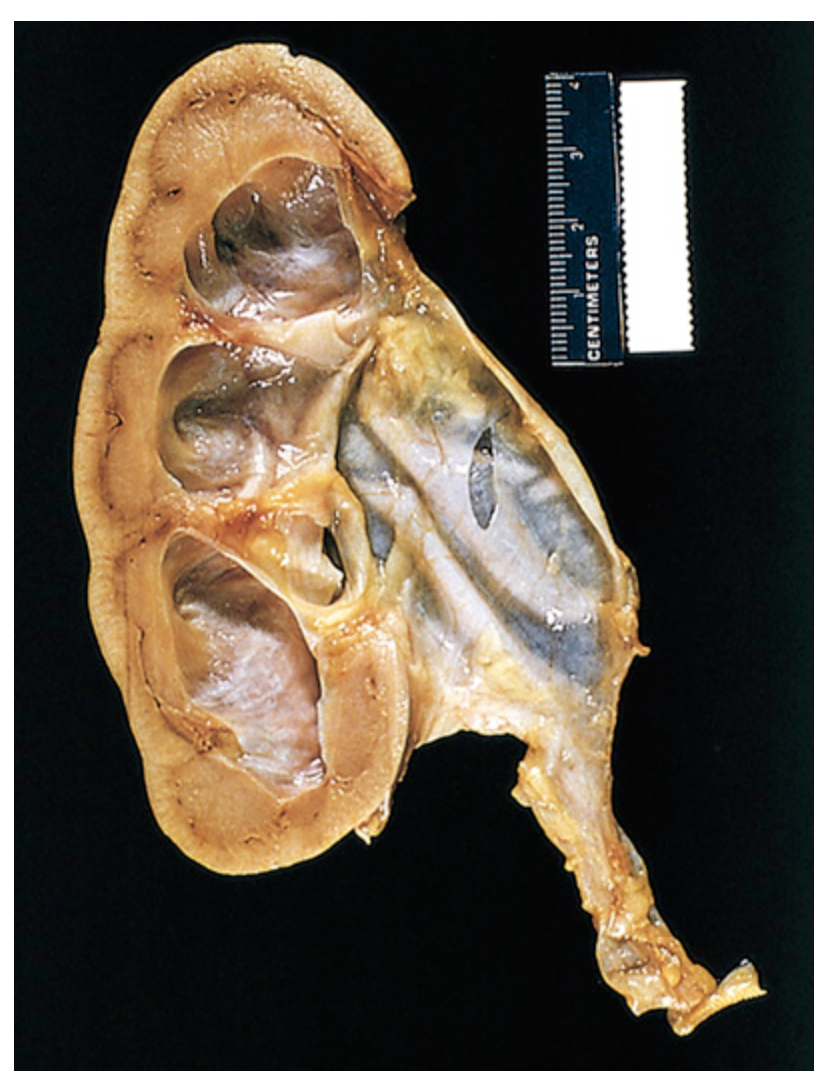
Polycystic kidney disease. (C) Autosomal recessive childhood PKD, showing smaller cysts and dilated channels at right angles to the cortical surface.
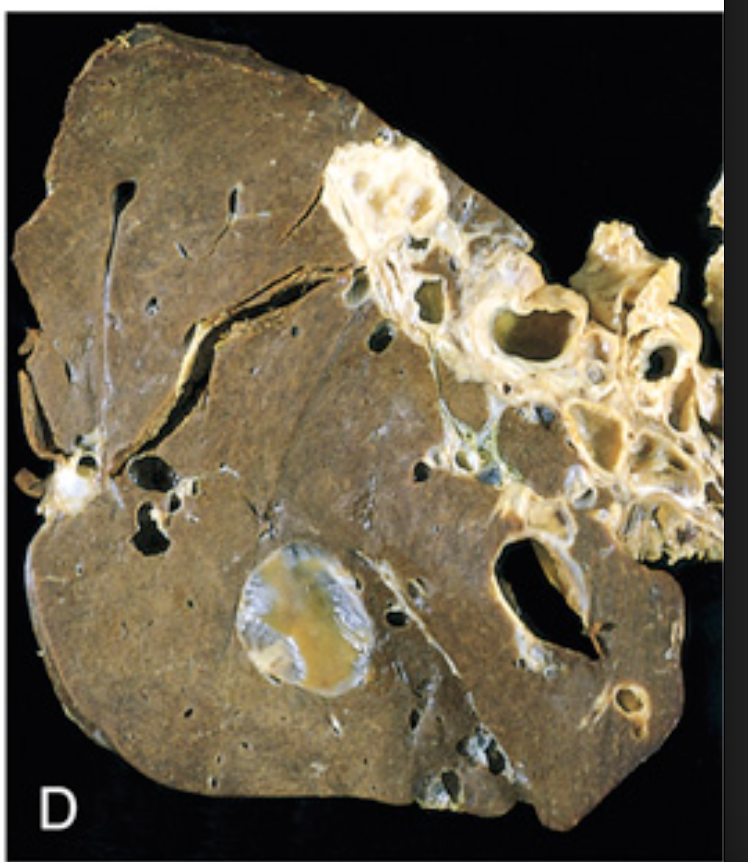
Polycystic kidney disease. (D) Liver cysts associated with PKD.
