Pregnancy Complications - OB/GYN EOR
1/44
Earn XP
Description and Tags
Y'all know how in fanfiction they put a like a signature song, well listen to Avenged Sevenfold lmao for this set of cards
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
45 Terms
Old maternal age (35+), prior loss, infection (Syphilis, B19, zika, etc), DM, obesity, thyroid disease, stress, factor V leiden, antiphospholipid syndrome, IUD, smoking, caffeine, EtoH, lead, arsenic, radiation
Risk Factors for spontaneous abortion
fetal chromosomal abnormalities (m/c), Maternal anatomical anomalies (fibroids, polyps, adhesions, septa, asherman syndrome), trauma, Rh immunization, malnutrition
Etiology for spontaneous abortion
Uncomplicated bleeding (patient is stable) and cramping
Typical clinical presentation of spontaneous abortion
Missed abortion
Lack of fetal development without cardiac motion on TVUS with NO dilation (dead baby, closed cervix)
Incomplete abortion
Lack of fetal development w/o cardiac motion with incomplete uterine emptying (Cervix, open, dead baby coming out)
Complete abortion
Lack of fetal development w/o cardiac motion with complete uterine emptying (open cervix, dead baby GONE)
Threatened Abortion
Vaginal bleeding and cramping + Fetal development with cardiac motion on TVUS + closed cervix
Thug
Treatment plan for SAB under 13 weeks - EVERYBODY gets RhoGAM
Mifepristone (softens the cervix), Misoprostol (induce contractions), if refractory D and C (1st trimester) or evacuation of the uterus (2nd trimester)
Treatment plan for SAB over 13 weeks or elective abortion - EVERYBODY gets RhoGAM
Septic abortion
An abortion that results in an infection of the uterus characterized by fever, chills, closed cervix, cervical motion tenderness, and foul brown discharge
D and E, Levofloxacin + metro
Treatment for septic abortion
Ectopic pregnancy
A pregnancy in which the egg implants in the wrong spot (usually the ampulla of the fallopian tubes)
previous ectopic, previous tubal surgery (tube is occluded) tubal ligation, tubal pathology, in utero DES exposure, IUD usage, IVF, previous cervicitis or PID, multiple partners, smoking, previous pelvic surgery, douching, early age of intercourse
Risk factors for ectopic pregnancies
Something delays the passage of the fertilized oocyte OR the embryo wants to implant too early
Patho for ectopics
ABD pain, hx of amenorrhea or + pregnancy test, vaginal bleeding
Triad of ectopics
SEVERE abd pain/shoulder pain (Kehr’s), SHOCK type shit (tachy, syncope, hypotension, n/v), look for free fluid on a FAST exam
Presentation of a ruptured ectopic
2 BhCG quant 48 hours apart (failure to double is suggestive), TVUS (diagnostic if you can visual the sac in the wrong spot)
Diagnostics for Ectopic Pregnancy
Discriminatory zone
The serum hCG level above which a gestational sac should be visualized by U/S exam in an intrauterine pregnancy (1500-2000 on TVUS, 6500 on transabdominal)
Methotrexate (2 doses), laparoscopic salpingectomy/salpingostomy, RhoGAM if Rh neg
Treatment for Ectopics
serial beta-hCGs to make sure there is a 15% decrease in 4-7 days
Follow up for ectopics
breastfeeding, immunodeficient, EtOH usage, allergy, lungs/bone marrow/liver/kidneys/stomach are fucked, hCG above 5,000, cardiac motion on U/S, mass over 3.5 cm
C/I for Methotrexate
unstable, impending rupture, C/I to methotrexate, coexisting intrauterine pregnancy, lack of follow up, desire for permanent contraception, failed medical
Surgical management indications for an ectopic
Gestational DM
What develops in pregnant people whose pancreatic beta-cell function is insufficient to overcome the insulin resistance associated with the pregnant state?
placental hormones such as HPL, progesterone, estrogen, and cortisol induce a progressive decline in maternal insulin sensitivity and the beta cells are unable to match the demand
Patho for Gestational DM
Hx of GDM, fam hx of DM, obesity, older maternal age, non-caucasians, PCOS, previous macrosomia
Risk factors for gestational DM
Fetal macrosomia (shoulder dystocia), stillbirth, maternal obesity, Preeclampsia, gestational HTN, polyhydramnios, neonatal hypocalcemia, neonatal jaundice
Fetal complications of gestational DM
24-28 weeks
Screening for Gestational DM occurs when?
50g 1 hr → 100 g 3 hour (140+ is positive for both)
How is gestational DM screened for?
Diabetic diet and exercise (1st line), Insulin, Metformin
Treatment of gestational DM
uncontrolled/macrosomia (38 weeks+), 40wks if controlled/no macrosomia
When is gestational DM an indication for labor induction - check glucose every 2-4 hrs in labor
Gestational Trophoblastic disease (molar preg)
A neoplasm the occurs due to abnormal placental development with trophoblastic tissue proliferation that arises from gestational tissue (non maternal)
Complete (M/C)
A molar pregnancy characterized by NO embryonic/fetal structures, 46XX (with only paternal chromosomes - got in a egg with no nucleus), higher risk of malignant development (choriocarcinoma)
Partial molar
A molar pregnancy characterized by focal trophoblastic proliferation, degeneration of the placenta, and identifiable structures; usually triploid (69XXX or XXY), fetal tissue is NEVER viable
Prior molar pregnancies, under 20 y/o, over 30 y/om Asian
Risk factors for molar pregnancies
Painless vaginal bleeding, pre-eclampsia type shit before 20 weeks, hyperemesis gravidarum, uterus is TOO big for date
Clinical presentation of Molar pregnancies - can be diagnosed at 8 weeks
Beta-hCGs are hella high, TVUS shows snowstorm or cluster of grapes (complete) or normal (partial)
Diagnostics for molar pregnancies
surgical uterine evacuation, weekly beta hCGs, CXR to check for metastasis
Management of molar pregnancies
Choriocarcinoma
A malignant transformation of trophoblastic tissue that appears red/granular when cut and rapidly invades the lung, vagina, CNS, liver, and kidneys
abnormal bleeding for 6 weeks after pregnancy, failure to regress after treatment of a molar
Presentation of Choriocarcinoma
Chemo (allows for future fertility), if nonmetastatic than 1 dose of methotrexate
Treatment of choriocarcinoma - score with FIGO
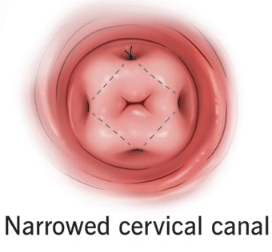
Incompetent cervix
The inability to maintain a pregnancy secondary to premature cervical dilation (usually in the second trimester)
previous cervical trauma/procedure (Leep or cone), DES exposure in utero, collagen disorder (Ehlers-Danlos, marfans)
Risk factors for an Incompetent cervix
pressure, braxton-hicks like contractions, bleeding/vaginal discharge, painless dilation and effacement of the cervix
Clinical manifestations of an Incompetent cervix - often asymptomatic
Cerclage performed at 14 weeks, bed rest, 17-alpha-hydroxyprogesterone (with history preterm birth hx)
Incompetent cervix management - HARD PASS BRO