Core Concepts of Nursing - Exam 1 2024
1/117
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
118 Terms
What Makes Nursing a Profession?
Regulation (Nurse Practice Act + Standards of Care)
Licensure (NCLEX)
Education (life-long learning process)
Professional Organization (ANA, AACN, NLN)
Code of Ethics (from the ANA)
What does ANA, AACN, and NLN mean
American Nurse Association (ANA)
American Association of Colleges of Nursing (AACN)
National League for Nursing (NLN)
7 Professional Nursing Behaviors
1. Appearance
2. Accountability (ability to answer to ones own actions)
3. Advocacy (support of clients health, wellness, safety, and personal rights including privacy)
4. Competence
5. Collaboration
6. Compassion
7. Integrity
Caring Interventions
Attitude - most important caring intervention
Compassion - 2nd caring intervention
Ethics
the study of conduct and character
- affect judgments about what is right/wrong; good/bad
Ethical Principles
Autonomy
Justice
Veracity
Fidelity
Beneficence
Nonmaleficence
DO NOT CHANGE (ABSOLUTE)
Autonomy
the right to make ones own personal decisions
Justice
fairness in care delivery and use of resources
Veracity
a commitment to tell the truth
Fidelity
fulfillment of promises
Beneficence
Action that promotes good for others, without any self-interest
Nonmaleficence
a commitment to do no harm
What about ethical principles DOES change?
interpretation and application
Ethical Decision Making
involves finding a balance between science, ethics, and personal moral values
Ex: vaccinations
ethical dilemma
occurs when ethical principles and their application DIFFER
self-reflection
first step in developing self-awareness
Self-Awareness
- first/most important step when facing an ethical dilemma
- deep understanding of what is important to you (developed over time)
ANA Code of Ethics
9 provisions that serve as a basic ethical guideline for nursing
Kindness
an outward expression of caring
5 Auscultation Sites of the Heart
1. Aortic: 2nd ICS (right)
2. Pulmonic: 2nd ICS (left)
3. Erb's Point: 3rd ICS (left)
4. Tricuspid: 4th ICS (left)
5. Mitral: 5th ICS (left)
Erb's Point
the transition point where "lub" (S1) becomes louder than "dub" (S2)
Mitral
the apex of the heart
- point of max impulse (PMI)(Apical Pulse)
- medial to the midclavicular line
S1
"lub" - first heart sound
- closure of the mitral and tricuspid valves (contraction; systole)
S2
"dub" - second heart sound
- closure of aortic and pulmonic valves (relaxation; diastole)
murmurs
abnormal heart sounds created by increased blood volume in the heart
Bruits
abnormal blowing or swishing sound of the heart; decreased blood flow
- listen with bell of stethoscope
Patient Position for Listening to the Heart
1. sitting, leaning forward, mouth open
2. lying supine
3. turned towards the left side (best for extra sounds)
Diaphragm of stethoscope
High-pitched sounds (lung, bowel, heart); place firmly against skin
Bell of stethoscope
low pitched sounds (extra heart sounds, murmurs); place lightly against skin
Normal BP Range
90-120 systolic
60-80 diastolic
General Survey of Patient
information gathered upon the *first encounter* with the patient
collect data for:
1. Physical Appearance (age, sex, race, color of skin)
2. Body Structure (height, weight, nutritional status)
3. Mobility (motor activity, ROM)
4. Behavior (facial expression, speech)
5. Vital Signs
Neurological Survey
Speech (clear/coherent)
Communication
Hearing
Level Of Consciousness (LOC)
Oriented x 3 (Person, place, time)
Components of a Health Assessment
1. systematic (head to toe make it flow)
2. critical thinking (using the data to make critical decisions)
3. patient's current and ongoing health status (70% of the diagnosis comes from the health history)
4. risk factors (modifiable or non-modifiable) modifiable=diet, exercise, smoking (can change) non modifiable = age, gender, race
5. identify health-promoting activities - (exercise)
Problems Presented by the Patient
1. Physical (pain, weight gain, rashes, etc)
2. Social (tobacco use, drug use, financial stress)
3. Emotional (recent life-altering events, depression, mental health, etc)
4. Cultural (language barriers, racial)
5. Environmental (occupation, home life, etc)
Four Types of Assessments
1. Initial (baseline): performed after admission to establish a baseline (head to toe assessment, vital signs)
2. Problem-focused: determines the status of a specific problem; ongoing process (pt. comes in w a sprained ankle, your gonna focus on the ankle)
3. Emergency: during a crisis to identify life-threatening problems (ABC method for respiratory distress)
4. Ongoing Reassessment: comparison of the patient's current status to the previous baseline data (head-to-toe every 4 hr or whatever the hospitals policy time is)
Sources of Data
Primary = the CLIENT
Secondary = all other sources which does NOT COME FROM the client (family, friends, patient record, literature, other healthcare providers)
Subjective Data
symptoms (anything reported by the patient)
- typically SAID; so will be in quotations
EX: pain, symptoms verbally expressed, family history, social history, etc
Objective data
things that the nurse observes
EX: heart rate, lab reports, weight, vital signs, etc
Methods of Data Collection
1) Observing
2) Interviewing
3) Examining
Observing (method of data collection)
Using the senses to observe patient data
Vision: skin color, body language, weight gain/loss, etc
Hearing: heart, lung, bowel sounds
Smelling: body odor, CDIFF
Touch: temperature (skin warm or dry?)
