1 Radiation Physics and Biology
1/119
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
120 Terms
what is energy in transit called?
radiation
what is the removal of electrons from an atom resulting in the formation of an ‘ion pair’ called?
ionization
what is the the attractive force that keeps electrons bound to the nucleus in their orbitals?
electron binding energy
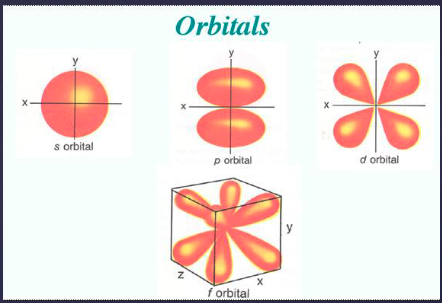
describe the structure of atoms
orbital electrons: S, P, D, F, G, H
what is the relationship between Z # and binding energy?
higher Z # = higher binding energy
what are characteristics of neutrons?
no charge (neutral)
mass is approx same as proton (1.68 × 10^-24 g)
what is Z-number?
# of protons (aka atomic #)
in a neutral atom, # of protons = # of electrons
determines the identity of an element
what is A-number?
# of protons + neutrons (aka atomic mass #)
movement of energy through space as a combination of electric and magnetic fields is known as…?
electromagnetic radiation (gamma rays, xrays, UV, visible light, infrared, microwaves, radiowaves)
what does the quantum theory suggest?
energy transfer in the form of “bundles” (or packets) of energy called photons (or “quanta”) that move at the speed of light and w a specific amount of energy
what are some important properties of x-rays?
no mass
no electric charge
travel in waves
travel w specific frequency (speed of light)
highly penetrating
travel in straight lines (diverging from central focus)
able to ionize
range of wavelengths (0.1A to 0.5A)
xrays are able to ionize. what does this mean?
affect photographic film
able to produce biological/chemical changes
what are the 2 mechanisms of X-ray production?
Bremsstrahlung (electron to nucleus interaction)
characteristic radiation (electron to electron interaction)
of the 2 mechanisms of x-ray production, which is the primary source of radiation generated by an x-ray tube?
Bremsstrahlung mechanism
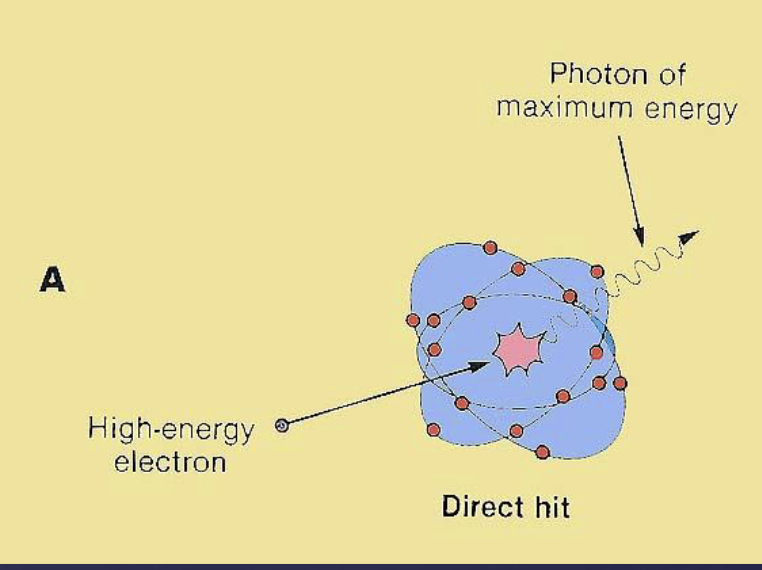
describe how the Bremsstrahlung mechanism produces x-ray.
X rays are produced when high velocity electrons are suddenly decelerated when they pass close to or directly hits the nuclei of high Z # absorbing material.
direct hit → entire kinetic energy of electron gets transferred to xray photon → high/max energy xray photon
indirect/near miss → only part of kinetic energy gets transferred → lower energy xray photon is produced
what types of xray photons are produced via bremsstrahlung mechanis?
photons w varying energy levels (within a specific range)
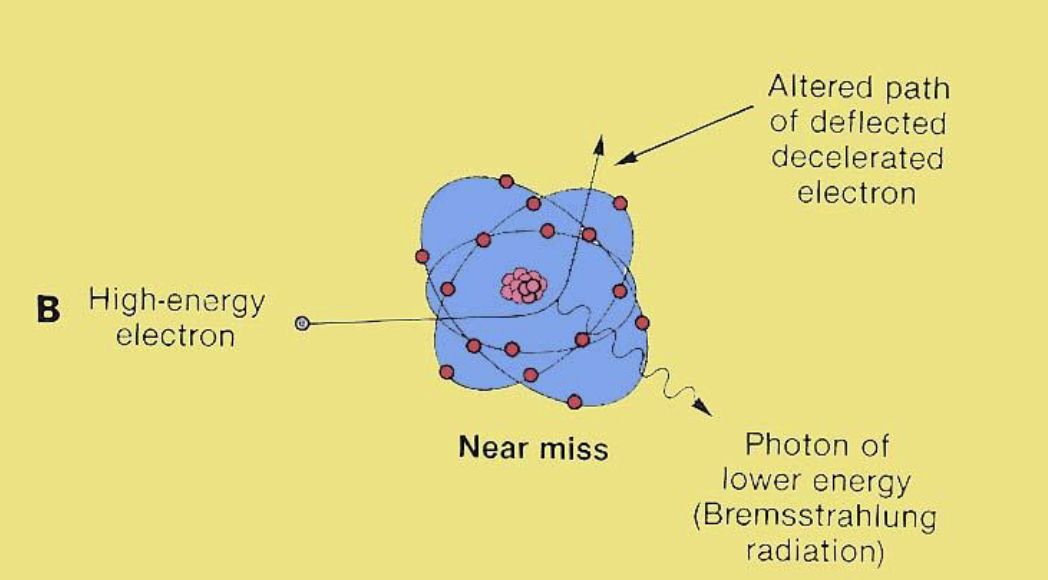
describe how the characteristic mechanism produces x-ray.
