Principles of Prescribing in Renal Disease
1/111
Earn XP
Description and Tags
Flashcards covering key vocabulary related to renal disease and principles of prescribing.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
112 Terms
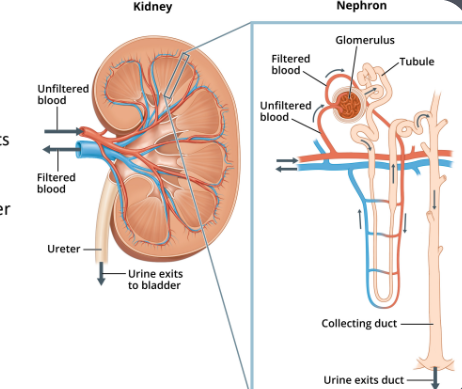
Role of the kidney
Filter blood to remove waste products of metabolism
Keep electrolytes (Na+ and K+) and water content of the body constant (regulates blood volume and plasma osmolarity)
Secrete several essential hormonesand maintain acid-base balance.
Two types of renal impairment
Chronic Kidney Disease (CKD)
Acute Kidney Injury (AKI)
Chronic Kidney Disease (CKD)
Reduction in kidney function or structural damage present for greater than 3 months.
Classically a permanent and progressive disease.
Acute Kidney Injury (AKI)
AN acute drop in kidney function
Chronic Kidney Disease (CKD)
A long-term reduction in kidney function or structural damage present for greater than 3 months.
Acute Kidney Injury (AKI)
An acute drop in kidney function, usually reversible.
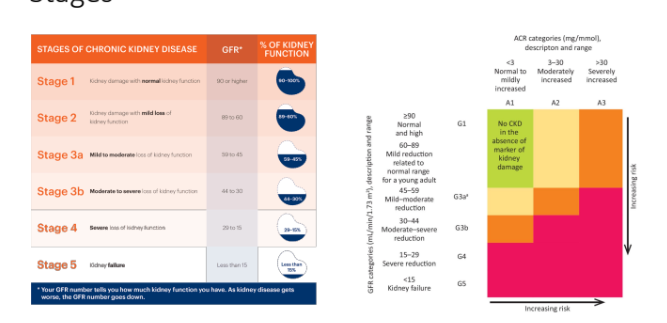
eGFR
Estimated Glomerular Filtration Rate, a measure used to assess kidney function.
Hyperkalaemia
Elevated levels of potassium in the blood, which can cause cardiac arrhythmias.
Proteinuria
The presence of excess proteins in the urine, often a sign of kidney damage.
Renal bone disease (RBD)
A condition associated with chronic kidney disease that affects bone health.
Anaemia
A condition marked by a deficiency of red blood cells or hemoglobin, commonly seen in CKD patients.
Nephrotoxic medications
Drugs that can cause damage to the kidneys.
Obstructive Uropathy
A condition caused by obstruction of urine flow, leading to kidney damage.
Causes of CKD
Diabetes can cause nephropathy. Last stage of nephropathy is kidney failure, end stage renal disease.
High blood pressure
Glomerulonephritis (inflammation of the glomerulus by trauma or infection)
Only significant Acute Kidney Injury
Sustained damage from medications. Can affect the structures of kidney such as afferent arteriole/efferent arteriole/ overall supply of blood to kidney and reabsorption in nephron depends on medicine
Obstruction in kidney leads to backlog of fluid in the actual organ which can lead to problems such as stretching resulting in decrease in function. Blockages are severe and quite difficult to treat but principles are the same
Obesity gives a much higher risk of chronic kidney disease usually due to the workload the kidneys are subjected to and over a long period of time can result in significant damage and other problems
Cardiovascular disease as the heart is responsible for pumping blood around body and kidneys do not work without a constant flow of blood and perfusion and the kidneys rely on a steady blood flow to function properly.
Unlike the liver, which can process waste products from the gastrointestinal (GI) tract without needing a constant blood supply, the kidneys require continuous perfusion (blood flow) and a certain level of pressure (known as back pressure) to filter waste and regulate fluid balance. Without this, the kidneys can't perform their vital functions effectively.
Volume of distribution (Vd)
A pharmacokinetic parameter that describes how a drug is distributed in body fluids and tissues.
Chronic Kidney Disease (CKD): When Do Symptoms Appear?
Early Stages: Usually asymptomatic, often detected through routine screening or blood tests during hospital visits for other conditions.
Later Stages: Symptoms develop, but they are often due to complications of CKD (e.g., fluid retention, electrolyte imbalances, anemia) rather than the kidney disease itself.
Presentation CKD
Pruritus (itching)-(due to buildup of urea)
Loss of appetite-(due to fluid overloaded)
Nausea
Oedema(buildup of fluid)
Muscle cramps
Peripheral neuropathy
Pallor
Hypertension
Most important of CKD
Complications are most important to know because people are going to be presenting without symptoms
Anaemia
Anemia is a condition where there aren’t enough RBCs to carry oxygen efficiently.
If the kidneys are damaged (e.g., in chronic kidney disease), they may not produce enough EPO, leading to anemia of chronic disease
Kidneys release a hormone called erythropoietin and that then stimulates the bone marrow to produce red blood cells
If the kidneys are damaged, the specialized cells responsible for producing erythropoietin (EPO)—called interstitial fibroblasts—can no longer function properly. Erythropoietin (EPO) is the hormone that stimulates the bone marrow to produce red blood cells (RBCs).
