Voice, Adult/Pediatric Dysphagia, Cognitive Communication, TBI, Dementia, Phonological Processes, and RHD
1/294
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
295 Terms
Voice disorders
conditions that affect the quality, pitch, loudness, or flexibility of the voice
Structural, neurological, or functional issues
Communication Disorder
affect a person's ability to receive, send, process, and understand concepts or verbal, nonverbal, and graphic communication.
Granulovacuolar degeneration
Degeneration of nerve cells because of the formation of small fluid-filled cavities containing granular debris
Ecolalia
The non-voluntary, automatic repetition or imitation of another person's spoken words or phrases
Left neglect
a disorder of attention and perception in which a person fails to notice, respond to, or attend to stimuli on their left side
Heterogenous
No two disorders are exactly the same
Confabulation
unintentional creation of false beliefs or inaccurate memories
Neuritic plaque
cortical and subcortical tissue taht is degenerating which DESTROYS NEURAL TRANSMISSION OF MESSAGES
What are the 3 neuropathies that occur with dementia?
1. Neurofibrillary tangles
2. Neuritic plaque
3. Granuloacuolar degeneration
Errorless learning
Ability to go through a task without making any mistakes, we want no struggle, much cueing as necessary to reach 100% accuracy, practice, practice, practice
Space retrieval
like errorless learning, but increasing the time between stimulization of a question and a correct response from the client
Agitation
a state of heightened restlessness, irritability, or emotional distress
Constructional Impairment
neuropsychological disorder where a person has difficulty performing tasks that require organizing or assembling parts into a whole, despite having intact motor strength and coordination.
Narrative
Struggle with story telling, struggle with organization, because of damage to right hemisphere
Limb apraxia
motor planning disorder that affects the ability to perform purposeful movements with the arms or legs, even though muscle strength, coordination, and sensation are intact.
Intracranial hemorrhange
ICH - a type of stroke caused by bleeding directly into the brain
Malnutrition
occurs when the body does not receive the right amount of nutrients
Organic voice disorders
Caused by structural abnormalities
Nodules
Polyps
Cysts
Neurological voice disorders
Result from nerve damage or dysfunction
vocal fold paralysis
Functional voice disorders
No structural damage, but improper use of vocal mechanisms
MTD
Psychogenic voice disorders
Related to emotional or psychological factors
depression
anxiety
conversational aphonia
Epidemiology of voice disorders
Study of voice disorders helps us to treat and identify how the disorder happened
Phonation
Vibrating vocal folds producing acoustic pressure waves, the source of speech
Pitch
Perceptual measure of vocal fold vibrations per second
high vs. low
Frequency
Physical measurement of pitch, measured in Hz
high vs. low
Loudness
Perceptual measure of volume of sound pressure level
loud vs. soft
Intensity
Physical measurement of loudness, measured in dB
loud vs. soft
Distance between speaker and listener
Quality
A mix of tonal and atonal in the acoustic pressure wave produced by the vocal fold and sound pressure level
Variable based on speaker and culture
EX: Arabic speakers
Tonal
Pitch, resonance, and vocal quality
piano keys
Anosagnosia
Lack of awareness or insight into their own deficits
Atonal
Noise such as humming from an AC unit
Intubation
a tube is inserted into the trachea through the mouth or nose to maintain an open airway or to administer medical treatments
Dysphonia
Voice disorder, either perceived by others or by oneself
Aphonia
No voice
__ of people have reported a voice disorder at some point in past 12 months
6%
Voice disorders are more prevalent in...
1. Ppl with fam history
2. Women
3. Professional voice users
Why are women more prevalent in voice disoders?
1. Talk more
2. High pitch
3. Frequent pitch changes
4. Hormones
List professional voice users
1. Singers
2. Teachers
3. Athletes
Diagnosis of voice disorders
1. Physician evaluation
2. case history
3. Perceptual impressions of own voice
4. Viewing imaging of vocal folds
5. Measurement of phonatory parameters (F0, intensity, frequency, voice spectrum)
Why does there need to be a physician evaluation before SLPs work with voice disorders?
