Lecture 6 - Genetic Concepts: Application in HLA and Blood Group Typing, Flow Cytometry
1/84
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
85 Terms
Gene - Mendelian definition
Basic unit of heredity
Gene - Molecular definition
A specific sequence of DNA which is transcribed to produce a protein
Locus
Specific location of a gene on c chromosome (i.e. RHD gene locus is on chromosome 1, and ABO is on chromosome 19)
Genotype
Combination of alleles for a specific trait
Phenotype
Anything that is produced by the genotype, could be an enzyme to control a blood group, or a protein to regulate RBC production
Allele
Different forms of a gene at the same locus
Autosomal
The chromosomes with number (1-22) are autosomes, every individual has 22 pairs of autosomal chromosomes and one pair of sex chromosomes, any trait/phenotype carried on any of the 22 pairs will have an ________________________ pattern of inheritance
X - linked
AA = Homozygous
AA = heterozygous
Any trait carried on X chromosome
AA =
AO =
Dominant gene or allele
it will be expressed in both homozygous and heterozygous states, in AA and AO, A will be expressed (A and B are dominant over O), usually denoted by capital letter
Recessive gene or allele
Usually denoted by lowercase, for instance h is recessive vs H, it can be expressed only in a homozygous state (hh, OO)
Amorph
Gene is inherited but cannot produce any product, O gene in the ABO system is...
Hemizygous
One allele is normal with the other is mutated or deleted (i.e. XY males with hemophilia A (FVIII) deficiency), chromosome X carries the mutated allele
Co-dominant
Both alleles inherited from both parents will be expressed, one gene is not dominant over the other
ABO, Rh, Kell, KIdd
What blood group antigens are inherited in co-dominant fashion?
Antithetical antigens
In the Kidd blood group sysem where the alleles JKA and JKB encode the Jka and Jkb antigens
Jka and Jkb are considered
cis position
trans position
When alleles found on the same chromosome, they are:
When alleles found on opposite chromosomes, they are
O
Which blood group cannot be inherited by any offpsring of parents with AA and BO genotypes?
A, AB, O, or B
OO
If the father's blood group is O, what is his most likely genotype?
AO, BO, AB, or OO
Both as they are co-dominant
If a person inherits K and k alleles (Kell blood group system), what antigens will be expressed on their RBCs
a) Only K because it is dominant over K
b) Only k because it is dominant over K
c) None of them, as both are amorph
d) Both, as they are co-dominant
Chromosome 6
Genes encoding HLA antigens are part of MHC gene system located on chromosome __?
MHC system
What system is first recognized and named from experiment in tissue transplantation?
Class I - A, B, C loci
Class II - D region; DR, DR, DQ
Class III - code for complement proteins and cytokines
Inheritance of HLAs
MHC genes are divided into 3 classes, name each class and the located
HLA genes
Genes that are closely linked and is inherited as one haplotype from each parent
Both haplotypes are expressed by offspring
Serologic or molecular methods
Each antigen with unique number are determined by what types of methods?
LOW
What is the probability that any two individuals will express the same HLA antigens
MHC region
Most polymorphic system of genes in humans, many possible alleles at each location
Letter - designates the locus
Number - indicates the antigen
HLA Nomenclature
Letter designates:
Number indicates:
At C locus
"W" distinguishes HLA C-locus antigens from complement components
HLA Nomenclature
At what locus is "w" included for?
What does it distinguish?
number of antigens
In HLA nomenclature, the number of alleles determined continues to increase. What stayed the same?
More accurate and specific molecular typing assays
When HLA nomenclature began, the only test method was the lymphocytotoxicity assay. What is there now in present day?
Serologic testing
Low-resolution typing
High-resolution testing
HLA Nomenclature
A2 for antigen level resolution is determined by?
HLA-A*02 is for:
HLA-A*02:01 is for:
HLA class I
Found on surface of platelets, leukocytes, and most nucleated cells
Mature RBCs
reticulocytes
What lacks HLA antigens?