Nephronophthisis-medullary cystic disease complex. Cut section of kidney showing cysts at the corticomedullary junction and in the medulla.

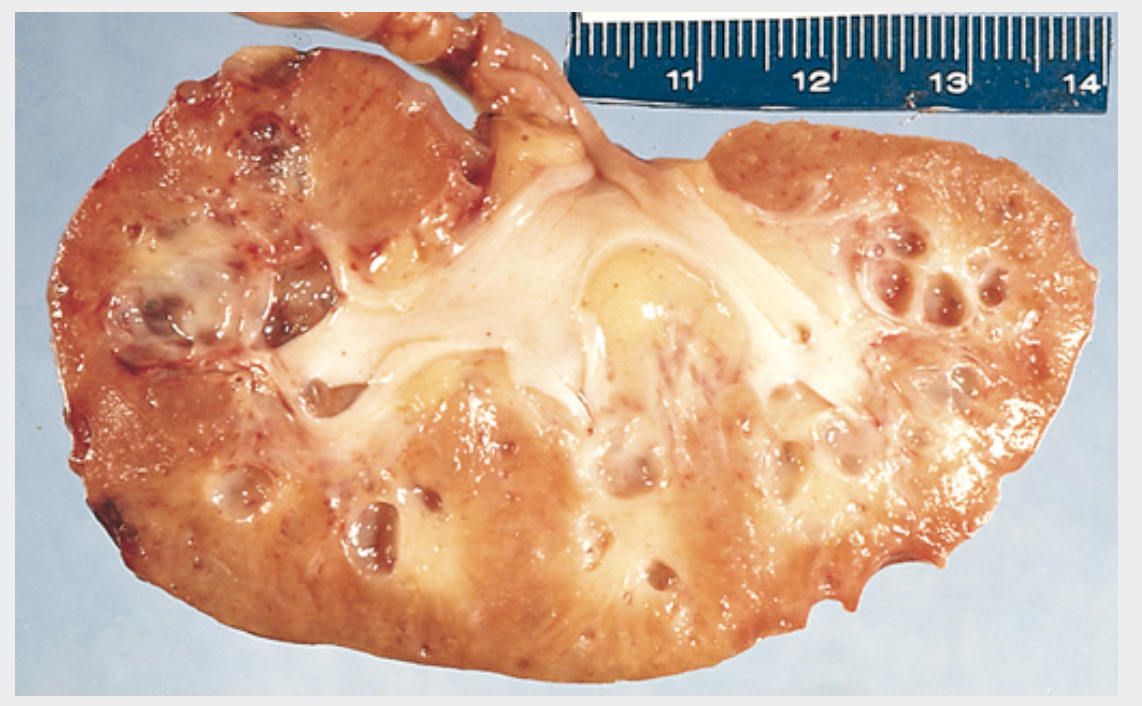
Multicystic renal dysplasia. (A) The kidney is replaced by multiple cysts.