high velocity electrons interact with an inner shell electron and knocks it out of the orbit
This vacancy( gap) is filled out by an outer shell electron.
The difference in the energy levels is released and an x-ray photon
what types of xray photons are produced via characteristic mechanism?
photons with specific energy level that is characteristic of the atom produced
of the 2 mechanisms of x-ray production, which contributes a small fraction of photons in the beam?
characteristic mechanism
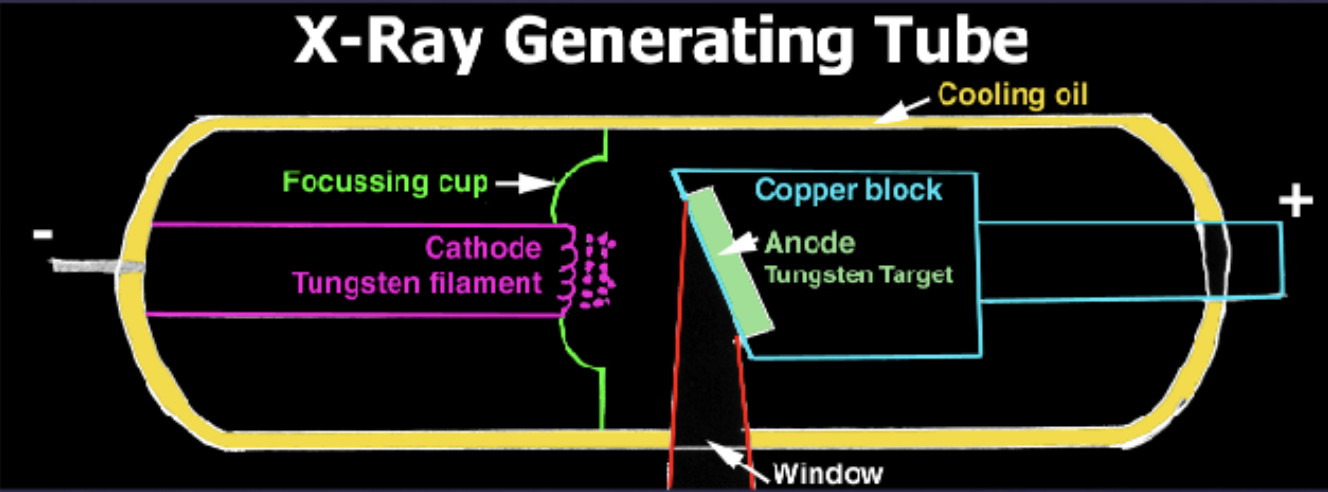
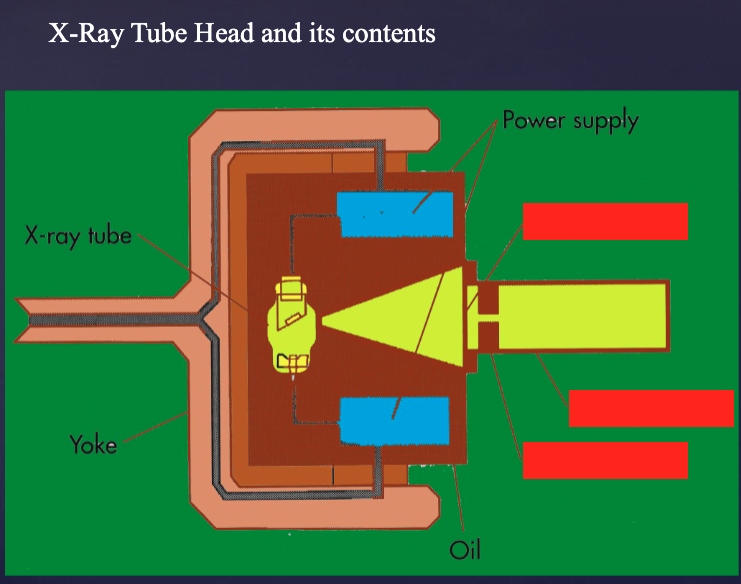
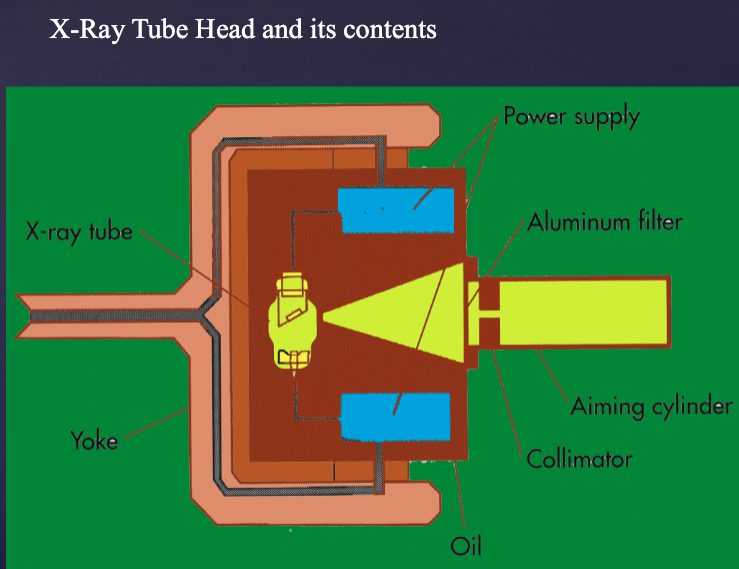
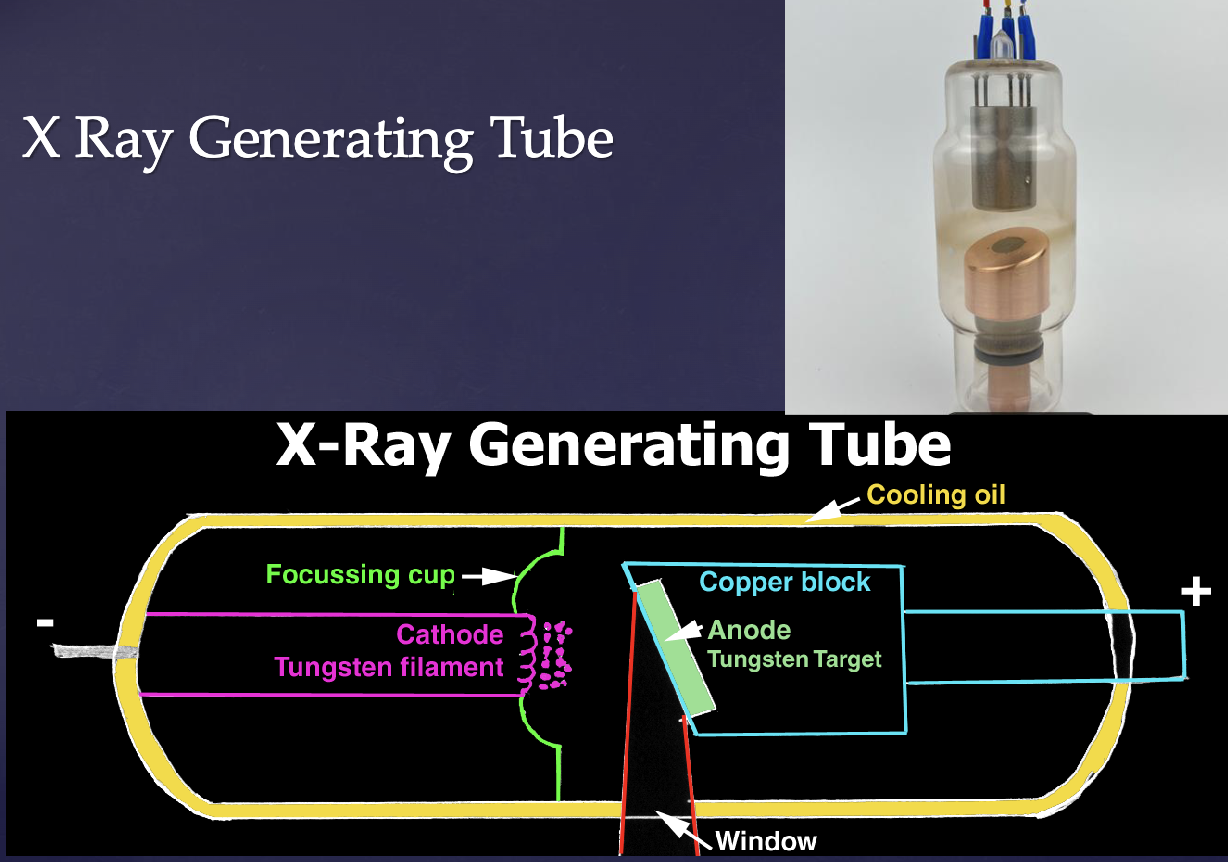
what are the key components of xray generating tubes?
electron source (cathode)
concentration of electrons (focussing cup)
mechanism to accelerate electrons (potential difference or tube voltage kVp)
suitable target to stop electrons (anode)
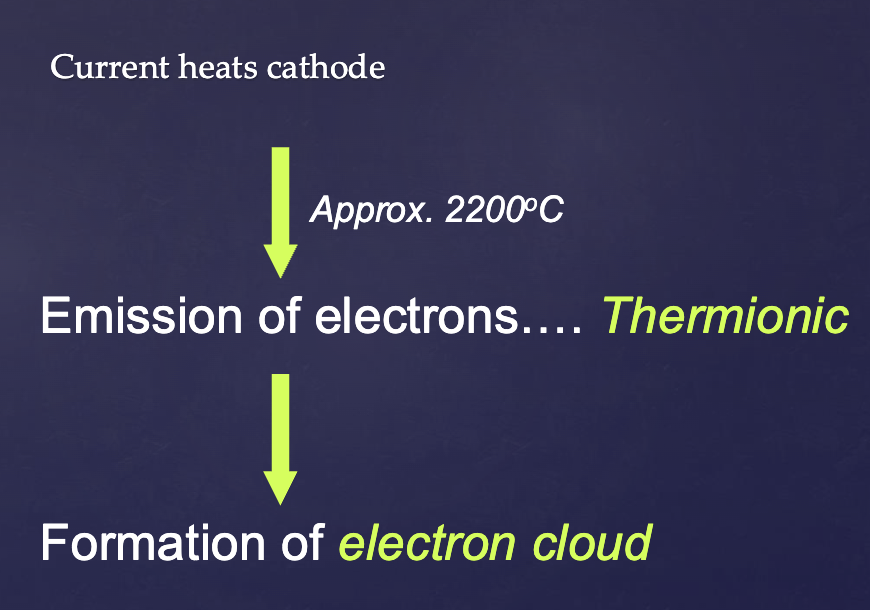
describe the process of thermionic emission.