Interviewing (method of data collection)
- Techniques: Standardized formats or Therapeutic techniques
- have privacy, consider having an interpreter, pull up a chair and face the patient
General Examining Sequence
1. Inspect (look)
2. Palpate (touch)
3. Percuss (tap) w pads of fingers
4. Auscultate (listen)
Abdomen Examining Sequence
1. Inspect
2. Auscultate
3. Percuss
4. Palpate
- Auscultation comes prior to steps 3 & 4 to ensure that the bowel sounds do not become obstructed
Data Collection and Interpretation
organize, validate, interpret
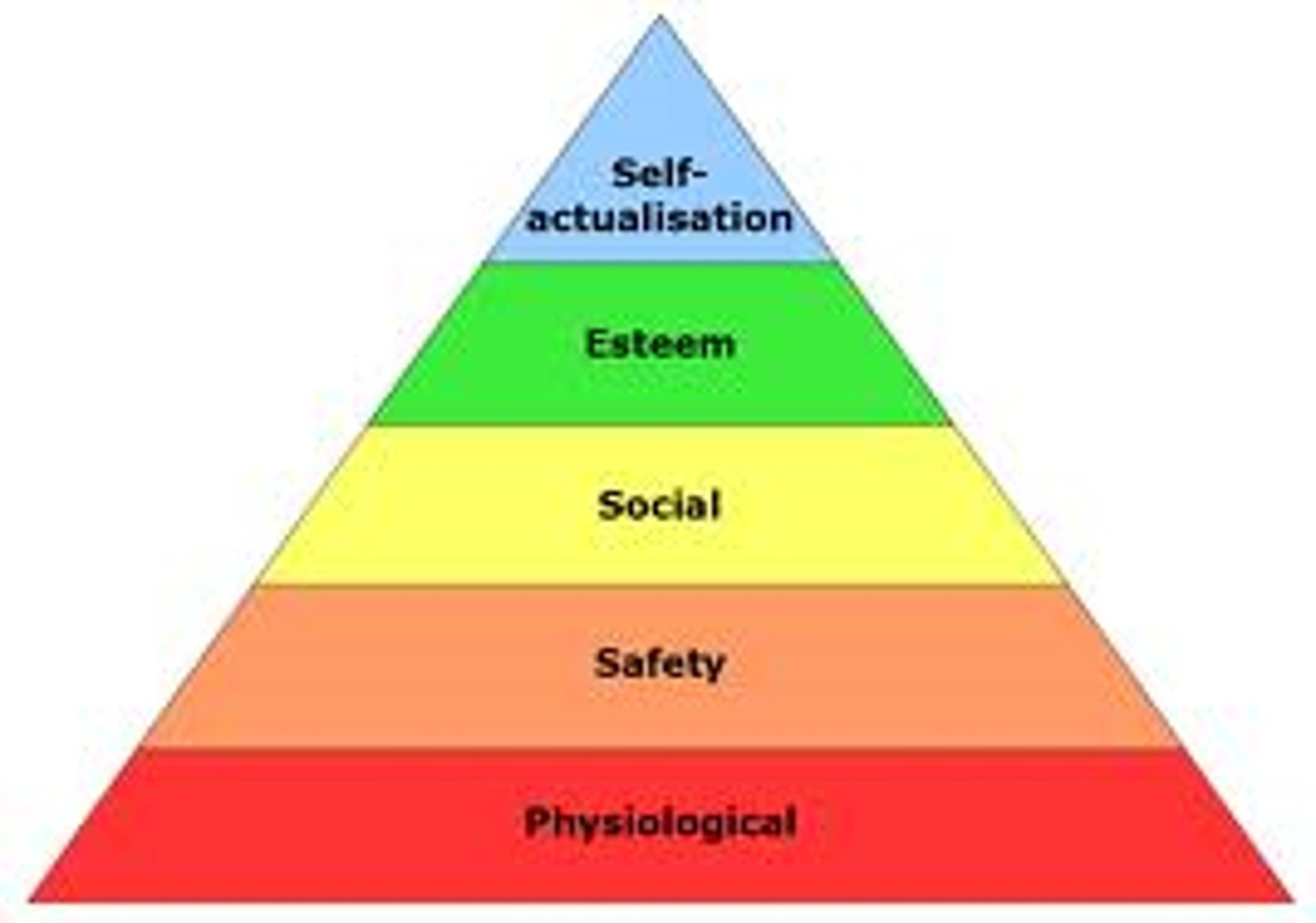
Organize Data Collection (Maslow's Hierarchy of Needs)
1. Physiological Needs: the priority concern to address first (respiratory status, food)
2. Safety and Security 3. Love and Belonging
4. Self-Esteem
5. Self-Actualization: lowest priority
Validating Data Collection
checking allergies, clarifying vague statements, checking extreme abnormal findings a second time or manually
Interpreting Data Collection
using the information to determine nursing care
- includes nursing autonomy
Documentation
a part of communication; if it was not documented, it was not done
- objective
- use SBAR during handoffs
Guidelines for older adults
Allow more time for responses
AIDET
Acknowledge
Introduce
Duration
Explain
Thank
PQRST
Provoked (what causes the pain?)
Quality (what does the pain feel like?)
Region (where is the pain?)
Severity (0-10 scale)
Timing (when did it start? is the pain consistent?)
What is the nursing action for a patient with an irregular pulse?
Count the pulses for the entire minute instead of 30 seconds
If there are no bowel sounds heard, what action should the nurse take?
Listen to each quadrant for 5 minutes
Regular Respiration Rate
12-20 breaths per minute
Regular Pulse Rate
60-100 beats per minute
- measure using radial pulse
Normal Blood Pressure Range
less than 120 systolic
less than 80 diastolic
elevated blood pressure
120-129 systolic and less than 80-89 diastolic
Stage 1 hypertension
130-139 systolic
80-89 diastolic
Stage 2 hypertension
greater than or equal to 140/90
Hypotension
Systolic less than 90
Tympanic Temperature
eardrum
- for older patients, pull the ear up and back
- for children, pull the ear down and back -may read as lower
Temporal Temperature
measuring the body temp using the forehead; higher than oral and axillary
Oral Temperature
measuring the body temp sublingually;
- 95.0° - 100.3°
- wait 10-30 mins if the client has been eating, drinking, etc
- instruct patient to breathe out their nose, if they breathe through their mouth don't take
What temperature is considered a fever?
100.4 F
false high BP
- cuff too narrow
- unsupported arm