In blood, what type of cells express HLA class I antigens?
HLA class II
Found on antigen-presenting cells (i.e. macrophages, dendritic cells, and B cells)
Greater than
In the circulation, the number of cells expressing class I antigens is _______________________ the number of cells with class II antigens
Because class II antigens are not found on platelets
Why is it NOT necessary to match class II antigens when HLA-compatible platelets are requested
Lymphocytotoxicity test method aka complement-dependent cytotoxicity (CDC)
What type of test does serologic HLA identification require?
What is it also known as?
Antibodies in micro-liter plates (96 well)
Serologic HLA Identification (typing)
Suspension of B or T cells is incubated with what?
Complement from rabbit serum
Vital exclusion dye
Serologic HLA Identification (typing)
What is added with additional incubation? What is it followed by?
Activation of complement
Takes in the dye -- the cells are stained
Serologic HLA identification (typing)
If Ab-Ag reaction occurs, what causes lysing of the cell? What does it take in?
Reaction Intensity
Serologic HLA identification (typing)
What is each well score based on?
Cells that tape up the dye are positive
Cells that have no color (white) are negative
Serologic HLA Identification (typing)
What is a positive result vs a negative result?
Antibodies cant react to more than one epitope (or cross-reactive bodies), and specific antibodies have not been developed to recognize many different HLA antigens
Why is serologic typing of HLA antigens being replaced by molecular methods?
ABO comptability
careful matching of HLA antigens in patients with existing antibodies
What do successful (viable) transplants require?
Pregnancy
Blood transfusion
Previous transplants
Patients may become sensitized to HLAs by the following exposures:
HLA-A1
A negative test in serologic HLA identification indicates that the patient does NOT possess
Serologic tests on microtiter trays (30-60 antigens)
% Panel-reactive antibody (PRA)
What are the tests that are administered prior to organ transplant for HLA antibodies?
% Panel-reactive antibody (PRA)
The proportion of lymphocytes in the panel that are killed by the patient's serum or the number of antibodies
A high PRA means that the recipient patient has many reactions, making it less likely compatible with available donor organs
If the patient has a high PRA, what is the probability that the patient will be compatible with available donor organs?
Calculated panel-reactive antibody (CPRA)
Newer solid-phase method/more sensitive and specific/determines probability of compatibility to donor organ
Antigens that the organ candidate is reactive against
Unacceptable antigens
What is the CPRA number based on?
What is this called?
Determining reactivity within the general donor population
What does the CPRA provide a statistical guide for?
Genetic relatedness of the donor and the recipient
What is the transplantation of cells or tissues classified by?
Autograft
Transfer of tissue from one area of the body to another of the same individual
Allograft
Transfer of cells or tissue between two genetically disparate individuals of the same species
Syngeneic graft aka isograft
Transfer of cells or tissues between individuals of the same species who are genetically identical
Ex) identical twins
Xenograft
Transfer of tissue between two individuals of different species
Allografts and xenografts
What tissue transfers results in a vigorous cellular and humoral immune response to the foreign MHC antigens? What does this primarily stimulate?
Direct Allorecognition
Indirect Allorecognition
The immune system of the recipient recognizes foreign HLA proteins by what mechanisms?
Direct allorecognition
Cytotoxic T cells from the host bind directly to foreign HLA (MHC I) proteins on graft cells
Indirect allorecognition
APCs from the host present foreign MHC I or MHC II antigens to CD4+ Th cells, which produce cytokines that stimulate graft rejection
T cells proliferate in response to foreign HLA-D antigens
In mixed lymphocyte reaction (MLR)-an in vitro assay, if the HLA-D antigens (class II antigens) of two cell populations differ, what occurs?
Incorporation of thymidine into the DNA of the proliferating cells
How is the T cell response in mixed lymphocyte reaction (MLR)-an vitro assays quantitated?
Donor is more likely to simulate graft rejection
A high level of radioactivity indicates what in the mixed lymphocyte reaction (MLR)?
