13- included canines
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
Characteristics of an included canine and its frequency in upper vs lower vs locations?
Retained after period of eruption (9-13 yrs) despite having fully formed root
0.90% upper, 0.35% lower
50-80%- palatal, 15-30%- Buccal, 15-20%- intermediate
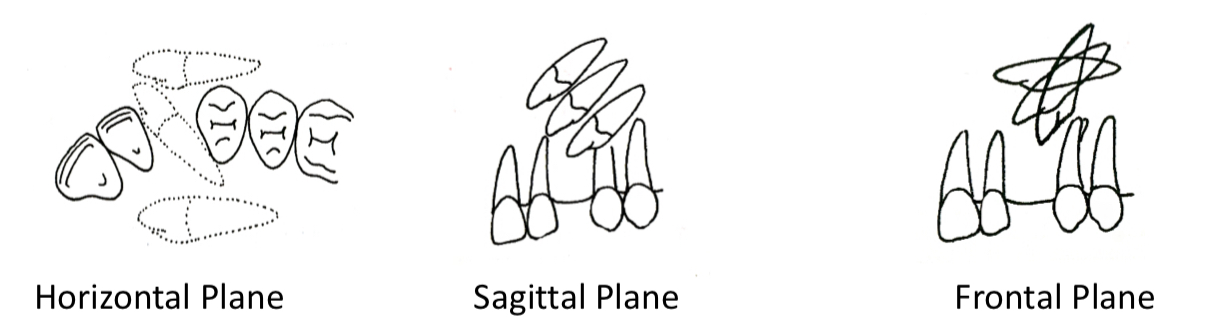
How can included canines be classified according to their position?
Horizontal plane- palatal, Buccal, intermediate
Sagital- upper, leveled or lower to adjacent apex
Frontal- vertical if less than 45 degrees, horizontal if over, angulated at 45
How can you classify an included canine according to their grade of inclusion?
Complete- no eruption
Intraosseous- crown and follicle fully covered by bone
Subgingival- crown emerges through bone covered by fibromucosa
Partial- some degree of eruption
What are some predisposing factors of included canines?
Evolutionary- arch teeth discrepancy
Anatomical- has longest and complex eruption path
Mechanics- physical obstacles
What are general vs local etiological factors leading to included canine?
General syndromes and diseases- hypothyroidism, crouzon disease, cleidocranial dysplasia
Vs
Germ- Malformation, loss of eruption potential
Environment- missing lat incisor, varying size or root formation, supernumerary teeth, cysts, tumours
What are most frequent clinical signs of an included canine?
If perm canine absent or temp still present above 13-14 yrs
Effects fit of unstable prosthesis
Linked to alopecia
Palpation of hard bulge in palate
Mechanical manifestation of included canine
Displacement or rotation of adjacent teeth- especially lateral incisor
Root reabsorption
What are causes vs consequences of infectious problems associated with included canines?
Pericoronal or adjacent infections- may cause odontogenic cellulitis, palatal abscess, maxillary sinusitis
How can you diagnose an included canine?
Panoramic
Cranium lateral teleradiography
CBCT
Occlusal x rays
Periapical
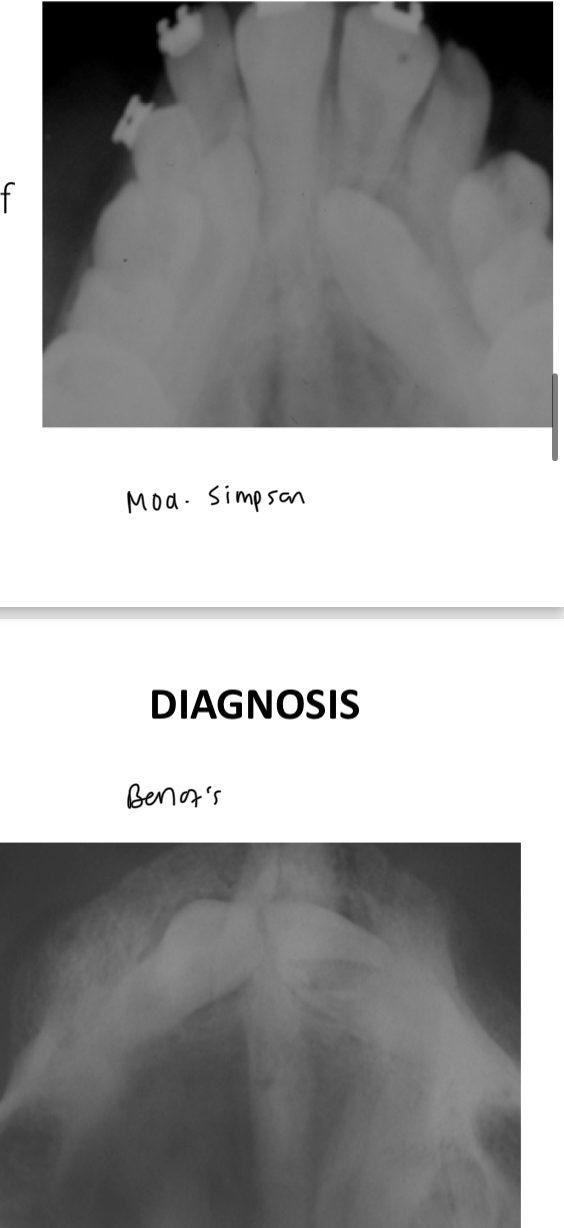
What are the 2 types of occlusal radiographs?
