GI 4: Oral Cavity and Esophagus Motility and Secretion
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
31 Terms
Chewing
the action that allows for movement of food through GI tract
- begins at the mouth, where the lips and oral cavity function in food intake
- Teeth & Tongue then perform an important process termed Mastication or more commonly Chewing
Purpose of chewing
o Size reduction
o Mixing initiates starch and fat digestion
o Propulsion
o Taste stimulates appetite through centers in the brain, which insures adequate food intake
o Protection by secretion of immunologic salivary agents
- NOT essential for adequate nutrient assimilation as long as particles are small enough to pass into the pharynx
Edentulous individuals
toothless
- unable to mince and mix ingestate with saliva
- Restricted to soft food because larger unminced food particles remain dry and difficult (even painful) to swallow
- Inability to fully savor (taste) food, can affect hunger and appetite
- Significant weight loss and malnutrition common
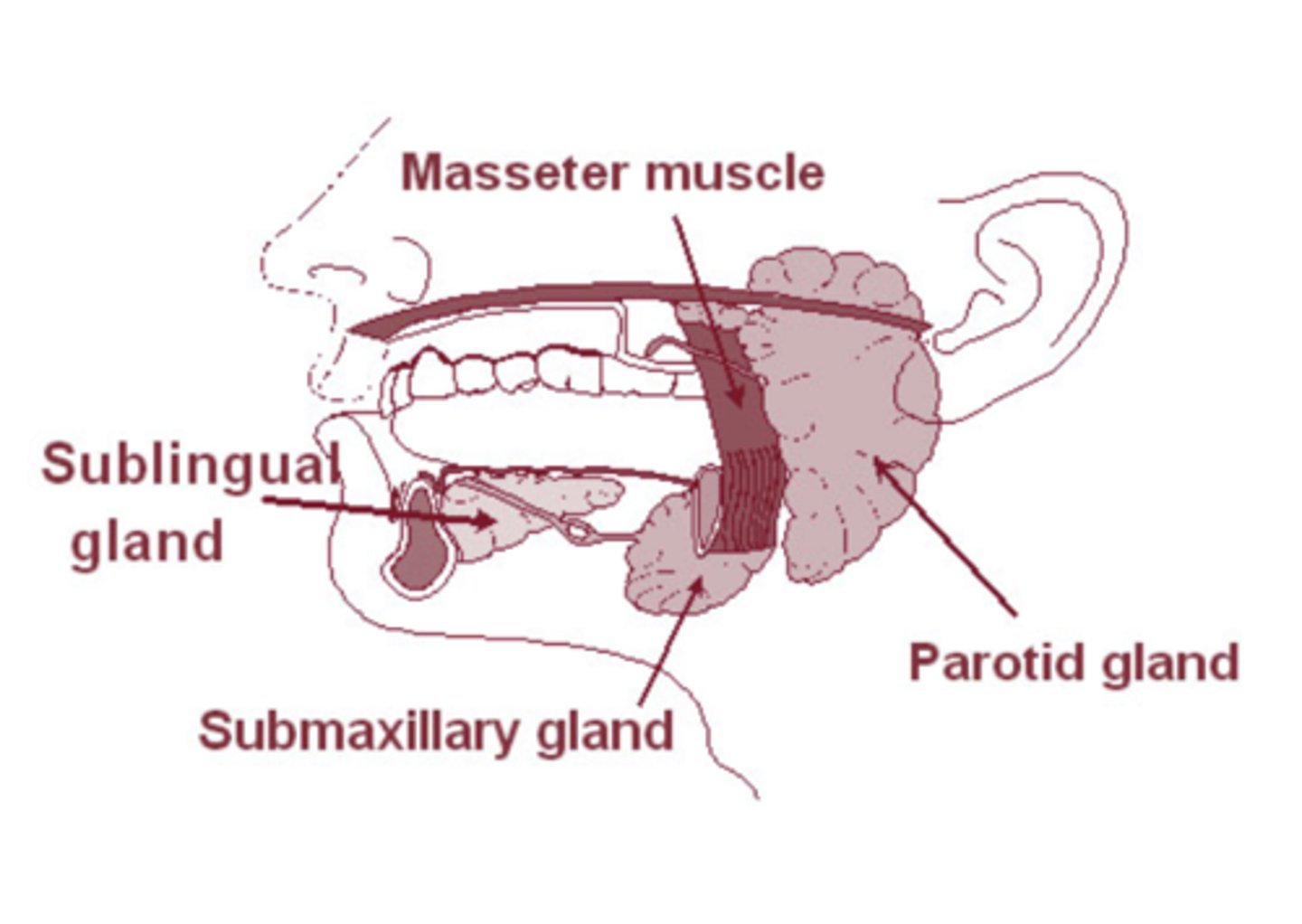
Salivary glands
parotid, sublingual, submaxillary glands
Composition of saliva
1. Mucin: H2O & Mucus
2. Electrolytes: Na+, Cl-, HCO3-, K+
3. Enzymes: Ptyalin, Lingual Lipase
- NOT Essential for Normal Digestion
4. Immunological Compounds: IgA
5. Bacteriocidal: Lysozyme, Lactoferrin
6. Blood Groups: A, B, AB, O
Functions of saliva
1. Lubrication: swallowing & speech
