Schizophrenia 1
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
70 Terms
Who was the first person to describe symptoms of Sz?
Emil Kraepelin (1898)
how did Emil describe the sympotms of patients as?
'Dementia praecox' - "precocious madness," is a historical term for the condition now known as schizophrenia
What does dementia praecox mean?
A global distruption of perceptual and cognitive processes which has an early adulthood onset
What were the main symptoms of Dementia Praecox?
Cognitive symptoms such as impairments in attention, memory and goal directed behaviour.
- progressive condition (doesn't return to premorbid functioning)
How did Eugen Bleuler (1911) reformulate Emil's 'dementia praecox'?
He coined the term 'Schizophrenia' - 'split mind'
What did Eugen Bleuler mean by the term 'split mind' ?
He characterised it as fragmented thinking
- distinguished between pos and neg symptoms
what are positive symptoms of Sz in the DSM? (shown in addition to normal behavioiur)
- Hallucinations
- delusions
- disorganised behaviour
what are negative symptoms of Sz in the DSM? (lack of healthy behavioiurs)
- lack of emotional expressions
- difficulty in experiencing pleasure
- social withdrawal
What are cognitive deficit symptoms in people with Sz?
has an effect on brain function (how well it can organise thoughts and make decisions)
- attentional dysfunctions
- working memory (encoding information and applying it)
- executive dysfunctions (ability to understand info and use it to make a decision)
What % of patients with Sz experience cognitive deficits?
75%-80%
What is disorganised thinking
A cognitive deficit where it becomes difficult to maintain a coherent chain of thinking to do activities such as having a conversation or reading a book
What is slowed thinking
A cognitive deficit when your thinking is slowed down. e.g can't keep up with flow of a conversation
What is difficulty understanding?
A cognitive deficit where particularly under stress - brain cant understand what is going on in the moment.
What is Anosognosia?
A lack of awareness/insight of ones own illness (Sz) - a cognitive deficit as brain is not recognising that illness is present.
- particularly for cognitive functioning
What are delusions?
A positive symptom:
- a false belief despite evidence to contrary, distorting reality. (e.g someone plotting against them)
- thought insertion (someoen else inserting thoughts into my brain)
- thought withdrawal (thoughts are being removed by an external force)
- thought broardcasting
- not being in control of own actions
What are hallucinations ?
A positive symptom:
- perceptual experience that seem real to the patient but aren't (absence of physical proof) such as
- auditory hallucinations
- visual
- olfactory (smelling things that are not there
What is Disorganised behaviour?
A positive symptom:
- difficulty with organising speech in a coherent way, routine tasks
- inappropriate emotions.
What is diminished emotional expression?
A negative symptom:
- blunted effect, mood or emotional state, limited range of emotions
- Alogia
What is Alogia?
A type of diminished emotional expression that affects speech (lack of conversation and reduced speech)
What is Avolition?
A negative symptom:
- Apathy (lack of motivation)
- social withdrawal from social situations
- Anhedonia
What is Anhedonia?
inability to experience pleasure
What is the definition of cognitive deficits in someone with Sz?
Substantial impairment in overall cognitive performance.
- can be variable.
What are the 5 most common cognitive deficits present in someone with Sz
1. Executive functions/cog control (verbal fluency like divergent thinking and problem solving)
2. attention (vigilance)
3. processing speed
4. memory
5. social cognition.
What is the presence of cognitive deficits associated with?
associated with poor daily functioning and quality of life.
At what age can cognitive deficits be detectable?
In childhood/early adolescence > neurodevelopmental disorder.
at what age are the positive/negative symptoms typically developed?
During late adolescence (later on from cognitive deficits)
Why is Sz considered a neuro-developmental disorder?
because there are changes in the brains neurochemistry and brain structures (slow emergence of brain normalities)
What are the asssumed causes of Sz?
No definite answer - combination of the genetics and the environment
What estimated % of Sz is considered heritable?
80%
What is the general prevalence of Sz in the population?
1%
How much more is a child or sibling of an affected individual likely to develop Sz?
10 times more likely.
Why is Sz a polygenic disorder?
Because at least 108 genes have been found to be linked in the development of Sz symptoms.
Genetics explain a....
small percentage of cognitive variance in individuals with Sz
What prenatal adverse events may increase chance of Sz development?
- poor maternal nutrition
- infections
- lack of oxygen for baby.
what happened when rats at birth had hippocampal injuries
it later on led to abnormalities in the dopaminergic organisation in the PFC.