Modified Simpson- beam perpendicular to sensor and parallel to incisors axis
Belot’s method- not perpendicular, palatal canines appear palatal but Buccal can be either
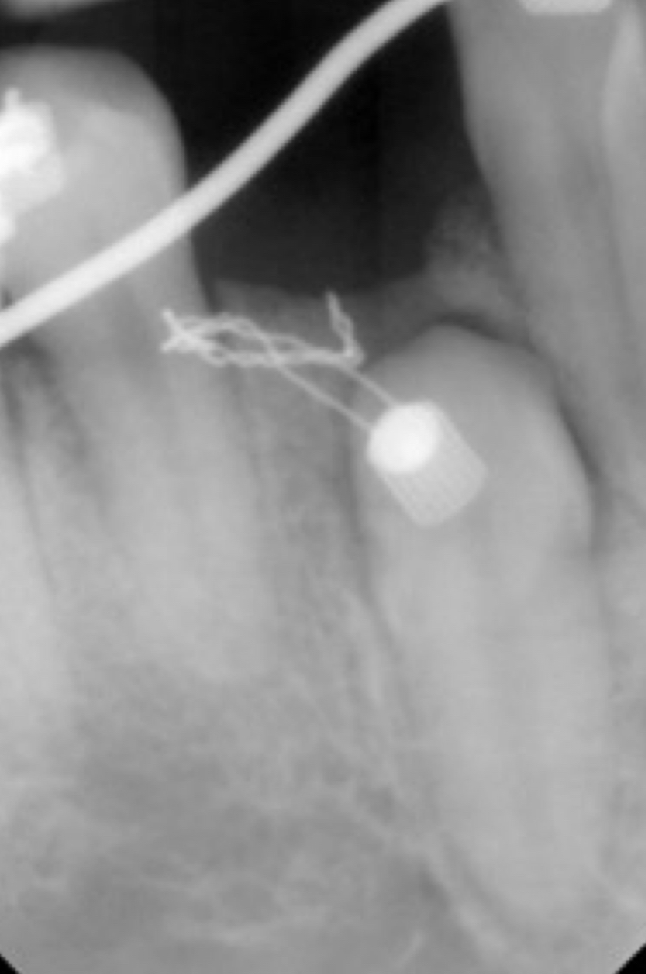
What is Clark’s positioning rule when considering periapical x rays?
Objects located in palate move in the same direction as the beam when two consecutive radiographs are obtained, the first centered and the second mesially or distally oriented
SLOB- sam lingual, opposite Buccal
What are the 3 general treatments for an included canine?