- insufficient rest before assessment
- deflating cuff too slowly
- assessing after smoking
false low BP
- cuff too wide
- deflating cuff too quickly
- arm above heart level
Before beginning any personal care delivery, what task should be completed?
an evaluation of the client's ability to participate in personal hygiene; encourage them to participate as much as they can
Types of Baths
complete baths, partial baths, and therapeutic baths
- bathe systematically from the upper extremities to the lower extremities
- long firm strokes form distal to proximal
Changing Bed Linens
- do unoccupied linen change as often as possible
- smooth wrinkles
- keep soiled linens AWAY from you
- DO NOT SHAKE linens because it spreads micro-organisms through the air
- mitered corners
Nail, Hand, and Foot Care
- Inspect the feet daily, do not apply lotion between the toes or fingers, cut nails straight across (check the facility's policy prior to cutting)
- Check nails for cracking, clubbing, and fungus
Nail and Foot Care for Patients with Diabetes Mellitus
- do not soak the feet due to the risk of infection
- do not cut the nails; file nails using a nail file
- do not apply lotions between the fingers and toes
-a qualified professional may be needed
Oral Hygiene for Unconscious Patients
- have suction set up at bedside
- use a soft-bristled brush & mouth swabs
- use a syringe with a small amount (10mL) of water
- place patient on one side with the head turned toward you or in semi-Fowler's position
- DO NOT put your fingers in their mouth
- perform oral care every 2 hours
Denture Care
- remove/insert the top dentures first (down and out)
- remove/insert the bottom dentures second (up and out)
- place a towel in the bottom of the sink
- use tepid water
- place the dentures in a cup with water to keep them moist
Perineal Care
always use fresh water and a new area of the washcloth to perform perineal care; cleanse from front to back
- Males: cleanse penis in a circular motion; retract foreskin to wash the tip (meatus outward) then replace the foreskin
- PAT dry
Hair Care
brush or comb hair daily with soft-bristled brush or wide-toothed comb
- use dry shampoo or no-rinse shampoo (heat activated) and shampoo cap
For Shaving:
- if patient is prone to bleeding, is on anticoagulants, or has a low platelet count, use an electric razor
- shave in the direction of the skin
- large strokes for large areas, short strokes for the chin and lips
Common Safety Concerns
1. Falls
2. Adverse Drug events
3. Healthcare Associated Infections (Priority Action: Hand Hygiene)
4. Restraints
5. Wrong-Site Surgery
6. Latex exposure
What's the priority action to prevent falls?
