Unit 1 - MSK Clinical Reasoning
1/124
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
125 Terms
What are the parts of CRAFTE (Clinical Reasoning Assessment for Thinking Effectively)?
patient history
physical examination
assessment
initial interventions
prognosis
education
plan of care
CRAFTE: Section1 (history)
initial hypothesis is based on your review of the patient's chart and intake forms
will list the possible diagnostic hypotheses for the patient's condition
including at least one nonmusculoskeletal condition or red flag hypothesis
therapist-generated body chart
subjective history, or patient interview
ICF
stage of change
stage of healing
symptoms
SINSS model
initial hypotheses should be…
plausible based on the information you have gathered from the patient's medical chart and intake forms
Under each hypothesis, provide evidence from the intake forms that indicates the reasoning as to why the hypothesis should be included
The three initial hypotheses will be labeled as
primary, most likely
secondary, less likely
remote, least likely
subjective exam
one of the most important parts of your examination
80% of the information needed to determine the source of the patient's symptoms can be gathered from the patient's responses during the history-taking process
Some key findings may include
demographics
occupation
role of mechanism of injury
current symptoms
past medical history
medications
prior activity level
self-identified functional impairments
prior treatments
24-hour symptom pattern
notes about current motivation
movement
yellow flags
goals
ICF
a framework to gain a holistic understanding of the patient's health condition in the broader context of their life
primary activity limitation is often the thing the patient most wants to do, or is most limited in doing
Participation restriction is how that activity limitation restricts the patient from engaging in social or environmental contexts
describe how these factors may act as barriers or facilitators to recovery
list at least two barriers and two facilitators
identify how you plan to intervene for any modifiable barriers
Personal factors include age, health and wellness, beliefs, education, occupational, motivational, or psychological factors
Environmental factors may include the patient's living environment, level and type of social support, and level and type of accessibility
stage of change
During the subjective interview, you will learn if the patient is in the precontemplation, contemplation, preparation, action, or maintenance stage
you will identify the body systems primarily involved in the patient's condition, which pain mechanisms are predominant, and any evidence of tissue healing
Signs of tissue healing
inflammatory phase
may include swelling, pain, redness, and/or warmth
proliferation phase
there's pain, redness, and swelling, but they will all begin to decrease
remodeling phase
the tissue will be in the final phase of healing with improved strength and durability
There should be little to no pain and no swelling present in this phase
Symptom sources
may include joint and bony structures under areas of symptoms, muscles and tendons under in the area of symptoms, ligaments, nerves, and other soft tissues under and in the area of the symptoms, neurological or musculoskeletal structures which may
refer to the area of the symptoms, or red flag conditions or visceral structures which may be screened.You may include up to three structures per region
SINSS model
severity
irritability
nature
stage
stability
Severity (SINSS)
the extent of the impact of symptoms on the patient's activity
The highest NPRS is often used to quantify
Irritability (SINSS)
includes the assessment of the time frames and/or intensity of activity which brings on symptoms
Nature (SINSS)
includes a suspected involvement system, pain mechanisms, structures, and psychosocial factors
Stage (SINSS)
can be classified as acute, subacute, or chronic, and may be linked to severity and irritability
Stability (SINSS)
related to the predictability and progression over time of the symptom behavior
How do you use SINSS with CRAFTE?
you will list each problem labeled as P within the form and justify your assessment of each using the SINSS model
You will include a rationale for your decision
CRAFTE: Section 2 (physical exam)
Which of your initial hypotheses were you able to roll down in likelihood from the subjective examination findings, and how?
What evidence can you identify from your interaction with the patient thus far that would support any changes to your hypotheses list?
What do you do after the patient interview but before the physical examination?
generate your revised working hypotheses
You will list a primary hypothesis
A critical factor in your physical assessment?
intensity of your range of motion examination
examination vigor spectrum
Most cautious
highly irritable patients, limit range of motion testing to first onset or change in symptoms, even if you suspect they have more available motion
This minimizes discomfort while still gathering useful information.
Moderately cautious
For example, patients with moderate irritability, you may test active range of motion to its limit even if it reproduces their pain. You might also apply passive overpressure to assess and feel, accepting some symptom reproduction in exchange for deeper clinical insight.
