4.1) electrical stimulation for pain modulation (not finished)
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
59 Terms
direct current
has charge, true anode, and cathode
Continuously used for iontophoresis
alternating current
has a waveform
no IPI
has frequency
continuous or interrupted
pulsed current
has a waveform
is mono or biphasic
has pulse/phase duration
has IPI
duration * amplitude =
pulse charge
steps of peripheral nerve activation
alpha, beta, delta, denervated muscle
(motor, sensory, autonomic) (myelinated --> unmyelinated)
strength-duration curve
subsensory, sensory, motor, noxious
carrier frequency modulation used only for
burst modulated AC currents
- russian waveforms
- interferential waveforms
burst frequency
number of bursts per second
transcutaneous electrical nerve stimulation (TENS)
complimentary treatment - still need to address impairments and function
can be used for acute and chronic pain conditions
TENS is the common name for
stim for pain modulation
gate theory
stimulation of large diameter afferent inhibits the nociceptor responses in the dorsal horn
ex- like grabbing hand and rubbing it after hitting it on something
main mechanisms
activation of peripheral opioid receptors
activation of CNS opioid receptors
Stimulation and neuropathways
stim may change endogenous neurotransmitters and affect plasticity of NMDA pathways
fiber activation at sensory level of TENS goal
is three or more times sensory threshold
sensory threshold is when
the pt first starts feeling a little tingle
motor threshold is when
the pt first feels a small movement
fiber activation at motor level of TENS
activate motor and sensory - benefits of contraction
more than 2 times motor threshold
high frequency of TENS
more than 50 pps
high frequency mechanisms
peripheral, SC, and supraspinal effects
- activation of delta-opioid
- GABA
low frequency of TENS
less than 10 pps
low frequency mechanisms
peripheral, SC, and supraspinal effects
- activation of mu-opioid
- GABA
if someone is taking opioids
low frequency is not gonna have an effect because the medication is already attached to the mu receptors
different frequencies of TENS activate
different neurotransmitters to decrease sensitization
sensory treatment duration
to fit intervention goal
sensory duration of analgesia (the effect)
length of treatment plus some
motor treatment duration
30-40 min - low frequency
10-15 min - high frequency
motor duration of analgesia
hours after treatment session
noxious/painful treatment duration
10-20 min
noxious/painful duration of analgesia
hours after treatment session
duration of analgesia definition
more energy in = longer duration of analgesia
sensory dosing intensity/amplitude
3 times sensory threshold
strong but comfortable
motor dosing intensity/amplitude
2 times motor threshold
noxious/painful dosing intensity/amplitude
sharp, prickly, stringing pain sensation
more than 3 times sensory and more than 2 times motor thresholds
when to choose between using sensory, motor, noxious
tissue type
patient presentation (high/low irritability)
patient preference
adaptation occurs with
constant sensory input
adaptation
