Renal Papers
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
Jacobs and Fecteau, 2019
Urethrotomy in combination with or after temporary tube cystostomy for treatment of obstructive urolithiasis in male goats
Objective: To report the clinical findings, outcome, and complications associated with urethrotomy performed in combination with or after temporary tube cystotomy for treatment of obstructive urolithiasis in male goats
Results:
89 tube cystotomy procedures were performed
83% did not require additional surgical intervention
17% had persistent obstruction that required a second surgical procedure
Analysis of the calculi in 14/15 goats revealed calcium carbonate (12), calcium phosphate (1), calcium oxalate (1)
For 13/15 goats, a urethrotomy was performed as a separate procedure afte rthe tube systotomy
13/15 (86%) goats discharged from the hospital a median of 13 days after urethrotomy
Similar to rates of hospital discharge from modified perineal urethrostomy (90%), vesicoperputial anastomosis (100%), and urethroscopy and laser lithotripsy used as a primary or secondary surgical option is also similar (80%)
Median time to urethrotomy after temporary tube cystotomy was 5.5 days (0-13 days)
Median voluntary waiting period between urtehtotomy and occlusion of the Foley catheter to “challenge” to goats after the second procedure was 3 days (2-8 days)
Complications related to the urinary system occurred in 5 goats
Recurrent obstruction (2)
Urination from open urethrotomy (1)
Uroabdomen and intra-abdominal adhesions after removal of the Foley catheter (1)
Incisional infection (1)
Complications unrelated to the urinary system included
Anemia/diarrhea (1)
FUO (1)
Upper airway obstruction requiring tracheostomy during intubation (1)
5/7 goats with long-term follow-up (2-24 months after surgery) were healthy, with normal urinary function
Remaining 2 goats returned to the hospital with signs of reobstruction that were attributed to uroliths at necropsy in 1 goat
Benefits of urethrotomy
Maintain normal anatomy of the genitourinary tract to maintain urinary continence and avoid urine scald and prevent adhesions to the penis in breeding animals
Conclusion: Goats treated with urethrotomy for persistent urethral obstruction after temporary tube cystotomy generally survived the procedure. Normal long-term urinary function was obtained in some goats, although recurrence was the most common complication
Keir and Kellum, 2015
Acute kidney injury in severe sepsis: Pathophysiology, diagnosis, and treatment recommendations
Human Data Synthesis
Sepsis-induced AI is diagnosed in up to 47% of human ICU patients and is seen as a major public health concern associated with increased mortality and increased progression to CKD
AKI develops from a complex relationship between the initial insult and activation of inflammation and coagulation
In contrast to the traditional view, clinical and experimental data dispute the role of renal ischemia-reperfusion in the development of sepsis-induced AKI
Renal tubular dysfunction with activation of the tubuloglomerular feedback mechanism appears to be a crucial contributor to sepsis-induced AKI
Furosemide and n-acetylcysteine (NAC) do not appear to be helpful in the treatment of AKI
Hydroxyethyl starches (HES), dopamine, and supraphysiological concentrations of chloride are harmful in patients with AKI
Veterinary Data Synthesis
Community and hospital-acquired AKI is a significant factor affecting survival in critically ill patients
Sepsis-induced AKI occurs in 12% of dogs with abdominal sepsis and is an important contributor to mortality
Early detection of AKI in hospitalized patients currently offers the best opportunity to improve patient outcome
The use of urinary biomarkers to diagnose early AKI should be evaluated in critical care patients
Human and Experimental Research
Definition and classification
RIFLE criteria (Risk, Injury, Failure, Loss of kidney function, End-stage kidney disease) - stratifies patients based on the presence of risk, injury, or failure based on increases in serum creatinine or decline in urine output; the worst criterion within each domain is used
The outcome criteria, loss or end-stage kidney disease, define the duration of kidney dysfunction
Benefit of focusing the clinician's’ attention to preventing severe loss of kidney function rather than just dealing with the most severely affected
Acute kidney injury network (AKIN)
Risk category widened to include an absolute increase in creatinine of 0.3 mg/dl or more, even if this is below a 50% increase from baseline as long as it is documented within a 48 hour period