1. We must know the cause of the disorder in order to have a detailed treatment plan
2. If surgical intervention is needed, that must happen first
Fundamental frequency
1. Highest in kids
2. Related to the size of the larynx
3. Declines in childhood to puberty
4. The adult average is constant in males and females
5. Higher = higher pitch
Hypofunction voice disorder
breathy voice, vocal fold cycles are too slow to close
Hyperfunction voice disorder
Rough, tense voice, vocal fold cycles close too fast
Phonotrauma
Dysphonia due to excessive phonatory behaviors, resulting in damage to the vocal folds
Excessive phonatory behaviors
1. Chronic screaming
2. Overuse of high intensity
3. chronic throat clearing
4. chronic low-pitched
5. tense voice
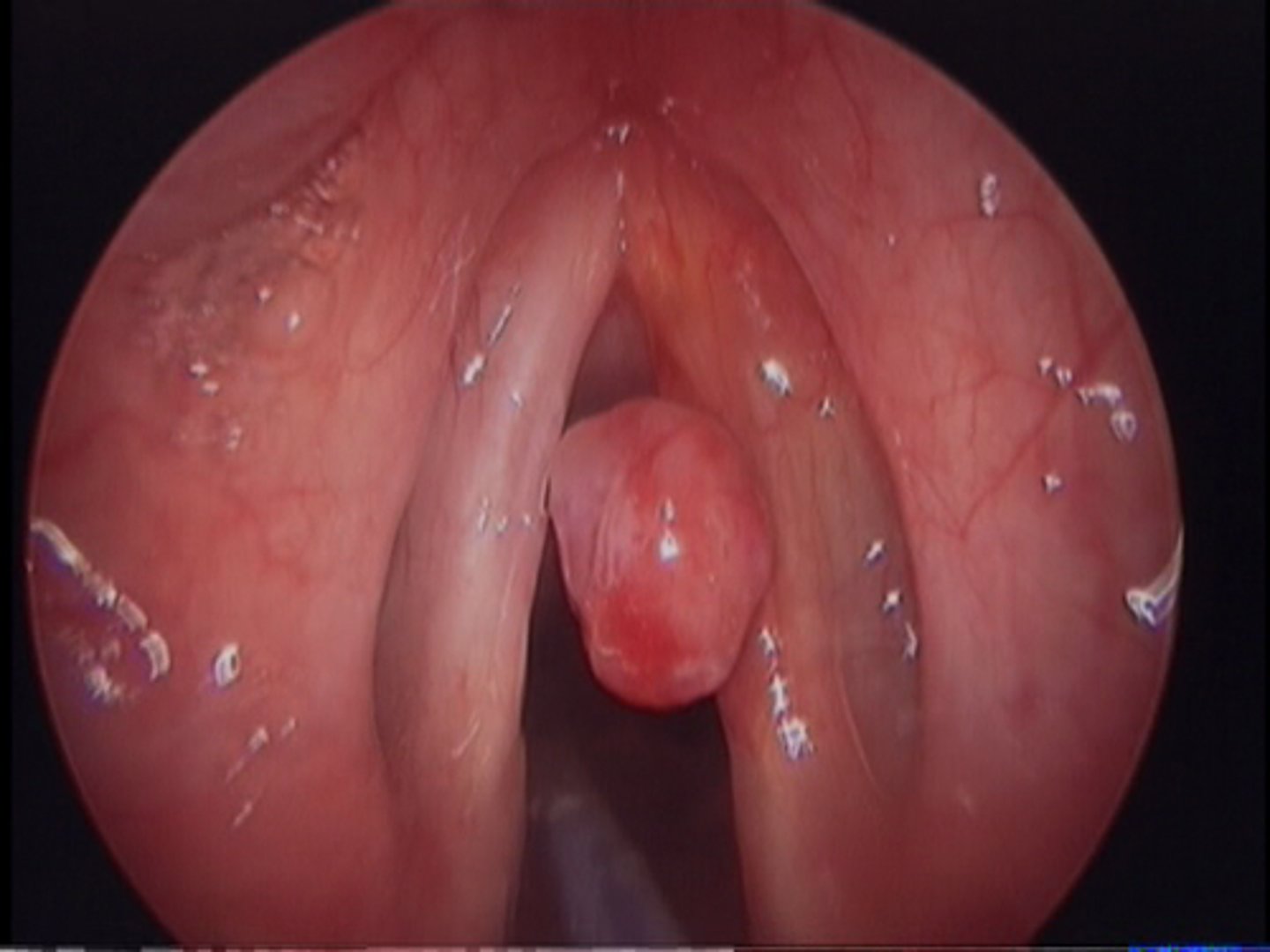
Healthy vocal folds

Vocal fold nodules
Benign masses resulting from chronic overuse
Begin soft, then turn callous texture
Occur bilaterally
Voice quality is breathy

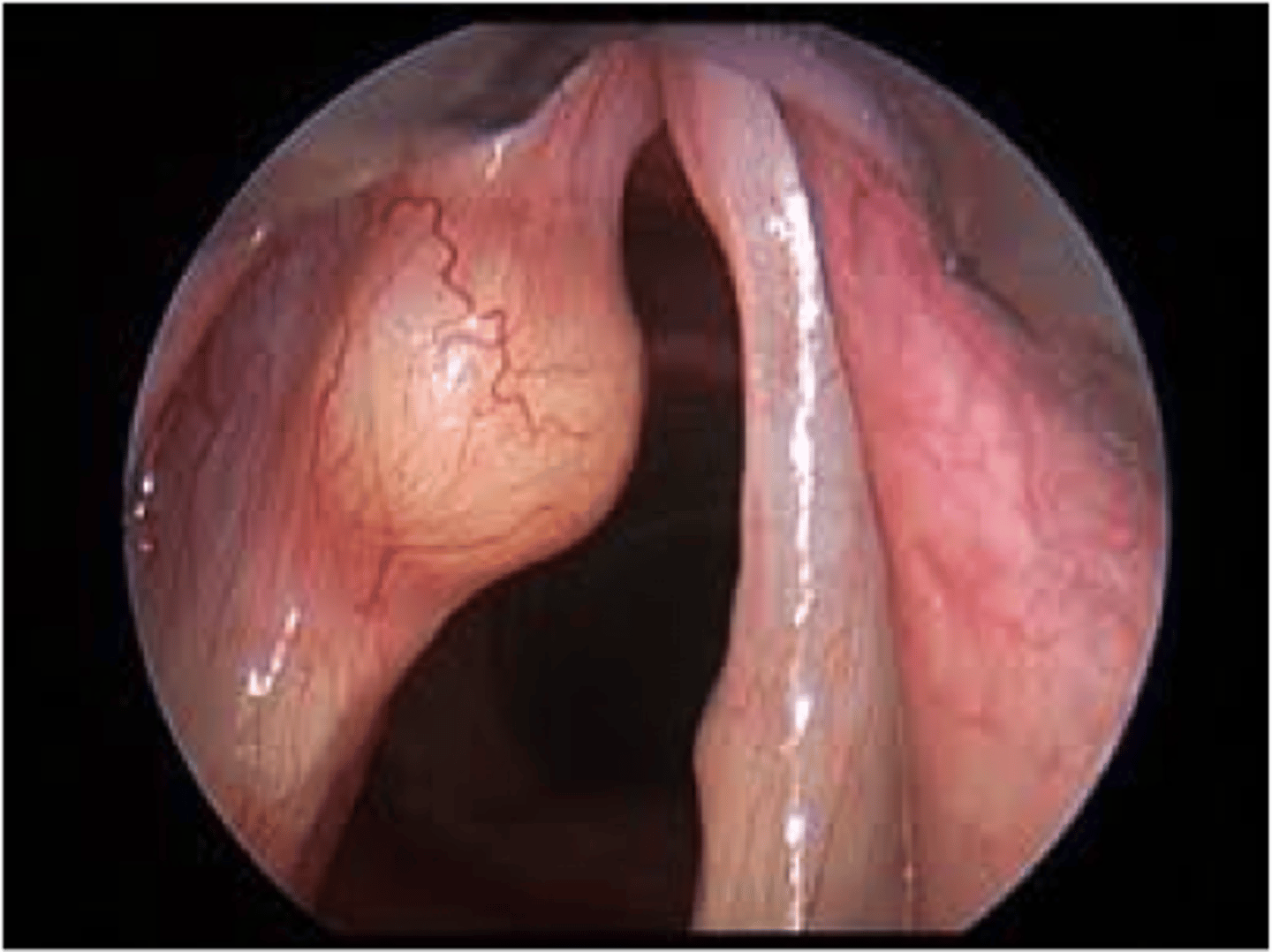
Vocal fold polyps
Softer than nodules, unilateral, can develop from a single scream
Laryngitis
Disturbs free motion of outer layers of vocal fold tissue, swelling
Chronic reflux
Acid on vocal folds, tobacco, alcohol
Vocal fold cysts
Fluid filled sac interfere with free motion of outer layer of vocal folds
Treatment of phonotrauma
For all, educate on vocal hygiene
Treatment of nodules
Vocal rest, may need surgery if unsuccessful
Treatment of polyps or cysts
Surgical removal, scar tissue can also become an issue after suergy
Acalculia
Loss of ability to perform simple arithmetic calculations, typically resulting from disease or injury to the parietal lobe of the brain.
treatment of laryngitis and reflux
Vocal hygiene for dysphonic episodes
Avoid straining voice
Teach them to use breath to increase volume
Arousal
The brain's ability to be awake, alert, and responsive to stimulation.
Lability
rapid shift of emotions
Manic
