CH 18. - Blood
1/144
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
145 Terms
Hematology
the study of blood
What were once thought to be transmitted through blood?
Hereditary traits
What type of cells were seen with the first ever microscopes?
Blood cells
4 Humors:
blood
bile
saliva
urine
Circulatory System consists of…
consists of the heart, blood vessels, and blood
Cardiovascular System refers only to the. . .
heart and blood vessels
Functions of the Circulatory System:
Transport
transporting things like O2, CO2, nutrients, wastes, hormones, etc
Protection
inflammation, limits spread of infection, destroys microorganisms and cancer cells, neutralizes toxins, and initiates clotting
Regulation
maintains homeostasis through fluid balance, stabilizing pH of ECF, and temp control
Components/Properties of Blood
Blood is a liquid connective tissue made of cells and an extracellular matrix
Includes:
Plasma
Formed Elements
*Adults have 4-6 liters of blood
smaller people have less blood, larger people have more blood
Plasma
the matrix/liquid of blood
Clear, light yellow fluid
has very little protein
Formed Elements
blood cells and cell fragments
includes red blood cells, white blood cells, and platelets
7 Kinds of Formed Elements:
Erythrocytes - RBCs
Thrombocytes - platelets
Neutrophils
Eosinophils
Basophils
Lymphocytes
Monocytes
Platelets
Cell fragments from a special cell in bone marrow
Leukocytes
white blood cells
5 leukocyte types divided into 2 categories:
Granulocytes
Agranulocytes
Granulocytes
WBCs with granules
Includes:
Neutrophils
Eosinophils
Basophils
Agranulocytes
WBCs without granules
Includes:
Lymphocytes
Monocytes
Order of WBCs from most common to least common/abundant:
Never Let Monkeys Eat Bananas
Neutrophils
Lymphocytes
Monocytes
Eosinophils
Basophils
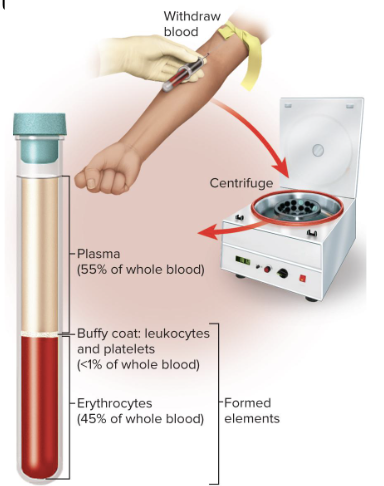
Hematocrit
measures the ratio of plasma to formed elements
centrifuges blood to separate components
Erythrocytes are heaviest and settle first
make up 37% to 52% total volume
White blood cells and platelets make up the middle layer
1% total volume
has a buffy coat
Plasma
makes up remainder of volume
47% to 63%
Complex mixture of water, proteins, nutrients, electrolytes, nitrogenous wastes, hormones, and gases
Serum in Plasma:
the remaining fluid when blood clots and solids are removed
Identical to plasma except for the absence of fibrinogen
3 major categories of plasma proteins:
Albumins
Globulins
Fibrinogen
Plasma proteins are formed by the liver
Except globulins which are produced by plasma cells
Albumin
smallest and most abundant plasma protein
Contributes to viscosity and osmolarity
influences blood pressure, flow, and fluid balance
Globulin
AKA antibodies
Responsible for the immune response
Made of alpha, beta, and gamma globulins, which combine to make hemoglobin
these do not directly target bacteria, they highlight the bacterial cells so white blood cells know what to destroy
produced by plasma cells
Fibrinogen
Blood clotting protein
is a precursor protein (almost active protein)
is one covalent bond from becoming fibrin, which is what we actually use for blood clotting
can be dissolved in water, while fibrin cannot
Other Components of Blood Plasma:
Nitrogenous Compounds
Nutrients
Gases
