Chapter 27: Fractures
1/12
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
13 Terms
Chapter 27: Fractures
When the force on a bone exceeds its strength, causing a break in its structure.
Healing in Children:
Faster healing than adults.
Due to a thicker periosteum and better blood supply.
Growth Plate (Epiphyseal Plate) Injuries:
Can affect bone growth.
Require careful monitoring to avoid long-term complications.
Red Flag for Abuse or Disorders:
Multiple fractures in different healing stages (especially in infants) may indicate:
Non-accidental trauma (abuse)
Osteogenesis imperfecta (brittle bone disease)
Fractures in Children S/S
Pain
Crepitus (grating sound or sensation)
Visible deformity
Edema (swelling)
Ecchymosis (bruising)
Decreased use of injured area
Fractures in Children Medications
Analgesics (e.g., opioids)
Immunizations (tetanus for open)
Antibiotics (for open)
Fractures in Children
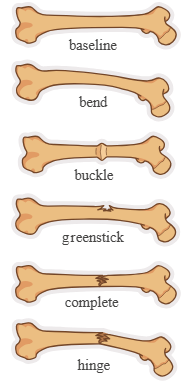
Types
Plastic deformation (bend): Bone bends ≤ 45° without breaking.
Buckle (torus): Bulge or raised area from compressed bone.
Greenstick: Incomplete break.
Transverse: Break straight across the bone.
Oblique: Diagonal break.
Spiral: Twisting break around the bone.
Physeal (growth plate): Break at the end of a long bone.
Stress: Tiny cracks from repetitive stress (e.g., sports or weight-bearing activities).
Complete: Bone fragments are separated.
Incomplete: Bone fragments are still attached.
Closed or simple: The fracture occurs without a break in the skin.
Open or compound: The fracture occurs with an open wound and bone protruding.
Complicated fracture: The fracture results in injury to other organs and tissues.
Comminuted: The fracture includes small fragments of bone that lie in surrounding tissue.
Risk Factors
Obesity
Poor nutrition
Normal play activities or sports that involve running, climbing, jumping (e.g., skateboarding, skiing, soccer, basketball)
Fractures in Children Management
General Interventions
Assess pain often; use age-appropriate pain scale
Monitor neurovascular status regularly
Maintain bone alignment
Encourage movement of unaffected fingers/toes
Teach activity restrictions
Provide comfort and reassurance
Emergency Care at Time of Injury
Get a history of the injury
Maintain ABCs (Airway, Breathing, Circulation)
Monitor vitals, pain, neuro status
Check neurovascular status of the injured limb
Positioning:
Supine: for leg, pelvis, or lower arm injuries
Sitting: for shoulder or upper arm injuries
Remove jewelry near injury site
Stabilize injury to prevent movement
Splint above and below injury
Monitor for shock (esp. with pelvic fractures)
Elevate injury and apply ice (max 20 minutes)
Administer pain meds
Keep child warm
Neurovascular Assessment (6 P’s)
Sensation: Check for numbness or tingling
Skin Temperature: Should be warm, not cool
Skin Color: Look for changes (pale, blue, etc.)
Capillary Refill: Press nail beds—should return pink in ≤ 3 seconds
Pulses: Compare with unaffected limb; should be strong and equal
Movement: Fingers/toes distal to the injury should move normally
Fractures in Children Dx
Radiograph (X-ray):
Confirms fracture and bone alignment
Nursing Action: Help the child remain still during the procedure
Fractures in Children Therapy: Casting
Purpose:
Immobilize injury
Maintain bone alignment
Promote healing of fractures
Types:
Long-leg, short-leg, bilateral long-leg
Long-arm, short-arm
Shoulder spica, 1½ spica, full spica, single spica
Materials:
Plaster of Paris: Heavy, not water-resistant, dries in 10–72 hrs
Fiberglass: Light, water-resistant, dries in 5–20 mins
Before:
Inspect and clean the skin
Apply stockinette or waterproof liner
Pad bony areas to prevent breakdown
Nursing Actions
Use age-appropriate teaching (toys, dolls)
Check neurovascular status regularly
Elevate casted area for 24–48 hrs
Apply ice for the first 24 hrs to reduce swelling
Reposition every 2 hrs to dry the cast evenly
Avoid heat lamps or hair dryers
Use sling or pillow for support
Mark and monitor any drainage on cast
Check skin around the edges of the cast
Keep skin clean and dry
Petal rough cast edges with moleskin
Cover cast when near urine/feces
Teach proper crutch use
Client Education
Cast may feel warm when applied but won’t burn
Report severe pain or pain not relieved 1 hr after meds
Teach how to do neurovascular checks
Review proper crutch use
Instruct on perineal care for spica cast
Do NOT insert objects into the cast
Use proper restraints during transport
Teach about cast removal and cutter
Report soft spots, increased pain, or changes in sensation
Clean soiled skin with damp cloth
Soak extremity in warm water after cast removal
Fractures in Children Therapy: Traction
Purpose:
To immobilize a fracture, reduce dislocation, maintain bone alignment, and relieve muscle spasms using pulling force.
Types:
Skin:
Uses weights with tape/straps on skin (e.g., Buck, Russell, Bryant traction).
Skeletal:
Pins/rods inserted into bone; stronger force than skin traction.
Pulley system applies continuous traction.
Weights must not be removed by the nurse.
Halo (cervical):
Metal halo around head attached to vest or bed for neck/spinal injuries.
Manual:
Hand-applied during casting or reduction by the provider.
Nursing Actions
Maintain proper body alignment.
Give pain/spasm medications (pharmacologic + nonpharmacologic).
Report unrelieved severe spasms.
Monitor neurovascular status (pulses, cap refill, sensation, movement).