Failure on any patient requiring renal replacement therapy regardless of the urine output or serum creatinine concentration
improves sensitivity for diagnosing patients with AKI, but change typically only affects <5% of patients
Kidney Disease: Improving Global Outcomes (KDIGO)
Epidemiology
AKI associated with an increase in mortality with each RIFLE category independently associated with increasing odds of mortality
Etiology
Sepsis-induced AKI is characterized by marked reductions in kidney function with only mild histological changes in the kidney
In contrast to AKI due to nephrotoxins or ischemia where there is diffuse glomerular and tubular damage with extensive necrosis
Ischemia/reperfusion injury
Observation of AKI in association with “low flow” states makes restoring and maintaining renal perfusion a target for preventing AKI in critically ill patients
Treatments that included the use of dopamine, a renal vasodilator, has not proven beneficial in the treatment or prevention of AKI in septic patients
Current evidence suggests that sepsis-induced AKI can occur in the presence of normal or even increased renal blood flow
Inflammation
Following tissue injury at the site of sepsis, cells release DAMPs that result in a further proinflammatory response at distant organs (including the kidney) through activation of immune cells such as T-cells and dendritic cells in these organs
In people with community acquired pneumonia, risk of AKI correlated with plasma IL-6 concentrations
Oxidative stress
Reactive oxygen species (ROS) scavengers have been shown to blunt renal tubular injury during endotoxemia
Epithelial dysfunction
Inflammatory response in the kidney results in widespread renal tubular epithelial dysfunction
Link between tubular dysfunction and reduction in GFR may be through activation of the tubuloglomerular feedback mechanism
Tubular dysfunction → lack of NaCl reabsorption in the proximal tubule
Macula densa cells in the distal tubule detect an increase in sodium and chloride delivery
Results in widespread vasoconstriction of the afferent arteriole and a drop in GFR → clinical manifestations of AKI: decreased urine output and increased serum creatinine
Epithelial dysfunction also seen with disruption of tight junctions between renal tubular epithelial cells, resulting in back leakage of tubular fluid across the epithelium
Cellular injury → loss of cellular adhesion to the basement membrane and shedding of epithelial cells into the tubular lumen → tubular epithelial casts in the urine
Absence of these findings in sepsis-induced AKI casts doubt on this mechanism and treatments aimed to “flush out” the tubules
Sublethal injury
Disrupts cellular function, particularly transport processes
Produces renal dysfunction in the absence of histological abnormalities in the renal tubular cells
Growing evidence to suggest that even mild cases of AKI, which have apparent complete resolution, may be associated with long-term negative outcomes
May result in persistent inflammation and tubulointerstitial fibrosis in proximal tubular cells
persistent tubulointerstitial fibrosis is characteristic of lost renal function
Use of Biomarkers to Detect AKI
Production of creatinine is decreased during sepsis, further limiting its use as an early indicator of AKI
Septic-induced AKI has a distinct pathophysiology when compared to non-septic AKI
urine concentrations of IL-18 are higher in septic patients with AKI compared to non-septic AKI patients
Neutrophil gelatinase associated lipocalin, kidney injury molecule-1, cystatin C, and liver fatty-acid binding protein have demonstrated potential for early detection of AKI and prognostic value for predicting renal recovery
2 novel biomarkers of G1-G0 cell-cycle arrest (tissue-inhibitor of metalloproteinases-2 and insulin-like growth factor binding protein-7) are increased in the urine prior to clinical evidence of AKI
AKI in Veterinary Critical Care
Definition and classification
Using a RIFLE-like criteria in dogs showed a progressive increase in mortality at 30 days associated with increasing severity of kidney injury
Veterinary AKI staging system - same criteria as AKIN criteria, similar results to RIFLE-like system
Both of these systems require knowledge of baseline creatinine if urine output isn’t measured, which may limit use to hospital acquired AKI
International Renal Interest Society (IRIS) AKI grading system for veterinary patients - grades the severity of injury from I-V
Epidemiology
Small changes in creatinine, can have significant influence on mortality
Small increases in serum creatinine after a patient has been admitted to the hospital has a negative impact on mortality
Biomarkers of AKI