What other environmental risk factors may contribute to the development of Sz?
- early childhood viruses
- growing up in an urban environment vs countryside
^ air pollution?
- Drugs: some individuals develop SZ after taking certain drugs (cannabis)
Which 4 neurotransmitter systems are prominently involved in schizophrenia?
Dopamine
acetylcholine
Glutmate (Glu)
GABA
Which symptoms does the dopamine system play a part in?
Positive symptoms, attention, working memory.
What type of nt is Glutamate?
the main excitatory neurotransmitter
What type of nt is GABA?
the main inhibitory neurotransmitter.
Which symptoms does the Acetylcholine system play a part in?
Attention and memory.
Where do dopaminergic Neruons mainly originate?
in the midbrain (substantia nigra/VTA)
Where do dopaminergic neurons mainly project to? Haber 2014
- The striatum
- frontal cortex
What is the dopamine hypothesis?
there is a modulated amount of Dopamine in individuals with Schizophrenia, causing psychotic (positive) and cognitive symptoms.
What is the mesocortical dopaminergic pathway?
The dopamine system where neurotransmitters are projected to the frontal cortex from the Ventral tegmental area.
- VTA > FC
Evidence for dopamine hypothesis: which agonists induce psychotic symptoms?
Cocaine, amphetamine, L-DOPA
Evidence for dopamine hypothesis: What do post-mortem and neuroimaging studies show?
Altered/modulated levels of Dopamine in the midbrain in individuals with Sz. (PET studies)
What does an increased striatal dopamine release correlate with?
Correlated with the severity of more psychotic (positive) symptoms.
Why can the dopamine hypothesis not be the full explanation as evidence for Sz?
Because increased striatal dopamine does NOT correlate with negative symptoms.
What are the limitations of the DA hypothesis?
- typical antipsychotic medication today reduces DA levels in the brain bUT does not reduce negative/cognitive deficit symptoms and can even be detrimental to them.
What is a Hypo-dopaminergic state?
When there is too little dopamine in the cortical areas in Sz indivudals.
What is a Hyper-dopaminergic
When there is too much dopamine in the striatum in Sz individuals
What does antipsychotic medication address and why is this an issue?
It addresses DA modulations in the striatum (reduces dopamine levels) which then potentially worsens the Hypodopminergic state in the cortex.
DA levels...
fluctuate in individuals with Sz ovetime
Cognitive symptoms....
are much more stable over time in individuals with Sz (unlikely they are due to dopamine therefore.)
What are region specific treatments?
Treatments that would be ideal to reduce excess dopamine in the striatum whilst enhancing dopamine function in the cortex (McCutcheon et al 2019)
What do current medications for Sz treat?
positive symptoms (30% of patients are resistant)
- no effect for negative symptoms or cognitive dysfunctions.
What is the assumption of Glutamates effect on the neurotransmitter systems and Sz?
The disregulation of the dopamine system is a cause/knock on effect from impaired glutamate function. (poels et al 2014)
What was found in postmortem brains of Sz patients that support the glutamate hypothesis?
There was a loss of glutamate neurons prominently in the Anterior cingulate cortex (ACC)
- Consistently comes up in literature
What is MRS?
A neuroimaging technique to identify neuro-metabolites changes in the brain
- magnetic resonance spectroscopy.
- represents the levels of diferent nts.