When the kidneys fail to produce enough EPO, the bone marrow doesn’t get the necessary stimulation. As a result, fewer red blood cells are produced, and those that are made may be less healthy and less effective at carrying oxygen. This leads to anemia, which causes symptoms like fatigue, weakness, and shortness of breath.
CKD Complication
Anaemia
Renal bone disease (RBD)(weak bones)
Cardiovascular disease(due to poor clearance of waste products and a backlog of fluid)(Incidence of stroke increases significantly as well as MI so there is a big risk)
Peripheral neuropathy(normally associated with the imbalance of electrolytes)(can cause tingling sensations in your hands and feet.)
Okay. Um, this, uh, pins and needles
Dialysis related problems
Cardiovascular disease due to chronic kidney disease
When the kidneys are not functioning properly, they can’t remove excess fluid from the body as efficiently. This leads to fluid buildup (also called fluid overload).
As more fluid accumulates in the bloodstream, the heart has to work harder to pump the extra volume. This increased workload puts the heart under more stress, which can lead to damage over time. The extra strain can contribute to high blood pressure, heart failure, or other cardiovascular issues.
The Link Between Kidneys & Bone Health
The kidneys help regulate important minerals and hormones involved in bone metabolism, such as:
Vitamin D (needed for calcium absorption)
Calcium (essential for strong bones)
Phosphate (must be balanced to prevent bone issues)
Parathyroid Hormone (PTH) (regulates calcium and phosphate levels)
When kidney function declines, they can’t properly regulate these substances, leading to electrolyte imbalances and abnormal absorption of calcium and phosphate in the gut
How Kidney Disease Disrupts Bone Health
Vitamin D Activation is Impaired → Less calcium is absorbed from food.
Low Calcium Levels → The body tries to compensate by increasing parathyroid hormone (PTH), which pulls calcium from the bones.
High Phosphate Levels (due to poor excretion) → Further triggers PTH release, worsening bone loss.
Result: Weakened bones, fractures, and abnormal bone turnover = Renal Bone Disease
CKD Management
Monitor renal function
Suspend nephrotoxic medication if at risk of AKI (acutely)
FBC-rule out anaemia
Bone profile - rule out RBD
Monitor renal function
No compelling evidence to support one calculation over another.
eGFR and CrCl often are similar
eGFR (ml/min/1.73m2)
CrCl (ml/min)
ACR
Monitor renal function
eGFR (ml/min/1.73m2
Estimated glomerular filtration rate
True GFR can be accessed via IV radioisotope
Monitor renal function
CrCl (ml/min)
Creatinine Clearance
Creatinine is a waste product from the normal wear and tear of muscles
Compare to body weight to calculate how well kidneys are working. It is specific to persons size, muscle mass and body weight.
Best one to use if dose needs to be changed or adjusted
Monitor renal function
ACR
Albumin: Creatinine ratio
Test to measure amount of albumin (protein) in the urine vs creatinine
Best one to use for people with CKD
If there is more albumin or a lot of albumin then indicates more significant glomerular damage
Big large molecules are not supposed to be filtered by kidney but they are
eGFR
Can use 1 of 2 different equations
Reports using standardised body surface area (BSA) of 1.73m2
Overestimates renal function in smaller patients
Underestimates renal function in larger patients
DO NOT USE IN – drug dose titrations, elderly patients or
extremes of muscle mass
Good at measuring kidney function
How to work out kidney damage
Use eGFR and creatinine:albumin ratio
Stages of CKD
Principles of management
Identify underlying cause and manage to slow progression
Treat complications
Identify underlying cause and manage to slow progression of disease
Control DM(make sure cbg’s circulating blood glucose doesn’t rise too high)
Control HTN
Treat glomerulonephritis
Treat complications
Metabolic acidosis (too much acdic products)- give Sodium bicarbonate (mops up H+ ions)
Anaemia -Synthetic Erythropoietin(beta) + Iron replacement
RBD - Vitamin D
Dialysis? Renal transplant?
Pharmacological management
Ace inhibitor(first line-nephrotoxic. Long term renal protective)(Inhibit RAS system prevent further damage)
Anti platelet(manage cardiovascular risk)
Statin (manage cardiovascular risk)
SGLt-2(Dapagliflozin-have a mild diuretic effect so reduce pressure on kidneys, capillaries and glomerulus-reduces free circulating glucose)
Serum creatinine blood test
Serum creatinine is a blood test that measures kidney function.
It is not an equation but simply a number obtained from the test.
We then apply this number to an equation (like the eGFR formula) to assess how well the kidneys are functioning
Acute Kidney Injury (AKI)
NICE Guidelines criteria for AKI:
SrCr ↑ of ≥ 26 micromol/L in 48 hours
SrCr ↑ of ≥ 50% in 7 days
Urine output <0.5ml/kg/hour for >6 hours (only applicable where output can be measured, e.g. catheter)
Diagnostic Criteria for AKI
Serum creatinine increases to 1.5 times the patient’s baseline within 7 days.