complete a fall-risk assessment for each client upon admission and at regular intervals
Room Exit Safety to Prevent FALLS
1. Bed in Lowest position
2. Appropriate # of side rails raised
3. Locked wheel
4. Bedside table w/in reach
5. Call light within easy reach (make sure they know how to use)
Which organization sets the National Patient Safety Goals?
The Joint Commission (TJC) in 2002
QSEN 6 Core Competencies
1. Patient-centered care
2. Informatics and Technology
3. Evidence-based practice
4. Quality improvement
5. Safety
6. Teamwork and collaboration
- ensures that nurses have knowledge, skills, and attitude (KSA)
Fire Safety
All staff must know the location of exits, alarms, fire extinguishers, and oxygen shut-off valves; know the evacuation plan
- change smoke detector batteries twice a year
- use cotton material to prevent fire
- have "No Smoking" signs
RACE
fire response acronym
R = rescue and protect/evacuate clients
A = activate the alarm system
C = contain/confine the fire by closing doors and windows
E = extinguish the fire
PASS
acronym for fire extinguisher use
P = pull the pin
A = aim at the base of the fire
S = squeeze the handle
S = sweep the extinguisher from side to side
Why is Carbon Monoxide so dangerous?
It binds to hemoglobin and reduces oxygen; it cannot be seen, smelled, or tasted; can cause death
Food Poisoning
- most caused by bacteria
- most occurs due to unsanitary food practices
ABCDE principles
Airway: open airway?
Breathing: chest rise and fall, RR
Circulation: heartbeat, pulse, cap refill, BP, stop any bleeding
Disability: level of conciousness
Exposure: prevent hypothermia; warm blankets, fluids
CPR
sustains oxygenation and circulation to vital organs
- involves "CAB"
CAB
components of CPR
C = chest compressions
A = airway
B = breathing
What should be the temperature of the water heater in someone's home?
below 120 degrees
Standard Precautions
- proper hand hygiene
- PPE
- effective management of potentially contaminated surfaces
Restraints
protective devices used to limit physical activity of the client or a part of the body
- used to protect the patient from self-harm and to protect other patients and staff
- physical, chemical, seclusion
Physical Restraints
any manual method attached to the patient's body to limit or restrict free movement
- limb restraints
- belts
- mitts
- wheelchairs with stationary lap trays
- bed rails
Need to tie to a non movable thing Ex: bed head-frame
Chemical Restraints
pharmacological agents administered for the purpose of controlling behavior
- sedatives (EX: Benedryl)
Unethical uses of Restraints
- convenience of staff
- punishment for the patient
- clients who are physically/mentally unstable
Policies and Procedures for Using Restraints
- MUST BE PRESCRIBED AFTER A F2F ASSESSMENT
- can be applied in emergencies, but a prescription must be obtained from the provider within 1 hour
- max 24 hours
- Length of application: Adults = 4 hours; Ages 9-17 = 2 hours; under 9 = 1 hour
- Assess skin every 2 hours
- always offer food, fluids, and bathroom breaks
- pad bony prominences
- use a *QUICK-RELEASE KNOT*
- do not secure restraints to the bed rails
Homeopathic medicine and herbal remedies are...
...not FDA approved
Pain
an unpleasant sensory and emotional experience associated with actual or potential tissue damage
THE #1 PRIORITY
- based on duration and origin
pain threshold
the point at which a person feels pain
Pain tolerance
the amount of pain a patient can endure
Acute Pain
pain that lasts less than 6 months
- has a direct cause, SUDDEN ONSET, and is temporary
- fight or flight
- causes changes in physiological responses (vital signs)
- can lead to chronic pain if not handled
EX: breakthrough pain