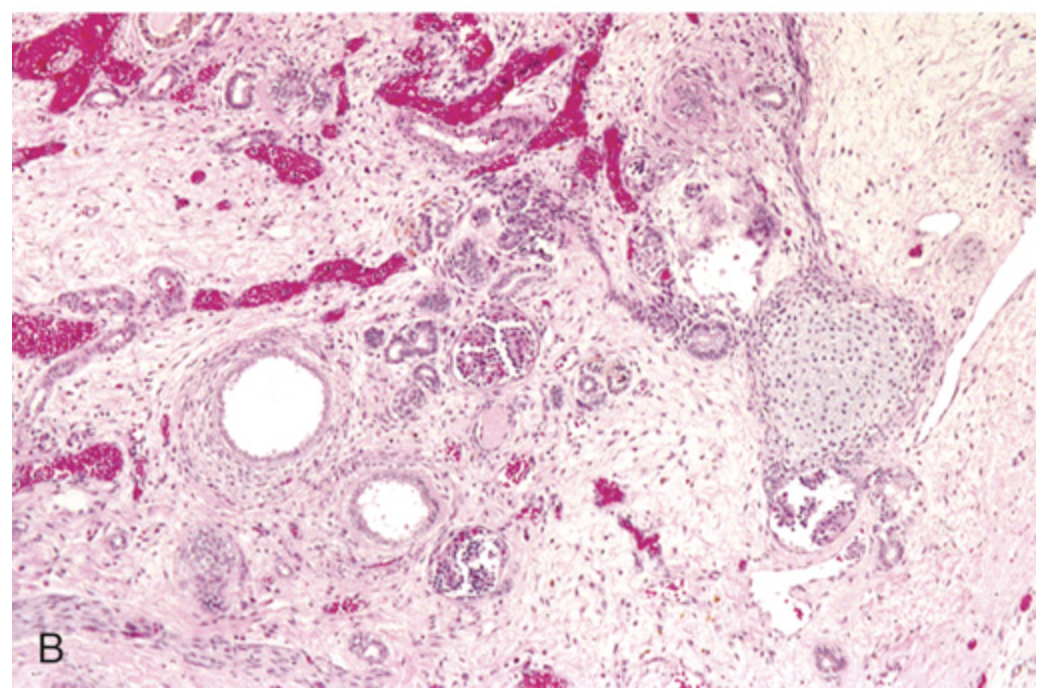
Multicystic renal dysplasia. (B) Disorganized architecture, dilated tubules with cuffs of primitive stroma, and an island of cartilage (hematoxylin and eosin stain).
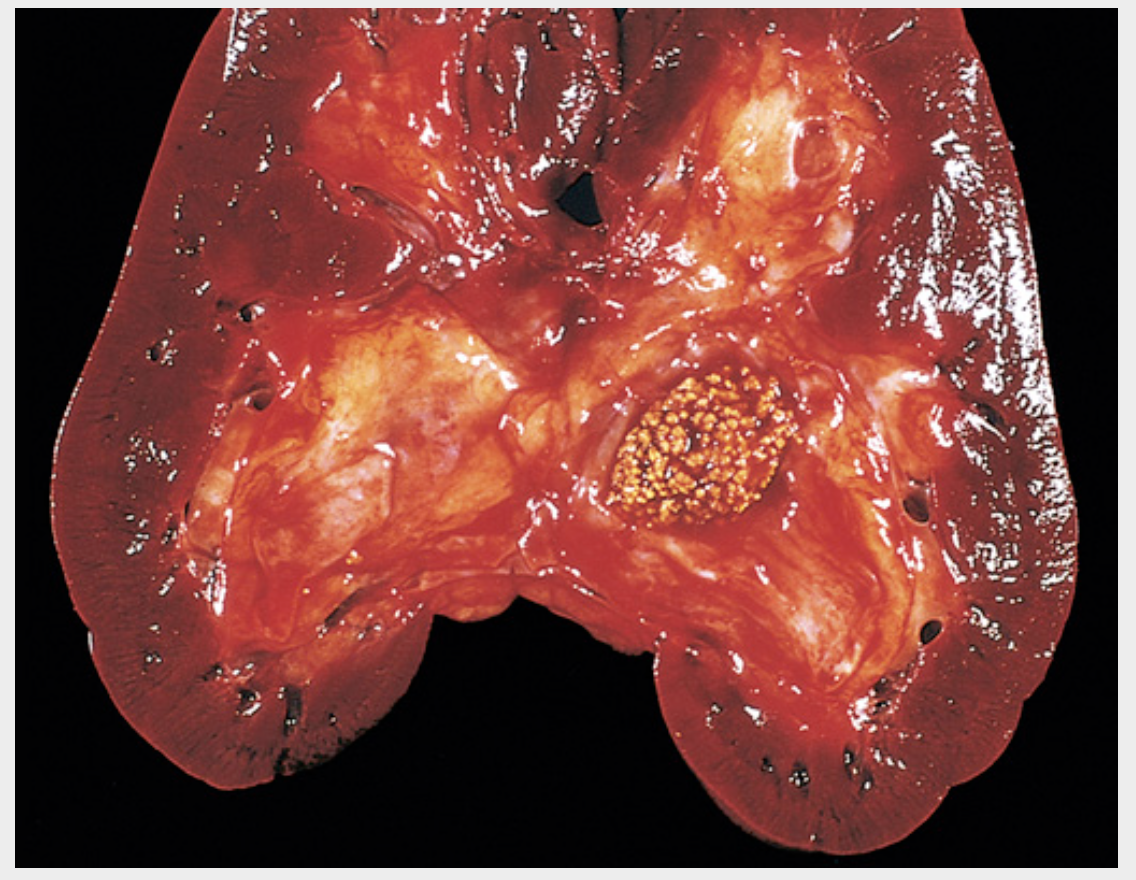
Nephrolithiasis. Stones impacted in the renal pelvis.
