Foot & Ankle Disorders
1/75
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
76 Terms
how do ankle sprains most often occur?
as a result of a twisting injury of the ankle
- inversion & plantarflexion are the most common
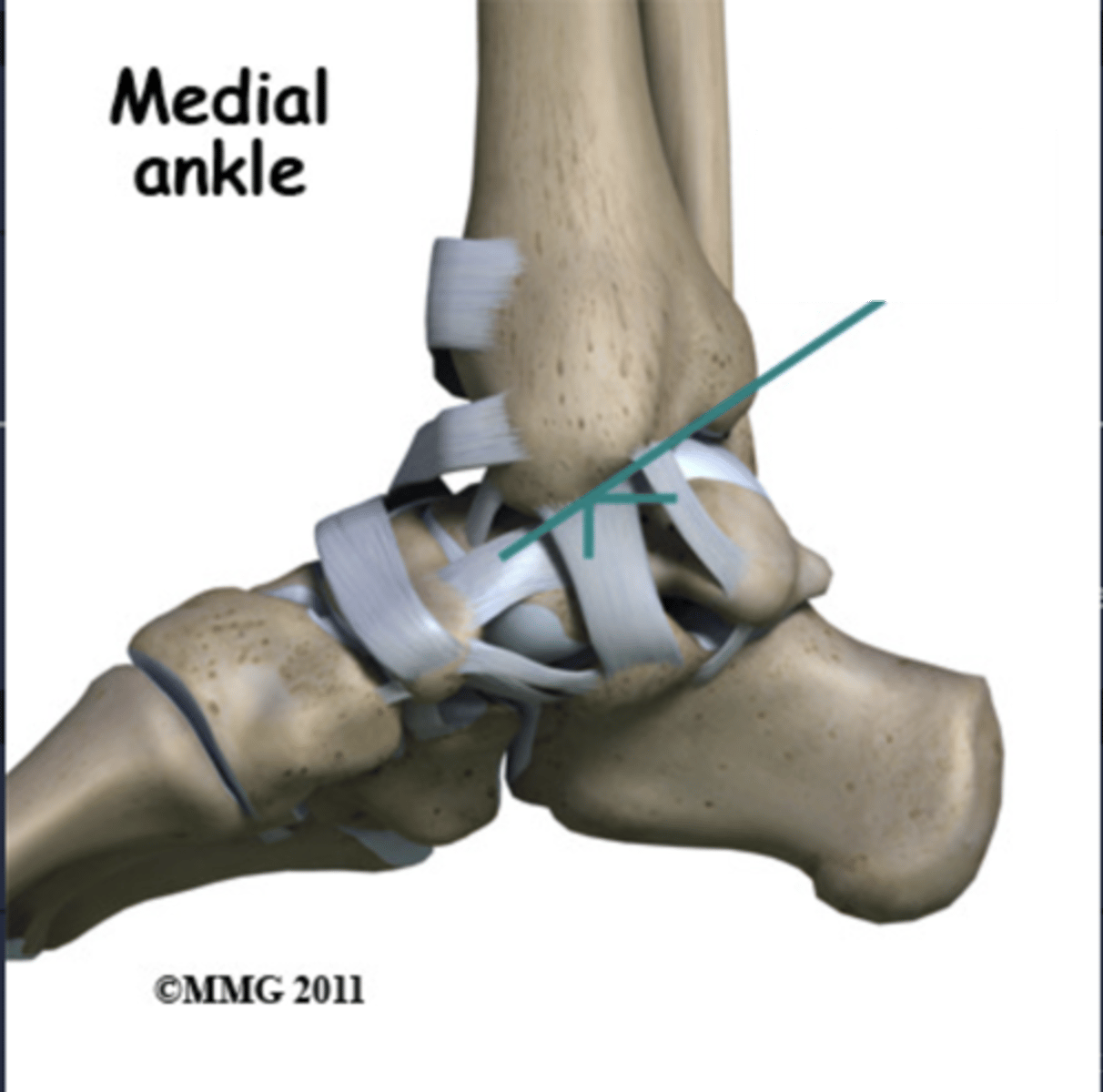
___________ ligament can be injured in eversion injuries
deltoid
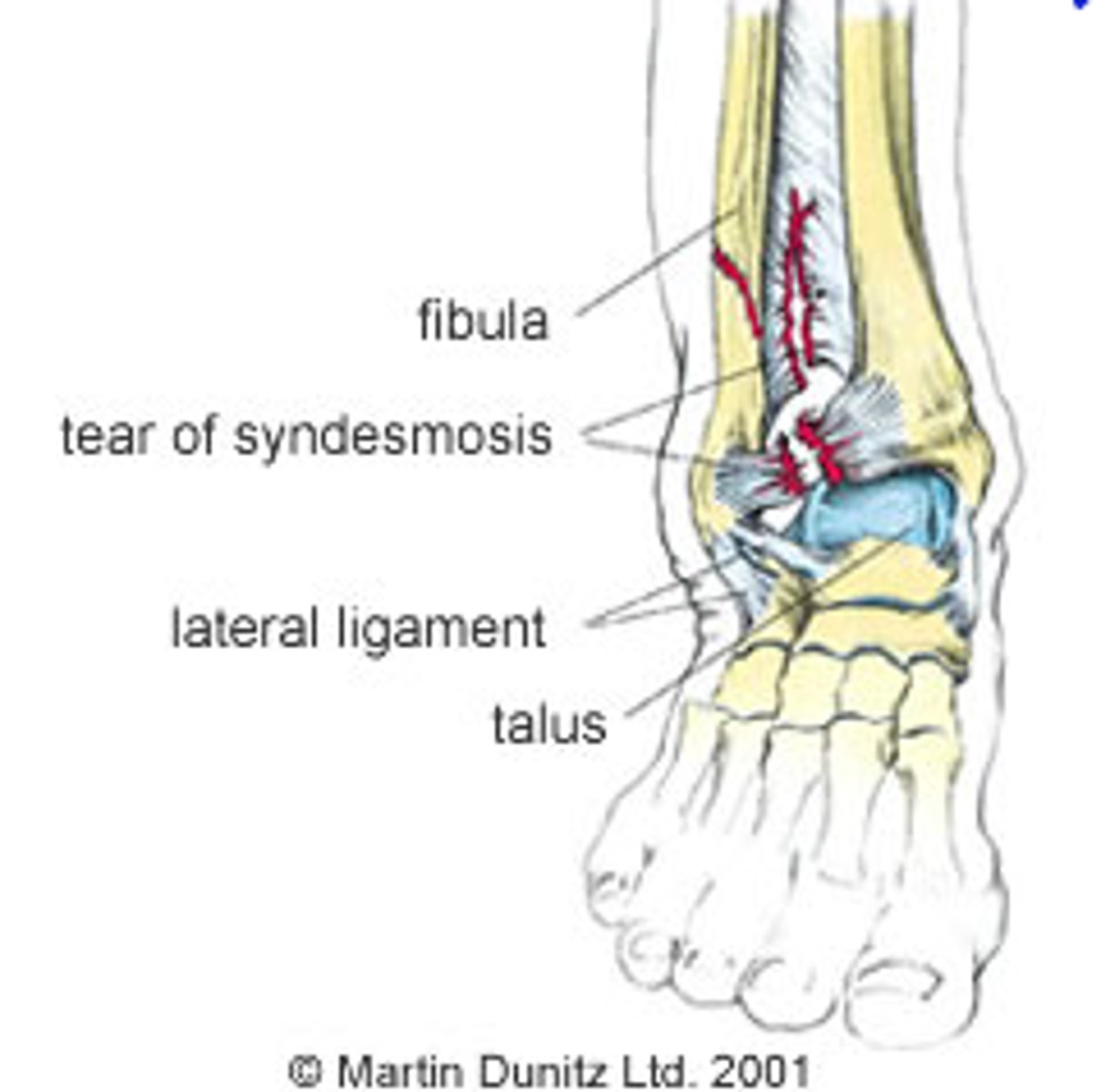
what is a high ankle sprain?