2. Protection: dilutes, buffers, cools, warms
3. Hygiene: rinsing; immune & bacteriocidal agents
4. Digestion: carbohydrates & lipids (not essential)
Salivary Secretion Rate
Secrete an average of 1-1.5 L/day of Saliva into the oral cavity
salivon
Basic secretory unit of salivary glands
- produce & secrete salivary fluid
- modify its electrolyte composition before it is secreted into the oral cavity
- comprised of an Acinus (blind sac end)
- Possess a high blood flow rate, which facilitates fluid and electrolyte flux into the salivon and produces high saliva volumes

Salivary Secretion
expelled into the oral cavity through stimulated contraction of smooth muscle Myoepithelial Cells surrounding the acinus
- Initially secreted as an Isotonic fluid of Neutral pH
Before entering the oral cavity, saliva passes through an:
1. Intercalated Duct (still Isotonic & Neutral)
2. Striated Duct where it becomes Hypotonic & Alkaline
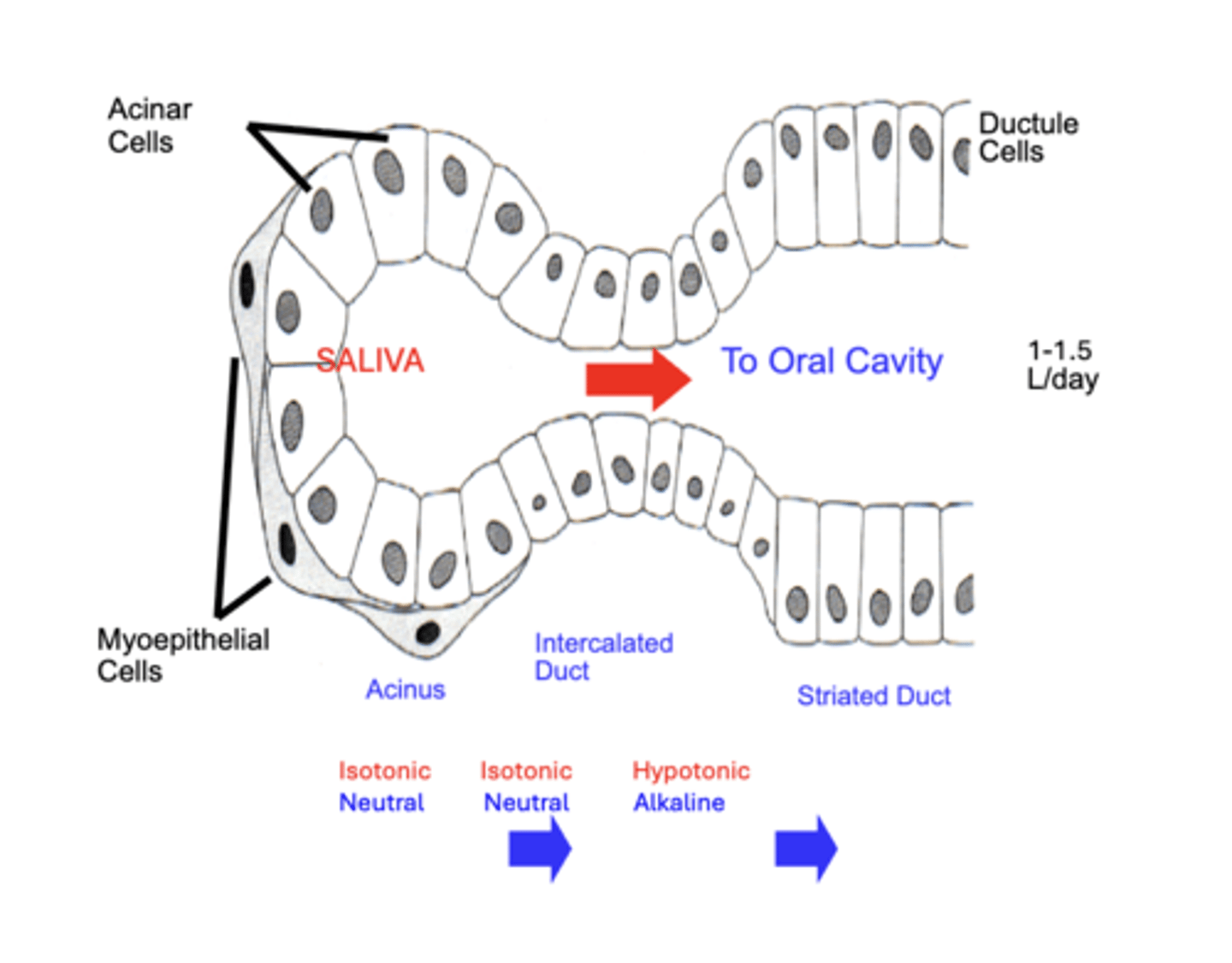
Striated Duct role in salivary secretion
cause saliva to become Hypotonic & Alkaline
through the actions of ion channels:
- reabsorb much of the NaCL
- secrete HCO3- into the secretion
Physiologically, this causes:
- removes much of the “salty” taste from the initial secretion
- alkalinizes the saliva to neutralize acidic foodstuffs that are ingested
Change in Salivary Secretion Rate
- as secretion rate increases, less time is available for saliva modification.