Electrolytes
Nitrogenous Compounds in Plasma
Includes:
Free amino acids from dietary protein or tissue breakdown
Nitrogenous wastes (urea)
toxic end products of catabolism
usually removed by kidneys and excreted through urine
Nutrients in Plasma
Anything that can be metabolically active
Includes:
Glucose
Vitamins
Fats
Cholesterol
Phospholipids
Minerals
*You need a little bit of these, but not too much
Gases in Plasma
Dissolved O2, CO2, and nitrogen
CO2 is essential for maintaining blood homeostasis, it is not always a waste product
Electrolytes in Plasma
Sodium (Na+) makes up majority (90%) of cations in plasma
Viscosity
how thick a fluid is / the rate of flow of a fluid
Whole blood is 4.5 to 5.5 times as viscous as water
Plasma is 2x as viscous as water
Important in circulatory function
Erythrocytes have the highest influence on blood viscosity
Osmolarity of Blood
the total molarity of the dissolved particles that cannot pass through the blood vessel wall
osmolarity pulls fluid across membrane
If too high, blood absorbs too much water, increasing the blood pressure
If too low, too much water stays in tissue, blood pressure drops, and edema (swelling) occurs
hard time retaining fluids
Optimum osmolarity is achieved by the body’s regulation of sodium ions, proteins, and red blood cells
Hemopoiesis
production of blood (especially its formed elements)
How Blood is Produced (5 ways):
Hemopoietic Tissues
Multipotent Stem Cells (hemocytoblasts)
Colony-Forming Unit
Myeloid Hemopoiesis
Lymphoid Hemopoiesis
How Hemopoietic Tissues Produce Blood
Hemopoietic tissues produce blood cells at a very high rate
Yolk sac stem cells create the first blood cells in utero
these colonize in fetal bone marrow, liver, spleen, and thymus
Liver stops producing blood cells at birth
Spleen remains involved with lymphocyte production and stores red blood cells
What is the primary site for hemopoiesis in adults?
red bone marrow
Hemocytoblasts / Hemopoietic Stem Cells
Red blood cell builders
type of multipotent stem cell
Colony-Forming Unit
specialized stem cells that only produce one class of formed element of blood
divides over and over again to form one kind of blood
Myeloid Hemopoiesis
blood formation in the bone marrow
Lymphoid Hemopoiesis
blood formation in the lymphatic organs
beyond infancy, this only involves lymphocytes
2 Principal Functions of Erythrocytes:
Gas transport = major function
Carry oxygen from lungs to cell tissues
Pick up CO2 from tissues, modify it to not carbonate the blood, and bring it to the lungs
does NOT transport CO2
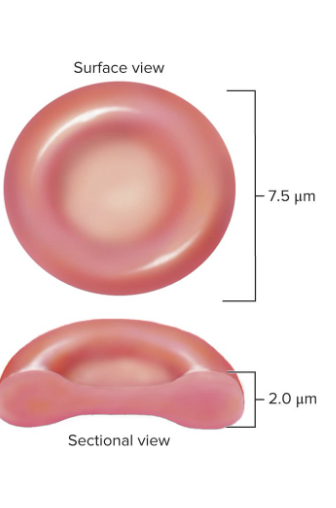
Structure of Erythrocytes
a disc-shaped cell with a thick rim
loses nearly all of its organelles during development so the cell wont consume O2 and can transport it instead
lacks mitocondria
uses anerobic fermentation to produce ATP
lack of nucleus and DNA
NO protein synthesis or mitosis
concave shape maximizes surface area, which allows for faster rate of diffusion
What is blood type determined by?
surface glycoproteins and glycolipids
Cytoskeleton of Erythrocytes:
spectrin and actin
give the membrane durability and resilience
They stretch and bend as they are squeezed through small capillaries
What is the most common dissolved substance in erythrocytes?