Hydronephrosis of the kidney, with marked dilation of the pelvis and calyces and thinning of renal parenchyma
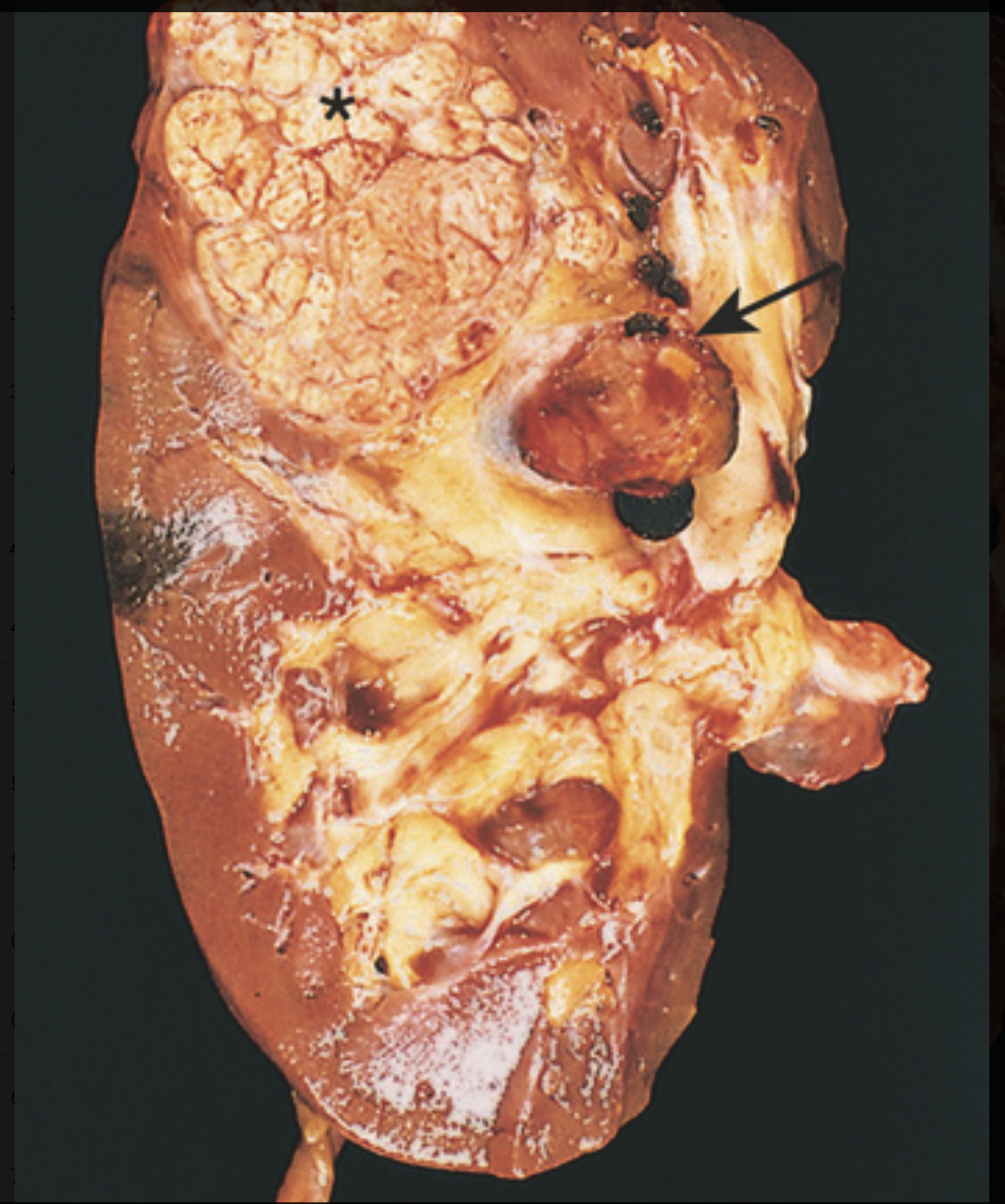