Urine output drops below 0.5 mL/kg/hour for a prolonged period
AKI
Medications to HOLD:
• DAMN
Diuretics
ACEi/ARB
Metformin
NSAIDs
• Contrast media
Detecting AKI – Often an Incidental Finding
AKI is often discovered incidentally when a patient comes to the hospital for other issues.
As part of routine tests, we check blood results (including creatinine) and urine output to assess kidney function.
An electrocardiogram (ECG) may also be done to check for heart-related complications.
Immediate Response to AKI
Once AKI is identified, the medical team acts quickly to prevent worsening kidney damage.
The first step is to stop any medications that could make the kidney injury worse (such as certain antibiotics, NSAIDs, or contrast dyes).
Contrast media
Makes blood shine bright on a CT scan but it is very nephrotoxic and bad for the kidneys
Serum creatinine
Estimate of a patients kidney function
Not based off BSA, less likely to over/under estimate function
Provides a ‘snapshot’
NB -if a patient is on renal replacement therapy creatine provides no useful information

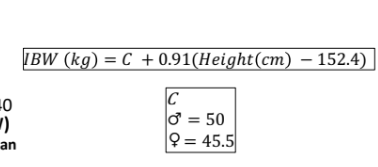
When is creatinine clearance used
For elderly patients or dose titrations or starting new medicines
CrCl Limitations and Warnings
Caution in elderly, body builders, amputees, muscle wasting disorders and vegans
Patients with BMI <18kg/m² or >40 kg/m² use ideal body weight (IBW)
Not accurate in periods of rapidly changing renal function (e.g. AKI) as serum creatinine has a delayed response
Risk Factors
Diabetes (Glucose check image)
Heart conditions (Images of the heart)
Liver disease (Cirrhotic liver image)
Elderly population (Elderly woman walking with a cane)
Medical imaging with contrast (CT scan image)
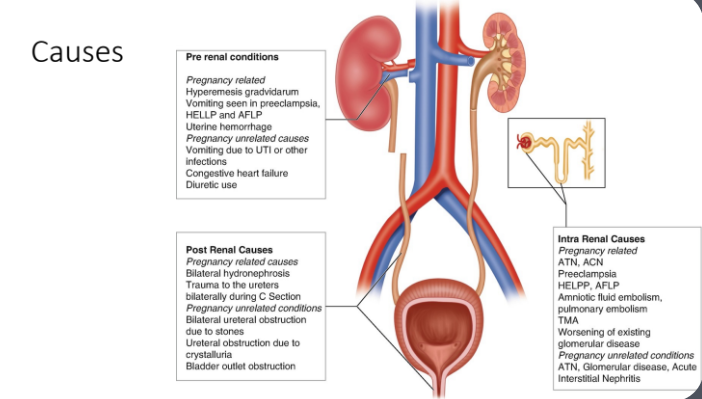
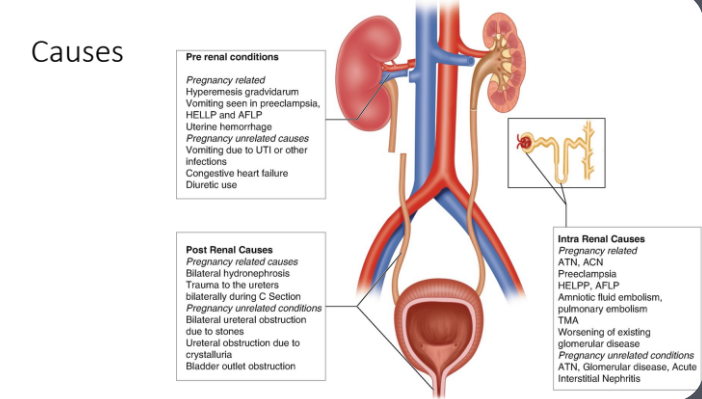
Causes
Diabetes (Glucose check image)
Heart conditions (Images of the heart)
Liver disease (Cirrhotic liver image)
Elderly population (Elderly woman walking with a cane)
Medical imaging with contrast (CT scan image)
Why do we have to understand the causes of AKI?
As it will to dictate the treatment
Pre-renal acute kidney injury (AKI)
Most common type of AKI. It happens when the kidneys don’t get enough blood flow, which means they don’t get enough oxygen and nutrients to function properly.
Causes of pre renal conditions
Diuretic Use
Pregnancy related
Hyperemesis gradvidarum
Vomiting seen in preeclampsia
HELLP and AFLP
Uterine hemorrhage
Pregnancy unrelated causes
Vomiting due UTI or other infections
Congetsive heart failure
Excess Diuretic use
Sepsis
Any sort of shock can include sepsis but also blood loss
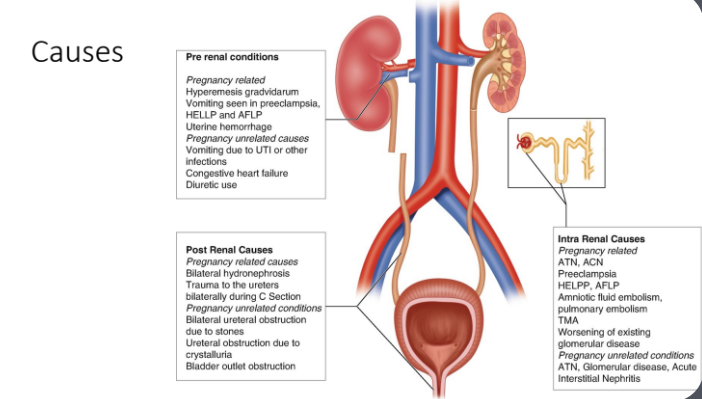
How sepsis leads to pre renal AKI
Instead of just fighting the infection locally, the immune system overreacts and causes widespread inflammation.