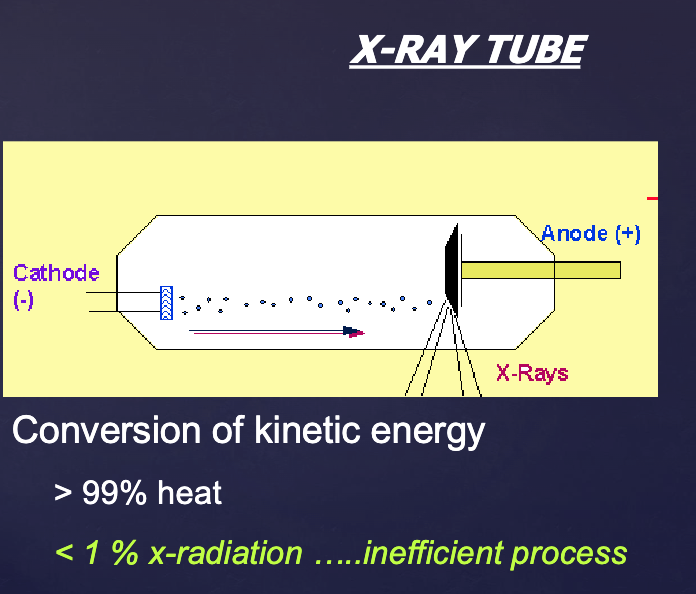
why is conversion of kinetic energy in a xray tube an inefficient process?
>99% is lost as heat
only <1% becomes xradiation
what are the 2 components that make up the anode of a xray tube ?
tungsten target
copper stem (good thermal conductor)
why is tungsten a good anode target?
high atomic #
high melting point
low vapor pressure
high degree of thermal conductivity

what factors control the xray beam? (6)
tube voltage (kVp)
exposure time (S)
tube current (mA)
filtration
collimation
distance of xray tube from pt/receptor
what factor of the xray beam controls the acceleration of electrons from cathode to anode?
Tube Voltage (kVp)
what does filtration control in an xray beam?
removes lower energy xray photons
what does collimation control in an xray beam?
adjusts shape/size of xray beam
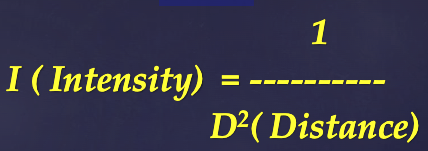
how does distance of xray tube from patient/receptor affect xray beam?
controls intensity of xray beam
how does tube current (mA) affect xray beams?
controls heating of cathode to produce electrons
how does exposure time (S) affect xray beams?
controls heating of cathode to produce electrons
what 2 factors control heating of the cathode to produce electrons in xray beam?
exposure time (S) and tube current (mA)
in an x-ray generating tube, what material makes up the anode vs cathode?
cathode → tungsten filament
anode (tungsten targe in a copper block)
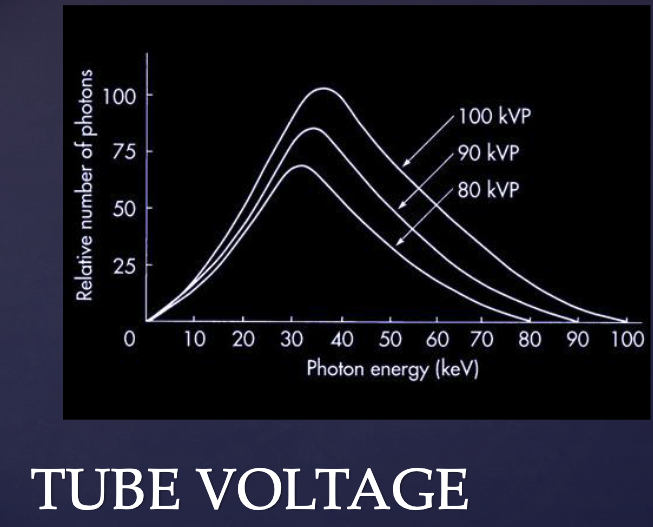
what does this graph tell us about what happens when kVP of a beam is increased?
increased kVP →
total # of photons increase
max energy of beam increase
mean energy of beam increase
Movement of energy through space as a combination of electric and magnetic fields is referred to as…?
electromagnetic radiation (gamme rays, x-rays, ultraviolet, visible light, infrared, microwaves, radio waves)
what category of organs and cells are MOST sensitive to radiation (highest radiosensitivity)?