Kidney and pancreas transplants
Crossmatching recipient serum with T and B cells from the potential donor to avoid rejection caused by antibodies to the donor tissue is possible for
compatibility and D (class II) antigen typing
Mixed lymphocyte (MLC) crossmatching was historically used for...
Immuno-fluorescent flow cytometry techniques
What has replaced MLC crossmatching?
Aplastic anemia
Leukemia
Lymphoma
Hodgkin's disease
What does can be treated by HPC transplants?
HLA matching at the allelic level
What is important in HPC transplants in order to avoid rejection and graft-versus-host disease (GVHD)?
Graft-versus-host Disease (GVHD)
Occurs when grated immunocompetent cells from donor mount immune response against host tissue
- can occur in any organ transplant
When recipients of HPC transplants become immunosuppressed to allow for donor cell growth
When is GVHD more likely to occur?
Platelets do not contain class II HLA antigens
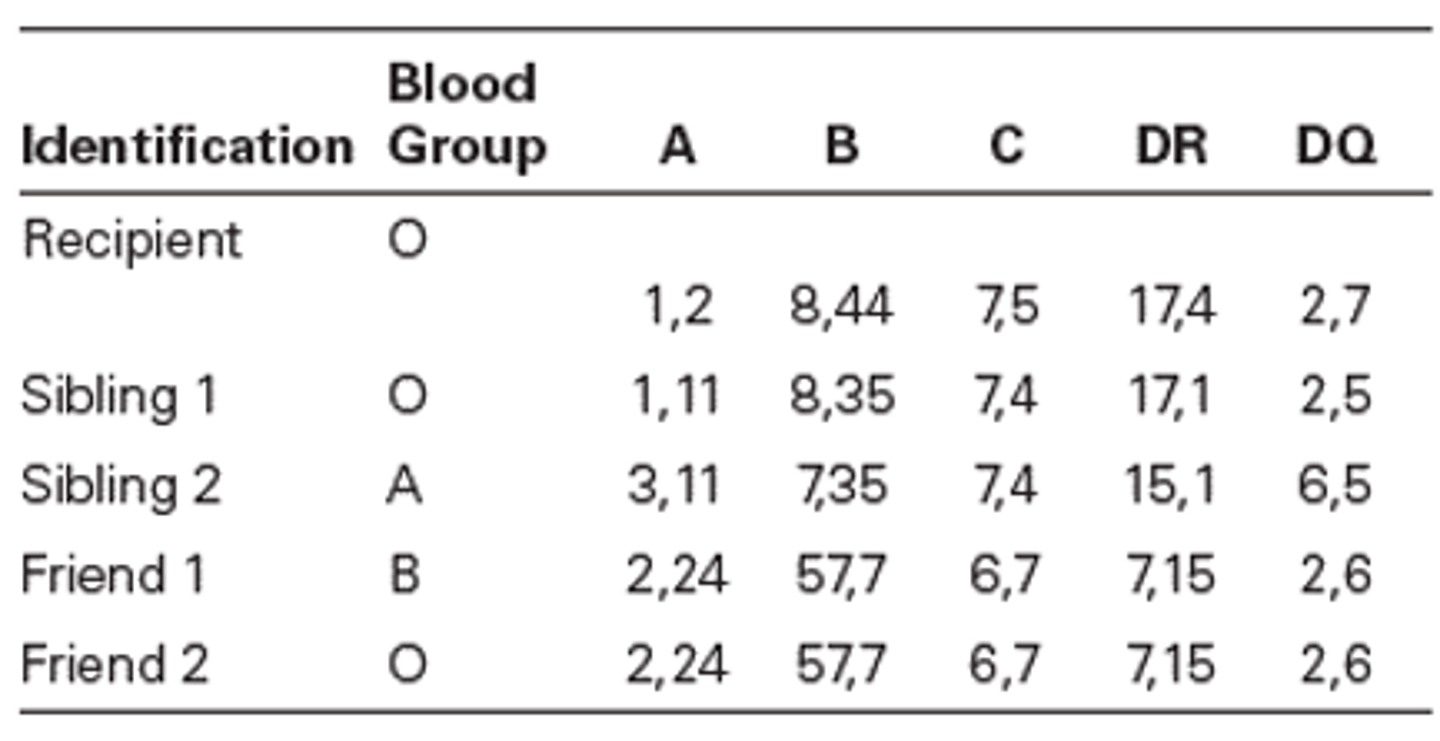
Case Study 1: HLA Graft/Donor Selection
A patient who is not responding to platelet transfusions requires HLA matched platelet transfusion. The patient's HLA type is determined and is reported as A2, A11, B8, B35. No report of the HLA C antigen is given. A donor with a compatible type is called on to donate for this patient.