One key effect of this response is massive blood vessel dilation (vasodilation). Imagine all the blood vessels suddenly expanding like a balloon. This happens because the body is trying to rush blood to fight the infection.
Blood pressure drops drastically → The heart can’t push blood effectively.
The kidneys don’t get enough blood flow → Since they depend on a steady supply of blood to function, this leads to pre-renal AKI.
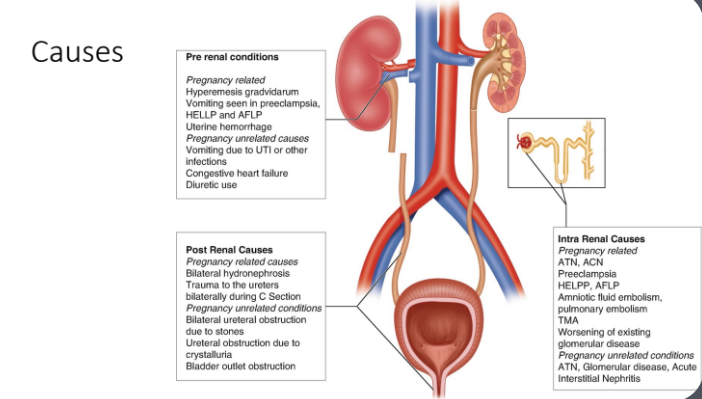
Intrarenal causes
Problem with the kidney normally associated with glomerulitis
Glomerulitis is associated with rapid decline of renal function often associated with blood and protein in the urine, because the filter of the glomerular is so damaged that things are leaking through.
Tumour lysis syndrome-when cancer is treated very aggressively and lots of cells are broken down and it overwhelms the kidney. Part of the cells are kind of attacked and die are the ones in the kidney which can cause this intrarenal AKI.
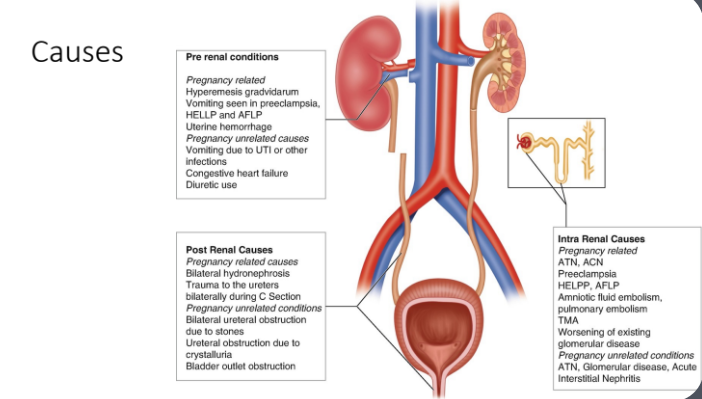
Post renal causes
Anything past the kidney that can cause problems to it
Main one is obstruction
Kidney stones,
Benign Prostatic Hyperplasia (BPH)-growth of prostrate that can be some form of tumour. can block urine from leaving the bladder. When this happens:
Urine backs up into the bladder.
If the blockage is severe enough, it can push urine back up into the kidneys (hydronephrosis).
This pressure buildup damages the kidneys and can lead to post-renal AKI (kidney injury due to obstruction).
Teatment of AKI summary
Pre-renal-need fluids
Intrarenal-Specific treatment to the cause
Postrenal-Obstruction removal mainly through surgery
Temporary measure in emergency use catheter
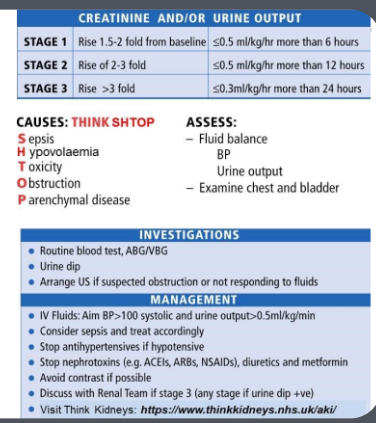
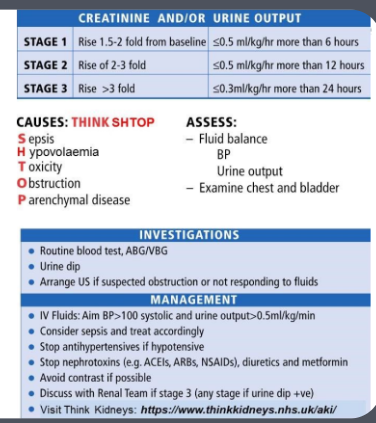
What are the three stages of AKI based on creatinine and urine output?