Bone marrow (lymphoblasts, lymphocytes, plasma cells, erythroblasts)
intestines (epithelial stem cells)
oral mucous membrane (basal cells )
Spermatogenic cells
what cell types are an exception to the law of Bergonie and Tribondeau?
small lymphocytes & oocytes (mature in differentiation yet sensitive to radiation)
what are the teratogenic effects (deterministic, safe doses) of radiation on an embryo/fetus?
intrauterine death (1st week of pregnancy)
intra-uterine growth retardation
congenital malformations
developmental abnormalities
what are the stochastic effects (no safe dose) of radiation on an embryo/fetus?
cancer in childhood
what factors influence the probability of radiation effecting an embryo?
dose to embryo/fetus
stage of gestation at time of exposure
A dose threshold of ______ to the fetus is required to produce x-ray induced birth defects
100-250 mSv
This is orders of magnitude above the fetal dose from dental radiographs (<.01 mSv)
what are possible radiogenic effects at a gestational age of 0-9 days (preimplantation stage) ?
all or none
what are possible radiogenic effects at a gestational age of 10 days - 6 weeks (organogensis stage) ?
congenital anomalies, growth retardation
what are possible radiogenic effects at a gestational age of 6-40 weeks (fetal stage) ?
growth retardation, microcephaly, mental retardation
t/f: Risk of Stochastic effects (childhood cancer/ genetic mutation) occur throughout pregnancy
true
acute radiation syndromes occur usuaully as a result of…?
whole body irradiation (accidental, nuclear plant disasters, etc.) → never happens any other way
acute radiation syndromes are ___-dependent.
dose
Prodromal symptoms (1-2 Gy)
Hematopoietic syndrome (2-7Gy)
Gastrointestinal syndrome(7-15Gy)
Central nervous system syndrome (50Gy)
acute radiation syndrome: prodromal symptoms
dose?
time of onset?
manifestation?
dose: 1-2 Gy
time of onset: minutes-hours after exposure
manifestation: anorexia, nausea, vomiting, fatigue
acute radiation syndrome: hematopoietic symptoms
dose?
time of onset?
organs affected?
manifestation?
dose: 2-7 Gy
time of onset: days to months
organs affected: hematopoietic stem cells in bone marrow and spleen
manifestation: infection, hemorrhage, anemia (death 10-30 days)
acute radiation syndrome: gastrointestinal symptoms
dose?
time of onset?
organs affected?
manifestation?
death?
dose: 7-15 Gy
time of onset: few weeks to months
organs affected: small intestine
manifestation: nausea, vomiting, diarrhea, electrolyte imbalance, circualtory collapse
death 3-10 days
acute radiation syndrome: cardiovascular and CNS symptoms
dose?
time of onset?
organs affected?
manifestation?
dose: 50 Gy
time of onset: death in 1-2 days
organs affected: brain
manifestation: lethargy, tremors, convulsions, ataxia, coma
radiation therapy in the oral cavity is used to target malignant oral lesions that are radiosensitive. what is the total dose used?
64-70 Gy in 6-7 weeks
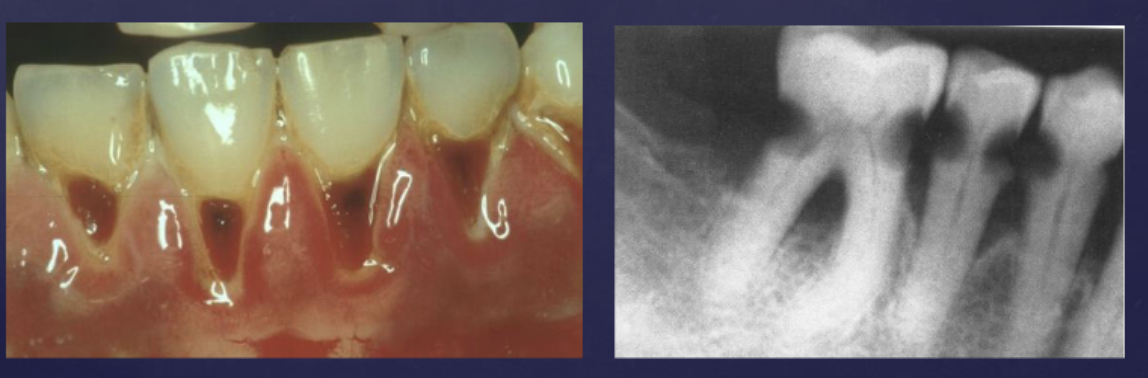
how does radiation affect salivary glands?
radiation caries
reduced secretion (xerostomia)
pH altered (decalcification of enamel)
how does radiation affect taste buds?
decrease taste acquity
recovery to almost normal 60-120 days post irradiation
how does radiation affect teeth? (pre-calcification vs post-calcification vs post-eruption)
prior to calcification → tooth bud destroyed
post calcification → malformations, arrested growth
erupted teeth → radioresistant
severity is dose dependent
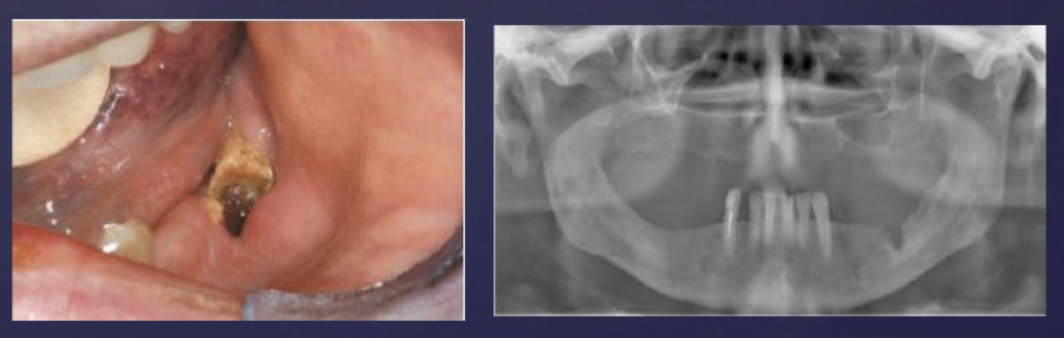
how does radiation affect bone?
