Surgery - CMS III Final
1/123
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
124 Terms
Which antiseptic is preferred for use around areas with hair?
Iodophor-based (Betadine)
Describe the technique utilized in surgical prep of the patient
Start at the incision and move OUTWARD in a circular motion
Who often performs surgical prep on the patient?
Circulating nurse (requires sterile gloves)
What areas are considered "sterile" on surgical personnel?
Above the waist and below the shoulder
if something falls below the level of the pt table, it is contaminated
How should you position your hands when rinsing during a surgical scrub?
- Fingertips toward ceiling
- Scrub distal to proximal
- Dry Distal to proximal
Allows water to flow down the arms and away from the hands
How should you pass a team member in the OR?
Front to front
Back to Back
The Surgical "time out" must occur BEOFRE what ?
The first incision
- Verify patient, site, & procedure with team
What are the factors considered when calculating a Revised Cardiac Risk Index?
- High risk Surgery
- Ischemic ♥ Dz/HF
- Cerebrovasc Dz
- Pre-op tx w insulin
- Pre-op Cr > 2
each factor = 1 point
(3+ factors --> 15% risk cardiac event)
According to the AHA, what patients should receive prophylactic ABX prior to surgery to prevent infective endocarditis?
- Prosthetic valve/repair
- PMHx Endocarditis
- Unrepaired Cyanotic CHD or residual defect
- Heart Transplant
How long after the placement of a drug-eluting stent, should patients delay elective non-cardiac surgery?
6 mo - 1 year
How long after the placement of a bare metal stent, should patients delay elective non-cardiac surgery?
30 days
How long after a balloon angioplasty should patients delay elective non-cardiac surgery?
14 days
How do you pretreat alcohol dependence before surgery?
IV cocktail of...
-Vitamins
-Thiamine
-Folate
Thiamine reduced risk of Wernickes Encephalitis
What patients require pre-op stress doses of steroids?
Having been on > 20 mg prednisone QD > 3 wks within the last year
What lab is checked 2 wks prior to surgery to test for chronic malnutrition?
Albumin
acute malnutrition --> prealbumin
How long before surgery should patients D/C Warfarin & Clopidogrel ?
5 Days
How long before surgery should patients D/C Rivaroxaban or Apixaban?
2-3 Days
What platelet count corresponds with a risk of spontaneous bleeding?
< 10k-20k
Bridging therapy is indicated in patients with a high risk for thromboembolism. What agent(s) are initiated and how long are they used for?
Short Acting Anticoagulants (UFH/LMWH)
INITIATE:
- 3 days before surgery
D/C:
- UFH: 4-6 hrs pre-op
- LMWH: 24 hr pre-op
Which ASA Class:
Normal, health patient
- non-smoker / minimal or no alcohol use
ASA I
Which ASA Class:
Mild Systemic Dz w/o substantial functional limitations
- Smoker, social drinker
- Pregnant, obese
- Controlled DM/HTN, mild lung dz
ASA II
Which ASA Class:
Systemic Dz with substantial functional limitations ( 1+ mod-severe diseases)
- Poorly controlled DM/HTN/COPD
- Morbid obesity, Active hepatitis
- Alcohol dependence
- Implanted pacemaker
- Moderatley reduced Ef
- ESRD on dialysis
- Premature infant
- PCA < 6 wk, MI/CVA/TIA/CAD/Stents
ASA III
Which ASA Class:
Severe systemic Dz constantly posing a threat to life
- RECENT MI/CVA/TIA/CAD/Stents
- Ongoing cardiac ischemia
- Severe valve dysfunction/ reduced Ef
- Sepsis
- DOC/ARDS
- ESRD NOT on dialysis
ASA IV
Which ASA Class:
Moribund patient, not expected to live w/o the operation
- Ruptured abdominal/thoracic aneurysm
- Massive trauma/ brain bleed
- Ischemic bowel
- Significant cardiac patho
- Multiorgan dysfunction
ASA V
Which ASA Class:
Declared brain dead patient whose organs are being removed for donor purposes
ASA VI
How long prior to surgery should breastmilk be D/C?
4 hours 🍼
other milk - 6 hrs
clear liquids - 2 hours
When is Type & Cross used?