Stage 1: Creatinine rise 1.5-2 fold or urine output ≤0.5 mL/kg/hr for >6 hours
Stage 2: Creatinine rise 2-3 fold or urine output ≤0.5 mL/kg/hr for >12 hours
Stage 3: Creatinine rise >3 fold or urine output ≤0.3 mL/kg/hr for >24 hours
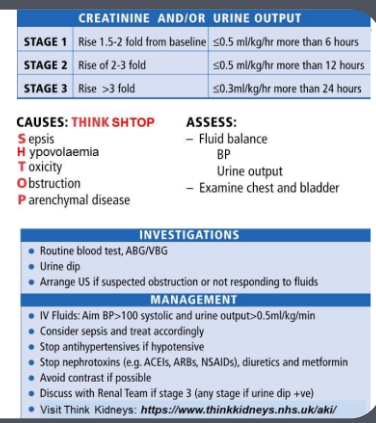
What does the acronym “THINK SHOP” stand for in AKI causes?
Sepsis
Hypovolaemia
Toxicity
Obstruction
Parenchymal disease
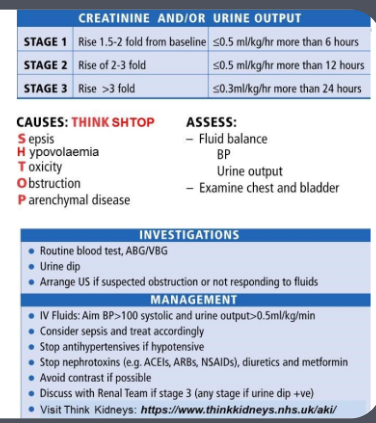
What key assessments should be done in AKI?
Fluid balance
Blood pressure (BP)
Urine output
Examine chest and bladder
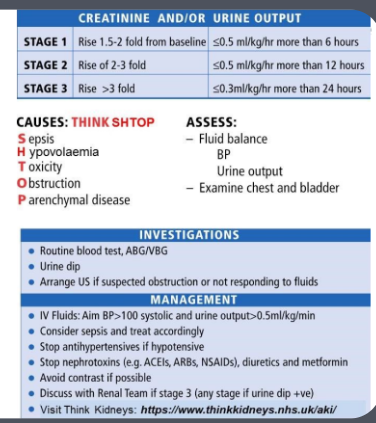
What are important investigations in AKI?
Routine blood tests, ABG/VBG
Urine dip
Imaging if obstruction is suspected or the patient is not responding to fluids
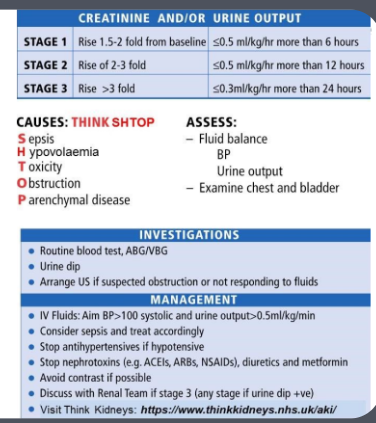
What is the initial management approach for AKI?
IV fluids to maintain BP >100 systolic and urine output >0.5 mL/kg/min
Consider sepsis and treat accordingly
Stop antihypertensives if hypotensive
Stop nephrotoxins (ACEIs, ARBs, NSAIDs, diuretics, metformin)
Avoid contrast if possible
Discuss with the renal team if Stage 3 AKI (or earlier if needed)
Why should nephrotoxic drugs and antihypertensives be stopped in AKI?
Nephrotoxic drugs (e.g., NSAIDs, ACEIs, ARBs) can worsen kidney function
Antihypertensives can further lower blood pressure, reducing kidney perfusion and worsening AKI
Management
Correct underlying cause
use fluid to increase blood flow to the kidneys to increase perfusion-use crystalloid IV fluid
Pre-renal cause
Provide IVT resuscitation
Post-renal cause
Relieve obstruction – insert catheter?
Hold nephrotoxic
Types of IV fluid
Crystalloids
Colloids
Types of IV fluid in pre renal AKI management
Crystalloids (Preferred for Pre-Renal AKI)
What are they? Water + electrolytes (e.g., sodium, chloride)
Examples: Normal saline (0.9% NaCl), Ringer’s lactate
Why do we use them? They increase blood volume without pulling fluid from other parts of the body.
Colloids (Not Used in Pre-Renal AKI)
What are they? Large protein or starch molecules (e.g., albumin, gelatin-based fluids)
Why not use them? They work by pulling water from tissues into the bloodstream, but in pre-renal AKI, we don’t want to shift fluids around—we just need to add more fluid to restore kidney perfusion.
Complications-Hyperkalaemia(High potassium)
Normal range → 3.6 – 5.2 mmol/L (over 6 medical ememrgency)
Results in potentially fatal cardiac arrhythmias (ventricular fibrillation)
Perform ECG
Remember medications can cause HYPERkalaemia along side AKI
What potassium is important for the heart?
Cardioprotective
Potassium (K⁺) is essential for heart function because it helps control the electrical signals that keep your heart beating normally.
What happens when potassium is too high?
Danger: Too much potassium disrupts the heart’s electrical activity.
Risk: Can cause ventricular tachycardia (VT), which is a life-threatening, fast heart rhythm that can lead to sudden cardiac death.
What Happens When Potassium is Too Low (Hypokalemia)?
Danger: Not enough potassium makes the heart more unstable.