Check skin and pin sites (redness, swelling, drainage).
Monitor elimination patterns (urine/stool).
Ensure bed and hardware are secure and knots don’t touch pulley.
Do not adjust weights or equipment unless ordered.
Use overbed trapeze to help child reposition.
Encourage range of motion on non-immobilized limbs.
Promote deep breathing with incentive spirometry.
Reposition frequently to avoid skin breakdown.
Use pressure-relieving mattresses if needed.
Fractures in Children Therapy: Surgery
When needed
Common for supracondylar, humerus, and femur fractures.
Types of reductions:
Closed reduction: No incision.
Open reduction: Requires incision, possibly with pins.
Distraction: External fixator used to:
Immobilize fracture
Correct deformities
Lengthen bone
Nursing Actions
Monitor incision site for infection.
Encourage early mobilization (as ordered).
Administer pain medications.
Teach crutch use for lower limb fractures.
Educate on limited weight-bearing for affected limb.
Pre-Op & Immediate Post-Op:
Explain procedure expectations, including NPO instructions.
Emphasize infection monitoring.
Discuss pain control.
After Discharge:
Teach cast and pin care (if applicable).
Perform neurovascular checks and know when to call the provider.
Use anti-itch medications if prescribed.
Follow all physical restrictions.
Teach proper pain management.
Report signs of infection (redness, swelling, fever).
Encourage follow-up appointments.
Fracture Complications
Compartment Syndrome
Cause: Tight casts, traction, trauma, burns, surgery, hemorrhage, IV infiltration.
Patho: Increased pressure in a muscle compartment leads to:
Nerve/blood vessel compression
Ischemia
Common in tibial or forearm fractures
If untreated: Can lead to deformity, paralysis, or infection.
Volkmann Contracture: Permanent hand/forearm deformity from compartment syndrome.
Key Findings: "5 P's"
Pain (not relieved by meds or elevation)
Paresthesia (tingling/numbness)
Pulselessness (late sign)
Paralysis (nerve damage)
Pallor (cold, pale skin, cyanosis)
Nursing Actions
Assess hourly for first 24 hours
Ensure space for 1 finger between skin and cast
Report signs immediately
Avoid elevation
Loosen dressings
Prepare for fasciotomy if needed
Client Education
Report pain not relieved by meds or worsening pain
Watch for color change or numbness
Renal Calculi (Kidney Stones)
Cause: From immobility or poor hydration during non-weight-bearing
Nursing Action: Encourage fluids, monitor urine output
Fat Embolism
Fat from bone marrow enters bloodstream after long bone fracture
Pulmonary Embolism
Clot from injury site travels to lungs
Nursing Actions
Monitor for chest pain and difficulty breathing
Notify provider if suspected
Give anticoagulants and oxygen
Promote movement (active/passive ROM)
Elevate HOB
Apply SCDs (compression devices)
Osteomyelitis
Bone infection caused by bacteria from
External source (e.g., open fracture)
Bloodstream (hematogenous spread)
Key Manifestations
Irritability
Fever
Fast heart rate (tachycardia)
Edema (swelling)
Constant pain, worse with movement
Avoids using the affected limb
Infection site: tender, swollen, warm to touch
Nursing Actions
Assist with diagnostic testing (blood, skin, bone cultures)
Assist with joint/bone biopsy
Give IV and oral antibiotics
Monitor liver, kidney, and blood labs
Monitor vital signs, I&O, and infection drainage
Watch for superinfections (e.g., candida, C. diff)
Position limb for comfort and limit movement
Administer pain meds
Coordinate with parents and physical therapy
Client & Family Education
Treatment may require long-term antibiotics
Monitor for hearing loss from some antibiotics
Avoid putting weight on affected limb
Support normal development with safe activities
Encourage nutritious diet for healing
Compartment Syndrome
Cause: Tight casts, traction, trauma, burns, surgery, hemorrhage, IV infiltration.
Patho: Increased pressure in a muscle compartment leads to:
Nerve/blood vessel compression
Ischemia
Common in tibial or forearm fractures
If untreated: Can lead to deformity, paralysis, or infection.
Volkmann Contracture: Permanent hand/forearm deformity from compartment syndrome.
Key Findings: "5 P's"
Pain (not relieved by meds or elevation)
Paresthesia (tingling/numbness)
Pulselessness (late sign)
Paralysis (nerve damage)
Pallor (cold, pale skin, cyanosis)
Nursing Actions
Assess hourly for first 24 hours
Ensure space for 1 finger between skin and cast
Report signs immediately
Avoid elevation
Loosen dressings
Prepare for fasciotomy if needed
Client Education
Report pain not relieved by meds or worsening pain
Watch for color change or numbness
Fat Embolism
Fat from bone marrow enters bloodstream after long bone fracture
Osteomyelitis
Bone infection caused by bacteria from
External source (e.g., open fracture)
Bloodstream (hematogenous spread)
Key Manifestations
Irritability
Fever
Fast heart rate (tachycardia)
Edema (swelling)
Constant pain, worse with movement
Avoids using the affected limb
Infection site: tender, swollen, warm to touch
Nursing Actions
Assist with diagnostic testing (blood, skin, bone cultures)
Assist with joint/bone biopsy
Give IV and oral antibiotics
Monitor liver, kidney, and blood labs
Monitor vital signs, I&O, and infection drainage
Watch for superinfections (e.g., candida, C. diff)
Position limb for comfort and limit movement
Administer pain meds
Coordinate with parents and physical therapy
Client & Family Education
Treatment may require long-term antibiotics
Monitor for hearing loss from some antibiotics
Avoid putting weight on affected limb
Support normal development with safe activities
Encourage nutritious diet for healing