osteoradionecrosis
damage to vasculature of periosteum, cortical bone
destruction of osteoblasts
how does radiation affect oral mucous membrane?
-Desquamation
-Inflammation/pain
-white/yellow pseudomembrane
-Secondary Fungal Infections
-Long term: atrophic, thin, avascular mucosa
-healing –2months after
what is the Removal of low energy photons from the x ray beam while allowing passage of high energy photons called?
filtration
why is filtration important?
Low energy photons do not contribute to radiograph formation and contributes to patient risk
Filtration reduces intensity of x-ray beam (hence requires compensatory increase in exposure time)
what is the total filtration in xray tube?
inherent filtration
glass and oil
added filtration (by manufacturer)
aluminum disk
total filtration = aluminum + inherent
by law, when operating a tube at 50-70 kVp, ___ mm aluminum equivalent of total filtration is required. what about at above 70 kVp?
50-70 kVp = 1.5 mm aluminum equivalent
above 70 kVp = 2.5 mm aluminum equivalent
when filtration is increased, how is exposure time and pt skin exposure affected?
increase in exposure time
decrease in pt skin exposure
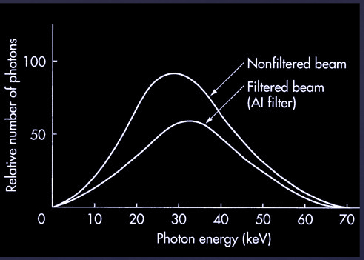
how does filtration affect the beam?
decreased number of photons
increased mean energy of photons
same max energy of photons
Although filtration requires an increase in exposure time up to % to compensate for loss of intensity, it reduces patient skin exposure by as much as %
50%
80%
what is a useful way to characterize the penetrating quality (mean energy) of an x ray beam?
Half Value layer (HVL)
HVL is defined as the thickness of an absorber that reduces the quantity of photons by …?
1/2
as average energy of beam (kVp) increases, what happens to HVL?
increases
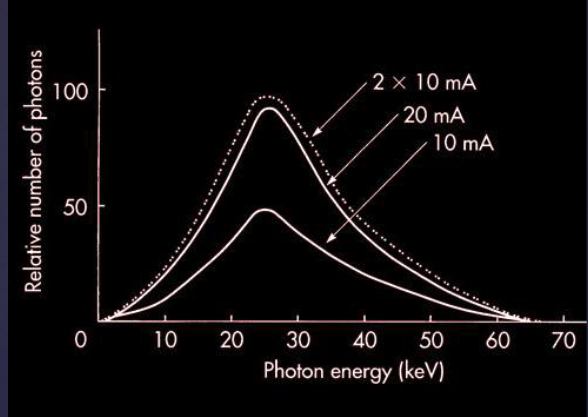
how does changing tube current (mA), affect beams?
increasing tube current = increasing number of photons
no affect on quality (mean and max energy stays the same)
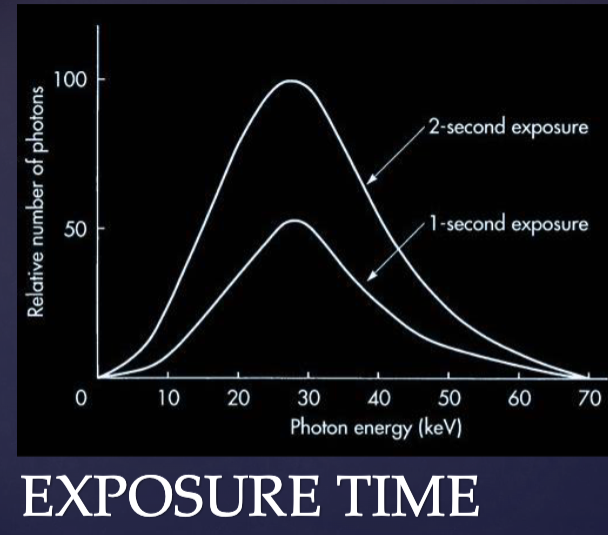
how does changing exposure time (S) affect beams?
increasing exposure time = increasing number of photons
no affect on quality (mean and max energy stays the same)
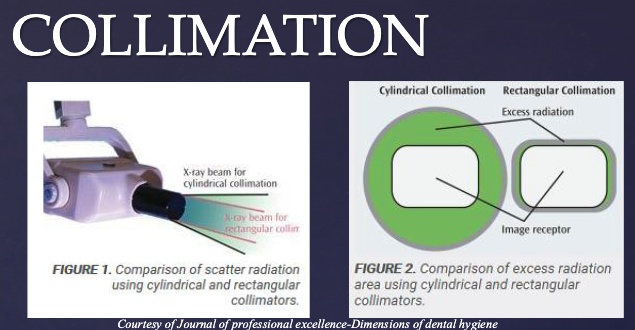
Collimator is a metallic barrier with an aperture that:
1. Reduces size and modifies shape of beam
2. Reduces volume of tissue irradiated
3. Improves image quality
what law describes the effect of distance from xray source to receptor on intensity?