Least cautious
When working with low irritability patients, you can perform sustained, repeated, or combined movements without significant concern for symptom exacerbation
In these cases, you are confident that the vigorous examination will not provoke excessive discomfort
plan for the physical examination
Which symptoms will you try to reproduce, and how?
Do you expect it to be easy or hard to reproduce these symptoms?
What is the anticipated vigor or limit of your range of motion examination?
CRAFTE: Section 3 (assessment)
After your physical examination, you will assess your findings
Using the SINSS principle, do you have to change your assessment, level of irritability, or pain mechanisms?
One of the most important questions you will have to answer is if the patient is appropriate for physical therapy management
Is your clinical management to treat, treat and refer, a nonurgent referral, or an urgent referral?
If you are deciding to refer out, to whom will you refer?
What is the clinical reasoning for this referral? What will you suggest for the referral, such as imaging or lab work?
If deemed appropriate for physical therapy management…
you will list your baseline objective findings
you will choose your primary hypothesis and describe the clinical evidence that supports this choice
You will do the same thing for an alternative hypothesis
CRAFTE: Section 4 (initial interventions)
What do you expect to primarily be treating initially?
Pain and symptom modulation, range of motion, muscle performance, activity performance, or contextual factors?
What evidence indicates that this treatment approach is appropriate for your patient?
You will then list two specific interventions, the expected response for each, and choose a comparable sign to reassess after the treatment
The comparable sign reassessment is crucial to determining if your treatment was effective
At least one intervention should be active in nature
Your home exercise program should include three interventions with listed frequency, intensity, and time.
provide a rationale for your dosage selection.
CRAFTE: Section 5 (prognosis)
You will start by describing any contrast between the individual's prior, current, and desired level of function
You will justify your choice with evidence from the subjective and physical exams
Is there any natural history of the disorder that can guide your prognosis?
List any positive or negative prognostic indicators, likelihood of recurrence, and the rationale.
Overall, how would you rate this patient's prognosis? Is it poor, fair, good, or excellent?
Finally, you will create short and long-term goals using the SMART goals concept and the ICF framework
CRAFTE: Section 6 (education)
What's wrong with me?
most important
How long will it take?
What can you, the therapist, do about it?
And what can I, the patient, do about it?
These questions are designed to give the patient a clear and foundational understanding of their condition and the path forward.
To answer them effectively, you'll need to integrate all the information from the CRAFTE form along with your clinical reasoning skills.
CRAFTE: Section 7 (plan of care)
You will answer how you expect the condition to progress over time considering the patient's impairments, activity limitations, participation restrictions, and tissue healing.
How many visits?
Over what period of time do you expect to see the patient?
you will use the targeted ICF framework to pull all of your clinical decision making together.
You will address the ICF components using specific interventions and describe the dosage for each.
Each ICF component will have an associated goal
CRAFTE body chart symbols
circle
X
slash mark
arrow
check mark
P_
Body chart: circle
dull or aching
Body chart: X
numbness
Body chart: slash
tingling
Body chart: arrow
shooting/radiating
Body chart: check mark
clear, noninvolved
Body chart: P_
each symptom
Using the Body Chart
Can significantly improve your subjective examination by precisely identifying the patient's specific symptoms.
The symptom investigation can include subcategories of:
Symptom location and descriptor of the pain
Onset of symptoms
Behavior or pattern of symptoms over time
Using the Body Chart: Ruling Out
Noting the exact location of symptoms and descriptors of symptoms (e.g. ache, burning, shooting), paresthesia, numbness, and weakness can be extremely valuable.
Note where the patient does not have symptoms with a check mark
Overlap between pain location patterns associated with visceral disorders and common musculoskeletal disorders
Tell me, what brings you in today, and how can I help you?
“Listen to your patient, he is telling you the diagnosis”
Sir William Osler, Physician, 1 of 4 founders of Johns Hopkins Hospital
Start with OPEN-ENDED questions
Clarify with CLOSE-ENDED questions
“Patients spoke, uninterrupted, an average of 12 seconds” (Rhoades, D. et al. 2001)
One of our greatest interventions begins with the first question: LISTEN
Can you show me exactly where your pain is?
Identify through tracing with hand
Pinpoint versus General
Where did it start?
Does it move up or down?
Spreading
Referral Pattern
Are you having this pain right now?
If so, how would you rate this pain, 0 - 10?