In dogs, urinary neutrophil gelatinase-associated lipocalin (NGAL) was able to identify patients with AKI 12 hours before changes in serum creatinine or serum NGAL occured
Urinary cystatin-C in dogs with preexisting renal disease
N-acetyl-beta-D glucosaminidase (NAG) and retinol-binding protein shown to be increased prior to creatinine in dogs with CKD
Management of AKI: Evidence from human and veterinary studies
Primum nonnocere
Discontinuation of nephrotoxic drugs
Re-evaluate the scale of objective monitoring and be prepared to react to small changes
Optimizing treatment of the underlying condition
Hemodynamic monitoring and support
The injured kidney is unable to maintain autoregulation of blood flow making the kidney more vulnerable to changes in blood flow as blood pressure varies
Fluid therapy
Vasopressors can result in reduced blood flow in the setting of volume depletion, but patients that develop AKI will be at risk of volume overload and continued resuscitation can result in harm with a positive fluid balance associated with an increased mortality
Use isotonic crystalloids rather than colloids for volume expansion in patients with or at risk for AKI
No benefit of 4% albumin over isotonic saline and HES associated with significant kidney dysfunction and coagulation abnormalities
Chloride restrictive versus chloride liberal fluid administration
Significant association with incidence of AKI and use of chloride-rich fluids
May be due to higher concentration of sodium and chloride being delivered to the renal tubules, activating the macula densa and causing renal afferent arteriole vasoconstriction
Avoid fluids containing supraphysiological concentrations of chloride
Vasoactive drugs
Recommended to use vasopressors in conjunction with fluids in patients with vasomotor (ie septic) shock
Septic shock characterized by high cardiac output with low vascular resistance producing hypotension despite adequate fluid resuscitation or optimization of the vascular volume
In septic shock the only method to maintain or improve renal perfusion is to use vasopressors once intravascular volume status has been restored
Unknown which, if any, vasopressors is the most beneficial for the prevention or treatment of AKI and septic shock
Dopamine out of favor due to lack of beneficial effects on the kidney and is associated with an increased number of adverse events
Trend toward vasopressin for septic shock refractory to norepinephrine as it increases blood pressure and urine output
Current evidence supports norepinephrine as a first line vasopressor
The use of diuretics in AKI
Recommended that diuretics not be used to prevent AKI and suggested that diuretics not be used to treat established AKI, except to reduce volume overload
Prophylactic use of furosemide to prevent AKI shown to be ineffective and even harmful in critical illness
No evidence to support the use of diuretics to reduce severity of AKI once established
Furosemide has no significant effect on patient outcome, need for renal replacement therapy, or percentage of patients with persistent oliguria
Vasodilator therapy (eg, dopamine, fenoldapam)
Dopamine administered to healthy individuals at low doses (1-3 ug/kg/min) it causes renal vasodilation, increased GFR, and diuresis
Effects not seen in AKI
In AKI dopamine significantly increases renal vascular resistance and reduces blood flow, causes tachyarrythmias and myocardial hypoxia, reduces splanchnic blood flow, and suppresses T-cell function
No evidence to support use of dopamine in treatment or prevention of AKI
Fenoldopam mesylate is a pure dopamine type-1 receptor agonst that causes renal vasodilation but without the a and B adrenergic activation seen with dopamine
May also have anti-inflammatory effects in AKI
Suggested the fenoldopam not used in the treatment or prevention of AKI
N-acetylcysteine (NAC)
Can be used to regenerate glutathione stores, is a potent scavenger of ROS within the body, and enhances nitric oxide availability promoting vasodilation
Animal studies have shown attenuated ischemic and nephrotoxic AKI but these results haven’t translated to human clinical trials
Current evidence doesn’t support the use of NAC in AKI
Renal replacement therapies
Goals of RRT in the treatment of AKI
Maintain fluid and electrolyte balance and solute homeostatis
Prevent further detrimental insults to the kidneys
Permit renal recovery
Allow concurrent supportive measures to proceed without limitation or complication
Controversy whether continuous renal replacement therapy (CRRT) vs intermittent hemodialysis (IHD) is better for patients with AKI
Research has found no difference in outcomes, ICU mortality, and renal recovery between the two