involves the syndesmotic ligaments between the tibia & fibula
- < 10% of all sprains
- take longer to heal
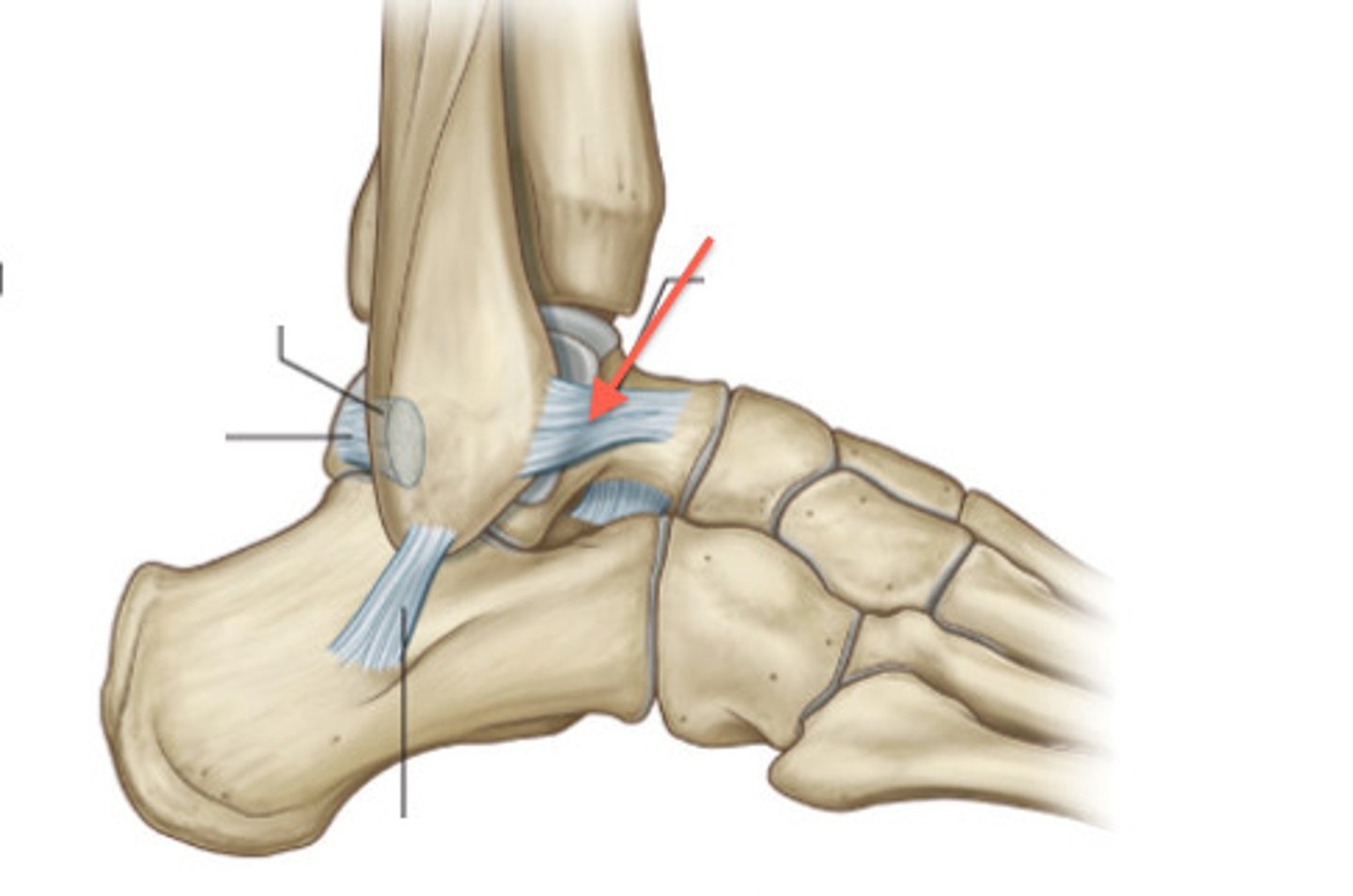
what is the primary function of the anterior talofibular ligament (ATFL)?