- accounts for the slightly "Salty" taste that occurs when salivation is greatly stimulated
- e.g. biting tongue; smell or site of food, etc.
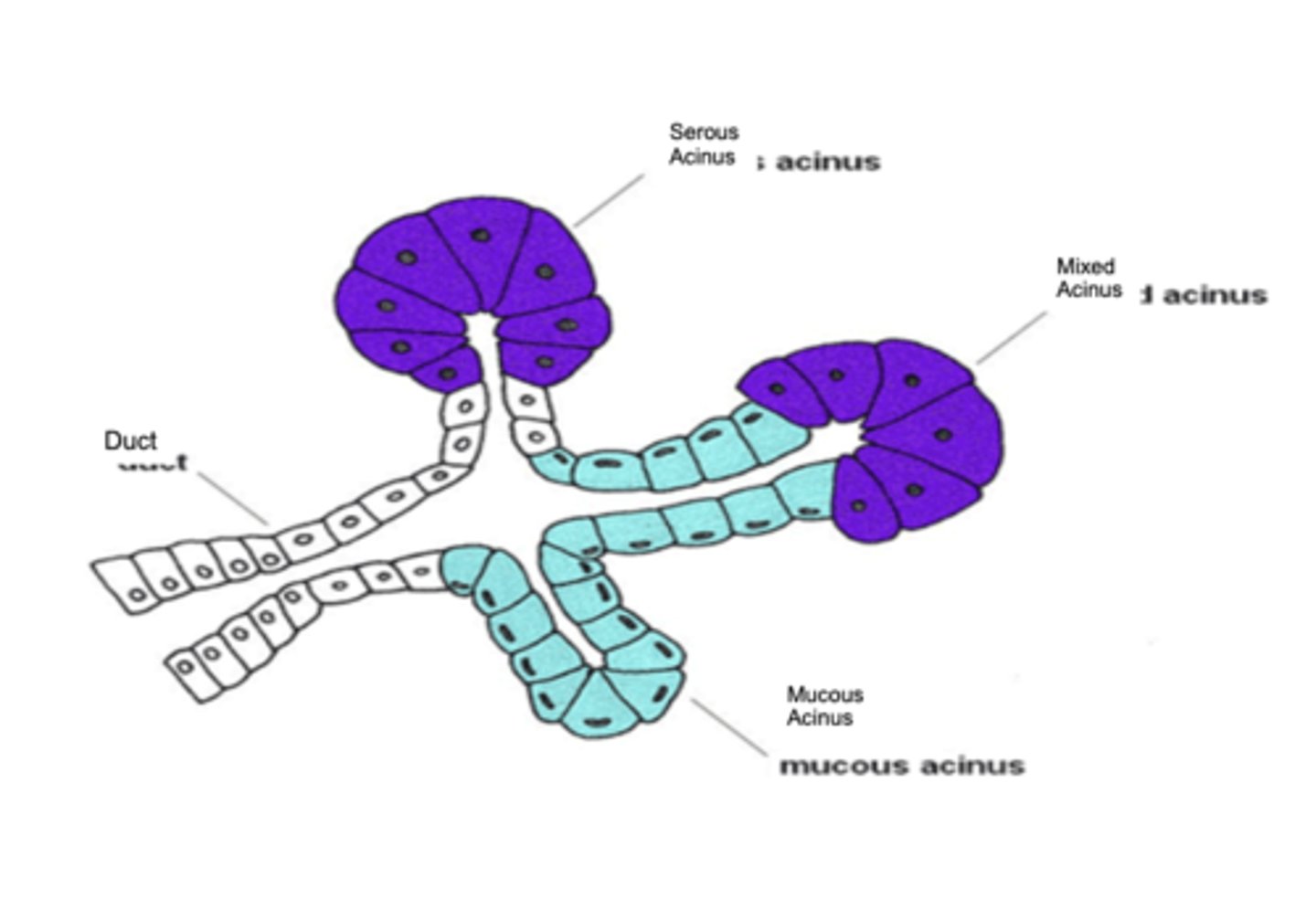
Acini
Composed of serous & mucous secretory cell types
- Serous cells produce a thin, watery saliva containing the enzyme α-amylase.