reduced perception of a sensory level stimulus when experienced for a long period of time (aka accommodation)
preventing tolerance is critical for
full effectiveness
adaptation is minimized by
modulating current
- pulse/phase duration
- pulse/phase amplitude
- frequency
- combined (duration and amplitude)
interferential current is what type of current
specific type of current used primary for pain modulation
interferential current requires
a special machine that delivers IF current
Interferential Current
interference of currents (AC) from 2 channels each with different carrier frequencies
the carrier frequencies for IF current are usually
different by approx 100 Hz
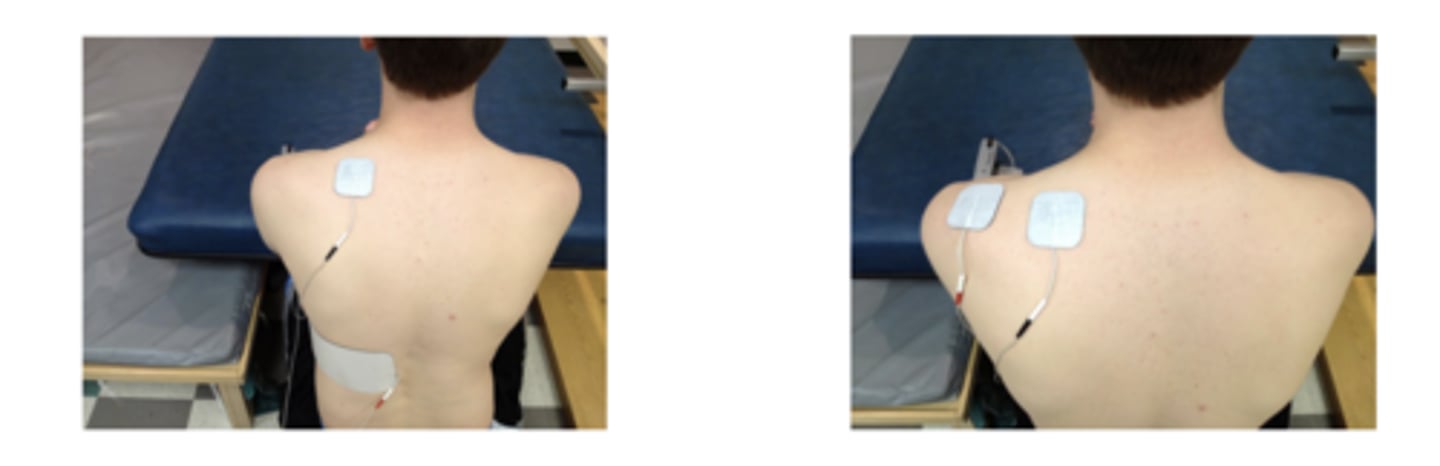
options for electrode placement
site of pain
anatomically or physiologically related site (dermatome, spinal nerve)
other remote sites
must activate large diameter afferents
goal for current flow
to get current field to pass through affected deep tissues
if not getting the response you want change
- electrode placement
- electrode configuration
contraindications for TENS
- other electronic devices
- low back or abdomen of pregnant women
- regions of known or suspected malignancy
- recent radiated tissue
- near/over eyes
- anterior neck
- damaged skin
precautions for TENS
- sensory impairments
- chest wall
- active epiphysis
- cog/communication impairments
- regenerating nerves
when assessing outcome of TENS treatment what do we look for
pain
skin
did it help? did it make things easier?
when documenting use of TENS
mode of TENS
waveform type
waveform parameters
if IF current
level of stimulation intensity (mA)
electrode (type, shape, size, and #, placement/location)
integrity of skin before and after
patient position
treatment duration
What is the configuration of channels used in sensory-level TENS for knee OA?
Two channels with electric fields criss-crossing the joint.
What should be avoided during sensory-level TENS for knee OA?
Contractions of the quadriceps and anterior compartment muscles.
Sensory or noxious TENS: subacromial pain
- electrodes placed just anterior and posterior to acromion
- promotes deeper penetration of current than anterior placement of electrodes
- will get some muscle activation - even at 3 times sensory threshold
goal for sensory or noxious TENS subacromial pain
to provide analgesia to subarcomial bursa to supraspinatus
motor level stimulation is usually used for what type of pain
non-acute pain (low irritability)
possible mechanisms for analgesia with motor level stimulation
- blocks signal peripherally from going to brain
- endogenous opioid mechanism
- increased blood flow to area of injury
chronic active trigger point: levator scapula/upper trapezius
stimulation will cause some head/neck rotation
can also place electrode over posterior cervical musculature
2 pps, 400 microsecs. 1 min on/1 min off, 10 min duration
when doing noxious TENS where should we place elctrode?
tendon, ligament, fat pad pain - should be a palpable structure
noxious level stimulation uses perception of pain to
inhibit pain
parameters the elicit noxious response
long pulse duration and high amplitude