Hemoglobin
33% of the cytoplasm in RBCs is hemoglobin
helps deliver O2 to tissues and CO2 to the lungs
Carbonic Anhydrase (CAH) in the Cytoplasm
CAH is the enzyme that turns CO2 into carbonic acid
important role in blood pH balance and gas transport
keeps our blood from becoming carbonated
Each hemoglobin (Hb) molecule contains:
4 protein chains (globins)
adult Hb has 2 alpha and 2 beta chains
fetal Hb has 2 alpha and 2 gamma chains bc gamma has a higher affinity for O2
globins bind to CO2
4 heme groups
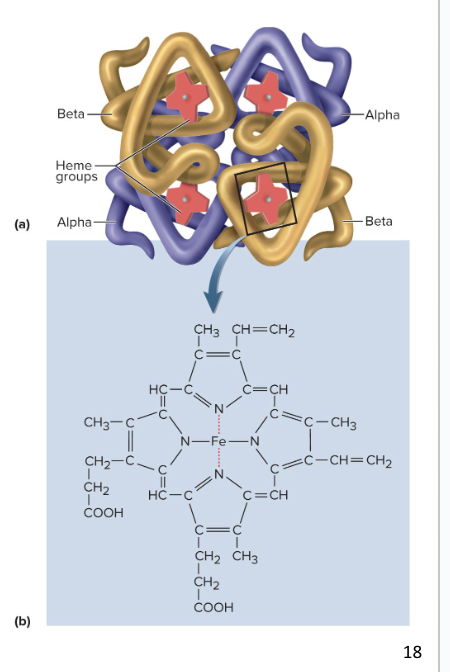
Heme Groups
a nonprotein component that binds O2 to Fe at its center
4 heme groups = 4 iron molecules in hemoglobin
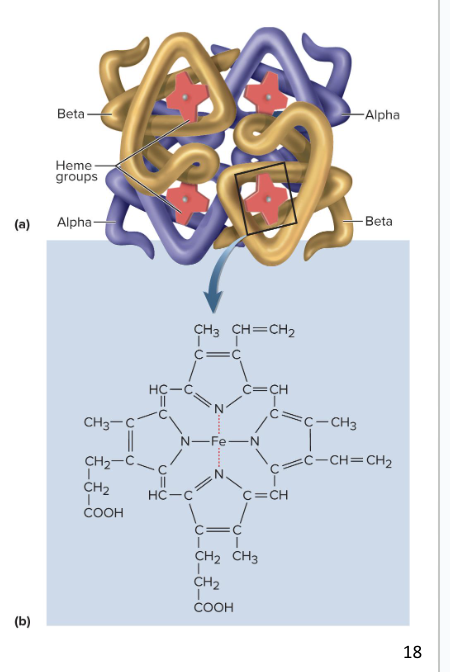
What is the ratio of globular protein to heme to stored oxygen?
1 globular protein - 1 heme - 1 stored oxygen
What determines that amount of O2 blood can carry?
RBC count and hemoglobin concentration
RBC Hematocrit Men vs. Women:
the percentage of the whole blood volume that is composed of red blood cells
Men have higher RBC hematocrit, related to testosterone (high skeletal muscle, low adipose) compared to women
Men typically have higher hemoglobin concentration and RBC count
too high of a hematocrit causes mini clots and mini heart attacks
Values are lower in women because…
Androgens stimulate RBC production, which women have less of
Women have periodic menstrual losses
Hematocrit is inversely proportional to percentage of body fat, which women have more of
Increased androgens correlate to lower body fat percentage
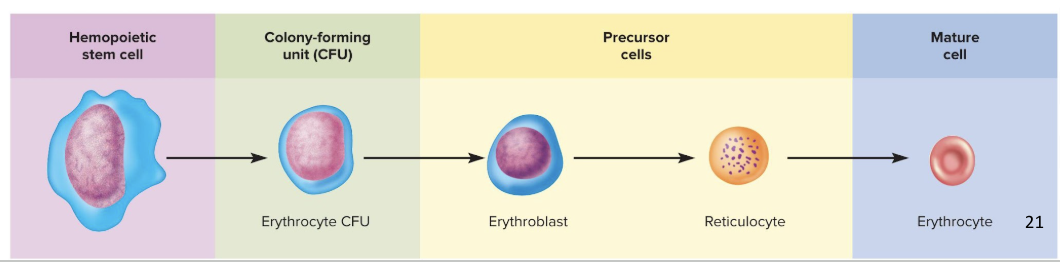
Erythropoiesis
red blood cell production
1 million RBCs are produced per second
we replace our RBCs approx. 3 times a year
development takes 3-5 days
Reduction in cell size, increase in cell number, synthesis of hemoglobin, and loss of nucleus
the first cell is a colony-forming unit that has receptors for erythropoietin (EPO) from the kidneys
erythropoietin triggers erythropoiesis in the body
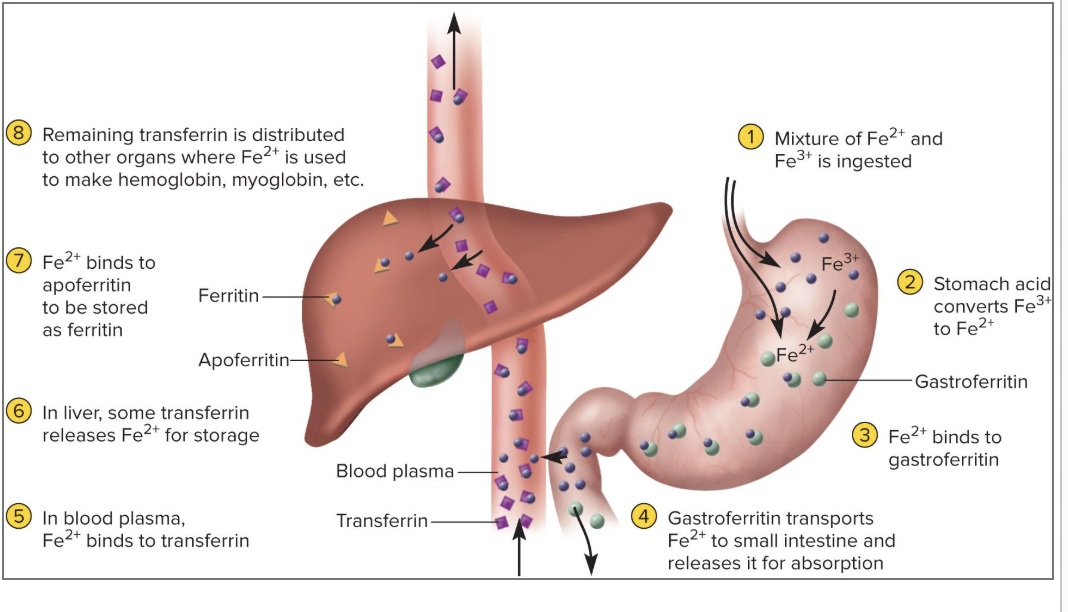
Iron (Fe)
a key nutritional requirement
dissolved iron is very metabolically active