resistance of translational motion of the talus in the sagittal plane
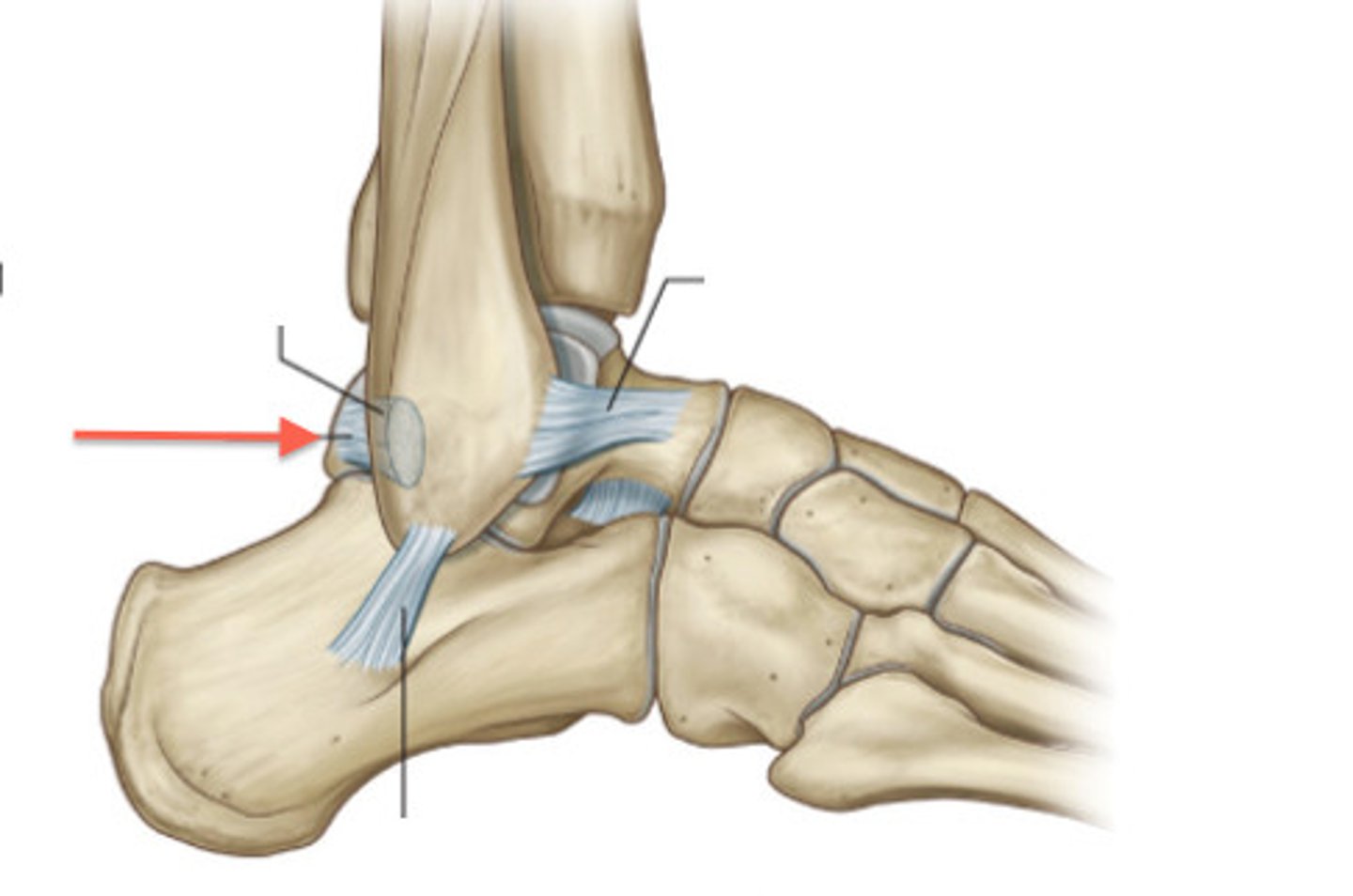
what is the primary function of the posterior talofibular ligament (PTFL)?
resistance to inversion & external rotation
- strong
which is the most commonly injured ligament?
a. ATFL
b. PTFL
a. ATFL
1 multiple choice option
why is the ATFL the most commonly injured ligament?
due to biomechanics of the foot/ankle, inversion/plantarflexion
- energy moves in line w/ this ligament
- lowest threshold for failure
s/s of an ankle sprain:
- pain & tenderness, usually over the lateral ankle (can occasionally occur over medial ankle)
- possible pain w/ weight bearing
- bruising or swelling over the lateral ankle which may extend into foot
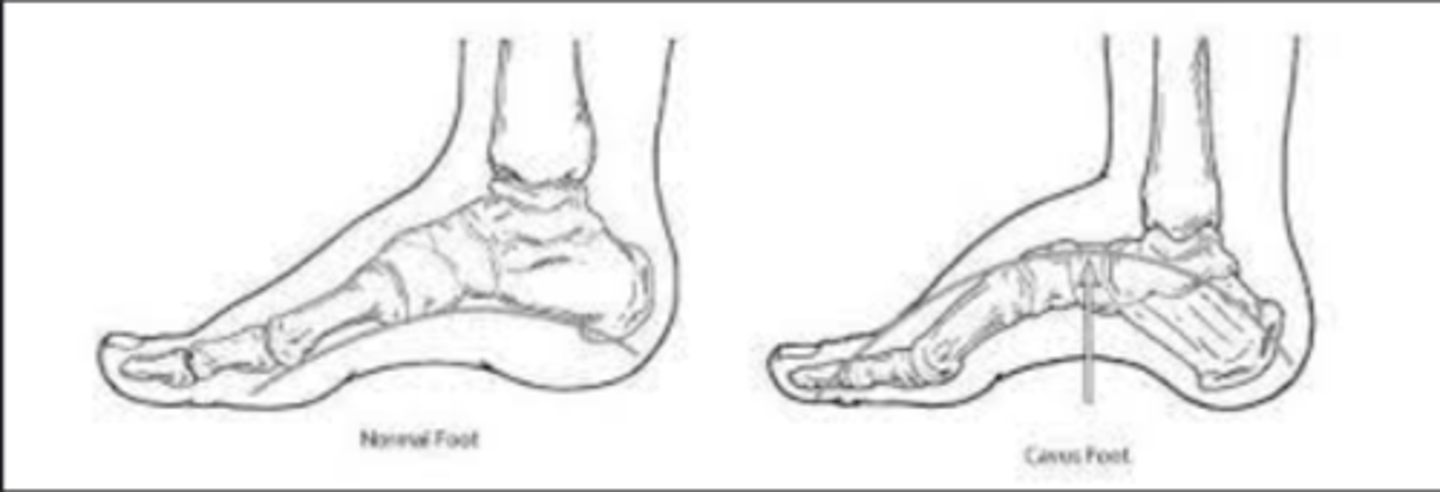
what foot deformity predisposes the ankle to recurrent ankle sprains?
cavovarus foot
- arch of foot is higher than normal, & heel turns inward
possible associated injuries w/ an ankle sprain:
- osteochondral injuries (damage to the joint surface of the talar dome at time of injury)
- peroneal tendon injuries (pain w/ palpation over tendons or w/ stressing of tendons)
- other fractures
what is a snowboarder's fracture?
fracture of the lateral process of the talus

what is the squeeze test?
grasp the patient's leg midway up the calf, compress & release motion
+ = patient experiences pain in the area of the syndesmosis
what are the ottawa ankle rules?
get XRs if any of the below are true (3 standard views):
- inability to bear weight
- medial or lateral malleolus point tenderness
- 5th metatarsal base tenderness
- navicular tenderness
what is the role of MRI in ankle sprain?
rarely used acutely
- do if OCD or tendon injury is suspected
- will show ligament injury
- won't change treatment in any way
- may be indicated if pain persists after 8 wks of appropriate treatment
how are ankle sprains treated?
- initially: RICE
- if severe: 1-2 wks of weight bearing immobilization in a CAM boot or walking cast (early immobilization is helpful)
- after pain subsides: PT (ROM, strengthening, proprioceptive training)
- prophylactic: bracing
- refer if not better in 8 wks
- last resort: surgery
what leads to the best results for ankle sprain therapy?
early functional rehab
which is better?
a. lace-up ankle brace
b. stirrup ankle brace
a. lace-up ankle brace
1 multiple choice option
the vast majority of ankle sprains heal w/o sequelae, but what can they result in?
chronic instability of the ankle
what is the largest tendon in the body?
achilles tendon
- formed by the confluence of the soleus & gastrocnemius tendons
what is the primary (but NOT only) plantarflexor of the ankle?
achilles tendon
what is the function of the achilles tendon?
storage of elastic energy during gait cycle, jumping & running
risk factors for achilles tendon injuries:
- men > women
- age 30-40
- "weekend warriors," episodic athletes
- quinolone antibiotics & steroid injections
should you ever inject steroids near the achilles?