Why were the HLA class II antigens not considered for matching?
A2, B50, DR17
Sibling 1
Case Study 2: HLA Graft/Donor Selection
Parents of a kidney transplant candidate were tested for a potential compatible kidney match within the family because the patient had produced HLA antibodies. The patient's HLA antigens were typed and found to be:
A1, A2, B27, B50, DR11, DR17.
Antibodies identified were specific for:
A3, B18, and DR7 antigens.
The mother's HLA typing is:
A1, A3, B35, B27, DR4, DR11
The father's HLA typing is:
A2, A24, B50, B44, DR1, DR17
Siblings HLA Typing:
Sibling 1: A1, A24, B27, B44, DR11, DR1
Sibling 2: A3, A2, B35, B50, DR4, DR17
Sibling 3: A3, A24, B35, B44, DR4, DR1
What HLA antigens did the father contribute?
Select the sibling with the best match.
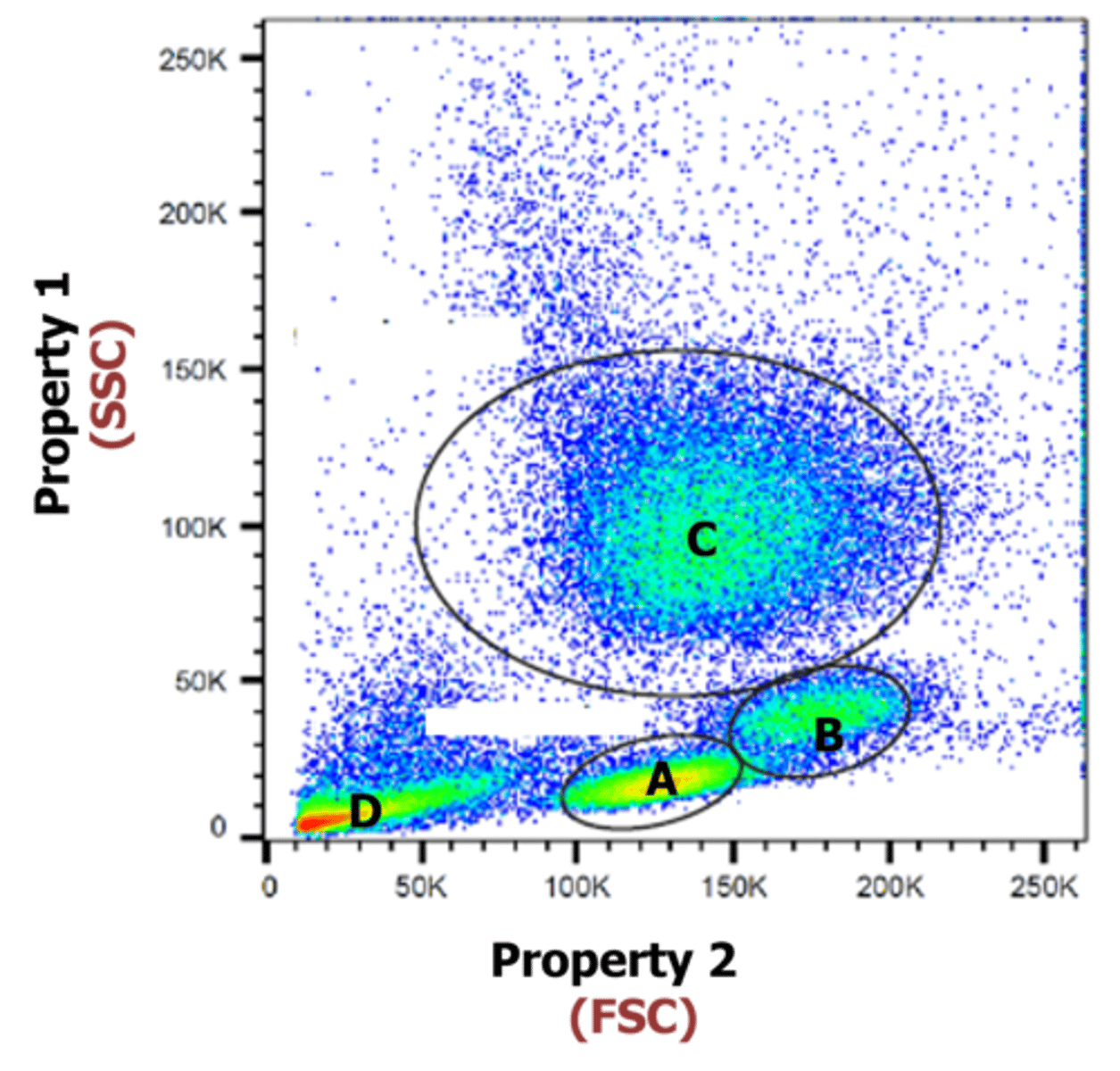
Flow Cytometry