Risk: Can cause supraventricular tachycardia (SVT) (a fast, irregular heartbeat from the upper chambers of the heart). Severe cases can lead to cardiac arrest
Hyperkalaemia Treatment
Nebulised salbutamol((a side effect of this asthma drug is lowering K⁺) → Also pushes K⁺ into cells)
IV fluids
PO calcium resonium (gets rid of excess potassium from the body.)((a cation exchange resin) swaps calcium for potassium, helping remove potassium through the gut.)
IV calcium gluconate(protects myocardium by stabilising cell membranes, prevent arrhythmias. Does not lower potassium)
IV insulin((given with glucose to prevent hypoglycemia) → Pushes K⁺ into cells.)
IV glucose
(Glucose+insulin+salbutamol:Moves potassium out of the blood and into cells, lowering the immediate risk.)
Complications
Fluid overload
Metabolic acidosis(excess acid, leads to lower blood pH)
Uraemia(kidneys fail to remove waste products and excess fluid) (results in encephalopathy(swelling in brain))
Fluid overload
Too much IV fluid
Pulmonary Edema – Fluid backs up into the lungs → Shortness of breath
Peripheral Edema – Swollen legs and arms
Hypertension – Increased blood pressure due to excess fluid
Heart Strain – If the heart can’t pump effectively, it may worsen heart failure
How does CKD and AKI affect drug absorption?
Impaired gut wall function and malabsorption can occur in kidney disease, altering drug absorption.
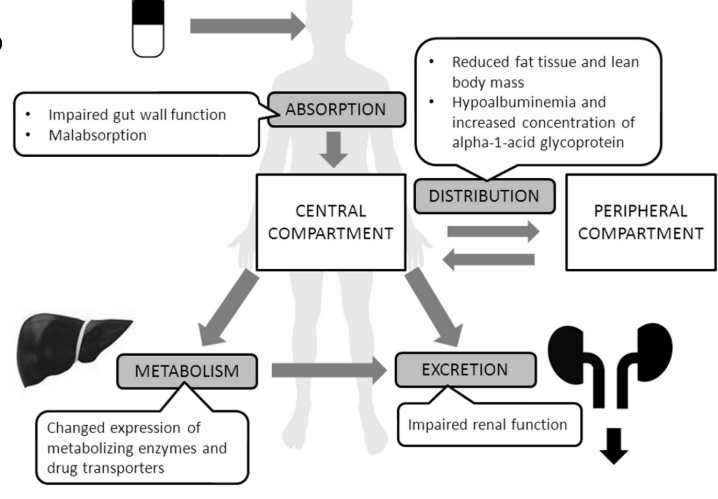
Why does drug distribution change in CKD and AKI?
Reduced fat tissue, lean body mass, hypoalbuminemia, and increased alpha-1-acid glycoprotein can alter drug binding and distribution.
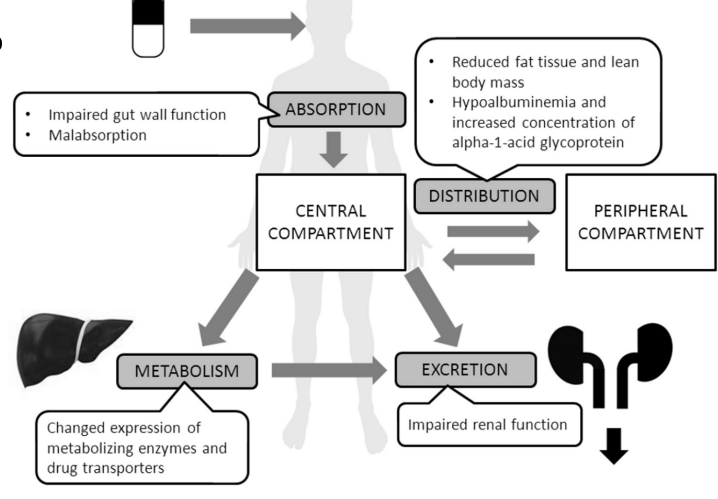
How does kidney disease impact drug metabolism?
CKD and AKI can lead to changes in metabolizing enzymes and drug transporters, affecting drug breakdown in the liver
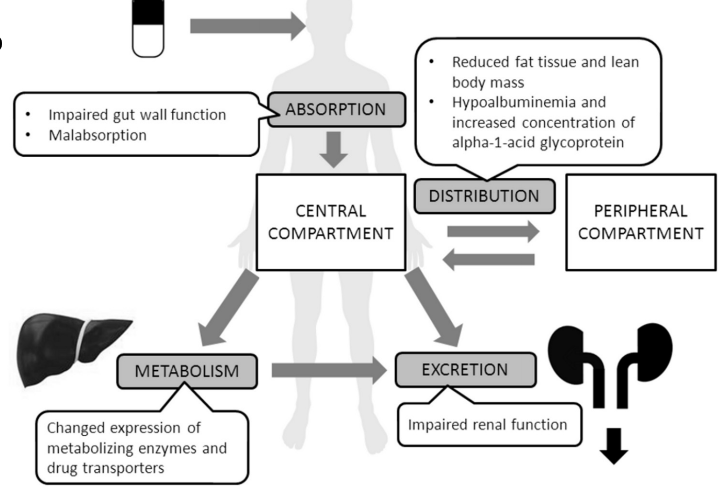
Why is drug excretion impaired in CKD and AKI?