NO
1 multiple choice option
s/s of achilles tendon injury:
- hx of traumatic inury
- "somebody kicked me in the back of the leg" or "somebody shot me"
- pain in heel/posterior lower leg
- weakness in ankle (difficulty walking or climbing stairs)
- limp
- CAN still plantarflex the foot
- inability to single stance toe rise
- palpable defect in tendon
- possible bruising
what are the 2 tests that almost always catch an achilles injury?
1. lay patient prone on exam table w/ legs bent at 90º; compare resting position of the 2 feet (if completely ruptured, the foot will be more dorsiflexed)
2. thompson test: squeeze calf muscles (foot will move if tendon is intact; foot will NOT move or will move minimally if it's ruptured)
if these 2 are negative: partial tear, strain, or gastrocsoleus tear still possible
___________ tendon rupture can mimic achilles injury
plantaris
how are achilles tendon injuries treated?
- if rupture is diagnosed (or even suspected): REFER! (the sooner the better)
- non-surgical or surgical
what is the nonoperative treatment of achilles tendon injury?
serial casting or bracing in plantarflexion w/ progressive return to neutral
- may be preferred for medically frail or sedentary patients
- fewer wound & nerve complications
- possible higher rate of re-rupture
- difficult to do correctly
what is the operative treatment of achilles tendon injury?
open repair or percutaneous
- higher incidence of wound complications & sural nerve injury
- possible lower rate of re-rupture
- more reliable outcome
what is the most common cause of heel pain?
plantar fasciitis
what is plantar fasciitis?
inflammation of the plantar fascia, usually at its origin from the calcaneus
- chronic overuse which leads to microtears
risk factors for plantar fasciitis:
- high BMI
- long hours of standing on hard surfaces
- pes planus or cavus
- achilles contracture
how can achilles contracture lead to plantar fasciitis?
- loads fascia earlier in gait cycle
- increases plantarflexion force during gait cycle
- stresses fascia
achilles contracture = there is increased tension on the achilles tendon, so it is shorter and tigher
do heel spurs cause plantar fasciitis?
NO
acceptable if the spur is pointing forward (in the direction of the plantar fascia). it is trying to help mediate the current issue.
1 multiple choice option
s/s of plantar fasciitis:
- insidious onset
- start up pain (first steps out of bed or after prolonged sitting)
- usually worse by end of day
- anteromedial plantar heel pain
- dorsiflexion of toes may worsen pain
what is the role of an EMG or NCV test in diagnosis of plantar fasciitis?
to r/o tarsal tunnel or radiculopathy
how is plantar fasciitis treated?
- stretching, both fascia & achilles (1st thing in the morning before arising & 5-6 times per day)
- night splint (keep achilles stretched & prevent shortening of fascia overnight)
- ice massage 2-3 times daily
- orthotics (arch support w/ heel padding; consider moldable heel cup)
- NSAIDs
- PT
- walking cast immobilization for 4-6 wks
- surgery (last resort)
- shock wave therapy (controversial)
- plantar fascia partial release or gastrocnemius release
should you do steroid injections for plantar fasciitis?
NO
this can result in rupture of the plantar fascia… would result in pt being non weight bearing for up to 3 months (theoretically, this would resolve the underlying issue of the tight plantar fascia… but at such an inconvenient cost that it is not worth it)
1 multiple choice option
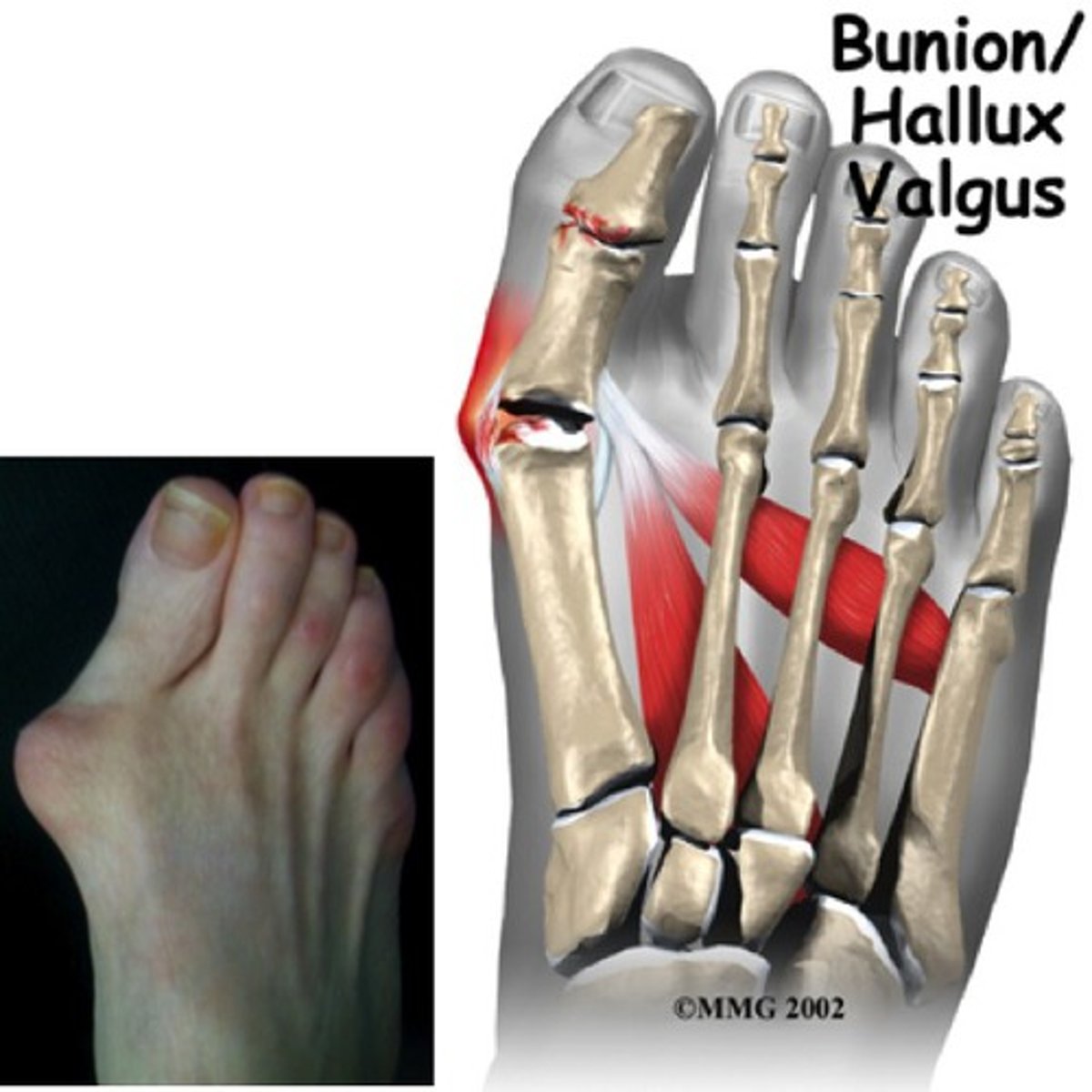
what is hallux valgus (bunion)?