Establish BASELINE
First indication of SEVERITY and IRRITABILITY
What does it feel like?
Pain Descriptors
Sharp
Dull
Stiff
Achy
Tight
Numbness or Tingling?
Dermatomal Pattern
Peripheral Entrapment Pattern
Strong indication of Neuropathic Mechanism
Throbbing
Vascular Pattern
Have you noticed anything that aggravates your symptoms?
BEHAVIOR: “Aggs”
The factors that aggravate symptoms
Positional?
Activity-related?
Stress-related?
time to aggravate
How quickly does this exacerbate symptoms?
Immediate
Gradual
Intensity (NPRS)
Rate 0-10 at its Worst
Persistence
How long does it last?
Have you noticed anything that makes your symptoms better?
BEHAVIOR: “Eases”
The factors that provoke or exacerbate symptoms
Positional?
Activity-related?
Stress-related?
Modalities?
Time to Onset: How fast does it go away?
First indication of IRRITABILITY
Immediate
Gradual
Intensity (NPRS)
Rate 0-10 at its Worst
Persistence
How long does it last?
Behavior
Symptom Presentation Characteristics
Constant?
Intermittent?
Consistent?
Variable?
Helps to determine NATURE
Involved system and structures
Pain classification
RED FLAG: Constant + Consistent
Non-mechanical
No easing factors
Refer
Is there anything this symptom is holding you back from doing?
Strongest indicator of SEVERITY
Activity?
ADLs
Work
Hobbies/Sport
Social
Insight into Fear Avoidance Behaviors
Best indication of patient-centered, functional Goal
Have you noticed any patterns in your symptoms based on the time of day?
24-Hour Pattern
Worse in A.M., eases with movement?
Good in A.M., worse as day progresses?
Does this pain wake you up at night?
Can you change positions to ease?
Can you fall back asleep?
If no: potential RED FLAG:
Unrelenting
Wakes up at same time each night
Would you say this pain is getting worse, getting better, or staying the same?
Strongest indication of STABILITY
Is it following a predictable pattern?
Expected rate of healing for tissue injury
Factor in co-morbidities
Predictable Aggs and Eases
Progression or Regression over time
When/How did this start?
Was there a mechanism of injury?
Trauma
Insidious Onset
Gradual/Overloaded
If tissue is injured, consider phases of tissue healing
Coagulation and Inflammatory
Migratory and Proliferative
Remodeling
Have you ever had anything like this before?
History of condition
Previous Injury
Previous Treatment
Have you / Are you participating in any other treatments?
Co-treatment with other health professionals
May affect progression / regression
Insight into beliefs around recovery
Are you taking any medications?
Effects of pain relievers / anti-inflammatories / steroids
Not just for present condition
Screening for compounding / non-conducive medications
Insight into co-morbidities
Insight into compliance
Have you had any imaging?
X-Ray, MRI, CT Scan —> Referral —> Discussing maladaptive beliefs
Review of Systems/Red Screening
Review of Systems: Have you considered all the systems?
1. Cardiovascular
2. Pulmonary
3. Endocrine
4. Eyes, Ears, Nose, or Throat
5. Gastrointestinal
6. Genitourinary/Reproductive
7. Hematologic/Lymphatic
8. Immune
9. Integumentary
10. Musculoskeletal
11. Neurologic
Currently I am experiencing: (please circle all that apply)
Difficulty swallowing
Nausea/vomiting
Shortness of Breath
Pulsing in abdomen
Unexplained Weight Loss
Change in bowel/bladder
Changes in appetite
Increase pain at night/rest
Poor Balance/Falls/Dizziness
Pain with eating
Pain with menstruation
Numbness/Tingling
Headaches
Depression
Vision Changes
Tell me, what do YOU think is causing your symptoms?
Insight into patient beliefs
Opportunity to break down fears, maladaptive beliefs
Opportunity for reassurance
What do YOU think will help it get better?
What is your number one goal?
Functional —> Activity —> Participation
SMART
Motivational
Recap
Review your findings to the patient
Is there anything else that I haven’t asked about or that you would like to tell me?
Open Opportunity for Patient
EXPLAIN: 4 Questions
Hypothesis
1) “What is wrong with me?”
Explanation of Objective Examination
Potential Prognosis
2) “How long will it take?”
3) “What can I do?”
4) “What can YOU do?”