having the quality of excessive excitement, energy, and elation or irritability
MTD
Functional voice disorder (muscular tension dysphonia), excessive tension in the head and neck, is a functional voice disorder
Can occur at any age
60% women
Strained vocal quality
Aphonia
If diagnosed with MTD
1. Counseling for psychological issues
2. Direct voice therapy to reduce tension
3. Laryngeal massage
Unilateral vocal fold paralysis
Functional voice disorder that has injury to the nerve on one side of the larynx bc of trauma, injury of the nerve in surgery, or inflammatory disease
Breathy, strained, weak voice quality
Treatment for Unilateral vocal fold paralysis
Direct voice treatment or surgical intervention
1. Speech breathing with controlled effort exercises
2. Surgery: injecting biomaterials to plump folds to meet at midline or moving the fold into a permanent position at midline
Spasmodic dysphonia
Neurological voice disorder that is rare, intermittent, and irregular voice spasms, where phonation can be nonexistent or have tremors of the folds
Treatment for spasmodic dysphonia
1. Botox injections to reduce spasms
2. Counsel client to live with condition
Cancer of the larynx
Occurs anywhere in the larynx, more in men, changes in voice increase in severity over time, hoarse, rough, irregular voice quality
Treatment for cancer of the larynx
1. Surgery and radiation
2. Voice therapy
Pediatric voice disorders
1. 4-6% of kids
2. More common in boys under 12
3. Behavioral voice therapy for benign conditions
4. Educate on vocal hygiene
Compensatory strategies
Help the person eat what they can right now, but do not strengthen the swallowing system
Dysphagia
Inability to manage and swallow food/liquid appropriately
Observed by patient symptoms
1. Issues putting food in mouth
2. Coughing before, after or at the end of a meal
3. pneumonia
4. wet/gurgly voice
5. Feeling of food stuck
6. food refusal
7. Weight loss
8. Dehydration
9. Malnutrition
Dehydration