lateral deviation of the great toe w/ medial deviation of the 1st metatarsal
- associated conditions: calluses or hammer toe
what are the risk factors for hallux valgus?
intrinsic:
- genetics
- convex metatarsal head
- pes planus
- RA
- cerebral palsy
extrinsic:
- shoes w/ high heel or narrow toe box
s/s of hallux valgus:
- shoes irritate area due to eminence
- pain over prominence at MTP joint
- cosmetic concerns
- pain underneath the 2nd metatarsal head
- compression of digital nerve
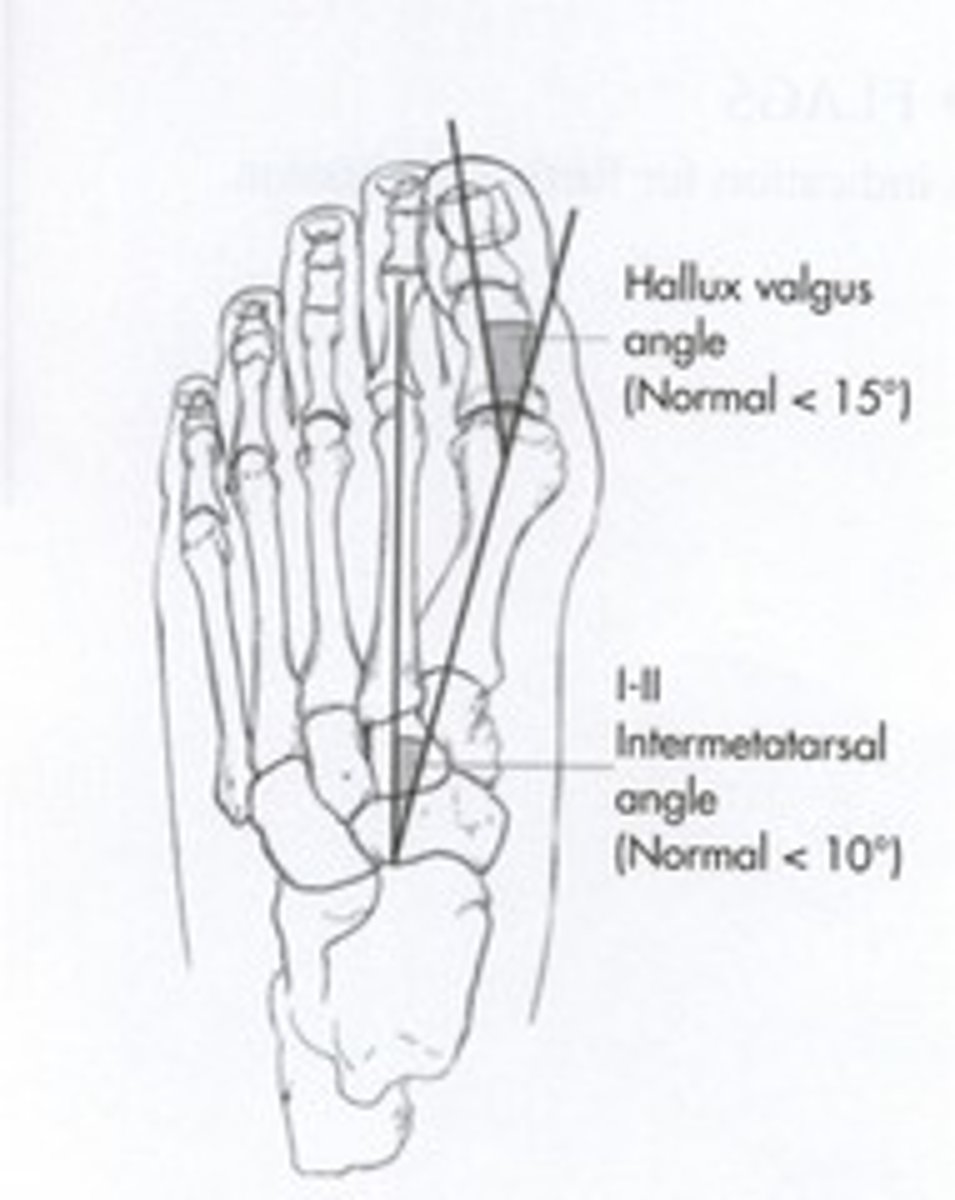
what is the normal 1st & 2nd intermetatarsal angle?
< 10º
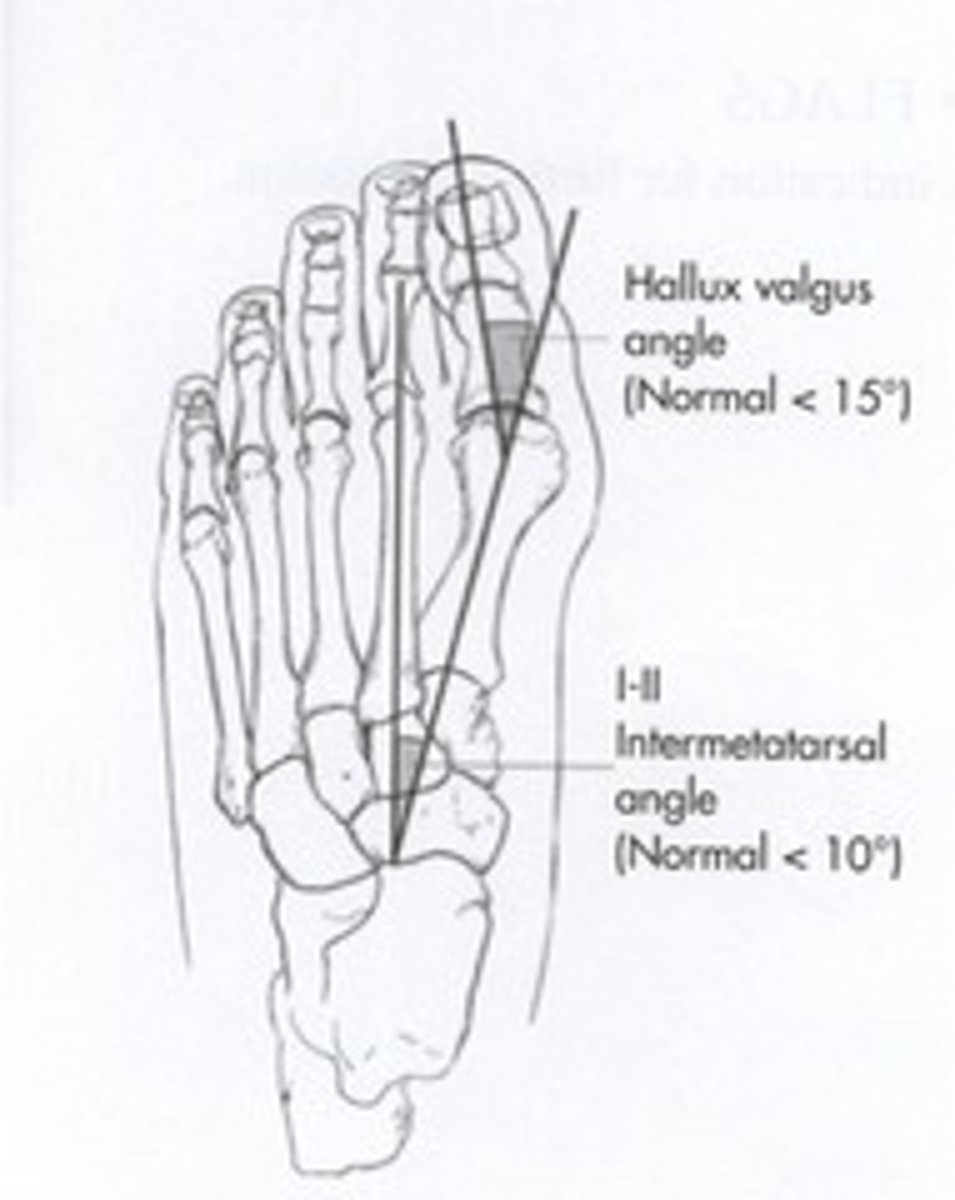
what is the normal hallux valgus angle?