Informed Consen
Subjective exam Conclusion
Allow your patient to tell THEIR story.
INVEST in your patient by LISTENING.
Explore the IMPACT on the patient’s life.
Demonstrate EMPATHY.
EDUCATE.
“Honesty without COMPASSION is Cruelty” - unknown
Screening Tools
“Brief triage instruments”
Used to
Identify patients who may be at risk for poor clinical outcomes
Improve the efficiency and effectiveness of care
Outcome Measures
Used to
assess a patient’s current status and ability
track functional changes over time
Types
Performance-Based
Timed Up and Go (TUG)
Self-Reported
Oswestry Disability Index (ODI)
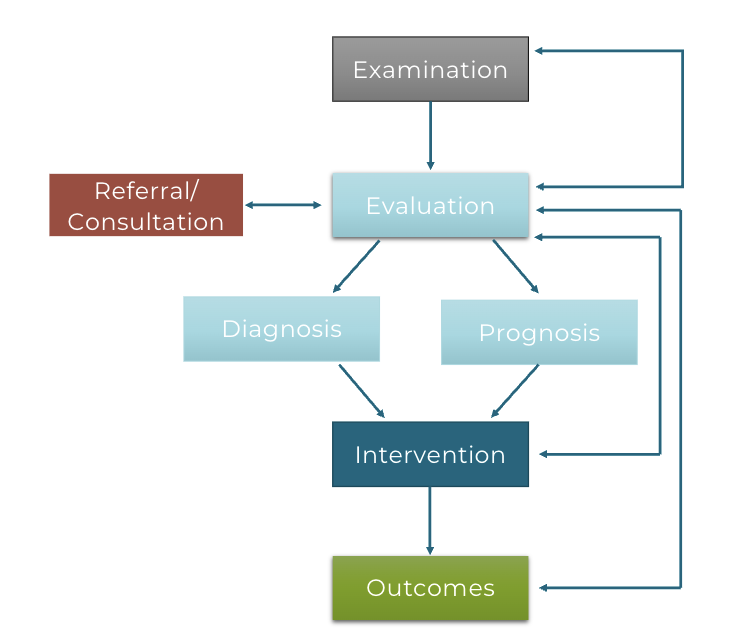
Patient Client Management Model
ICF Examples of Screening Tools/Outcome Measures
Health Condition:
PHQ-2 and PHQ-9
Body Structures/Impairments:
Beighton score
Activity Limitations:
TUG, Dynamic Gait Index, Noyes Hop Testing, NDI
Participation Restrictions:
PSFS, ODI, UEFS, LEFS
Environmental Factors:
Health-Related Social Needs Screening Tool
Personal Factors:
Tampa Scale of Kinesiophobia (TSK)
Which One Do I Choose?
Red and Yellow Flag screening
Differential Diagnosis
Map out the ICF Model for your patient
Which domain(s) do you need to assess?
Review the Psychometric Properties of the Tools/Measures
Validity
Reliability
Population
The SINSS
Characteristics of the patient’s presenting symptoms
Purpose:
Guide clinical decision-making
Reduce clinical reasoning errors

How to use SINSS?
Develop Hypotheses
Plan for Objective Examination
Vigor
Volume
Precautions
Plan for appropriate Intervention
Selection
Dosage
Application of SINSS
“The construct of SINSS appears in several textbooks and peer-reviewed articles. However, it has been inconsistently defined and applied in clinical practice”
Guidelines of SINSS
Must be assessed for each individual symptom
P1 - right sided neck pain
P2 - pain medial to the right scapula
P3 - pain over the right lateral elbow
Continually reassessed
SINSS: Severity
“The clinician's assessment of the intensity of the patient's symptoms as they relate to functional activities."