-Denote ABO & Rh type
- Crossmatch blood with donors for a planned transfusion
Your patient requires prophylactic Cefotaxime before their appendectomy. What is the appropriate time frame it should be administered before the first incision?
within 30-60 minutes
According to Surgical Post-Op Risk Prevention techniques, what is recommended to reduce post-op infections?
Removal of foley cath POD 1-2
Can a patient change DNR orders at any point up until the surgery?
YES
Your patient just got out of a surgery where they were positioned supine with their arms abducted. What is the biggest complication from this surgical position and how can you prevent it?
Brachial Plexus Injury
-Relieve undue pressure to the humerus by maintaining less than 90 degree angle of the arm
What injury can be caused by the lithotomy surgical position and how do you prevent it?
Peroneal n. Injury resulting in foot drop
Prevent by placing extra extremity padding
What is the MC injured nerve from malposition of the UE during surgery?
Ulnar nerve
What is the MC pathogen implicated in Surgical Site Infections (SSIs) ?
S Aureus
Which skin prep agents are CI in use on mucous membranes and hair?
- CHG (chlorhexidine)
- Alcohol-based
Do you prep contaminated areas of the skin first or last?
LAST
How should the drape be placed during surgical prep?
Start at the operative site and open it OUT towards the periphery
--AFTER pt is prepped
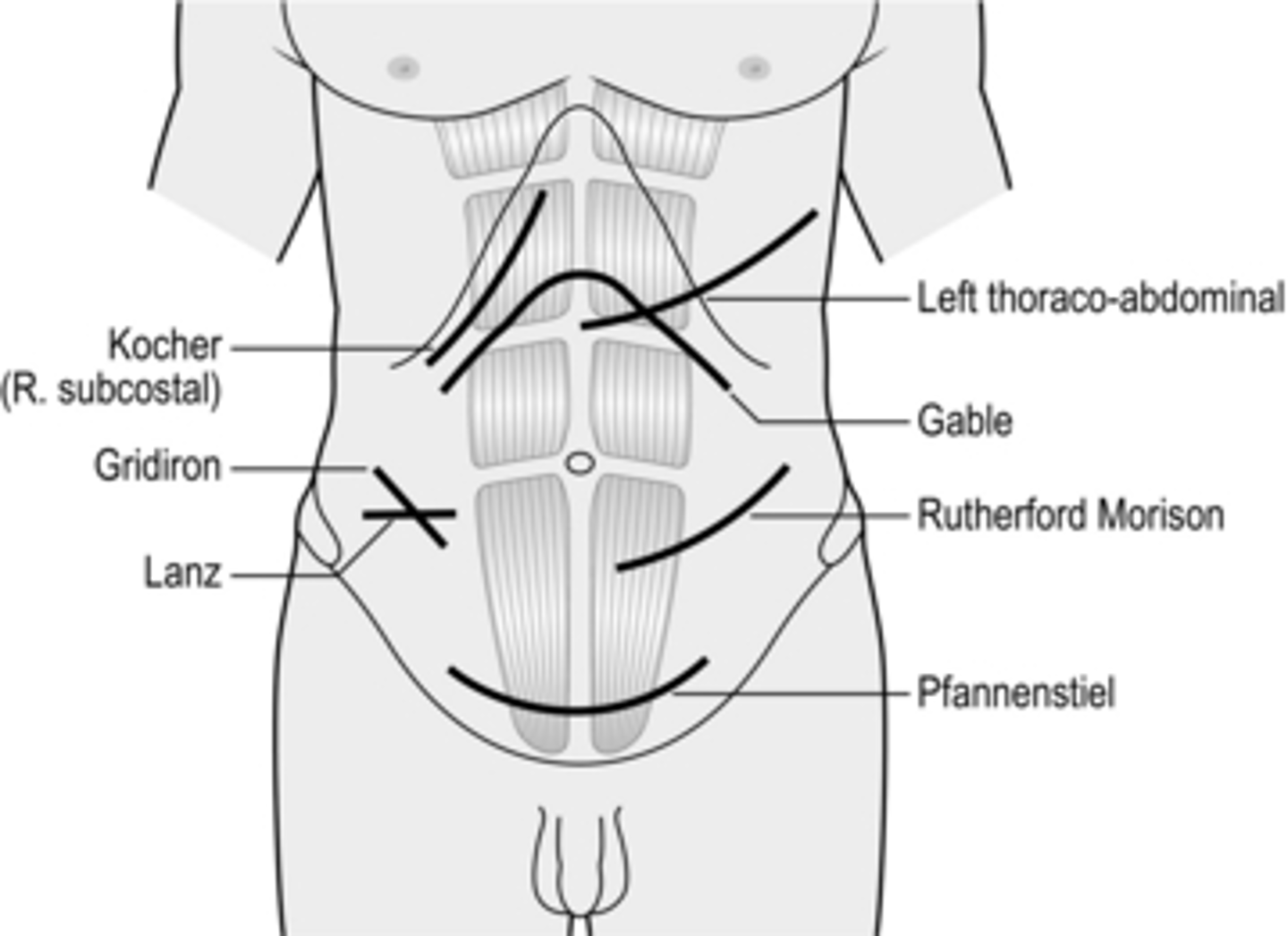
Which incision is placed on the right side of abdomen for open exposure of the GB & Biliary tree?