- Mucous cells produce a thicker saliva rich in mucins – a glycoprotein that lubricates food for swallowing
Regulation of salivary glands secretions
1. ANS
2. GI peptides
3. Physiological inhibitors
4. Physiological stimulators
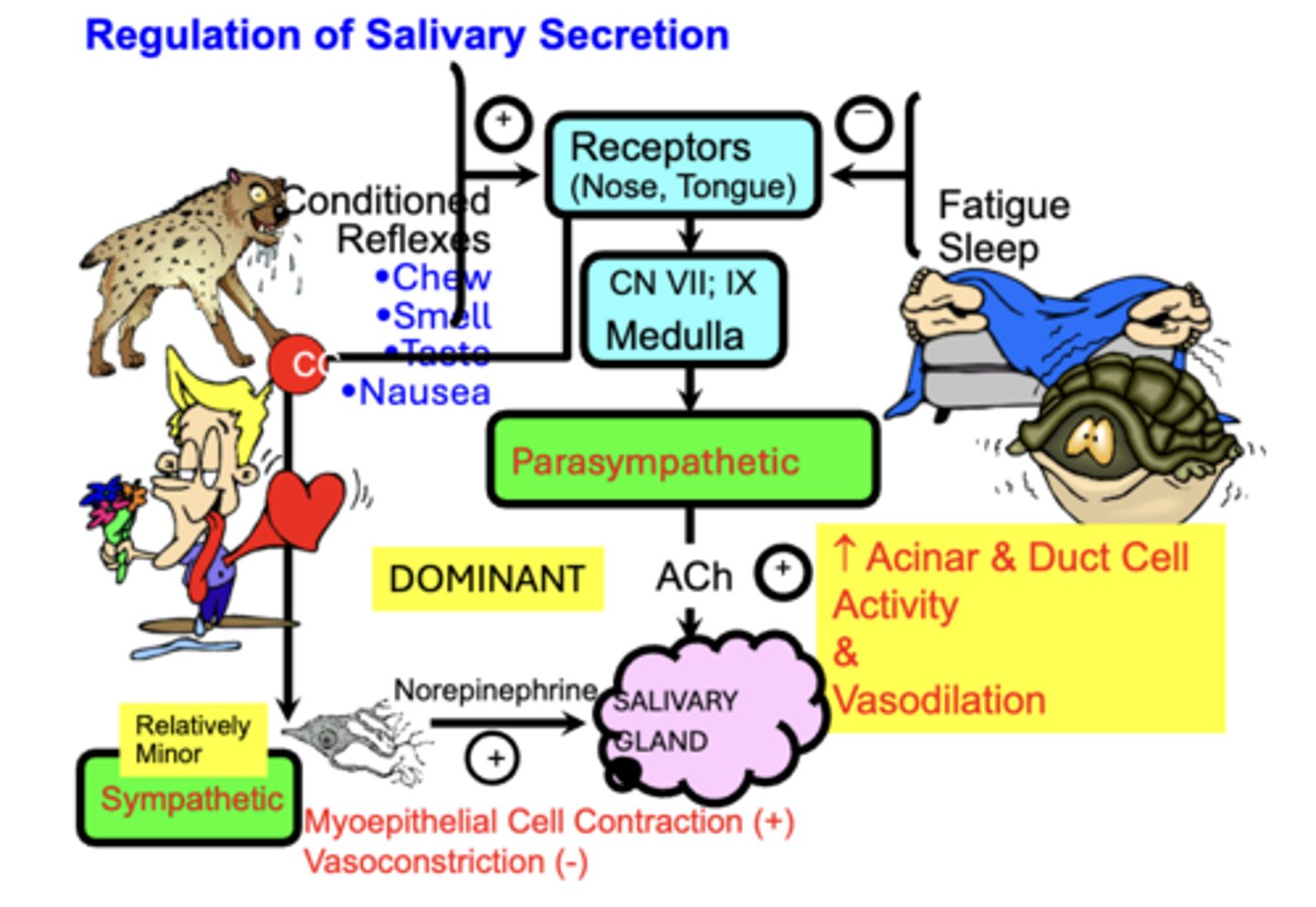
ANS
- Salivary secretion is under predominant Extrinsic Autonomic Nervous Control.
- Both Parasympathetic AND Sympathetic stimulation Increase salivary secretion rate.
A. Parasympathetic control is Dominant
• Via stimulation of Acini activity and blood flow
B. Sympathetic stimulation exerts a Minor increase in secretion
• via stimulation of Myoepithelial Cell Contraction
GI peptides, Physiological inhibitors + stimulators
GI peptides play a minor role
Physiological Stimulators (+)
- Chewing,
- Tasting,
- Smelling food.
- Clinically, Nausea increases salivary secretion rate
Physiological inhibitors (-)
- Sleep,
- Fatigue,
- Dehydration
- Fear
the esophagus passes through the?