Technique that involves measuring the physical and chemical properties of cells which are flowing in a stream of fluid
A. Lymphocytes
B. basophils
C. Monocytes
D. Neutrophils
Indicate what A-D is
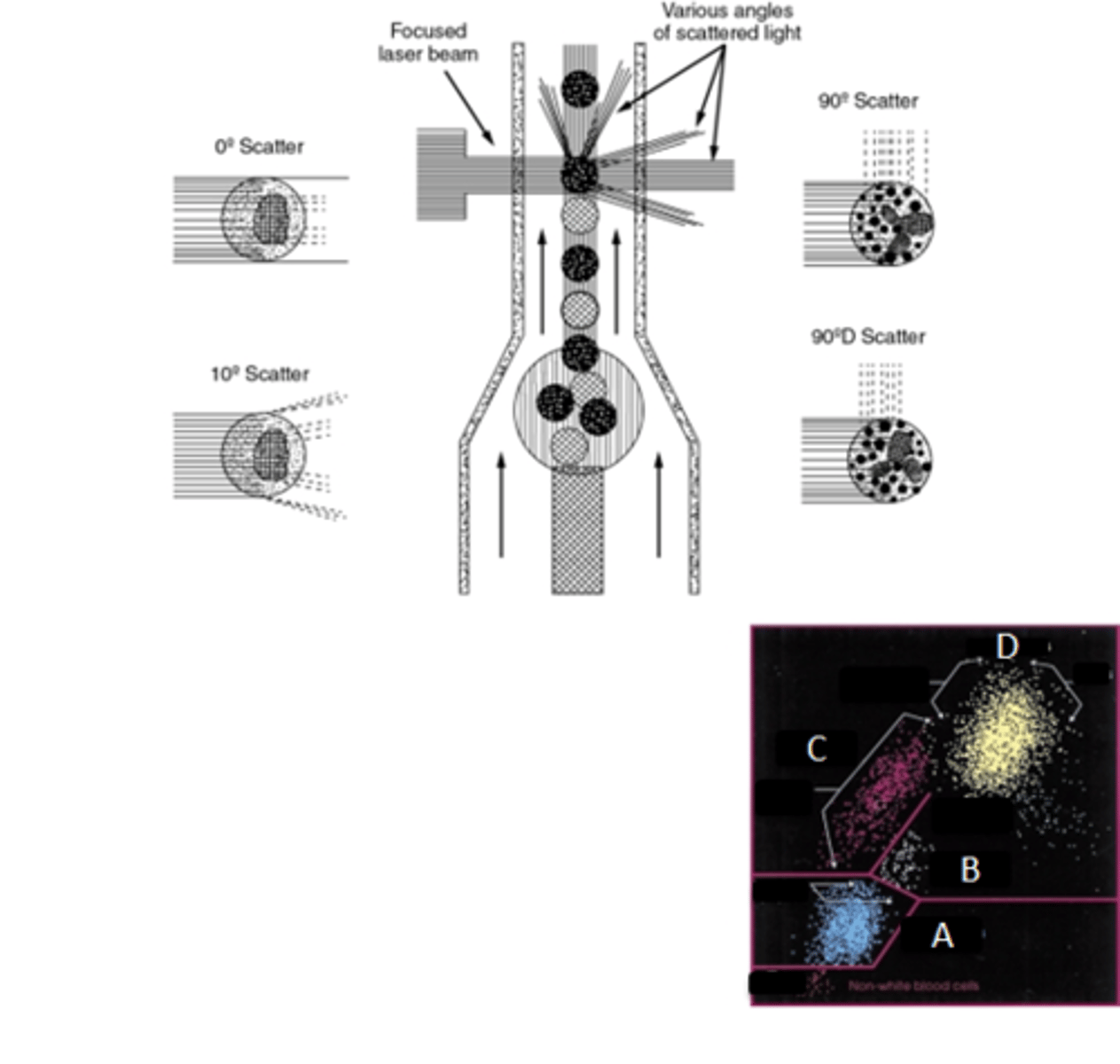
Fluidics - sheath fluid tank, flow cell
Optics - lasers, filters
Detectors - FSC, SSC, and FL
Electronics - ADC system, data processing system
Flow Cytometry components
Cluster of differentiation
The term "CD" stands for
Identification and characterization of leukocytes
Cell surface markers are useful for....
mAbs conjugated with FL
What is used to detect CD markers?
A - lymphocytes (small size, low complexity)
B - monocytes (largest size, low/medium complexity)
C - granulocytes (medium size, highest complexity)
D - dead cells, nRBCs, debris (smallest size, lowest complexity)
Indentify A-D
Friend 2
A 40-year-old mother of three needs to have a second kidney transplant. Her first transplant was lost because of chronic rejection. The mother's HLA type, HLA antibodies, and ABO blood group status were determined. The patient was found to have antibodies to HLA-B35 by flow cytometric testing with HLA-B35-coated beads. The HLA type and blood group were also determined for two of her siblings and two close friends who are interested in donating a kidney to the patient.
From the available donors, who would most likely be the most compatible patient?
(Percentage fetal cells x 1800 x 1.22)mL
FMH volume formula
6 lasers
21 detectors
23 parameters
96-well plate loader
CytoFLEX Lx Flow cytometry components
How many lasers?
How many detectors
How many parameters
What type of well is it equipped with?