it is lost daily through urine, feces, and bleeding
Men 0.9 mg/day and women 1.7 mg/day
Low absorption rate of iron requires consumption of 5 to 20 mg/day
to minimize bacteria growing in the blood stream, we have a protein called liver apoferritin that binds to iron to make ferritin so bacteria have a hard time accessing the iron
Steps of Iron Metabolism
We ingest iron through our diet
stomach acid converts Fe3+ to Fe2+
Fe2+ binds to gastroferritin
Gastroferritin carries iron to small intestine where it releases the iron
iron will be absorbed into blood stream by binding to transferrin
goes to the liver for storage
can be further processed in the liver
Negative Feedback Loop for Erythrocytes
a drop happens in RBC count, causing hypoxemia (low O2) to be detected by the kidneys
the kidney then produces erythropoietin which stimulates bone marrow
RBC count then increases in 3-4 days
What stimulates an increase in erythropoiesis?
low levels of O2
high altitude
increase in exercise
loss of lung tissue in emphysema
Where do Erythrocytes rupture?
RBCs rupture (hemolysis) in narrow channels of spleen and liver
9 Steps of Erythrocyte Death and Disposal
macrophages in spleen digest ruptured RBC membrane bits and separate the heme from the globin
in the small intestine, we ingest and absorb iron and other raw building blocks for erythrocytes
these materials enter the blood stream and go into red bone marrow
Then, we form erythrocytes, which circulate for 4 months before they die
dead ones are filtered out of the blood in the spleen
nutrients go back into the bloodstream, but the heme from the iron needs to get processed
iron is stored in liver to be reused while the rest of the heme group gets processed into biliverdin (one of the key components of bile)
Biliverdin gets converted to bilirubin and is released into bloodstream and filtered through the kidneys
some bilirubin will go into the digestive system, where it gets converted to urobilinogen (makes feces brown)
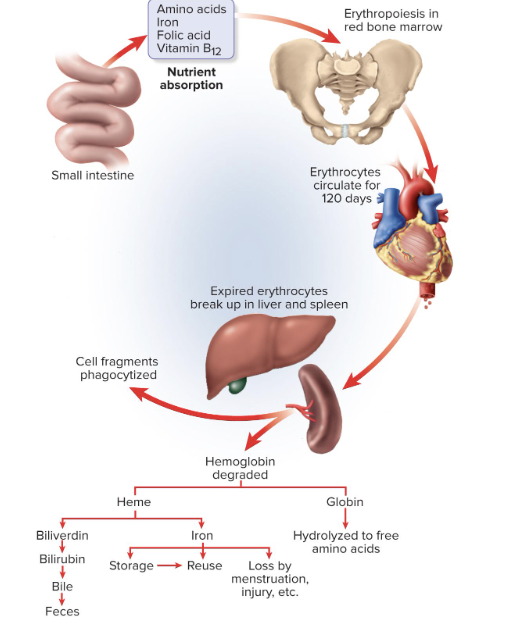
What makes our feces brown?