< 15
how is hallux valgus treated?
- 1st line = conservative, shoe modification, exercises, activity adjustments, orthoses
- surgery if sx present w/ secondary deformities & shoe modification fails (NOT for cosmetic reasons alone)
what is hallux rigidus?
a benign BONY GROWTHs involving the 1st metatarsal phalangeal joint
- can be due to: arthritis, trauma, or overuse
s/s of hallux rigidus:
- painful, reduced ROM
- bony prominence dorsally
- can be associated w/ hallux valgus
how is hallux rigidus treated?
- stiffer shoes (to limit the dorsiflexion of the toes that occurs naturally as we walk)
- forefoot shank
- surgical debridement of the spurs
what is metatarsalgia?
a general term used to describe pain in the ball of the foot
NOT ALL FOREFOOT PAIN IS A ________________________!
MORTON'S NEUROMA
what is the most common cause of metatarsalgia?
mechanical overload that results in capsulitis
- predisposed by: tight achilles, cavus foot, age-related fat pad atrophy, prolonged standing on hard surfaces, toe deformities, poor shoe wear (high heels!)
which toe is most commonly affect by metatarsalgia?
2nd toe
- longest in many people
3 multiple choice options
if pain is reproduced by palpation under the metatarsal heads, this indicates:
a. metatarsalgia
b. morton's neuroma
a. metatarsalgia
1 multiple choice option
how is metatarsalgia treated?
- shoewear/activity modifications
- achilles stretching or possible lengthening
- corrective insole or surgery for cavovarus foot
- surgical correction of deformities (hallux, valgus, clawed toe, weil or dorsal wedge osteotomy of the metatarsal head)
what is morton's neuroma?
compressive neuropathy of the interdigital nerve
- perineural fibrosis & entrapment of the interdigital nerve, probably due to repetitive microtrauma
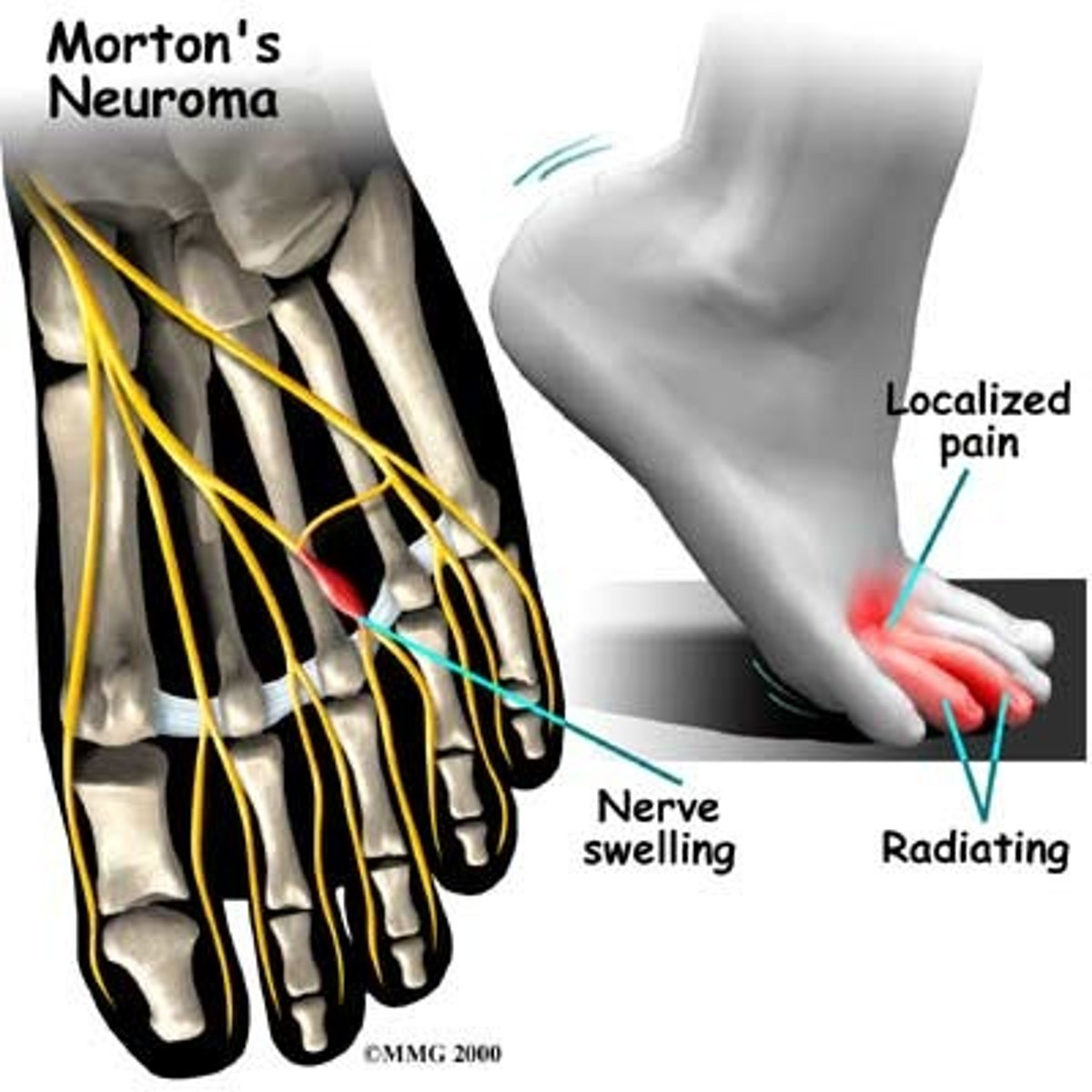
s/s of morton's neuroma:
- pain & paresthesia in plantar aspect of webspace ("wrinkle in my sock")
- worse w/ weight bearing & tight or high heeled shoes
- relieved by removing shoes & massaging foot
- neuroma may be palpable in web space, deep to the transverse metatarsal ligament
- provocative testing
what are the provocative tests for morton's neuroma?