Kocher Incision (subcostal)
What wound class:
- Inguinal hernia repair
- Thyroidectomy
I
What class wound is a Total Hysterectomy?
II
- Clean-contaminated
- Respiratory, GI/GU tracts
What class wound:
- Intra-abdominal abscesses
- Traumatic / Penetrating wounds
- Purulent or fecal material
IV
- Dirty or infected
- Inadequate tx of traumatic wounds
- Evident infxn / purulence
What Project standardizes practices that reduce the risks of surgical infections?
Surgical Care Improvement Project (SCIP)
Where is the initial trocar placed in a laparoscopic surgery?
The umbilicus
Should a clean-contaminated procedure receive prophylactic ABX?
NO
Post-op patient suddenly develops a fever of 104 F, tachycardia, and HoTN. Upon further exam, you find they are hyperkalemic and have muscle rigidity. How do you treat?
Dantrolene
Malignant Hyperthermia
Halogenated gases (halothane, sevoflurane, etc)
What is the best way we can prevent VTE in surgical patients?
EARLY AMBULATION
List the 5 W's as related to post-op fevers and the PODs they are most commonly associated with
WIND - atelectasis / PNA (POD 1-3)
WATER - UTI (POD 3-5)
WALK - DVT/PE (POD 3-7)
WOUND - SSI, Anastomic leak (POD 3-7)
WHAT did we do - Drugs (POD 7+)
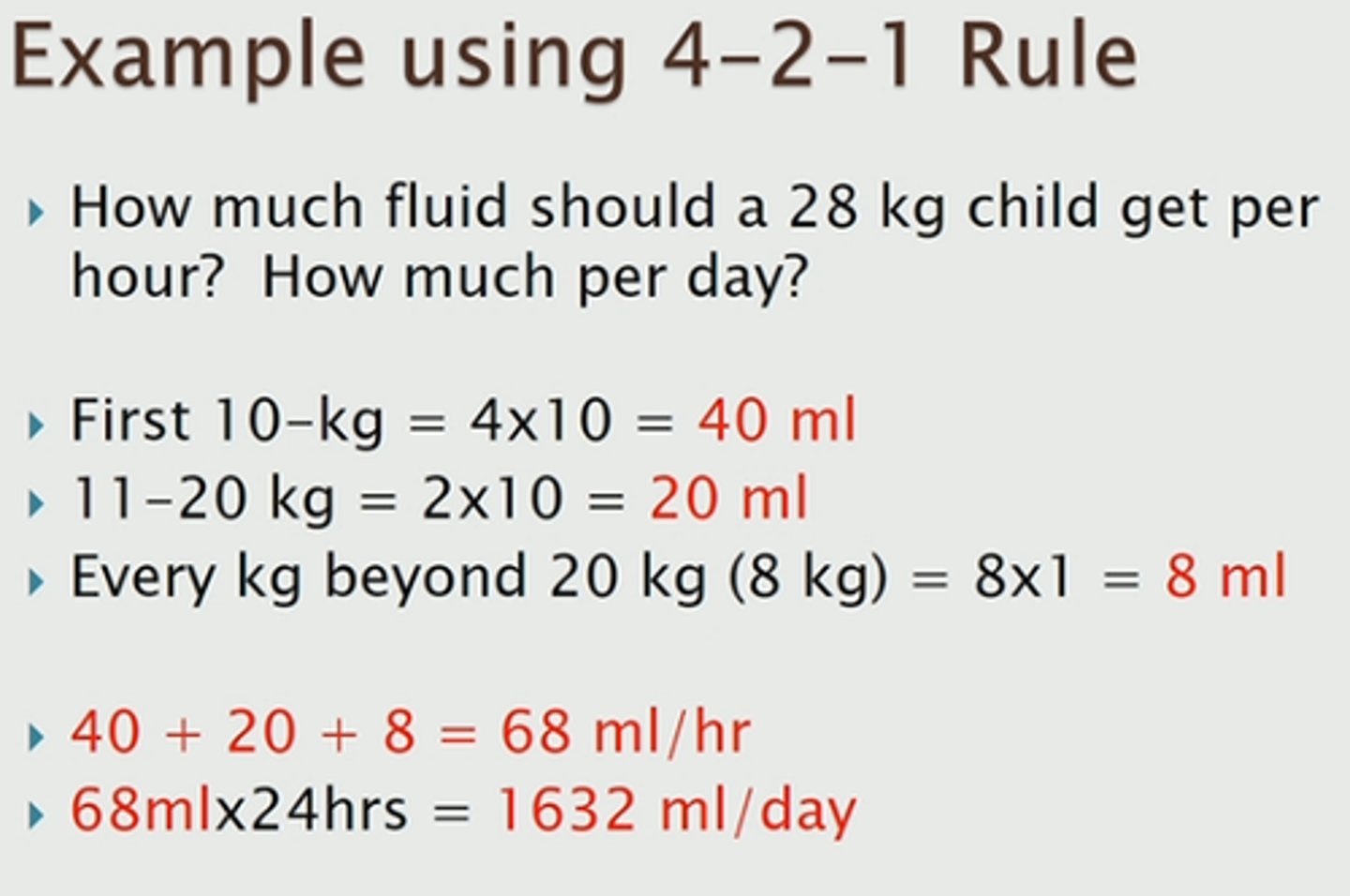
Calculate maintenance fluids for a 75 kg patient
4:2:1
40 mL + 20 mL = 60
75 kg - 20 kg = 55 kg left
(60 mL+ 55 mL) = 115 mL
Your patient develops a SSI 2 days after surgery. What type of infection is probable, based on the early post-op development?
Necrotizing soft tissue infection (NSTI)
MC POD 1-3
Your patient develops a SSI 6 days after surgery. Based on the time frame of development, what type of infection is probable?