pleural space between the lungs and inner thoracic wall
Pressure gradient of the esophagus
negative (>PB) intrapleural pressure (Ppl) pressure created by the opposing passive elastic recoil forces of the lungs and chest wall
= a constant pressure gradient favoring the entry of Air and Acid gastric contents into the esophagus
- Abdominal Pressure > PB
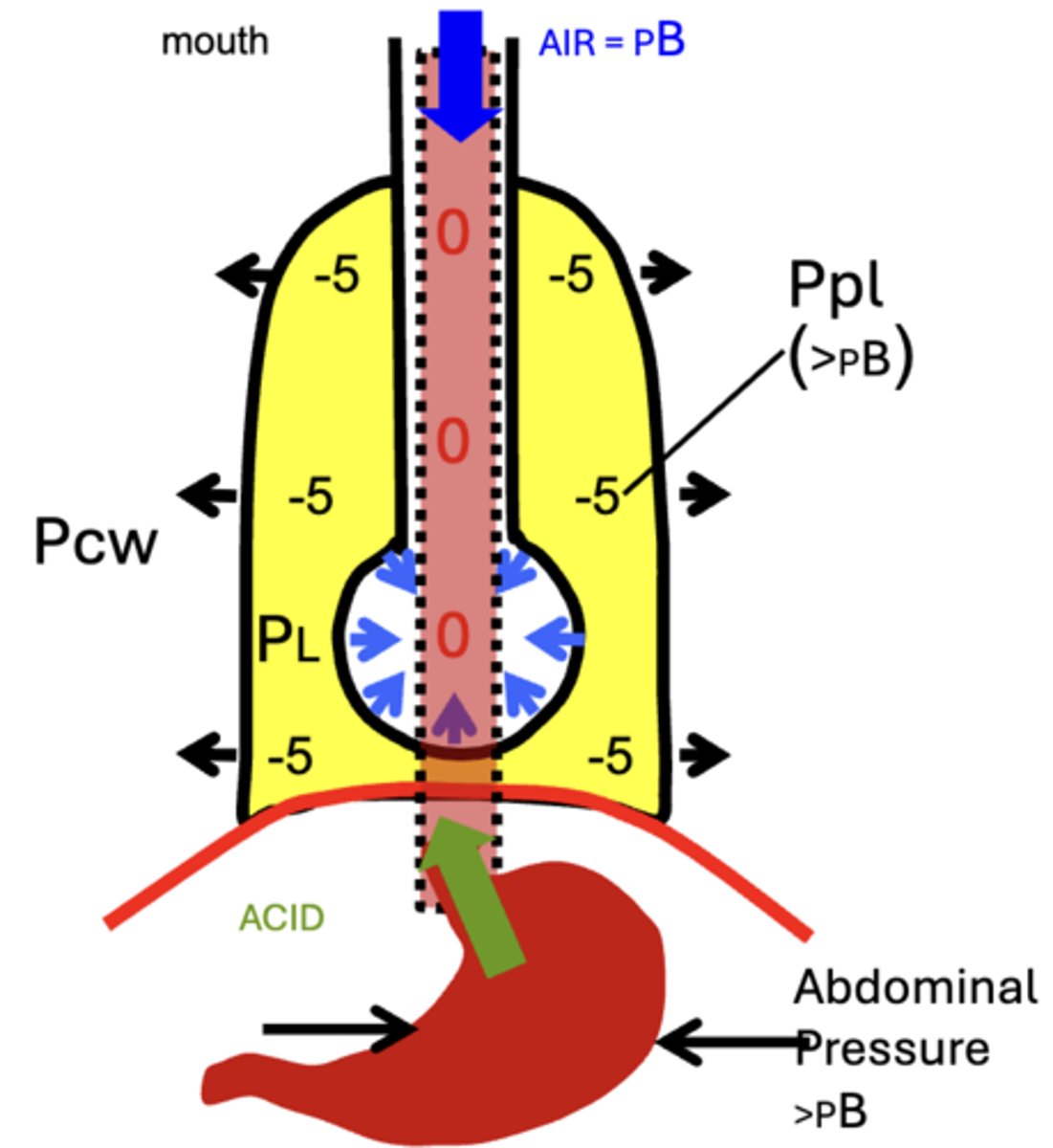
Hiatus Hernia
incompetence of the lower esophageal sphincter LES
- patients with severe reflux disease
- Symptoms are accentuated by positions favoring reflux (bending forward, lying supine) and obesity
Swallowing
the coordinated actions of the oral cavity, pharynx, esophagus, and orad stomach
- Allow passage of the food bolus into the esophagus and prevents aspiration into the nasal cavity and trachea
The Swallowing reflex
Swallowing occurs in two stages: Voluntary and involuntary
overall: Food Bolus → Pharyngeal Receptors → Afferent: Vagus and Glossopharyngeal → Medullary Center → Efferent
Inhibits: Ventilation & Speech
