Gas Laws 2
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
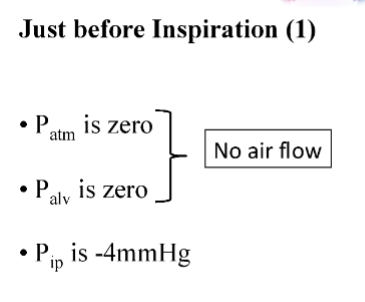
Pressure in the pleural space is always ________
negative
Intrapleural pressure (explanation & in mmHg)
Pressure in the resp system at rest
-4 mmHg
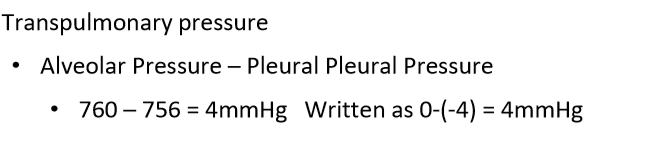
Transpulmonary pressure (explanation & calculation)
Difference between pressure on inside & outside of pleura
Pressure needed to keep lungs from collapsing (opposes the inward elastic recoil of the lung)
0mmHg - (-4mmHg) = 4mmHg
Alveolar pressure (same as atmospheric pressure) - (intra)pleural pressure = Transpulmonary pressure
760 - 756 = 4mmHg
FRC
functional residual capacity

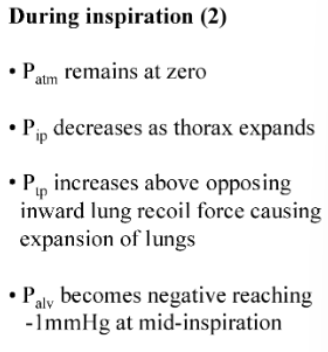
What is happening at point 2
Air is moving into the lung - pressure begins to equalise
Tidal volume of lungs (explanation & mL)
Air that flows into the lungs during quiet breathing
About 500mL
What happens to intrapleural pressure & trans-pulmonary pressure during inspiration
Intrapleural becomes more negative (-7mmHg)
Trans-pulmonary pressure becomes more positive
What happens to intrapleural pressure & trans-pulmonary pressure during expiration
The intra-pleural Pressure Increases
The trans-pulmonary Pressure Decreases
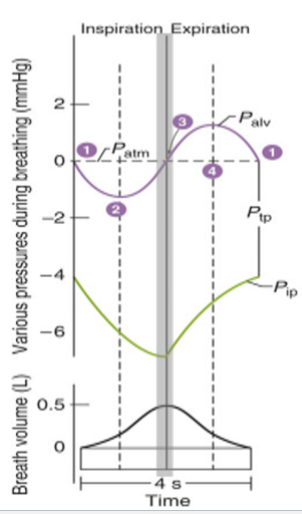
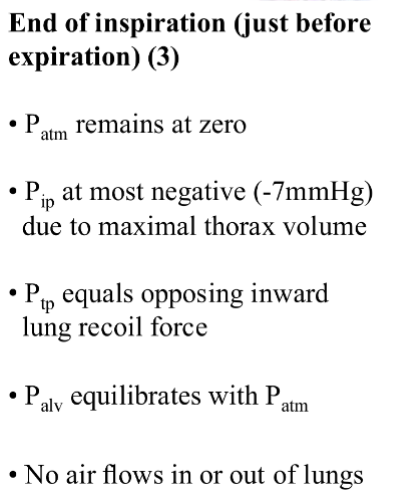
What happens at 3

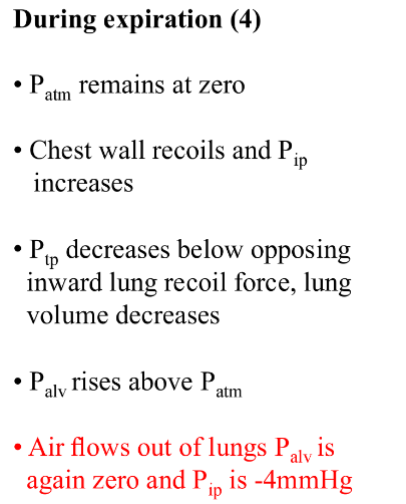
What happens at 4
Where is pressure inside the lung the most negative
The top of the lung
What is the transpulmonary pressure at the top, middle & bottom of the lung
Top: -10mmHg
Middle: -5mmHg
Bottom: -2.5 mmHg