urobilinogen
Polycythemia
an excess of RBCs
2 types: Primary polycythemia and Secondary polycythemia
Primary Polycythemia
aka polycythemia vera
Cancer (out of control production) of the erythropoietic cell line in red bone marrow
diagnosed when individual has a hematocrit of 80% RBC count (RBC count up to 8 million RBCs/μL)
Secondary Polycythemia
excessive RBC production caused by dehydration, emphysema, high altitude, or physical conditioning
RBC count up to 8 million RBCs/μL
hard time getting oxygen into blood - emphysema
What is the most common cause of polycythemia?
out of control hemocytoblasts in red bone marrow
Dangers of Polycythemia
Increased blood volume, pressure, viscosity
makes blood more likely to clot
Can lead to embolism, stroke, or heart failure
3 Causes of Anemia:
Inadequate erythropoiesis or hemoglobin synthesis
Hemorrhagic anemia from bleeding
Hemolytic anemia from destruction of RBC
5 ways inadequate erythropoiesis can happen:
kidney failure and insufficient erythropoietin
Iron-deficiency anemia
Pernicious anemia
Hypoplastic anemia
Aplastic anemia
Pernicious Anemia
autoimmune attack of stomach tissue that leads to inadequate Vitamin B12 absorption
Hypoplastic Anemia
slowing of erythropoiesis
Aplastic Anemia
complete cessation of erythropoiesis
What is the most common source of anemia?
Inadequate erythropoiesis
What type of anemia has RBCs that appear hollow or empty?
iron-deficiency anemia
can make erythrocytes, but have a hard time filling them
3 potential consequences of anemia:
Tissue hypoxia (low O2) and necrosis
Patient is lethargic
Shortness of breath upon exertion
Life-threatening necrosis of brain, heart, or kidney
Blood osmolarity is reduced, producing tissue edema (excess fluid/swelling)
Blood viscosity is low
Heart races and pressure drops
Cardiac failure may happen
Blood types and transfusion compatibility are determined by. . .
interactions between plasma proteins and erythrocytes
Blood types are based on interactions between . . .
antigens and antibodies
Antigens
Complex molecules on the surface of the cell membrane that activate an immune response
We have 3 medically important antigens
we have over 200, but only 3 are medically important
They are genetically unique to the individual
Used to distinguish self from foreign matter
Foreign antigens generate an immune response
Agglutinogens
antigens on the surface of the RBC that are the basis for blood typing
Antibodies
Proteins (gamma globulins) secreted by plasma cells
Part of immune response to foreign matter
You DO NOT form antibodies against your antigens
Bind to antigens and mark them for destruction
Forms antigen–antibody complexes
antibodies do not directly destroy the invader, but will highlight the issue and recruit leukocytes
the immune system should be trained not to be activated by. . .
self-antigens
Agglutinins (antibodies)
antibodies in the plasma that bring about transfusion mismatch
Found in plasma
Anti-A, anti-B, & anti-Rh
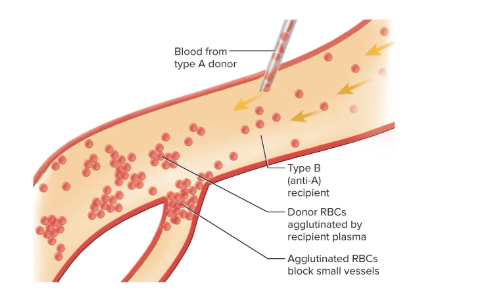
Clumping (Agglutination)
Process of an antibody molecule binding to antigens
Erythrocytes are stuck together by antibodies
Causes clumping of red blood cells
we don’t clot our blood, we clump our blood
Red Blood Cell Antigens
antigen A
antigen B
antigen Rh(D)
Determined by glycolipids on RBC surface
How is your ABO bloody type determined?
by the presence or absence of antigens on RBCs
Blood type A person has …
Blood type B person has …
Blood type AB has …
Blood type O person has …
Blood type A person has A antigens
Blood type B person has B antigens
Blood type AB has both A and B antigens
Blood type O person has neither antigen
What are the most common and most rarest blood types?