How the patient’s symptoms affect their activities of daily living (ADLs)
ICF
Activity Limitation
Participation Restriction
SINSS: Severity —> pain
The intensity of the patient’s pain
Numeric pain rating scale (0-10)
Rating:
Low
Mod
High
Also consider:
Medications used to control pain
Presence or absence of night pain
Impact of symptoms on sleep
Pain and activity do not always correlate
SINSS: Severity —> impact
Impact of pain on function
Patient-specific Functional Scale
a self-report outcome measure of function (0-10)
Identify ≥5 important activities and rate them
Total Score = sum of activity scores/number of activities
MDC = 2-point change
Identify 1 activity
MDC = 3-point change
SINSS: Severity —> rating: low
0-3/10 NPRS with 8-10/10 PSFS
No limitation to ADL's, work or recreational activities
Indications:
Verbal & nonverbal cues indicate minimal to no pain
Descriptors indicate intermittent low-grade symptoms
Not taking pain relieving medications
No impact on sleep
SINSS: Severity —> rating: moderate
4-7/10 NPRS with 4-7/10 PSFS
Moderate limitation to regular ADL's, work, or recreational activities & avoidance of more demanding requirements
Indications:
Verbal & nonverbal cues indicate the presence of moderate pain
Descriptors indicate constant but variable moderate intensity symptoms
Intermittent mild pain-relieving medications may be required to function & sleep
Sleep disturbance possible
SINSS: Severity —> rating: high
8-10/10 NPRS with 0-3/10 PSFS
Maximal limitation to regular ADL's and may be avoiding work or recreational activities
Indications:
Verbal & nonverbal cues indicate the presence of intense pain
Descriptors indicate constant high intensity symptoms
Frequent pain-relieving medications may be required to function & sleep
Sleep disturbance likely
SINSS: Irritability
The behavior of the symptoms.
Considerations
1. Amount and type of activity to aggravate symptoms
2. Amount and type of activity to ease symptoms
3. Ratio of the magnitude of aggravating factors to easing factors
SINSS: Irritability —> Ask yourself
“How easy will it be to reproduce the patient’s symptoms?”
“How likely is it that I will exacerbate those symptoms?”
“How long will it take and to what extent can the patient alleviate those symptoms?”
Implications:
Plan for the physical examination
Plan for Interventions
SINSS: Irritability —> Criteria To Assess
Aggravating Factors ("Aggs")
Intensity of the activity to agg
Sitting vs. walking vs. running
Time to onset or exacerbation
Intensity at onset – NPRS
Intensity at worst – NPRS
Easing Factors ("Eases")
Activity or reduction of activity to ease
Walking to sitting vs. running to lying down
Time to Ease
Intensity at best – NPRS
Constant vs. Intermittent?
Consistent vs. Variable?
SINSS: Irritability —> Symptom Characteristics
Constant vs. Intermittent?
Consistent vs. Variable?
Constant + Consistent
SINSS: Irritability —> rating: low
High intensity activity to agg
running
Minor reduction in activity to ease
walking
Greater time to agg and less time to ease
30 minutes to 2/10, 60 minutes to 6/10 // 10 minutes to 0/10
SINSS: Irritability —> rating: moderate
Moderate intensity activity to agg
walking
Moderate reduction in activity to ease
sitting
Similar time to agg and ease
60 minutes to 6/10 // 60 minutes to 0/10
SINSS: Irritability —> rating: high
Low intensity activity to agg
standing
Significant reduction in activity to ease
lying down
Less time to agg and greater time to ease
5 minutes 6/10 // 60 minutes to 0/10
SINSS: Nature
"Broad, conceptual term
Includes
the specific diagnosis or condition
the nature of the patients themselves
the nature of the pain itself."
Each clinical presentation is unique
All factors that should be considered as you are planning the physical exam
SINSS: Nature —> clinician’s assessment
Hypotheses
involved systems
involved structures (if appropriate)
syndrome/classification
Dominant mechanism of pain
e.g., nociceptive, neuropathic, nociplastic
Psychological and social factors
Precautions
What is Referred Pain?