- compression of webspace while compressing the metatarsal heads together
- mulder's click (palpable click & pop w/ lateral compression of metatarsals w/ reproduction of sx)
what is mulder's click?
palpable click & pop w/ lateral compression of metatarsals w/ reproduction of sx
- indicates a morton's neuroma
how are morton's neuromas treated?
- wide toe box shoes, MT pad orthotic
- steroid injection
- surgery (will leave permanent numbness of webspace)
types of ankle fractures:
- single malleolus
- bimalleolar
- trimalleolar
when a single malleolus is fractured, which is most commonly affected?
a. lateral
b. medial
c. posterior
a. lateral
2 multiple choice options
when a single malleolus is fractured, which is least commonly affected?
a. lateral
b. medial
c. posterior
c. posterior
2 multiple choice options
when 2 malleoli are fractured, it is most commonly the..
medial & lateral
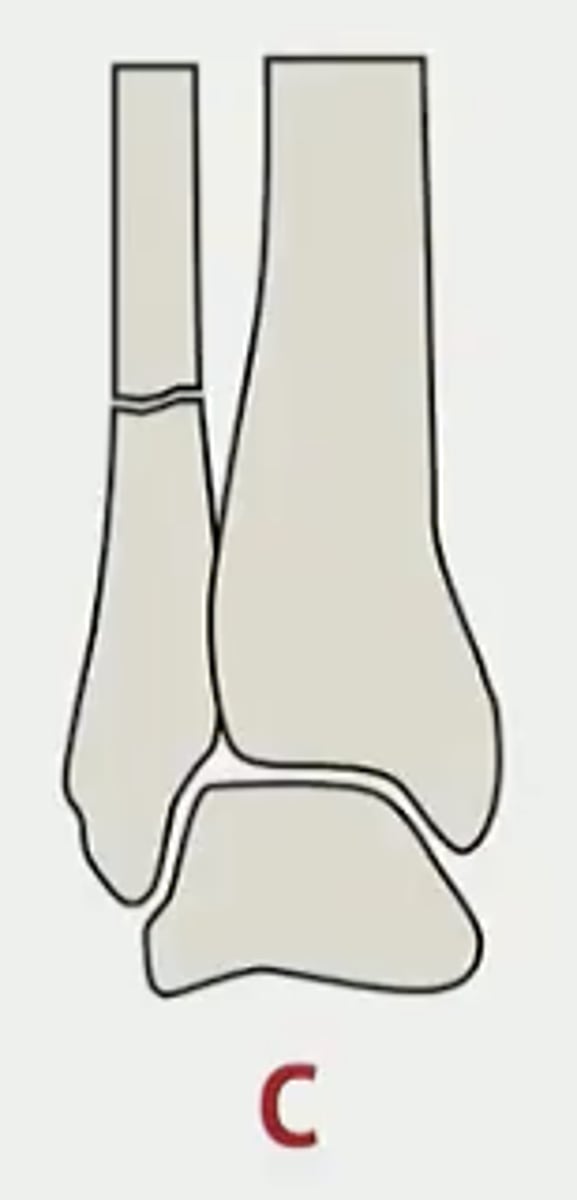
weber classification of LATERAL ankle fractures:
A: fracture below the talar dome
B: fracture begins below the talar dome & continues obliquely proximally
C: fracture is above the talar dome
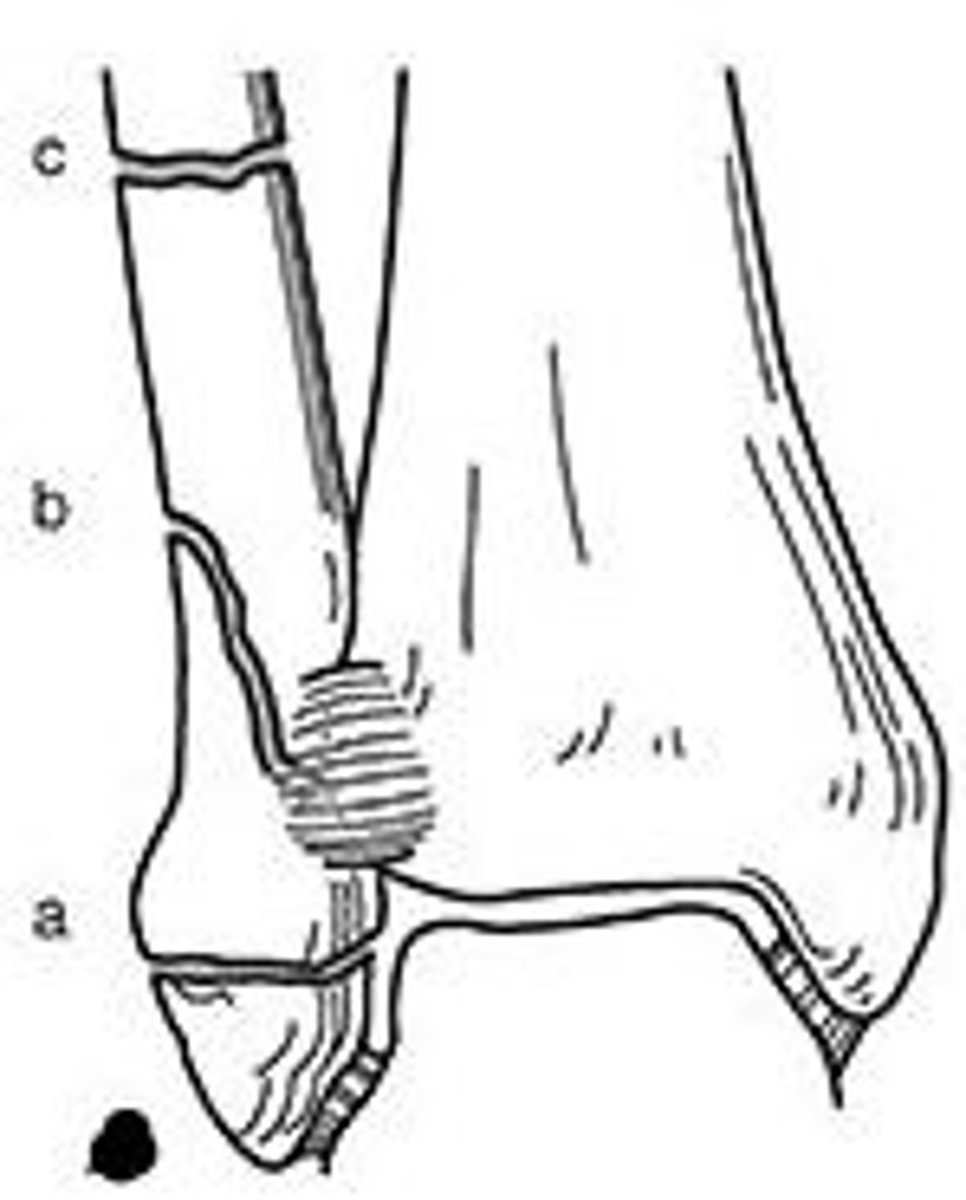
weber A ankle fracture
fracture is below talar dome
- if fragment is minimally displaced, can treat w/ casting
- screw fixation is sometimes needed
generally NO surgery

weber B ankle fracture
fracture begins at the talar dome & continues obliquely proximally
- usually displaced enough to require open reduction w/ internal fixation (ORIF)
- if non-displaced in a compliant patient, may elect to treat w/ casting & NWB
MAYBE surgery

weber C ankle fracture
fracture is above the talar dome
- inherently unstable due to syndesmotic ligament disruption
- requires surgical fixation, often w/ syndesmotic screw placement
YES always surgery
how are medial ankle fractures treated?