Minute Ventilation (VE) (explanation & formula)
Total ventilation per minute
Tidal Volume (Vt) x Respiratory Rate (f) per minute = Minute ventilation (VE)
500ml (Vt) x 12/min (f) = 6000ml/min (VE)
Alveolar ventilation
Portion of minute ventilation (VE) that reaches the alveoli
More important than VE for gas exchange
Anatomic dead space
Air that enters the resp system but doesn’t reach the alveoli
It ventilates the conducting airways and isn’t available for gas exchange
VD
Dead space volume
Flow (F) formula
Flow (F) is _________ to pressure difference between 2 points & ______________ to the resistance
proportional
inversely proportional
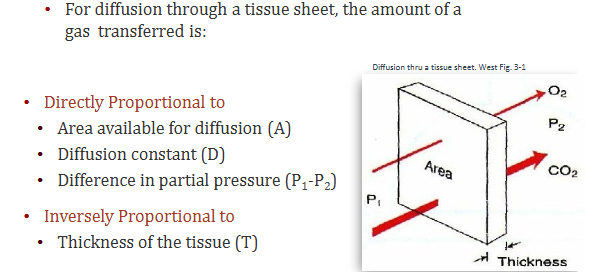
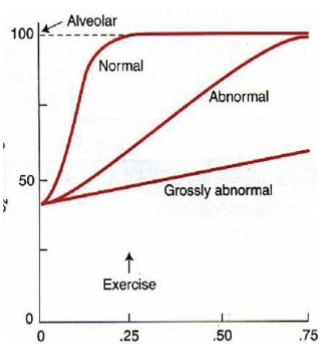
Diffusion of gases across the alveolar membrane is influenced by what?
Laws of Diffusion
Diffusion and perfusion limitations
O2 uptake along the pulmonary capillary
Measurement of diffusing capacity
Interpretation of diffusing capacity for CO2
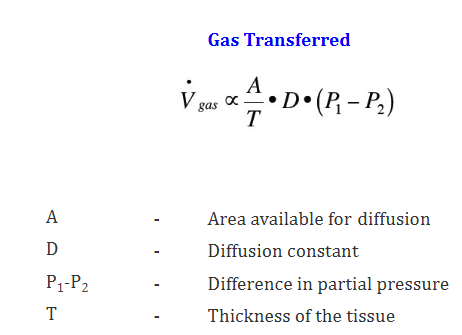
What does Fick’s Law describe
Diffusion through tissues
(Fick → Thick. What does thickness decide? Diffusion rate!)
Fick’s Law
The thicker the membrane, the less gas goes across
Put these in order of increasing %O2: Inspired air, Alveolar air, Expired air
Alveolar air, Expired air, Inspired air
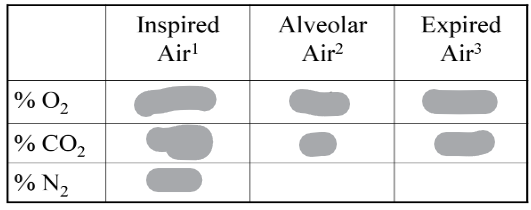
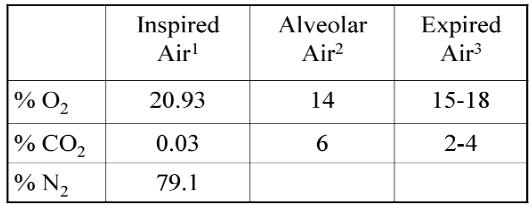
NB Vapour pressure in alveolar air at body temp is _____
47mmHg
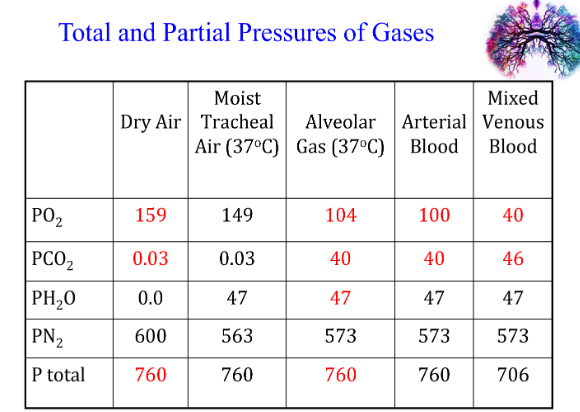
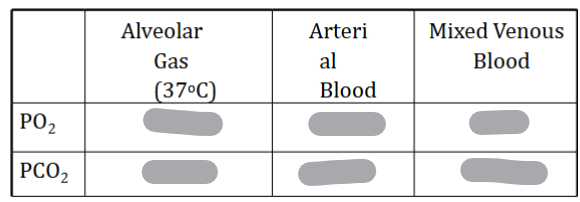
Why is the amount of oxygen in arterial blood not the same as in alveolar gas