Impaired renal function reduces the elimination of drugs, leading to accumulation and potential toxicity.
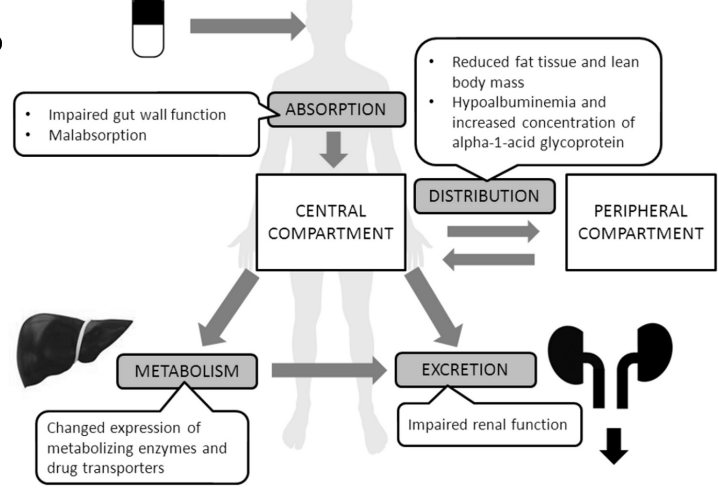
What are the clinical implications of altered pharmacokinetics in CKD and AKI?
Dose adjustments and careful monitoring are needed to avoid drug toxicity or inefficacy
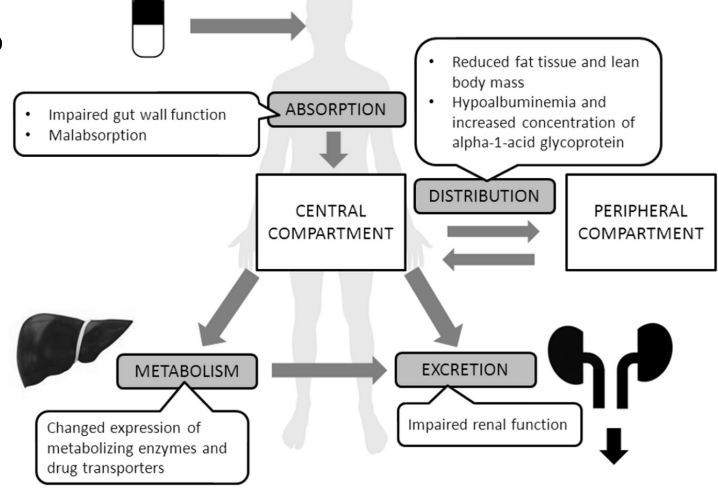
Pharmacokinetics in renal absorption
Absorption
May be reduced due to uraemia causing nausea, vomiting, diarrhoea
Patient may be taking phosphate binders
May be affected by the increase in gastric pH
Pharmacokinetics in renal absorption
Distribution
Drug-Plasma protein binding reduced-increased free (active drug
Uraemia increases permeability of BBB
Volume of distribution may be altered by changes in hydration state of patient (e.g. increased Vd in oedema so need higher doses)
Pharmacokinetics in renal impairment
Metabolism
Slower in CKD leading to increased ADRs
Vitamin D-need to use calcitriol or alfacalcidol
Insulin-may need dose reduction
Pharmacokinetics in renal impairment
Elimination
Glomerular filtration, renal tubular secretion and reabsorption all reduced
Accumulation of drug/active metabolites highly likely
Increased ADRs, toxicity
E.g. pethidine
Morphine and its metabolites
Morphine is metabolized into two active metabolites: morphine-6-glucuronide and morphine-3-glucuronide.
Both of these metabolites are excreted by the kidneys. If a person has kidney issues (like chronic kidney disease or dialysis), these metabolites may accumulate in the body, increasing the risk of toxicity. This is because the active metabolites keep binding to mu-opioid receptors and cause the analgesic effects and side effects.
Oxycodone:
Oxycodone is also metabolized, but its primary active metabolite is oxymorphone, which is produced in the liver.
After this, oxycodone undergoes a further metabolism step, producing an inactive metabolite, which is then excreted from the body.
Since the inactive metabolite doesn’t bind to the opioid receptors, it doesn't cause the same side effects or risk of toxicity, even if it accumulates in the body.
Why Oxycodone is Preferred in Renal Conditions:
In patients with kidney problems, oxycodone is preferred over morphine. This is because its inactive metabolites are not harmful or active in the body, reducing the risk of toxicity, unlike morphine which has active metabolites that can accumulate and cause adverse effects.
Drug administration
Many drugs are renally excreted
Riak of accumulation
Increased drug T1/2
Drugs may have reduced efficacy
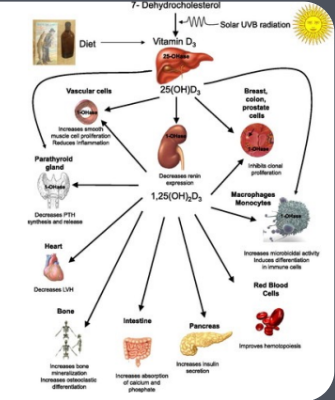
What role does vitamin D play in bone health?
Vitamin D is essential for calcium absorption, which is crucial for bone strength and turnover.
How do the kidneys affect vitamin D metabolism?