Therapeutic abstention- asymptomatic
Extract
Reposition in arch- combine surgery and ortho techniques
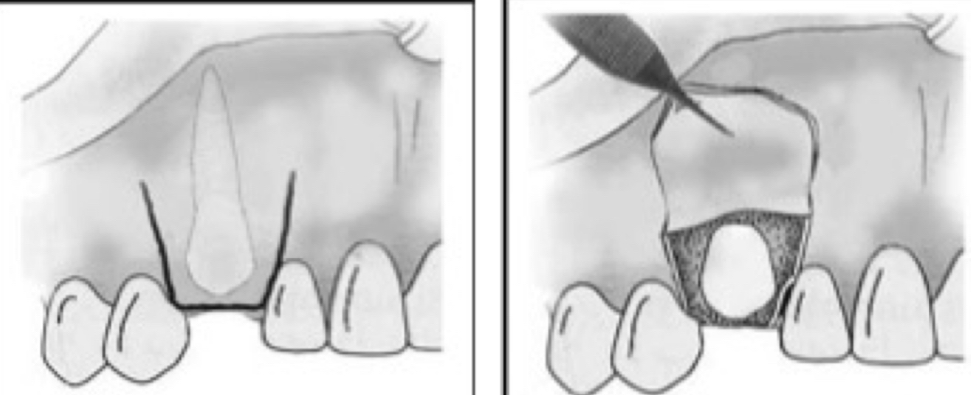
Anesthesia and incision for upper canine in palatal position
Infraorbital, nasopalatine, anterior palate from corresponding side
Scalloped from mesial 2nd molar to mesial lateral incisor of opp side OR from premolar to premolar
When an upper canine is in a palatal position- flap, ostectomy, extraction, wound review, flap
Full thickness mucoperiosteal flap
Expose crown and neck
Luxation- consider odontosection of crown
Curettage, rinse with saline and make bony borders regular
Reposition flap and suture
When an upper canine is in buccal position- anesthesia and incision
Infraorbital, nasopalatine, medium palatine from corresponding side
Bilateral- Newman from 1.5 to 2.5 with vertical relieving incisions
Unilateral- partial Newman from same side central incisor to dusta; 2nd premolar- M/D relieving incision
When an upper canine is in a buccal position- flap, ostectomy, extraction, wound review, flap
Full thickness mucoperiosteal flap
Expose crown and neck
What is the most frequent scenario of upper canines in mixed position?
Crown in palatable, root Buccal
Palatal- extract crown
Buccal- locate apex- ostectomy, lúxate towards palate or buccal
Lower canine in buccal position- anaesthesia and incision
IAN
Newman or semilunar
Lower canine in lingual position
If possible- extract from Buccal- difficult access, risk of damaging structures in mouth floor
If too lingual- linear lingual incision and pocket flap
Lower canine in mixed psition
Odontosection
Remove crown and root separately
What factors relating to surgical intervention should be considered before repositioning in arch?
Canine position and orientation
Angulation- avoid if over 45 degrees
State of tooth, periocoronal sack, ligament and apex
What is the purpose, indication and technique for conductive alveolotomy?
help eruption by exposing the crown after removing any obstacle