Shunting
Volume of gas over time ( dot = over time)
Volume of gas transferred over time through tissue formula
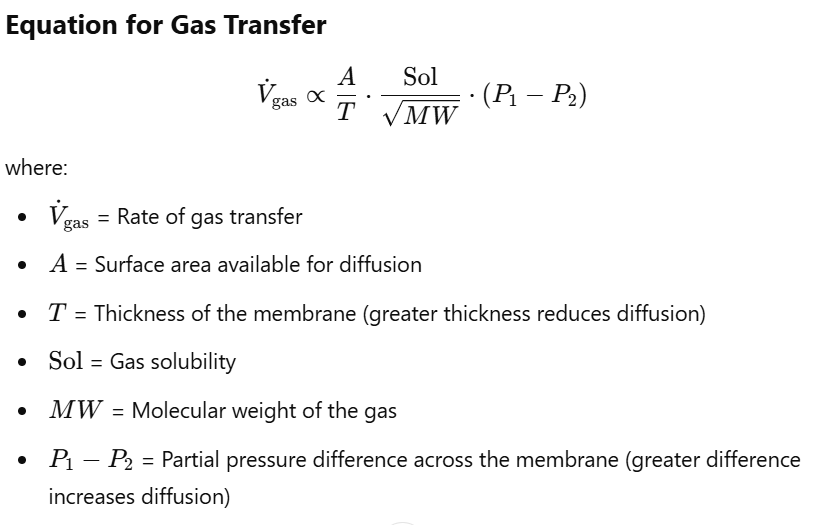
Gas transferred formula using gas solubility
What gases can exert a partial pressure in the blood
Only gas that dissolves in plasma exerts a partial pressure
Perfusion
the passage of fluid through the circulatory system or lymphatic system to an organ or a tissue
What is perfusion limited ventilation
Gas crosses the alveolar membrane and Dissolves in blood
The partial pressure of that gas in the capillary quickly equilibrates with the alveolar partial pressure
Further transfer will be possible if more blood passes with lower partial pressure passes through the alveolar capillary
What is diffusion limited ventilation
Gas crosses the alveolar membrane binds to haemoglobin - exerts NO Partial Pressure
NO equilibration of partial pressures
The gases ability to diffuse across the membrane is limiting factor
Does CO (carbon monoxide) in blood cause a big/small rise in partial pressure
very small
Is CO transfer perfusion/diffusion limited
diffusion limited
Laughing gas chemical formula & name
Nitrous Oxide (N2O)
Is Nitrous Oxide transfer perfusion/diffusion limited
perfusion
How is Nitrous Oxide perfusion limited
It depends on capillary blood flow
N2O diffuses into capillary
It doesn’t bind to Hb
Hb has low avidity for N2O
N2O dissolves in plasma
PN2O rises rapidly
Equilibrates with Alveolar PN2O
No more N2O is transferred
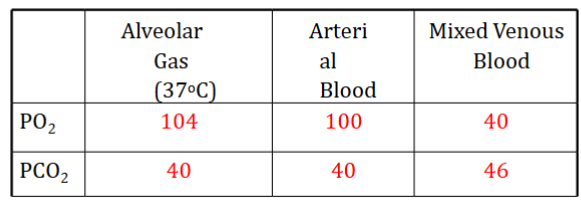
Is oxygen transfer perfusion/diffusion limited, how?