Renal cell carcinoma. Representative cross-section showing yellowish, spherical neoplasm (asterisk) in one pole of the kidney. Note the tumor in the dilated, thrombosed renal vein (arrow)
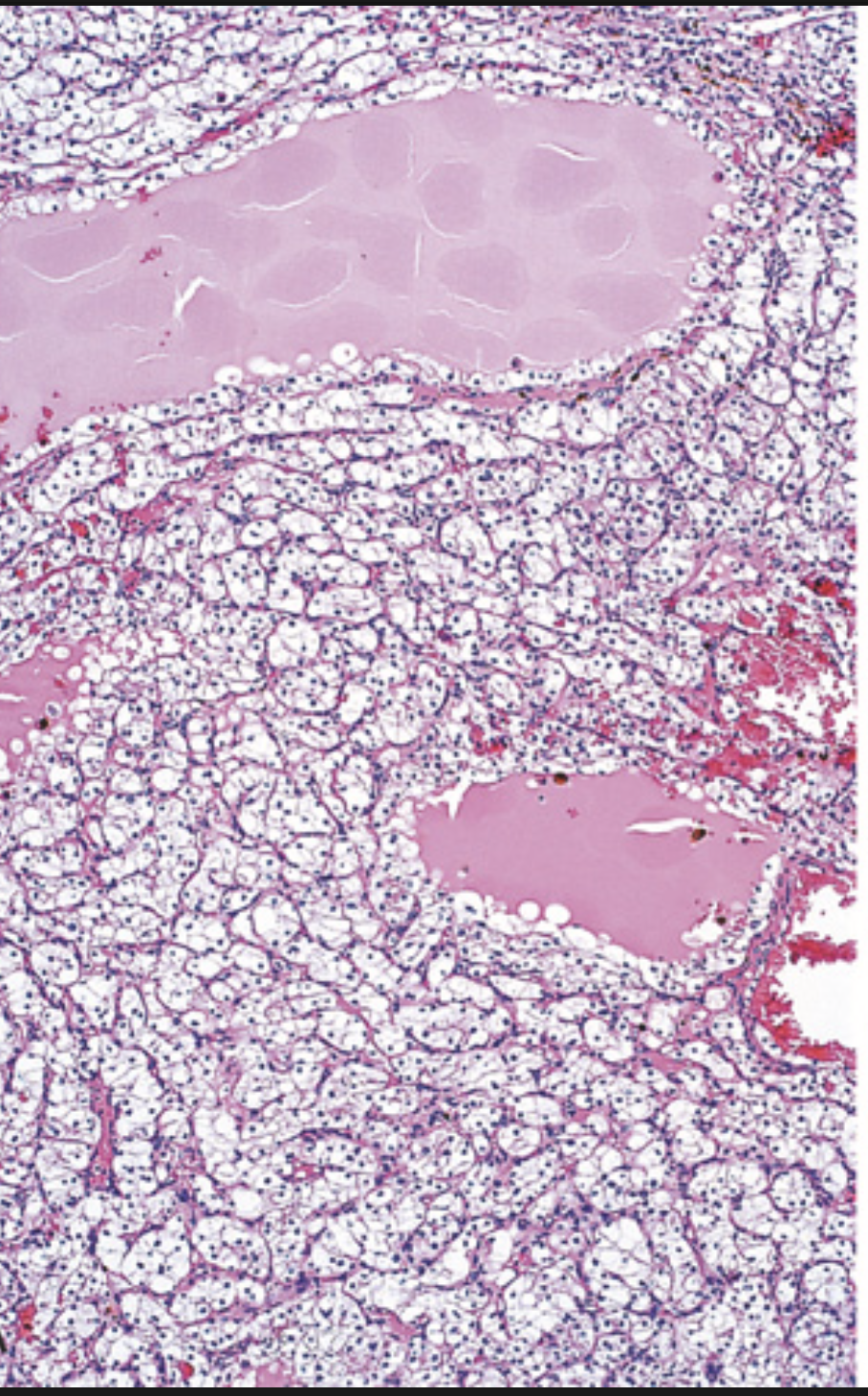
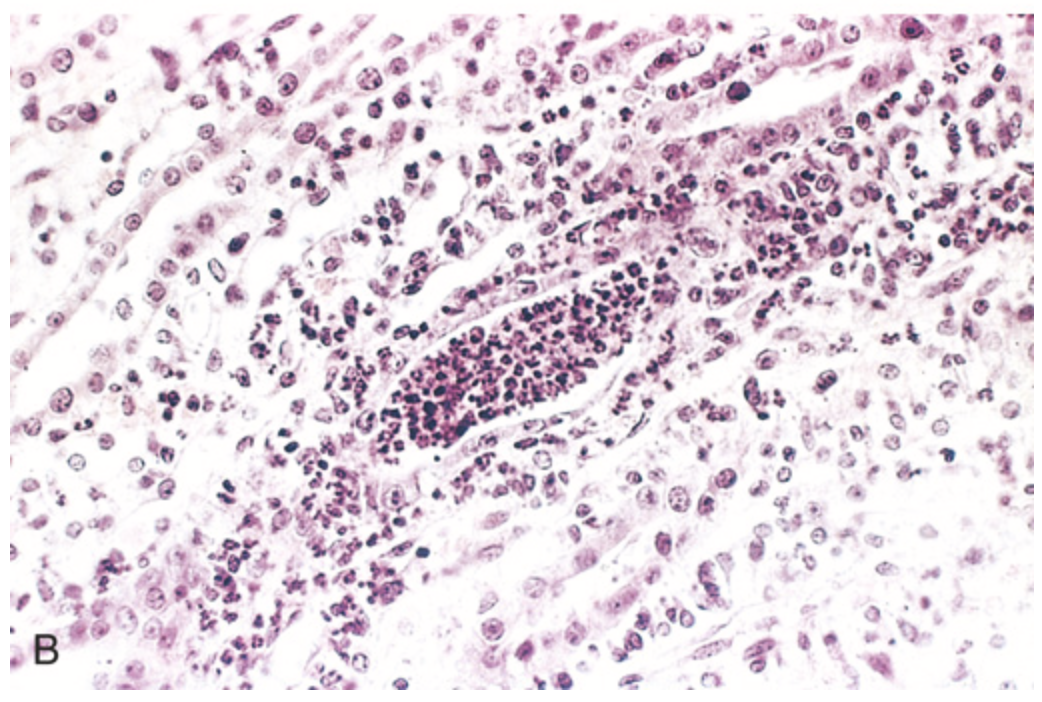
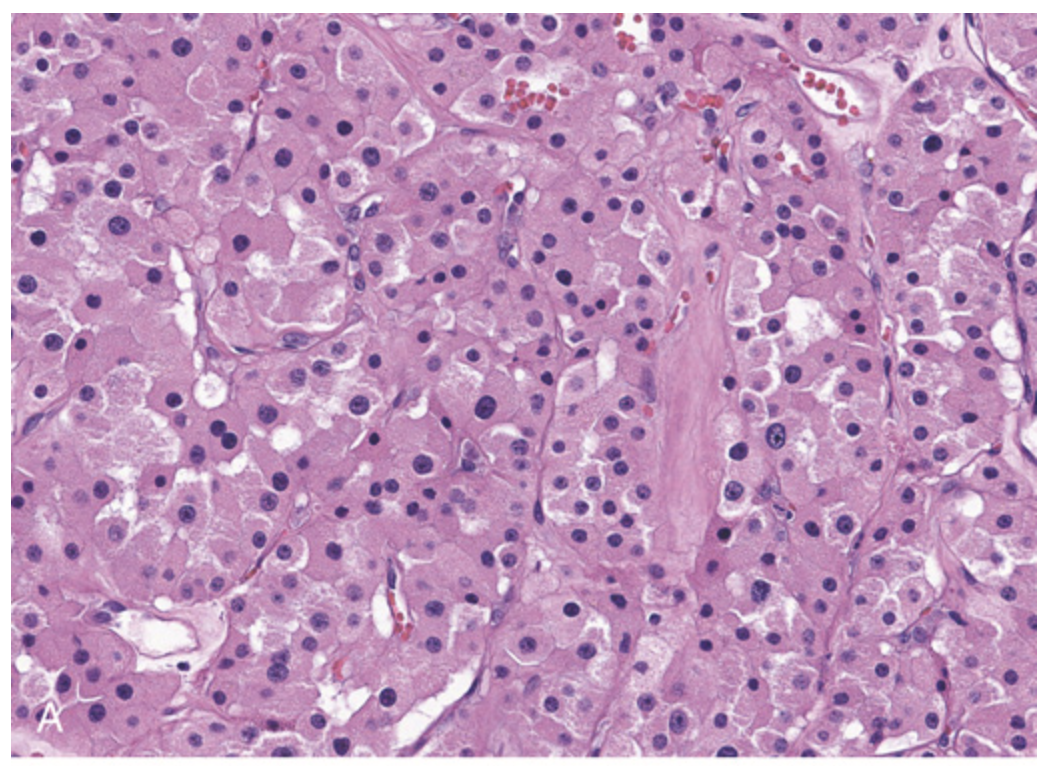
Renal cell carcinoma. (A) Clear cell type.