possibly conservatively w/ casting
- typically best to refer to ortho as there is a high chance of syndesmotic injury
NOT ALL PROXIMAL 5TH METATARSAL FRACTURES ARE ________ FRACTURES!
JONES
an acute fracture has:
a. sharp & pointy edges
b. rounded edges
a. sharp & pointy edges
1 multiple choice option
if the 5th metatarsal fracture GOES INTO THE JOINT, is it considered a JONES fracture?
no
1 multiple choice option
what are the 3 basic types of 5th metatarsal base fractures?
- avulsion of the tuberosity
- intra-articular
- jones
can also have shaft fractures distal to the proximal third
what is a jones fracture?
fracture of the base of the 5th metatarsal
- occur in a vascular "watershed" area
- much more likely to produce a delayed union or nonunion due to the vascular anatomy of the area
- DOES NOT EXTEND INTO THE JOINT
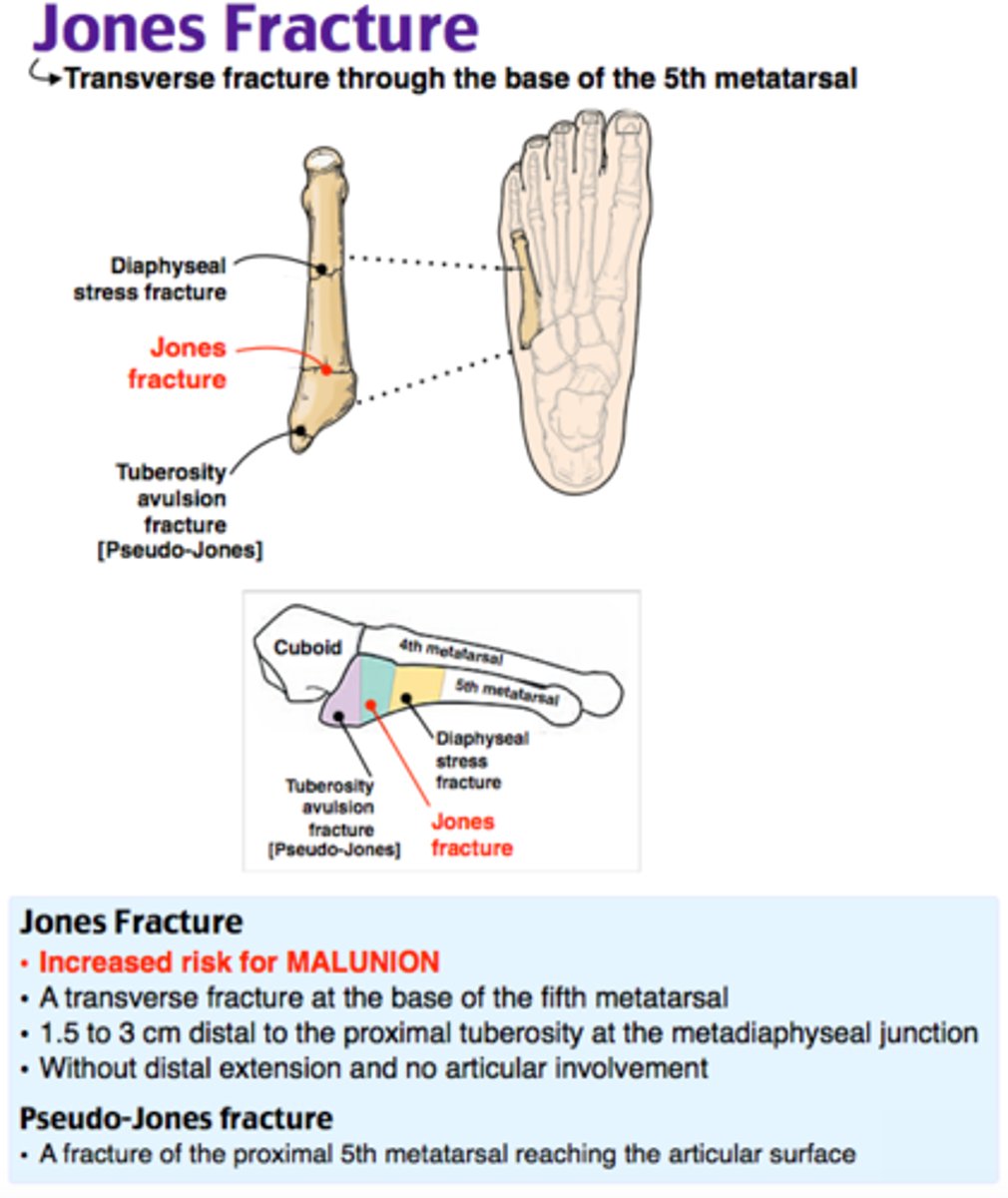
how are jones fractures treated?
- nonoperative treatment only appropriate for completely nondisplaced fracture in low demand patients (NWB for a minimum of 6-7 wks w/ careful follow-up)
- 90%+ need operative fixation
- if in doubt, REFER!
which metatarsal are stress fractures most commonly seen in?
similar to metatarsalgia, 2nd bc it's the longest
3 multiple choice options
how are stress fractures treated?
- CAM boot or post-op shoe
- f/u XRs in 2 wks (look for bony callus)
phalange fractures
hx of trauma; present w/ pain & bruising
- if no deformity, buddy tapping for 4-6 wks until healed
- if deformity present, consider digital block w/ reduction (pre & post reduction films required)