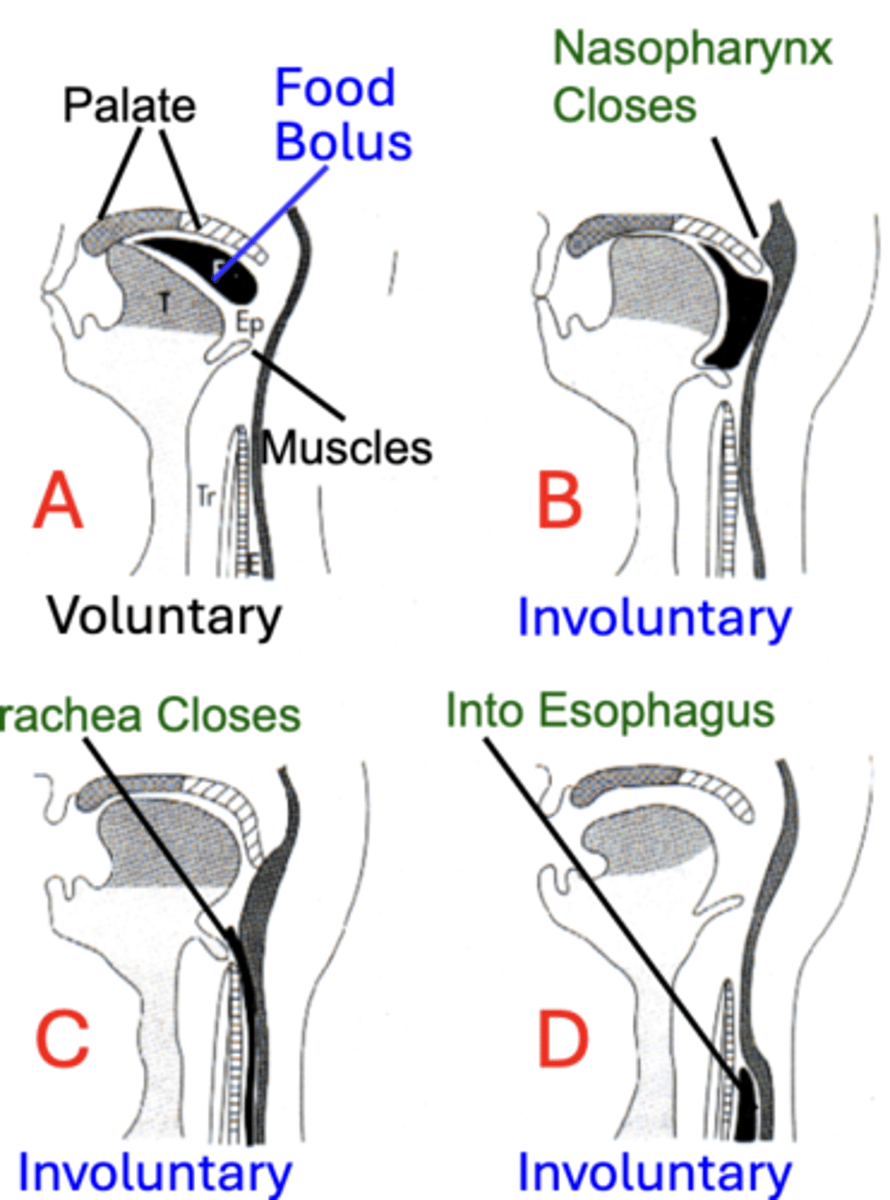
Voluntarily Stage
step 1 of the swallowing reflex
- Initiated by aborad propulsion of material into the oropharynx
- primarily by movements of the tongue, which separates and pushes the Food Bolus backward against the Palate
involuntary Stage
Steps 2-4 of swallowing reflex
begins as material passes into the oropharynx where:
2. the nasopharynx closes by contraction of Pharyngeal Muscles to prevent entry into the nasal passages
3. Trachea Closes to prevent aspiration into the lungs
4. In coordination with relaxation of the UES, the bolus is propelled Into the Esophagus
Dysphagia
Difficulty in swallowing
- Due to mechanical or neural factors
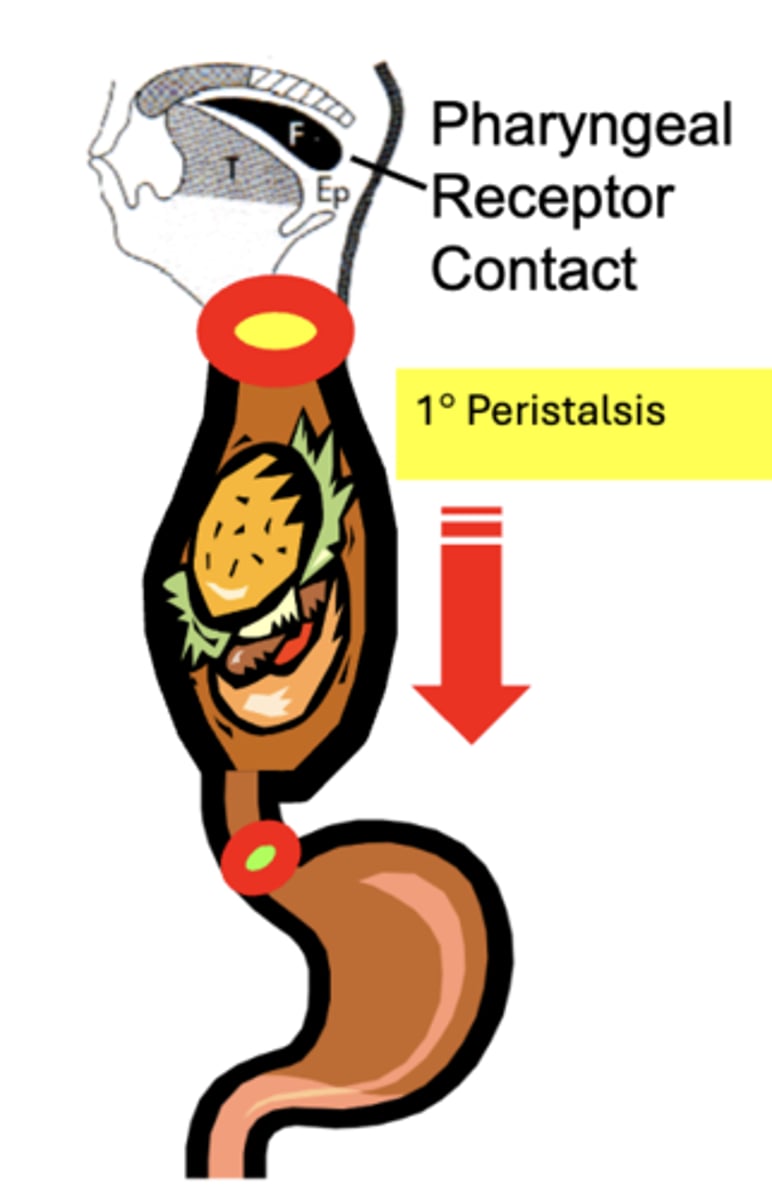
Primary (1°) Peristalsis
propulsive aborad contractile wave within the body of the esophagus
- initiated through Pharyngeal Receptor Contact
- functions to propel newly entering boluses of material down the esophagus towards the stomach
- initiated by swallowing (food bolus, fluid, saliva, etc.)