Lack of hydration/lubrication in vocal folds can cause voice disorder
Primary symptoms of dysphagia
Aspiration, penetration, residue, backflow
Aspiration
Food/liquid past the vocal folds into the vocal tract
epiglottis stops working, causing pneumonia
Penetration
food/liquid stuck in the laryngeal vestibule, does not drop below the folds
Residue
Any food/liquid that stays where it should not be after a swallow
Backflow
reflux from the stomach to the esophagus or into the larynx
Bolus
Food/liquid we are swallowing
Bolus feed
food/liquid that is inserted through a peg tube
Swallowing
Patterned response, reflexive, complex
Swallowing sequence
1. Medulla recognizes pattern of sensory and motor elements triggering swallow
2. Feedback from tongue helps trigger swallow
3. Input from both cerebral cortex and cerebellum responsible for coordination and timing of motor movements
Cranial nerves involved in swallowing
1. V Trigeminal
2. VII Facial
3. IX Glossopharyngeal
4. X Vagus
5. XI Accessory
6. XII Hypoglossal
V Trigeminal Nerve
Sensory - jaw, teeth, lips, cheeks, tongue, hard palate
Motor - chewing
VII Facial Nerve
Sensory - soft palate, taste anterior 2/3 tongue
Motor - superficial muscles of face, stylohyoid
IX Glossopharyngeal Nerve
Sensory - tonsils, pharynx, soft palate, taste, tactile posterior 1/3 tongue
Motor - pharyngeal elevators
Salvation and gag reflex
X Vagus Nerve
Sensory - larynx, pharynx, trachea, esophagus
Motor - intrinsic muscles of larynx, palatal muscles, pharynx
Swallowing
Runs all the way to stomach
XI Accessory Nerve
Motor - pharynx, extrinsic larynx, uvula
Swallowing
XII Hypoglossal Nerve
Motor - strap muscles of neck, extrinsic and intrinsic tongue muscles
Tongue movement
Neurogenic conditions
1. Stroke
2. Operable brin tumor
3. TBI
4. Dementia
5. Neurodegenerative disorders
6. Non-operable brain tumors
Stages of swallowing
1. Oral
2. Pharyngeal
3. Esophageal
Oral preparatory stage of swallowing