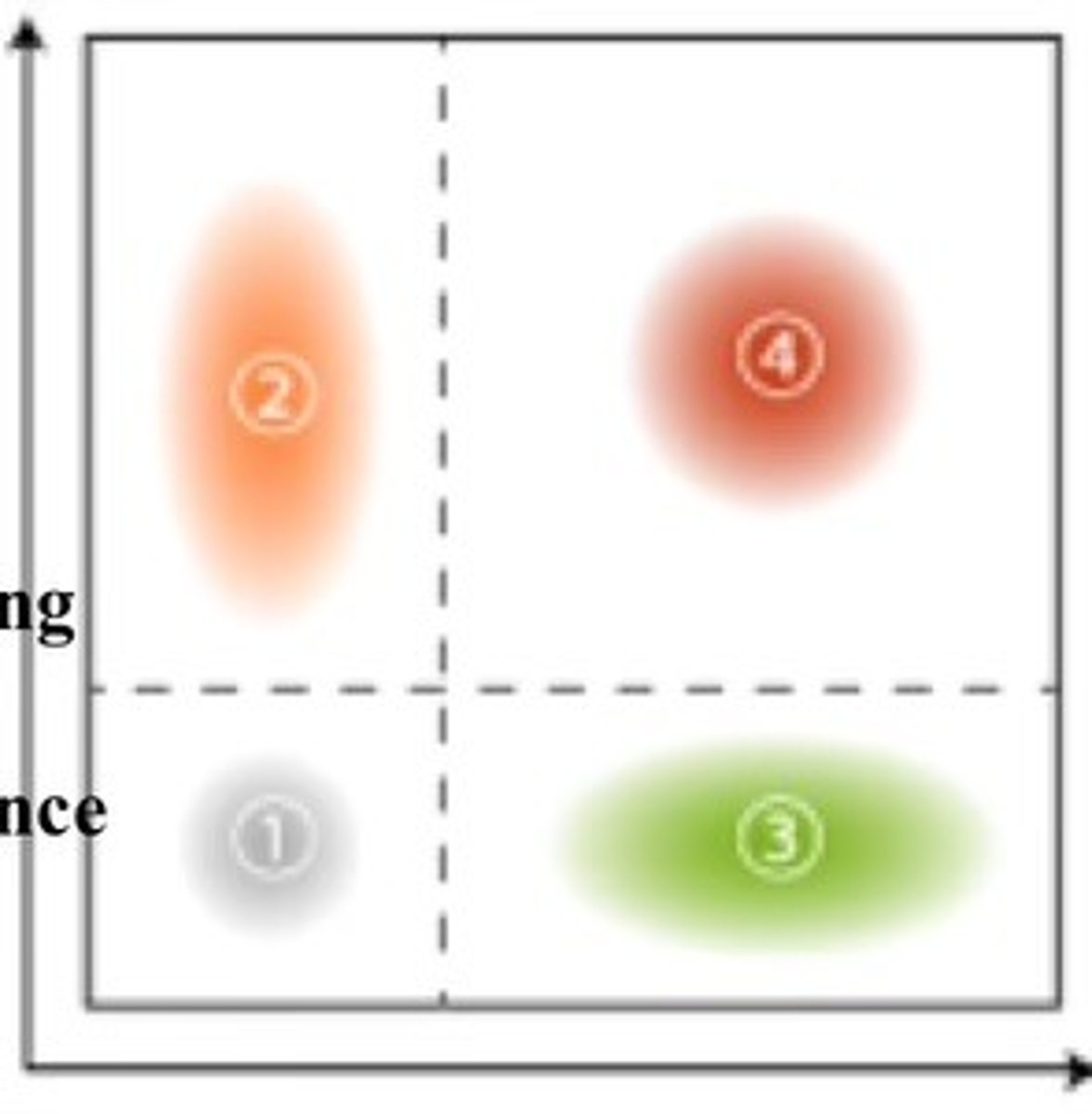
X-axis - increasing green fluorescence
Y-axis - increasing red fluorescence
1 - cells not expressing either A or B
2 - cells expressing only B
3 - cells expressing only A
4 - cells expressing both A and B
Identify the X and Y axis
Identify 1-4 and what it tells us
1) SCID/HIV
2) CD34
3) CD55/CD59
4) RNA binding dyes
5) Ab against HbF, RHD, CA
6) DNA content
7) HLA, flow cross match
Other applications of Fc in Hematology
List what pertains to each:
(Word Bank: CD34, CD55/CD59, SCID/HIV, RNA binding dyes, DNA content, HLA/flow cross match, Ab against HbF/RhD/CA)
1) immune deficiency
2) stem cell enumeration
3) PNH
4) Reticulocytes
5) FMH
6) Cell cycle analysis
7) Transplantation