Recommend the use of continuous and intermittent RRT as complimentary therapies in patients with AKI
“Late” initiation of RRT associated with greater mortality, longer duration of RRT, longer hospital stay, and increased dialysis dependence
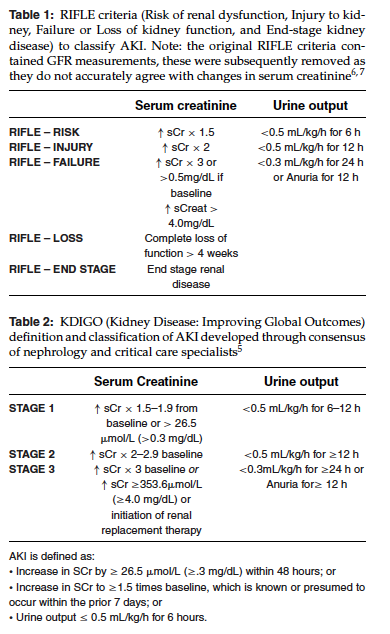
RIFLE - Risk Serum creatinine
Increase in sCr x 1.5
RIFLE - RISK Urine output
<0.5 ml/kg/h for 6 h
RIFLE - INJURY Serum creatinine
Increase in sCr x 2
RIFLE - INJURY Urine output
<0.5 ml/kg/h for 12 h
RIFLE - FAILURE Serum creatinine
increase in sCr x 3 or >0.5 mg/dl if baseline increased sCreat > 4.0 mg/dl
RIFLE - FAILURE Urine output
<0.3 ml/kg/h for 24 h or anuria for 12 h
RIFLE - LOSS Serum creatinine
Complete loss of function > 4 weeks
RIFLE - END STAGE Serum creatinine
End stage renal disease
KDIGO Stage 1 Serum Creatinine
Increase in sCr x 1.5-1.9 from baseline or >26.5 umol/L (>0.3 mg/dl)
KDIGO Stage 1 Urine output
<0.5 ml/kg/h for 6-12 h
KDIGO Stage 2 Serum Creatinine
Increase in sCr x 2-2.9 baseline
KDIGO Stage 2 Urine output
<0.5 ml/kg/h for 12h or more
KDIGO State 3 Serum Creatinine
Increase in sCr x 3 baseline or increase in sCr >/= 353.6 umol/L (>/= 4.0 mg/dl) or initiation or renal replacement therapy
KDIGO Stage 3 Urine Output
<0.3 ml/kg/h for 24 h or more or anuria for 12h or more
AKI is defined as
Increase in SCr by >/= 25.6 umol/L (>/= 0.3 mg/dl) within 48 hours; or
Increase in SCr to >/= 1.5 times baseline, which is known or presumed to occur within the prior 7 days; or
Urine output </= 0.5 ml/kg/h for 6 hours
IRIS AKI Grade I
Non-azotemic AKI, serum creatinine <140 umol/L (<1.6 mg/dL) with a rise in creatinine >/= 26.3 umol/L (0.3 mg/dl)
IRIS AKI Grade II
Creatinine 141-220 umol/L (1.7-2.5 mg/dl)
IRIS AKI Grade III
Creatinine 221-439 umol/L (2.6-5.0 mg/dl)
IRIS AKI Grade IV
440-880 umol/L (5.1-10.0 mg/dL)
IRIS AKI Grade V
>880 umol/L (>10.0 mg/dl)
Oman et al, 2019
Outcome and complications in goats treated by perineal urethrostomy for obstructive urolithiasis: 25 cases (2010-2017)
Objective: To determine short-term and long-term outcome and complications in goats undergoing PU for treatment of obstructive urolithiasis
Results:
20/25 goats had received 1 or more previous treatments for obstructive urolithiasis
Median time from onset of clinical signs to hospital admission was 2 days (<1-12 days)
PU surgery was performed with 24 hours of admission in 64% of cases
In 36% of cases, PU surgery was delayed but the goat received initial surgical treatment by tubcystotomy (8/9) or bladder marsupialization (1/9)
Mean time between admission and PU surgery was 13 days (2-33 days)
44% were treated by MMPU, 28% were treated with PU with the urethral mucosa spatulated to the skin and 28% with PU with the stump of the transected penis sutured to the skin without any spatulation of the urethra mucosa
3 goats died before discharge from the hospital
13/25 (52%) goats were alive at the time of follow-up
Mean time from surgery to follow-up was 34 months (4-65 months)
9/25 goats (36%) died between discharge and follow up with a mean survival time of 46 days (5-120 days)
Cause of death in 7/9 (78%) goats was related to urolithiasis
renal failure (1), aspiration of ammonium chloride (1), peritonitis associated with uroabdomen (1), surgical site leakage with infection (2), stricture of the urethral stoma (2)
The mean postoperative survival time for the 5 goats that had not previously been treated for urinary obstruction was 26.4 months (18 days - 65 months) compared to 15 months (2 days - 51 months) for those that received at least 1 previous treatment for urinary obstruction
Goats treated by use of a modified proximal perineal urethrostomy (MPPU) were significantly more likely to survive at least 150 days postoperatively
The most common postoperative complications were hemorrhage (1/25 [40%]), surgical site infection (3/25 [12%]), and re-obstruction of the proximal urethra (2/25 [8%])
Hemorrhage was significantly associated with MMPU (8/11 [73%])
Stricture of the surgical stoma occurred in 7/22 (32%) discharged goats
Mean time to stricture was 65 days (10-240 days)
Other complications included urine scalding (6/22 [ 27%]), re-obstruction of the urethra (5/22 [23%]), wetting of the rear limbs (4/22 [18%]), and cystitis (2/22 [9%])
4/5 of the goats with re-obstruction were able to be successfully treated with retrograde urethral catheterization and lavage to dislodge stones
6/7 goats with stricture were treated with balloons, revision of teh PU, catheterization of the urethral stoma, bladder marsupialization, and ammonium chloride