Most common: type O
Rarest: type AB
______ blood types has Rh antigen, ______ lack Rh antigen.
Positive blood types has Rh antigen, negative lack Rh antigen
How to test blood type:
use Antibodies anti-A and anti-B and mix with samples of the blood
You DO NOT form antibodies against your antigens, so your blood will mix with the antibodies and clot if your RBCs have the antigen

Why do we only want to introduce blood that has self-antigens to a patient?
Because otherwise clumping can happen
Each antibody can attach to several foreign antigens on several different RBCs at the same time
Responsible for mismatched transfusion reaction
Agglutinated RBCs block small blood vessels, hemolyze, and release their hemoglobin over the next few hours or days
Hb blocks kidney tubules and causes acute renal failure
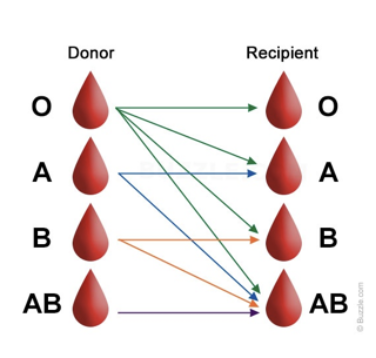
Universal Donor
Type O-
No RBC antigens
Donor’s plasma may have both antibodies against recipient’s RBCs (anti-A, anti-B, anti-Rh)
May give packed cells (minimal plasma)
we separate blood plasma and blood cells to separate antibodies
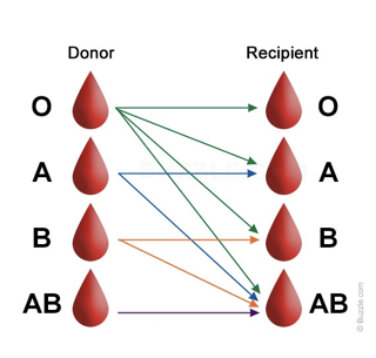
Universal Recipient
Type AB+
Lacks plasma antibodies
no anti-A, anti-B, or anti-Rh
If you have A blood type, you will be making ______ anitbodies.
If you have B blood type, you will be making ______ antibodies.
It you have O blood type, you will be making ______ antibodies.
If you have A blood type, you will be making anti-B anitbodies.
If you have B blood type, you will be making anti-A antibodies.
If you have O blood type, you will be making both anti-A and anti-B antibodies.
If you have negative blood type…
you cannot receive positive blood types
If you have positive blood type…
You can receive both positive and negative blood types
Hemolytic Disease of the Newborn
after a - blood type mother gives birth to a + blood type baby, the moms anti-rH antibodies will cross over and attack the babies blood
will only happen if mom has negative blood type
can tell if there is hemolytic disease if there is nucleated erythrocytes in the blood stream
Second pregnancy mother with negative blood type is most likely to develop this disease
How can we help Hemolytic Disease?
We inject the mom (who has - blood type) with anti-rH antibodies bc they will bind to the fetal rH-postive cells and "mask" them, making them invisible to the mother's immune system and stopping the immune response that would otherwise destroy the baby's red blood cells
If both parents are negative, you dont need to inject anti-rH antibodies bc its impossible to get a + blood baby then