Perfusion limited
Oxygen binds to haemoglobin & equilibrates with alveolar PO2
How long does oxygen take to equilibrate with alveolar PO2
0.25 sec
In an abnormal / non-healthy lung is transfer of oxygen diffusion/perfusion limited, how?
Diffusion
Thickened barrier
Diffusion impaired
Equilibrium may not be reached
Ability to diffuse across the membrane is limiting factor
What effect does severe exercise have on oxygen uptake in healthy and non-healthy lungs
During severe exercise, the RBC capillary time drops from 0.75 s - 0.25 s.
This is enough time for normal diffusion of oxygen in a healthy lung.
In a non-healthy lung with a thickened blood gas barrier & impaired diffusion blood PO2 doesn’t reach alveolar PO2
How are diffusion properties of the lungs measured
Single Breath Method
Single inspiration of CO mixture, hold for 10s, then expire
Calculate the rate of CO diffusion: Subtract CO in expired air from original CO concentration
How are diffusion properties of the lungs measured (formula)
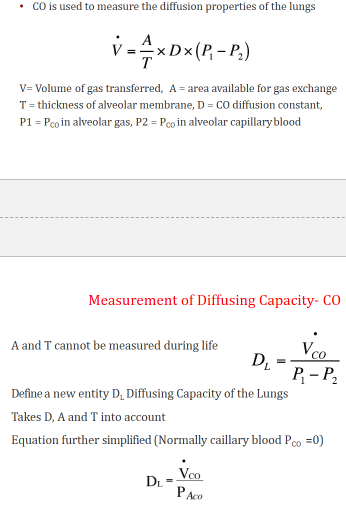
Normal value of diffusing capacity for CO at rest
Units important!
value of diffusing capacity for CO during exercise is how many times that of rest
2 or 3 times
Why blood gas barrier in lungs is ideal for diffusion
Area of barrier is large (50-100 m2)
Thin membrane of 0.3 μm in many places
Why CO2 diffuses more readily than O2
CO2 diffuses 20 x more readily through tissue than O2, even though it has a similar MW, as it has a much higher solubility in the tissues
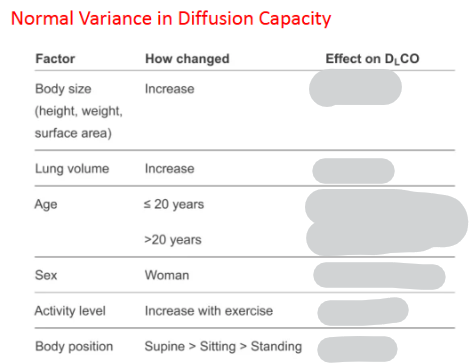
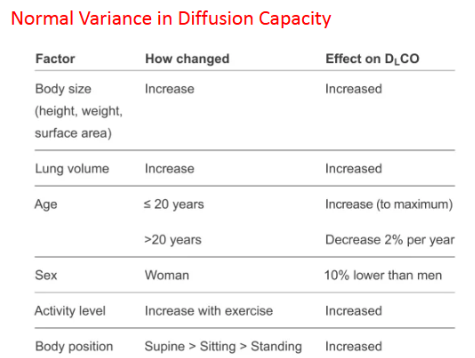
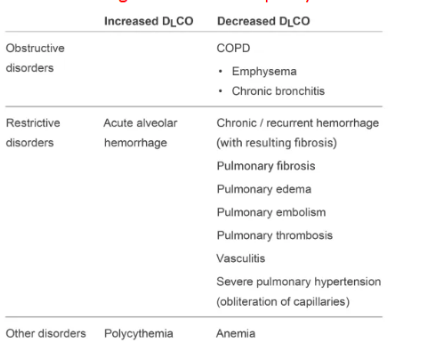
What diseases can increase/decrease diffusion capacity