Conclusion: Perineal urethrostomy can provide effective long-term resolution of obstructive urolithiasis in goats. Re-obstruction or stricture seems most likely within the first 2 months after surgery. MPPU may provide better long-term results but should be approached cautiously because it can be associated with life-threatening hemorrhage
Riedi et al, 2018
Clinical findings and diagnostic procedures in 270 small ruminants with obstructive urolithiasis
Objective: To describe the clinical presentation and diagnostic procedures in a large group of small ruminants with urolithiasis
Results:
Mean age of the overall population was 3.48 years or 2.94 years for sheep and 4.23 years for goats
81.2% of affected goats were castrated and 91.7% of sheep were intact males
Age at castration was available for 24 animals: 9 had been castrated at 3 months or younger, 9 at 3-6 months, and 6 after 6 months of age
The highest number of cases were presented in January (32 cases, 12%), February and April (29 cases each, 11%) and the lowest caseload in June and July (15 and 17 cases, respectively 6%)
Could be related to reduced water intake because of cold or frozen drinking water
Almost 60% of all animals were fed grain regularly
A high-grain diet is recognized as an important risk factor for the development of uroliths because high P intake with concentrate feed leads to high P excretion through the urinary system and facilitates the formation of struvite calculi
65.5% of the animals had been sick 2 or more days before referral
Median duration of clinical signs before the animals were brought to a clinic was 2 days (0-40 days)
Common abnormalities included dysuria (93.6%), indigestion (84.4%), reduced general state of health (79.5%), signs of pain (73%), increased heart and respiratory rate (53.6% and 39.1%), and azotemia (89.4%)
Absence of colic does not rule out obstructive urolithiasis, but possibly rather indicates an advanced stage of disease
37.4% of the animals were still passing urine, but the majority of them (80.2%) showed dysuria
Neither maintained micturition nor normal gross urine appearance precluded from a tentative diagnosis of urolithiasis
Uroliths were found in the urethral process in 73.8% of the cases
BUN and creatinine concentrations were strongly correlated
Hypochloremia (52.2%), hyponatremia (43.3%), hypophosphatemia (52.4%), and abnormal potassium concentrations (26.2% hypokalemia and 24.5% hyperkalemia) were the most common serum electrolyte imbalances
CK activity was increased in 138/224 (61.6%) of animals
PCV, plasma proteins, potassium, BUN, and creatinine concentrations were significantly increased in animals with uroperitoneum
Azotemia was present in 89.4% of animals, most common abnormality in the chemistry profile
Degree of azotemia was significantly associated with the stage of disease
Ultrasonography allowed for confirmation of diagnosis in 83.9% of cases (135/161 with sufficient available information), uroliths were visible on 34/56 radiographs
Localization of urinary calculi on the radiographs was urinary bladder and urethra (44.1%), urinary bladder only (17.6%), distal urethra only (14.7%), urethra only (11.8%), sigmoid flexure and distal urethra (2.9%), pelvic flexure only (2.9%), and sigmoid flexure only (2.9%)
Animals with clinical signs for >24 hours were more likely to present with uroperitoneum on ultrasonographic examination than those with shorter disease history
Conclusion: Confirmed that clinical and ultrasonographic examinations are sufficient to diagnose urolithiasis. Clinical signs can be divided into an early stage with discrete unspecific clinical changes, a painful stage with frequent straining, expression of pain and moderately reduced general condition, and an advanced state with a markedly reduced general condition and eventual recumbency
Riedi et al, 2018
Variables of initial examination and clinical management associated with survival in small ruminants with obstructive urolithiasis
Objective: The results of physical examination, laboratory analyses, and clinical management of male small ruminants presented to 2 referral clinics were investigated to identify variables significantly associated with disease outcome, so as to provide better recommendations to animal owners regarding the management of these patients
Results:
90% of the sheep were intact males, whereas 82.5% of the goats were castrated
Median age was 3 years for sheep and 4 years for goats
A significant association was found between age and castration status
The median age was significantly different between the surviving and nonsurviving groups, 2.5 years and 3.5 years, respectively
Only 39% of all patients considered for treatment and 52% of those undergoing tube cystotomy survived to be released from the clinic