The kidneys convert vitamin D into its active form, which is necessary for calcium absorption.
Why are people with kidney disease at risk of bone problems?
Their kidneys can't activate vitamin D, leading to poor calcium absorption and weaker bones.
Why doesn’t standard vitamin D supplementation help kidney disease patients?
Their kidneys cannot metabolize standard vitamin D into its active form
What is the alternative treatment for vitamin D deficiency in kidney disease?
Pre-activated vitamin D, such as alfacalcidol, which does not require kidney metabolism
Nitrofurantoin
Antibiotic to treat UTIs
Cannot be given to patients with impaired renal function
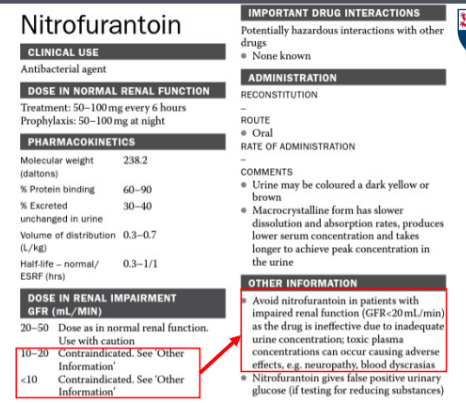
Prescribing approaches
Increase dosing interval(instead once 3x a day give it once 2x a day)(allows more time for excretion to happen and less chance to accumulate)
Decrease dose
Combination of dose reduction and increased interval
Review drug choice
DOACs in renal disease
• Has many indications – ensure you know the indication you are
treating
• E.g. Apixaban prophylaxis of stroke in AF
5mg BD
UNLESS 2 of the following 3 criteria are met:
>80 years old
<60kg or SrCr
<133micromol/L
• This rule does NOT apply in treatment on DVT/PE
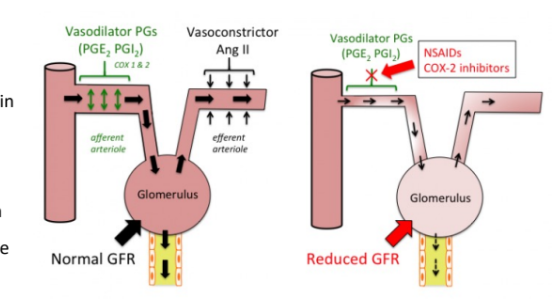
NSAIDs in renal disease
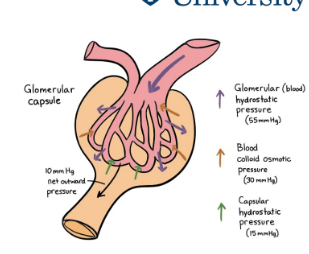
Avoid if possible (stop vasodilation of afferent arteriole which leads to reduction of blood flow to the glomerulus
• Prostaglandin synthesis inhibited, effecting renal perfusion –especially in those with renal disease
NSAIDs work by inhibiting prostaglandins, which normally help maintain blood flow to the kidneys. When prostaglandins are blocked, the blood vessels supplying the glomerulus constrict, leading to reduced blood flow. This lowers the glomerular filtration rate (GFR), which measures how well the kidneys filter waste from the blood.
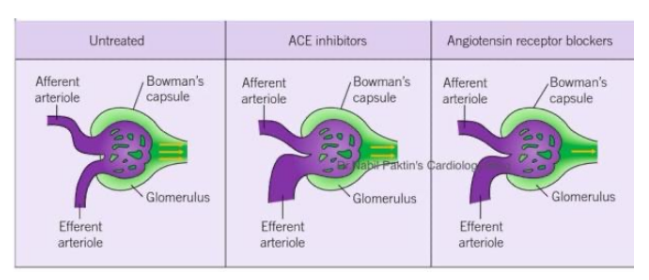
ACEi/ARBs in renal disease
ACE inhibitors cause dilation of the efferent arteriole (the vessel carrying blood out). This reduces the pressure within the glomerulus, which lowers the hydrostatic pressure needed for filtration. As a result, the glomerular filtration rate (GFR) decreases.
What are common signs of acute kidney injury (AKI)?
Sudden rise in creatinine, low eGFR, reduced urine output, electrolyte imbalances (e.g., hyperkalemia)
What nephrotoxic medications should be reviewed in patients with renal impairment?
ACE inhibitors (ACEi), NSAIDs, aminoglycosides, contrast agents, and certain diuretics.
How should antibiotic dosing be adjusted in renal impairment?
Many antibiotics (e.g., Co-amoxiclav, aminoglycosides, vancomycin) require dose adjustment or interval extension based on eGFR or CrCl.
What alternative pain management is recommended for patients with renal impairment?
Paracetamol is preferred over NSAIDs due to the risk of further kidney damage.
What medications should be adjusted for anticoagulation in renal impairment?
DOACs (e.g., Rivaroxaban, Apixaban) require dose adjustment based on CrCl; Warfarin may be an alternative in severe CKD
Why should ACE inhibitors be used with caution in renal impairment?
ACE inhibitors dilate the efferent arteriole, reducing glomerular pressure and potentially lowering GFR further
What is the recommended antihypertensive alternative to ACE inhibitors in patients with renal impairment?
Calcium channel blockers (CCBs) like amlodipine are often preferred.