Pain that is perceived at a site adjacent to or at a distance from the site of origin or stimulation
Multifactorial etiology
Common structures that refer pain
Viscera
Muscle
Intervertebral disc
Joint
Trigger points
Types of Referred Pain
visceral
somatic
neurological
Visceral pain
Pain referred from any visceral organ or peritoneum
Somatic pain
Pain referred from any innervated musculoskeletal structure of the body
Neurological pain
Pain referred from any neurological structure of the body
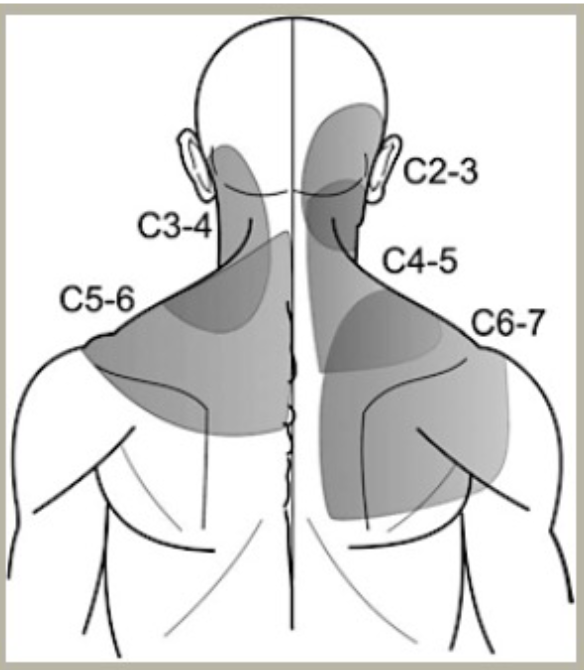
Cervicothoracic Referred Pain
Facet joints
Most commonly symptomatic (Bogduk, 2007)
C2-3
C5-6
Cervical disc
Muscle
Cervicothoracic Referred Pain: C1-2 and C2-3
suboccipital region
Cervicothoracic Referred Pain: C3-4
posterolateral neck, levator scapulae
Cervicothoracic Referred Pain: C4-5
angle between the neck and shoulder girdle
Cervicothoracic Referred Pain: C5-6 and C6-7
lower neck and periscapular region, most commonly the medial scapular borders
Cervical Facet Joint Pain Patterns
Cervical Facet Joint Pain Patterns: C1-2
Suboccipital region, can extend to occiput and vertex of head or into neck
Upper forehead, ear, and orbit
Cervical Facet Joint Pain Patterns: C2-3
Within a band from the occiput to the vertex
Lateral occiput toward the mastoid region and above
Occiput to parietal and upper temporal regions
Cervical Facet Joint Pain Patterns: C3-4
Anywhere over the suboccipital and occipital regions, or cranially in the vertex or forehead
Pain exclusively from this level is rare
Cervical Facet Joint Pain Patterns: C5-6
Focal symptoms, centered over the lower posterior quadrant of the neck
Can spread to proximal region of the shoulder girdle up to the occipital region
No pain reported in the head
Cervical Facet Joint Pain Patterns: C6-7
Centered over the junction of the base of the neck and top of the shoulder girdle to suboccipital region and lateral to the shoulder girdle and arm
No pain in head
Cervical Facet Joint Pain Patterns: C7-8
Junction of the neck and shoulder girdle
Spreads inferiorly and medially into or around the scapular region
Does not spread into the lateral arm or head
Craniofacial and Cervical Muscular Referral Patterns: Temporalis
Cheek area
TMJ
Maxillary Teeth
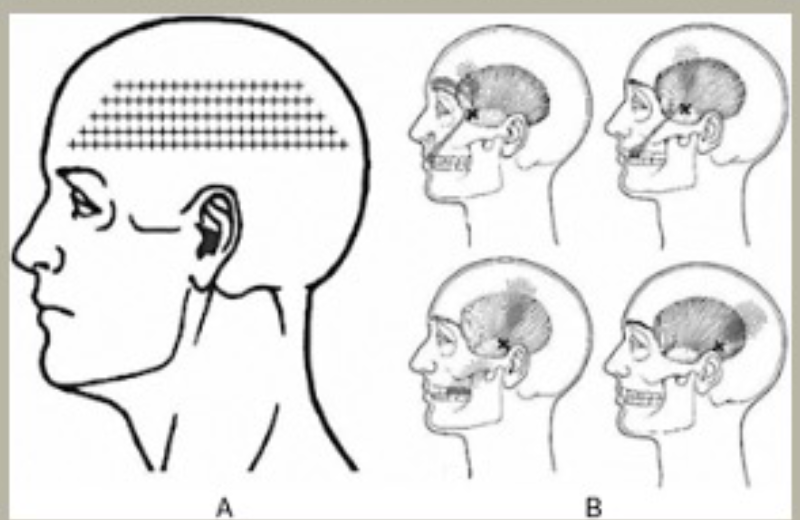
Craniofacial and Cervical Muscular Referral Patterns: Masseter
Mandibular
Teeth
Maxillary Teeth
Ear
Cheek Area
TMJ
Temple