inverse square law (For a given beam, the intensity is inversely proportional to the square of the distance from the source)
increased distance = decreased intensity/quality
Clinical Significance: Changing the distance between the x-ray tube and patient has marked effect on beam intensity, so position the cone of x ray tube as close to the patient (not touching) as possible
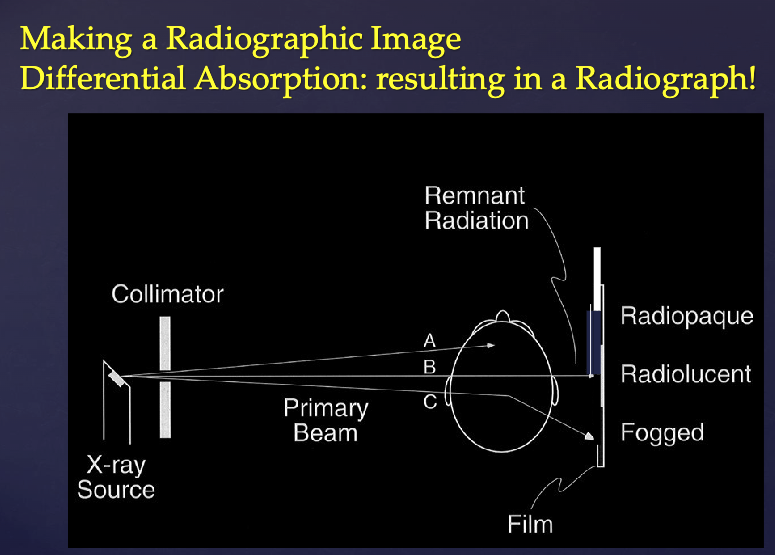
what are 3 types of interactions (scattering an absorption events) that can occur?
coherent scattering
photoelectric effect
compton scattering
what happens during coherent scattering?
low energy photon passes near an outer electron and releases that same energy in a different direction
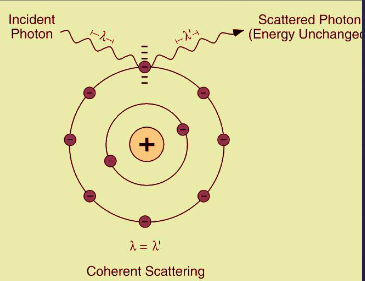
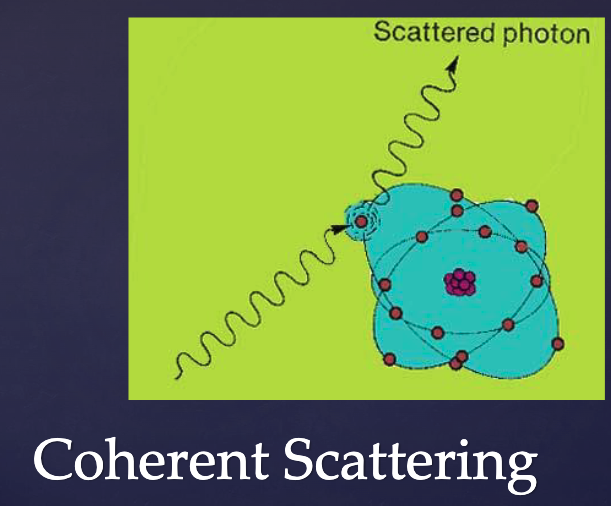
what % of total interactions are coherent scattering?
7%
what interaction is the primary contributor to image formation?
photoelectric effect
what happens in photoelectric effect?
Incident photon collides with an inner-shell electron in an atom of the absorbing medium
The electron is ejected (ionization)
Transfers all energy to the electron; incident photon ceases to exist
An electron from higher energy level fills the vacancy
Characteristic radiation is emitted (low energy, absorbed in the patient)
The recoil electron (photoelectron) travels a short distance before giving up all its energy
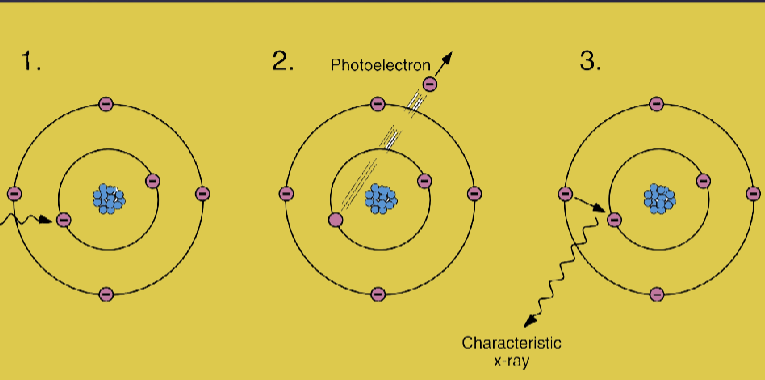
what % of total interactions are photoelectric effect ?
27%
how is photoelectric effect different from characteristic mechanism?
photoelectric is triggered by photon colliding with inner-shell electron
characteristic is triggered by a high energy electron colliding
what is the clinical significance of photoelectric effect?