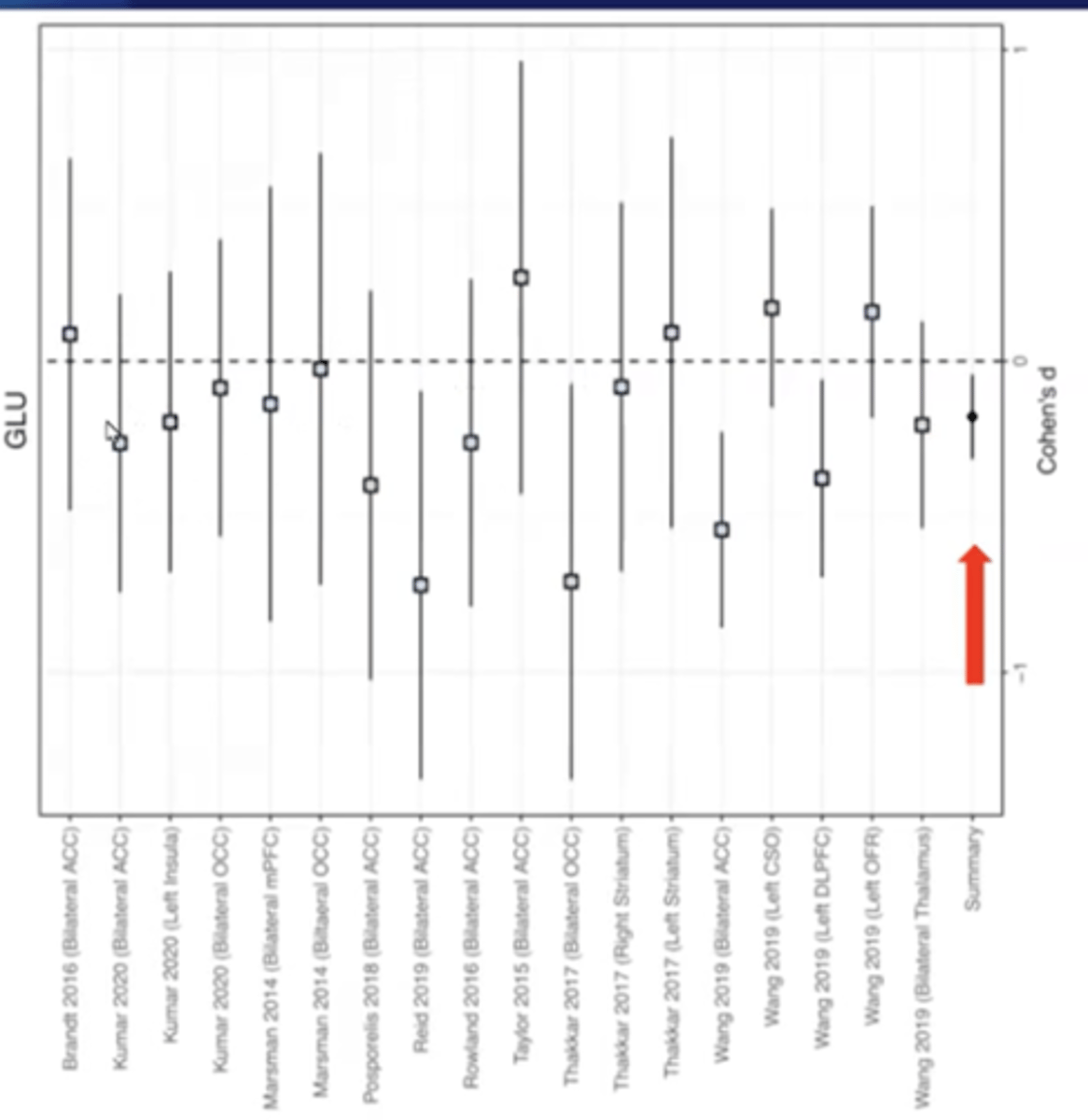
What did Sydnor & Roalf (2020) investigate?
they conducted a meta-analysis of MRS studies in patients with Sz.
What did Sydnor & Roalf (2020) find?
Decreased levels of glutamate in Schizohrenic patients compared to controls (healthy individuals)
- cohen's d found glutamate levels lower in individuals with Sz (significant result)
How did Merritt et al (2023) further investigate the glutamate hypothesis?
Found regional differences in Glutamate levels.
what did Merritt et al (2023) find in the cortical areas of the brain for patients with Sz?
reduced levels of glutamate in the medial frontal cortex linked to symptom severity.
what did Merritt et al (2023) find in the basal ganglia for patients with Sz?
increased levels of glutamate in the basal ganglia.
How do glutamate levels change over time in those with Sz? (Moghaddam & Javitt 2012)
There are two phases of glutamate modulations in individuals with Schizophrenia. (temporal development) "over time"
What is the first phase? (Moghaddam & Javitt 2012)
1. The early phase:
- NMDA (a type of glutaminergic receptor) mediated interneuron dysfunction - loss of inhibitory control which initially increase glutamate in the brain.
What is the second phase? (Moghaddam & Javitt 2012)
2. The later phase:
- Glu-induced excitoxicity from too much glu in the brain so neurons die which leads to a loss of glutaminergic connections - decreased Glu levels.
What do newer, atypical antipsychotics target?
A variety of neurotransmitters
- dopamine
- serotonin
- adrenalin
Why are available drugs not effective to the same extent in all patients?
because nt systems seem to be affected to different degrees in patients (variability in symptoms between patients)