Canines in a favorable position that still have eruptive potential
A buccal or palatal flap is raised from the root area toward the desired canine position, ostectomy exposes crown, tooth can erupt naturally
What is the purpose, indication and technique for fenestration?
Fully expose the crown and cement it to an orthodontic button for traction- pull tooth into position
Canines in an unfavorable position with no eruptive potential
How do you conduct extra mucosal fenestration in buccal vs palatal canines?
Buccal canines- similar to conductive alveolotomy, but flap is repositioned apically, suturing the attached gingiva around the neck
Palatal- remove mucosa to expose canine
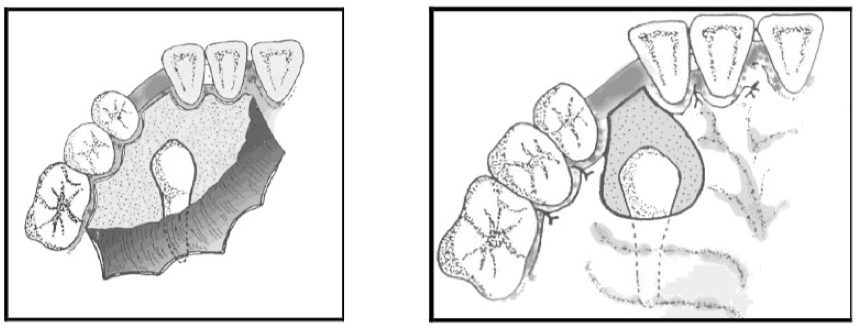
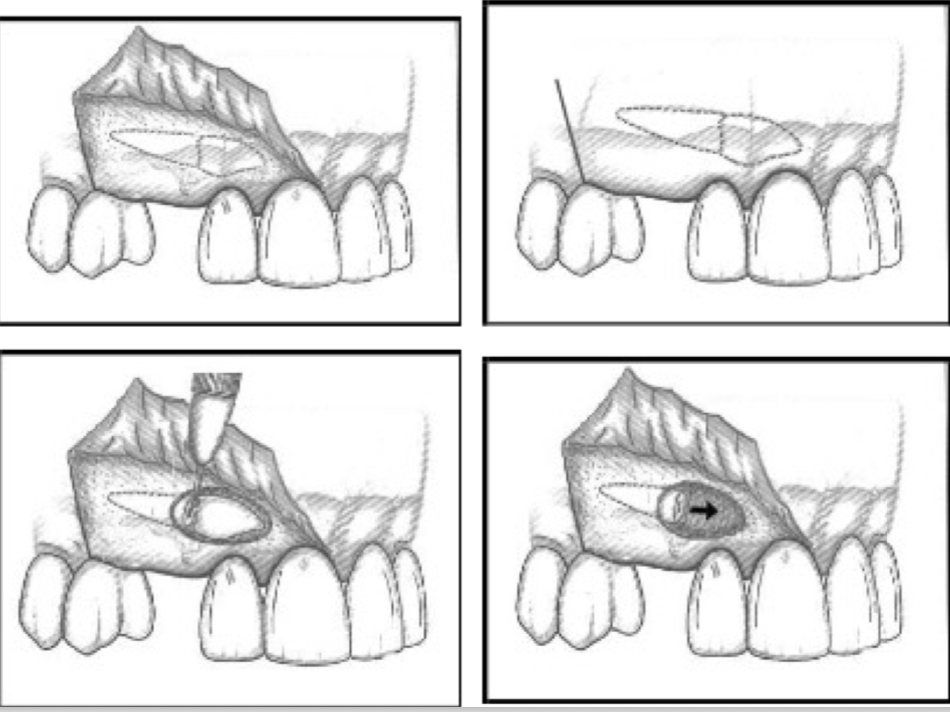
How do you conduct intra/submucosal fenestration?
Full thickness triangular flap
Cement orthodontic button, place ligature
Reposition flap and suture
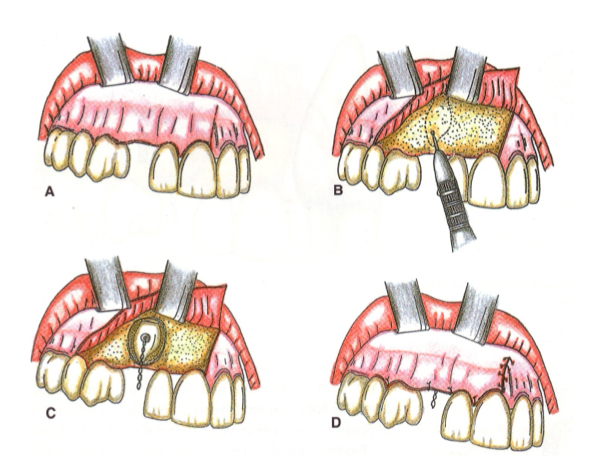
What is translation and when is it indicated?
Controlled mobilization of canine within the bone, maintains vascularization and vitality
Buccally impacted canines
Two-thirds of the root already formed
Apex in normal position
Crown mesially angulated
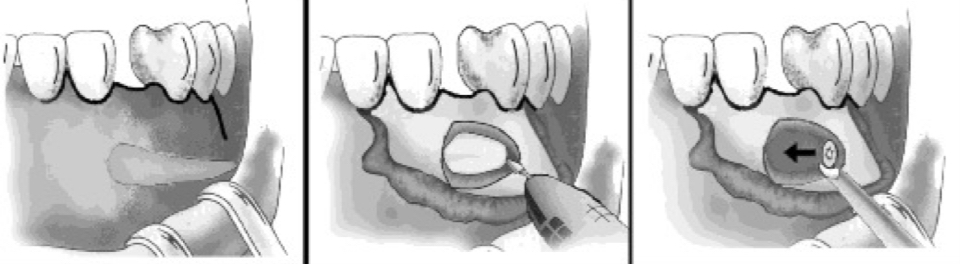
What is the technique for translation?
Crown and 2/3 of the root are freed from the surrounding bone
A new bone cavity is created distal to the canine and mesial to the first premolar
Canine is mobilized into this new position, aligning it within the arch
What is transplant?
Extraction canine and place into a prepared socket in correct position- loses og vascularisation
What are some possible intraoperative complications?
Perforation of palatal fibromucosa
Apex fracture
Injury to roots of neighboring teeth
Perforate maxillary sinus or nasal cavity
Injury to the nasopalatine or mental bundles
Postoperative complications?
Infection
Necrosis of palatal fibromucosa (from poor blood supply)
Palatal hematoma
Suture dehiscence (stitches opening)
Abnormal mobility of adjacent teeth (from trauma during surgery)