Z (atomic #) of bone is higher than Z of soft tissue- differential photoelectric absorption within different types of tissues, makes production of a radiographic image possible!
what happens in compton scattering?
Incident photon interacts with an outer orbital electron
Electron recoils and is ejected from the target atom
Incident photon is deflected as scattered photon with a lower energy
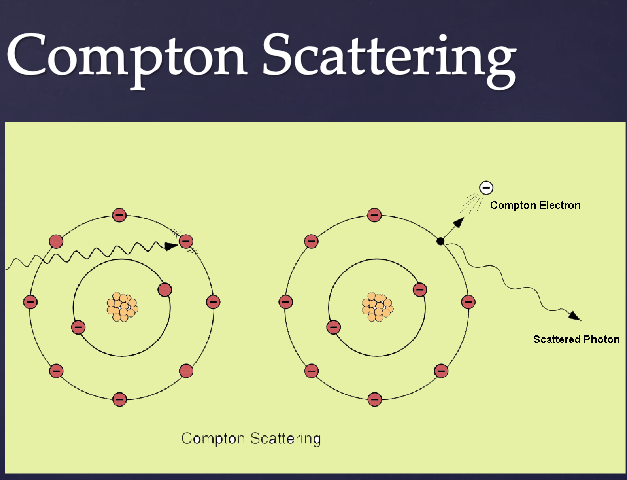
what % of total interactions are compton scattering?
57%
scattered photons caused by compton scattering travel in all direction. what % of scattered photons exit the pt’s head? what does this causee?
30%
Causes fogging (darkening) of the film/receptor while carrying no useful information due to altered path
what term refers to A Measure of comparison of Biological Effectiveness of Different types of radiation?
equivalent dose (eg. xray vs alpha radiaiton)
what unit is equivalent dose reported in?
Sievert Sv
what is used to estimate risk in humans by comparing different exposure types (Panoramic Vs chest radiograph)?
effective dose
what factors are taken into account when determining effective dose?
volume/radiosensitivity of tissue irradiated
biologic effectiveness of radiation
what unit is effective dose reported in?
Sievert (Sv)
what is the study of effects of ionizing radiation on living systems?
radiation biology
what types of ionizing radiation is uncharged and non-particulate (electromagnetic)?
xrays, gamma rays
what types of ionizing radiation is uncharged and particulate?
neutrons
what types of ionizing radiation is charged and particulate?
beta particles, alpha particles, protons, heavy ions
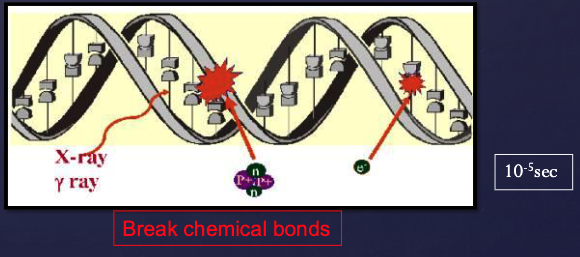
Radiation Injury /Damage is a result of…?
Ionizations within tissues/cells
what are the 2 mechanisms via which radiation causes cell injury?
direct effect
indirect effect
what proportion of all radiation-induced biologic effects is caused by x-rays by direct effect?
1/3
what is the direct effect (mechanism of radiation induced cell injury)?
ionization of biologic macromolecules directly by a photon of ionizing radiation
Majority of all radiation-induced biologic effects caused by x-rays is by ..?
indirect effect
what is the indirect effect? (mechanism of radiation induced cell injury
step 1: Photon absorbed by water (in living tissues),causing ionization of some water molecules to form free radicals (radiolysis of water)
Free radicals interact with macromolecules to produce biologic changes
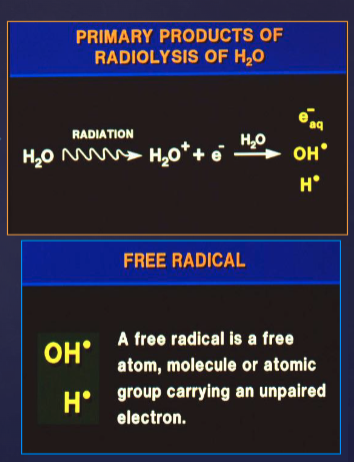
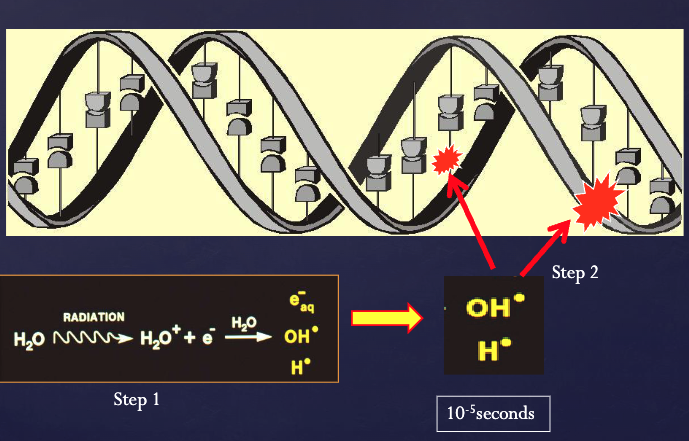
what proportion of all radiation-induced biologic damage caused by x-ray exposure is by indirect effects?
2/3
what is the primary target for cell damage from ionizing radiation?
DNA