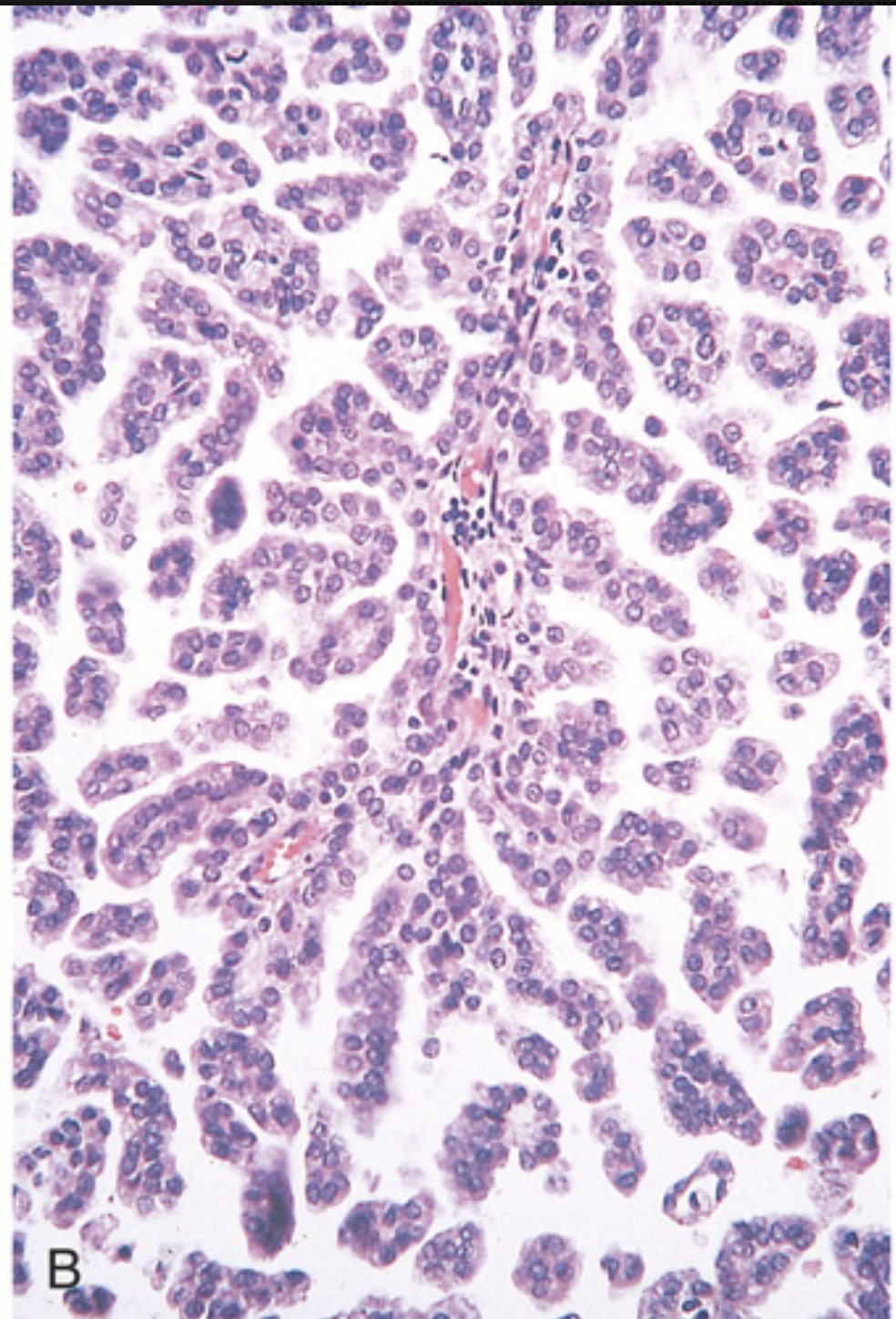
Renal cell carcinoma. (B) Papillary type.