Leukocyte Characteristics
least abundant formed element
5,000 to 10,000 WBCs/μL
if more than that, your body is actively fighting off an infection
huge nucleus
needs one bc it makes a lot of proteins to fight off invaders
Spend only a few hours in the bloodstream before moving to connective tissue
Keep their organelles for protein synthesis
Have granules (membrane-bound organelles)
Granules in Leukocytes
All WBCs (leukocytes) have lysosomes called nonspecific granules
Granulocytes (a type of WBC) have specific granules that have enzymes and other chemicals employed in defense against pathogens
Types of Leukocytes:
Granulocytes and Agranulocytes
Granulocytes include:
Neutrophils
Eosinophils
Basophils
Agranulocytes include:
Lymphocytes
Monocytes
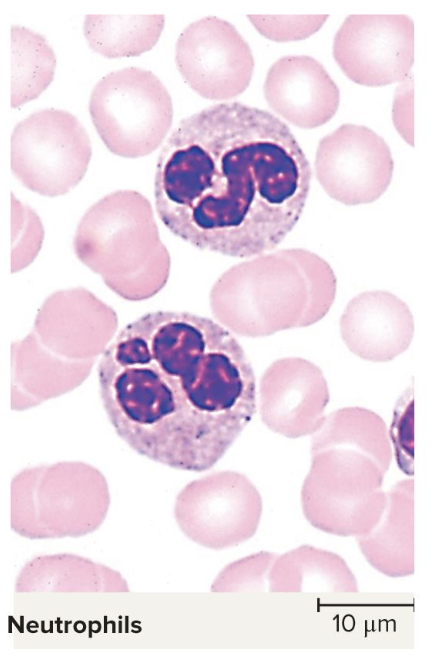
Neutrophils
fight off bacteria
makes up 60% to 70% of leukocytes
have multi lobe nuclei
the most common leukocyte
Have barely visible granules in the cytoplasm
1.5x diameter of a erythrocyte
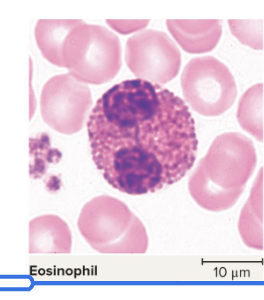
Eosinophils
fight off parasitic infections
make up 2% to 4% of leukocytes
Have large rosy-orange granules
has a bilobed nucleus
Phagocytize (eating) antigen–antibody complexes, allergens, and inflammatory chemicals
Release enzymes to destroy large parasites
4th most common leukocyte
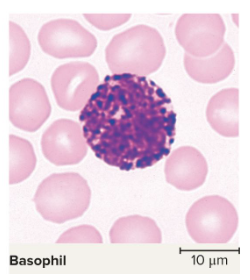
Basophils
involved with allergies
have purple granules fill cytoplasm
secretes histamine
this causes blood vessels to expand and let more blood flow to an area, causing area to be warm and red (inflammation)
secretes heparin -
this regulates blood clotting so its easier to get white blood cells to infection
you want a happy medium of it
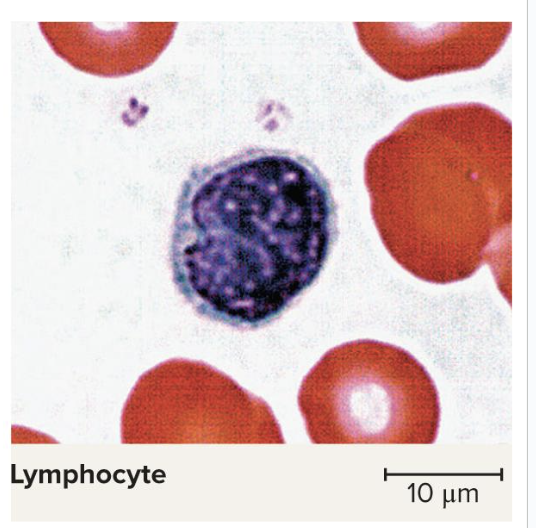
Lymphocytes
Destroys human cells (cancer, foreign, and virally infected cells)
most complicated
part of our active immune system
make our T cells and B Cells
“Present” antigens to activate other immune cells
Coordinate actions of other immune cells
Secrete antibodies and provide immune memory
look for little sliver of cytoplasm to tell the difference between these and basophils
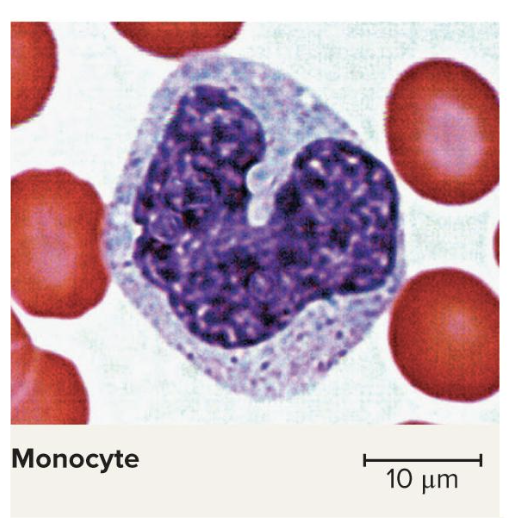
Monocytes
increased number of them in viral infections and inflammation
Very large, 2-3x the diameter of erythrocytes
have a horseshoe or C-shaped nucleus
Leave bloodstream and transform into macrophages
these go around swallowing things that do not belong there
will only swallow if its been covered in antibodies
“Present” antigens to activate other immune cells—antigen-presenting cells (APCs)