Follow-up determined that 48.7% were alive, 20.7% without relapse 6 months after discharge, and 45% were alive 1 year after discharge, 18% without recurrence
13/24 were euthanized because of relapse
Surviving animals had shown clinical signs before referral to the clinic for a significantly shorter time with a median of 1 day, whereas the median duration of disease for nonsurviving animals was 2 days
Nonsurvival was strongly associated with a very poor clinical condition upon presentation, obesity, castration, and evidence of uroperitoneum
Intact animals <4 years of age with clinical signs of 24 hours or less duration, normal BCS, normal demeanor, no free fluid in the abdomen, and no uroliths visible on radiographs were significantly more likely to survive
Among blood variable, abnormal PCV, severely increased serum creatinine concentrations, and increased activity of the creatinine kinase were associated with increased risk of nonsurvival
Azotemia was present in 167/210 (79.5%)
Severely increased serum creatinine concentrations were significantly associated with nonsurvival, whereas severely increased BUN concentrations were not
Hyperkalemia and hypochloremia were also associated with increased risk of nonsurvival
Hypokalemia was present more commonly than hyperkalemia - fluids choice should be based on chemistry if able because serum potassium concentration cannot be predicted based on clinical signs
CK mostly reflects disease severity
If an abnormal PCV was measured, the accuracy of the clinical model increased by 5%, from 69% to 74% so a negative outcome could be correctly predicted based on teh relevant clinical variables combined with PCV measurement in ~3/4 cases
Presence of signs of colic or macroscopic appearance of urine was not significantly associated with outcome
Of the animals with normal urine flow after urethral process amputation, 26.1% still had to be taken to surgery afterward
Of the animals with some urine flow after urethral process amputation, 37.5% had surgery and 54.4% of the animals with no urination after urethral process amputation received tube cystotomy
Normal urine flow was restored in 33% of the patients after urethral process amputation and these patients had a significantly higher short-term survival rate (73.9%) than animals for which only decreased or no urine flow was restored (29.2% and 27.3%) respectively
Survival until release from the clinic was significantly higher for the surgical (51.6%) than the nonsurgical group (29.8%) in the univariable analysis
No significant difference was found in long-term survival between animals having received surgical or conservative treatment
Conclusion: The prognosis of obstructive urolithiasis was guarded with survival rates of 39% (overall) to 52% (after tube cystotomy). Intact young males with normal body condition presented early in the course of disease had the best chances of survival
Zhang et al, 2019
Association Between the Use of Sodium Bicarbonate and Mortality in Acute Kidney Injury Using Marginal Structural Cox Model
Objective: Acute kidney injury with metabolic acidosis is common in critically ill patients. This study assessed. the associations between the use of IV sodium bicarbonate and mortality of patients with acute kidney injury and acidosis
Results:
24.5% of the eligible patients had received sodium bicarbonate treatment
Patients who received sodium bicarbonate treatment had a higher Sequential Organ Failure Assessment (SOFA, 9 vs 7), lower pH (7.16 vs 7.18), and bicarbonate concentration (16.51 vs 20.57 mmol/L) compared with those who did not receive sodium bicarbonate
On day 1 in the ICU, patients receiving SB had a lower urine output and were more likely to require vasopressors than those who did not receive SB
Regression model showed that bicarbonate concentration, pH, and PaCO2 were significantly associated with SB use
Other independent predictors of SB infusion included serum creatinine and SOFA score
Sodium bicarbonate treatment was not associated with mortality in the overall population, but it appeared to be beneficial in subgroups of pancreatitis and severe acidosis (pH <7.15)
Sodium bicarbonate appeared to be beneficial in patients with severe bicarbonate deficit (<50 kgxmmol/L)
Associated with increased risk of hospital death in those with bicarbonate overload
Conclusion: In the analysis by adjusting for potential confounders, there is no evidence that IV sodium bicarbonate is beneficial for patients with acute kidney injury and acidosis. Although this study suggested potential beneficial effects in some highly selected subgroups, the results need to be validated in experimental trials.