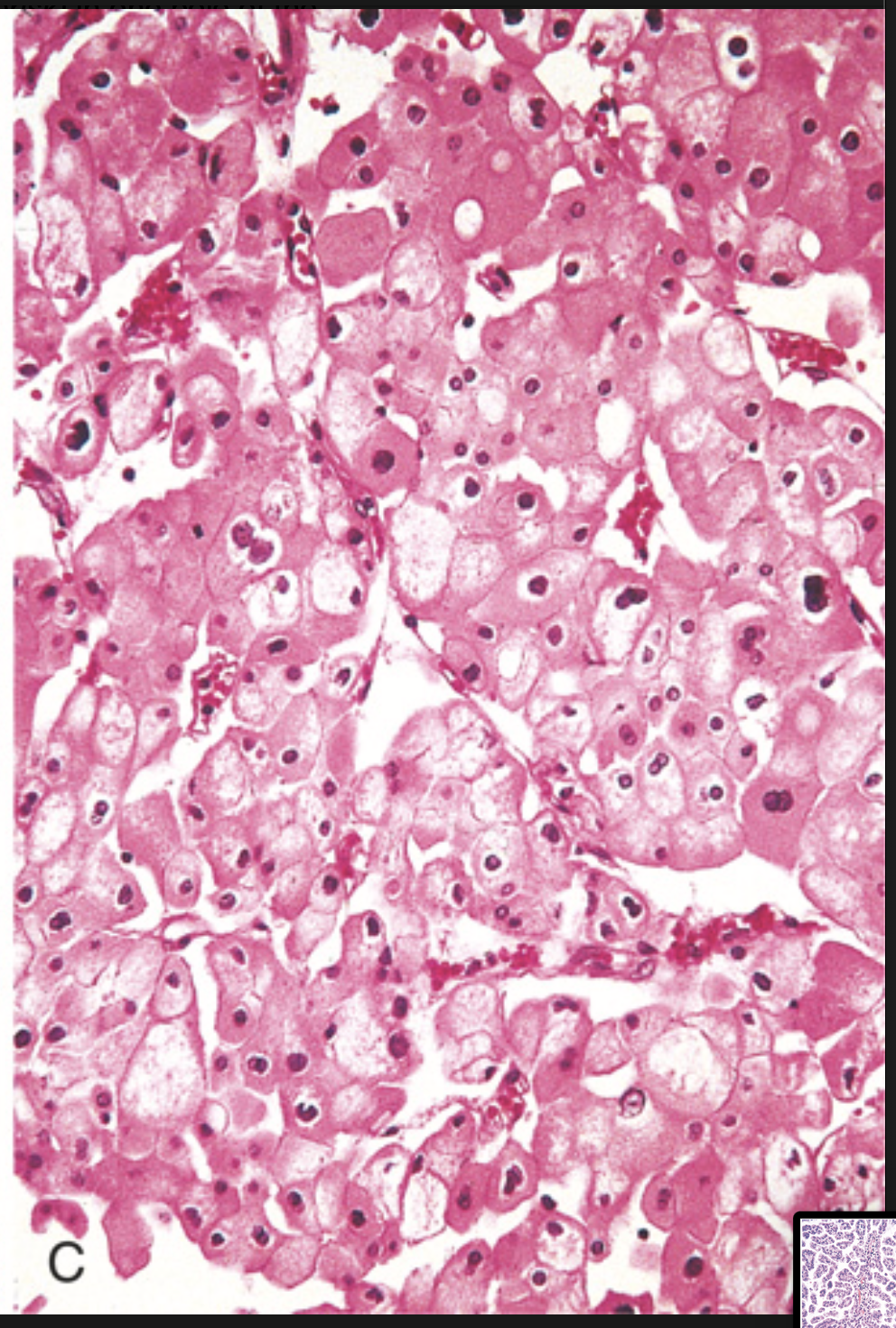
Renal cell carcinoma. (C) Chromophobe type
Renal oncocytoma. (A) Uniform cells with granular eosinophilic cytoplasm.