You have the food in your mouth, preparing to move food into the pharynx
Voluntarily eating
Rotary mastication
Teeth bite and chew
Mandible moves circular and opens
Saliva increases
Bolus formation via tongue movement
Velum drops down
Lips closed
Cheeks keep food in center of mouth
Duration varies based on what you eat
Positive pressure
Force from muscles compressing/pushing the bolus forward through the oral and pharyngeal cavities
Negative pressure
Region of lower pressure that helps draw the bolus forward
Structural Conditions
1. Head and neck cancer - stops and blocks food
2. Cricopharyngeal hypertrophy - overgrowth of muscle
3. Zenker's diverticulum - food stuck in pouch
4. Cervical neck disease - boney growths
Iatrogenic Conditions
Caused by the treatment
Tracheostomy
Ventilators
Drugs causing dry mouth, decreased sensation, taste, oral moisture
Post surgical nerve damage
Psychiatric/Behavioral Conditions
Globus pharynges - feeling like lump in throat
Delirium - physical or mental illness (UTIs or mania)
Alcohol
Systemic Conditions
Myositis - autoimmune disease-causing muscle inflammation
HIV/AIDS - mouth, throat, tongue sores or yeast infections of the mouth
Esophageal causes - GERD
Oral transit stage of swallowing
When the food leaves the mouth, tongue pushes up on hard palate to send food back and down the pharynx
Voluntary
Jaw and lips closed
tongue tip strips back on alveolar ridge
Breathing in and out
Peristaltic tongue motion
Bolus reaches anterior faucial pillar
Bolus enters pharynx
Pharyngeal stage of swallowing
Swallow is triggered
Pharyngeal stage of swallowing pharynx components
Moves bolus to upper esophageal sphincter
1. Velum elevates to block off nose
2. Pharyngeal walls squeeze in
3. Bolus pulled by negative pressure
4. Tongue pushes bolus to propel into pharynx, base of tongue is down
5. Muscles contract in wave from top to bottom naso-hypo pharynx
6. Ends when upper esophageal sphincter is in esophagus