Costa et al, 2023
Preliminary evaluation of hepatitis A virus cell receptor 1/kidney injury molecule 1 in healthy horses treated with phenylbutazone
Objective: To investigate if hepatitis A virus cell receptor 1/kidney injury molecule 1 (HAVCR1/KIM1) in urine is detectable concurrently with increases in serum creatinine concentrations in horses receiving a recommended dose of phenylbutazone (PBZ) for 7 days
Results:
None of the 10 horses had detectable HAVCR1/KIM1 in urine at baseline
Serum creatinine concentrations in placebo group did not increase and HAVCR1/KIM1 was undetectable in urine
At the end of treatment, 3/5 horses receiving PBZ developed increases in serum creatinine of >26.5 umol/L (>0.3 mg/dl) and HAVCR1/KIM was detectable in urine, despite normal findings on kidney ultrasonography in all horses
Only 1/5 horses had a serum creatinine above the reference interval
Serum creatinine increase ranged from 8.8 to 79.6 umol/L (0.1-0.9 mg/dL), representing an 8.3%-100% increase with a median of 22%
After treatment, USG remained within the reference interval in all horses from the placebo group and in 4 horses in the PBZ group
Two horses from the placebo group and all 5 horses from the PBZ group had detectable protein in the urine at the end of the study
In the horses with acute kidney failure, urinary HAVCR1/KIM1 concentration was higher than the horses receiving PBZ, but urinary HAVCR1/KIM1 was not detected in a horse with chronic kidney failure
Upregulation of HAVCR1/KIM1 occurs during AKI
Conclusion: HAVCR1/KIM is detectable in urine and is associated with increases in serum creatinine concentrations of >26.5 umol/L in horses following treatment with PBZ for 7 consecutive days. Thus HAVCR1/KIM1 might aid in the early detection of acute kidney injury in horses
Edwards and Magdesian, 2023
Retrospective evaluation of acute kidney injury in horses treated with nonnitrogenous bisphosphonates (2013-2020): 8 cases
Objective: To describe a population of horses with acute kidney injury (AKI) following administration of bisphosphonates including clinical signs, clinicopathologic data, treatment, and outcome
Results:
Five horses received intramuscular clodronate (5/8; 62.5%) and 3 horses received intravenous tiludronate (3/8; 37.5%)
No horses were diagnosed with AKI following administration of zoledronic acid
Six horses (6/8; 75%) received concurrent NSAIDs
There was no difference in the incidence of AKI between horses that received bisphosphonates with or without NSAIDs in this study
The most common initial presenting complaint was poor appetite (6/8; 75%) followed by abnormal urination (2/8; 25%), weight loss (1/8; 12.5%), and colic (1/8; 12.5%)
At the time of initial evaluation, the mean serum or plasma creatinine was 451.72 umol/L (5.11 mg/dL) and BUN was 18.84 mmol/L (52.75 mg/dL)
Apart from azotemia, horses often presented with electrolyte abnormalities, increased SDMA, and increased triglycerides
Hypophosphatemia was documented in 66.7% of horses
Serum calcium was normal in 55.6% of horses, mildly decreased in 11.1% of horses, and mildly increased in 33.3% of horses
Five horses (5/6; 83.3%) had either an increased number of red blood cells (4) or hemoprotein (1) in the urine
Renal ultrasound findings in 6/8 horses included bilateral renomegaly (1), increased cortical thickness (2), decreased corticomedullary distinction (2), increased corticomedullary distinction (1), moderate dilation of the proximal left ureter (1), and no ultrasonographic abnormalities (1)
All horses were treated with IV isotonic, balanced cystalloids either as a bolus, CRI, or a combination of the 2
Duration of IV fluid therapy was available for 6/8 horses with a median of 2.5 days (2-5 days)
Seven horses (7/8; 87.5%) survived the initial episode of AKI and 1 horse (1/8; 12.5%) was euthanized
Necropsy findings showed severe, acute, multifocal renal papillary necrosis with mineralization, consistent with NSAID toxicity