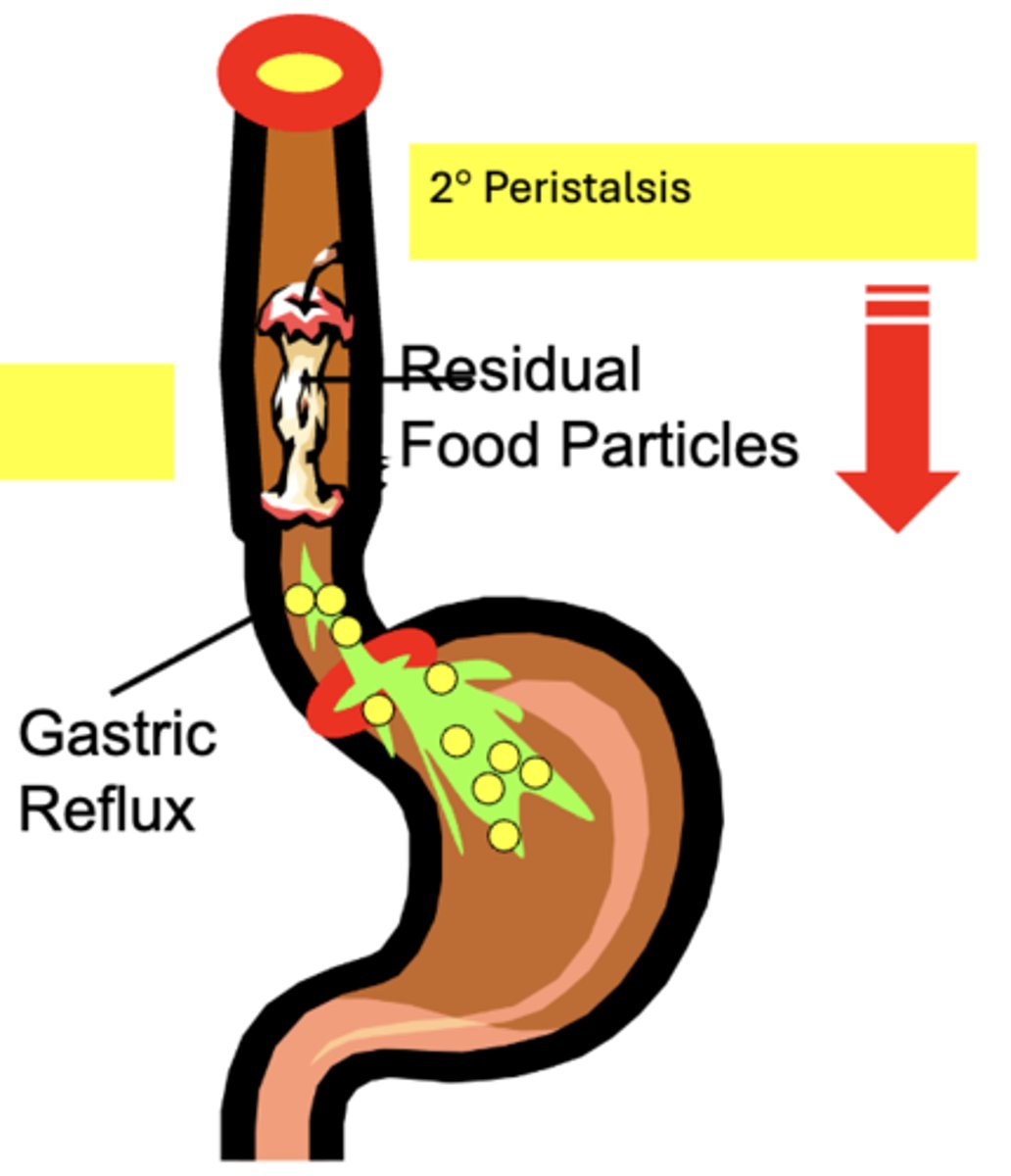
Secondary (2°) Peristalsis
- similar to 1° peristalsis, except it is initiated by distension of the esophagus body by material in the lumen (NOT Pharyngeal Contact)
function of secondary peristaltic contractions:
- to clear or "sweep" the esophagus of Residual Food particles remaining after the primary peristaltic wave
- to remove Gastric Reflux that enters from the stomach
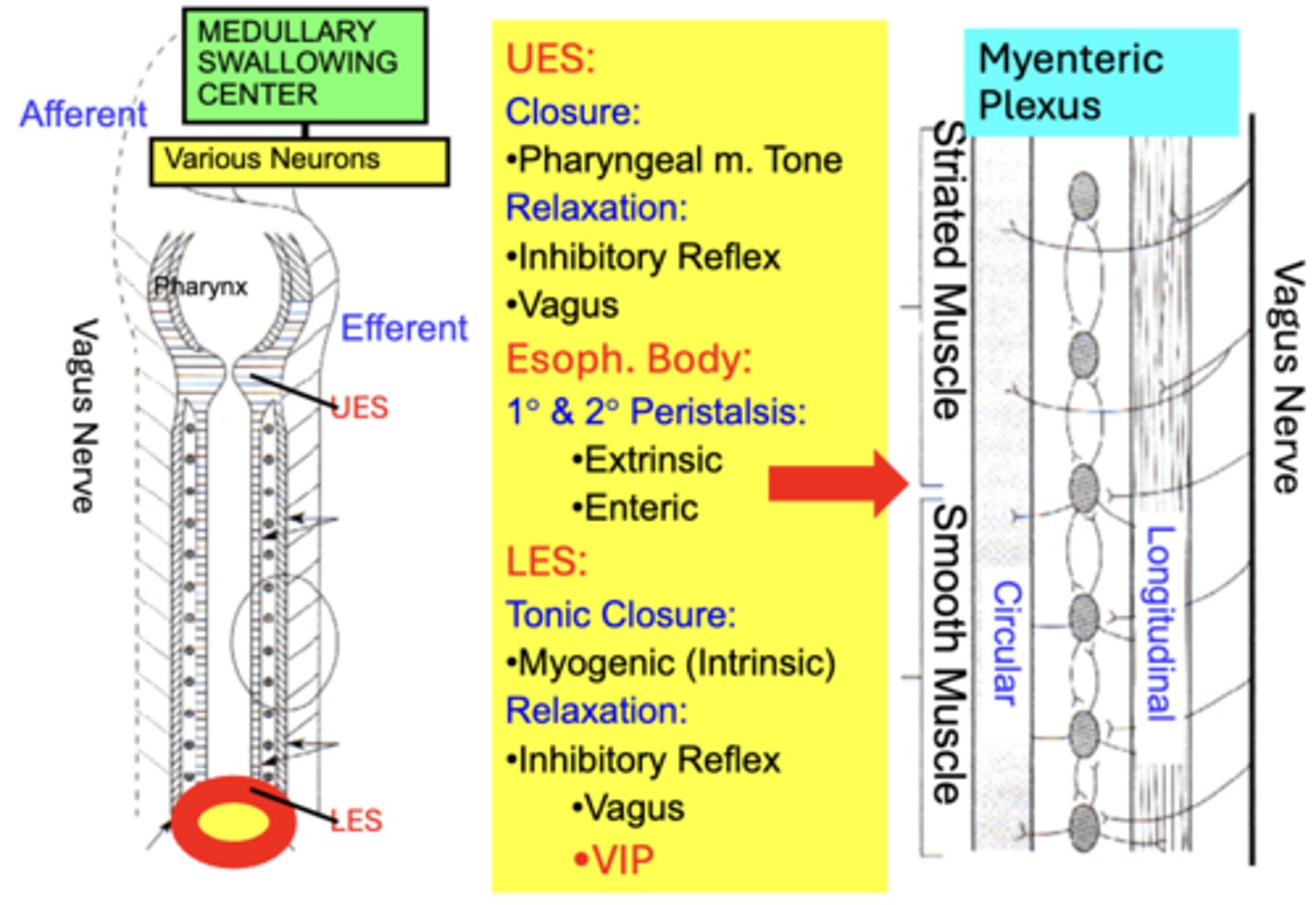
Regulation of esophageal motility
ANS Afferent & Efferent coordination of:
• UES
• LES movements
• Esophageal Smooth Muscle peristalsis
Most actions are mediated by:
• Vagus Nerve
• through Medullary Swallowing Center
• via various neurons integrating with the Myenteric Plexus
Regulation of esophageal motility: UES
A. Tonic Closure between swallows
- maintained by intrinsic Pharyngeal Muscle Tone
B. Relaxation during swallowing
- regulated by a Central Inhibitory Reflex between the Vagus and Swallowing Center that relaxes pharyngeal muscles
Regulation of esophageal motility: LES
A. Tonic Closure
- under smooth muscle Intrinsic Myogenic Control
- constricting in response to passive stretch (closing sphincter)
B. Relaxation during swallowing
- initiated by an Inhibitory Reflex integrated by the Vagus nerve
Regulation of esophageal motility: Esophageal Body (Muscle) Peristalsis
A. Regulated through Vagus Nerve innervation of Smooth Muscle layers
B. Enteric neurons (Myenteric Plexus) integrate extrinsic information but can also coordinate peristalsis independent of extrinsic innervation
Regulation of Esophagus Motility Overview
UES:
- Closure: Pharyngeal m. Tone
- Relaxation: Inhibitory Reflex + Vagus
Esophageal Body:
- 1° & 2° Peristalsis: Extrinsic and Enteric
LES:
- Tonic Closure: Myogenic (Intrinsic)
- Relaxation: Inhibitory Reflex, Vagus, + VIP
Achalasia
Results from an abnormally high LES Tone such that the LES fails to relax during swallowing and 1° peristalsis is weak and non-propulsive.
• Swallowed food may require several hours to empty into the stomach
• A common cause is the degeneration of ganglion cells of the myenteric plexus that impairs LES relaxation.