Histopathologic findings indicative of bisphosphonate related kidney injury included diffuse interstitial lymphoplasmacytic and neutrophilic nephritis and tubular cell necrosis and regeneration that was moderate in severity
Of the 7 surviving horses, 2 horses (2/7; 28.5%) went on to develop chronic renal dysfunction
Warmblood breeds were overrepresented in the AKI group, when compared to horses that received bisphosphonates during the study period and did not develop AKI
Approach to preventing adverse renal effects in horses being treated with bisphosphonates is to monitor serum creatinine concentrations before and 24-48 hours after administration, as well as to avoid administration of concurrent nephrotoxic drugs
Conclusion: Bisphosphonate administration, with or without concurrent NSAIDs, can be associated with AKI in horses, Serum creatinine should be monitored prior to and following bisphosphonate treatment to minimize this risk. Further evaluation of renal function is warranted in horses that develop clinical signs of poor appetite, lethargy, or altered urination in the days following bisphosphonate treatment
Smith et al, 2020
Clinical presentations and antimicrobial susceptibilities of Corynebacterium cystitidis associated with renal disease in four beef cattle
Objective: To describe clinical presentation, diagnosis, minimum inhibitor concentrations (MICs), and outcome of renal disease caused by C. cystitidis in beef cattle
Results:
All affected cattle had anorexia as a primary complaint
Of the 3 that had ante-mortem diagnostic tests performed, all had pyelonephritis based on azotemia in combination with urinalysis and ultrasonographic findings
Cultures yielded C. cystitidis which was identified by biochemical testing, 16S RNA sequencing, and mass spectrometry
All affected cattle deteriorated despite aggressive treatment, indicating that C. cystitidis infections in beef cattle may carry a poor prognosis
Bacterial isolates collected from 4 cattle showed similarities in MICs for ampicillin, florfenicol, gentamicin, neomycin, sulfadimethoxine, trimethoprim sulfonaide, and tylosin
Additional biochemical testing indicated that all clinical C. cystitidis isolates had the ability to hydrolyze Tween 80 but were unable to digest casein
Results are consistent with C. cystitidis but not C. renale
Conclusion: Corynebacterium cystitidis should be considered in the differential diagnosis of cattle with renal disease. Definitive diagnosis of C. cystitidis as compared to C. renale may be challenging
Boileau et al, 2021
Evaluation of the accuracy of an electronic point-of-care analyzer to quantify blood creatinine concentration in goats
Objective: The objective of the study was to validate the accuracy of a handheld point-of-care (POC) analyzer (Nova StatSensor) for quantifying blood creatinine concentration in goats. A secondary objective was to compare this POC against a chemistry analyzer to classify goats as normal or having mild or moderate azotemia.
Results:
A total of 101 blood samples were collected from 63 goats
There was high repeatability for creatinine concentrations obtained by the POC
Correlation of POC concentrations with those reported by the chemistry analyzer was moderate
Concordance declined as the creatinine concentration increased
The POC correctly classified 11/15 goat blood samples in the mild azotemia group and 15/20 in the moderate to severe azotemia group
When correctly categorizing goats with mild azotemia, the POC demonstrated a sensitivity of 73.3% and a specificity of 88.3%. For moderate to severe azotemia, the POC had a sensitivity of 75.0% and specificity of 97.5%
Chance of false positive was low
Conclusion: The Nova StatSensor POC provided above average accuracy for measuring blood creatinine concentration in goats compared with the gold standard test