Superficial Wound Infection or Intra-Abdominal Abscess
MC POD 5-10
If your patient develops a post-op fever, what do you want to rule out ASAP due to their high rates of mortality "the killers"?
- Necrotizing infection
- Anastomotic leak
- PE or MI
What are the common causes of subacute post-op fevers (after the first week)
- Wound infection
- UTI (mc w foley)
- PNA (mc if vent / COPD)
- C. diff
- bacteremia, line sepsis
- intra-abdominal abscess
Patients receiving tube feedings are at an increased risk for .... ?
Aspiration that can progress to ARDS
What is the MCC of post-op fever within 48 hrs of surgery. How do you prevent/manage this complication?
Atelectasis
Incentive spirometry
Post-op patient presents with sudden tachycardia, HoTN and narrow pulse pressure. What should you be sus of ?
hemorrhage
Your patients surgical drains continue to fill with blood, and you suspect a hemorrhage. What are the next steps in your diagnostic work-up?
- CBC, PT/INR, PTT
- I/Os
- Imaging
Patient s/p abdominal surgery presents with obstipation, intolerance of oral intake, and diffuse abdominal distension. PE reveals absent bowel sounds. What is the likely complication present?
Ileus
inflammation of intestinal smooth muscle causing disruption of normal peristalsis
How do you treat ileus or bowel obstruction s/p surgery?
- NPO until bowel function returns
- NGT (decompression)
Wound dehiscence is most likely to occur during POD ______
5-8
Disruption of operative wound due to excess tension, ischemia, improper suturing
Which phase of wound healing is characterized by hemostasis, chemotaxis and inc vascular permeability?
Inflammatory (0-7)
-plt aggregation
-clotting cascade
-mast cell degran
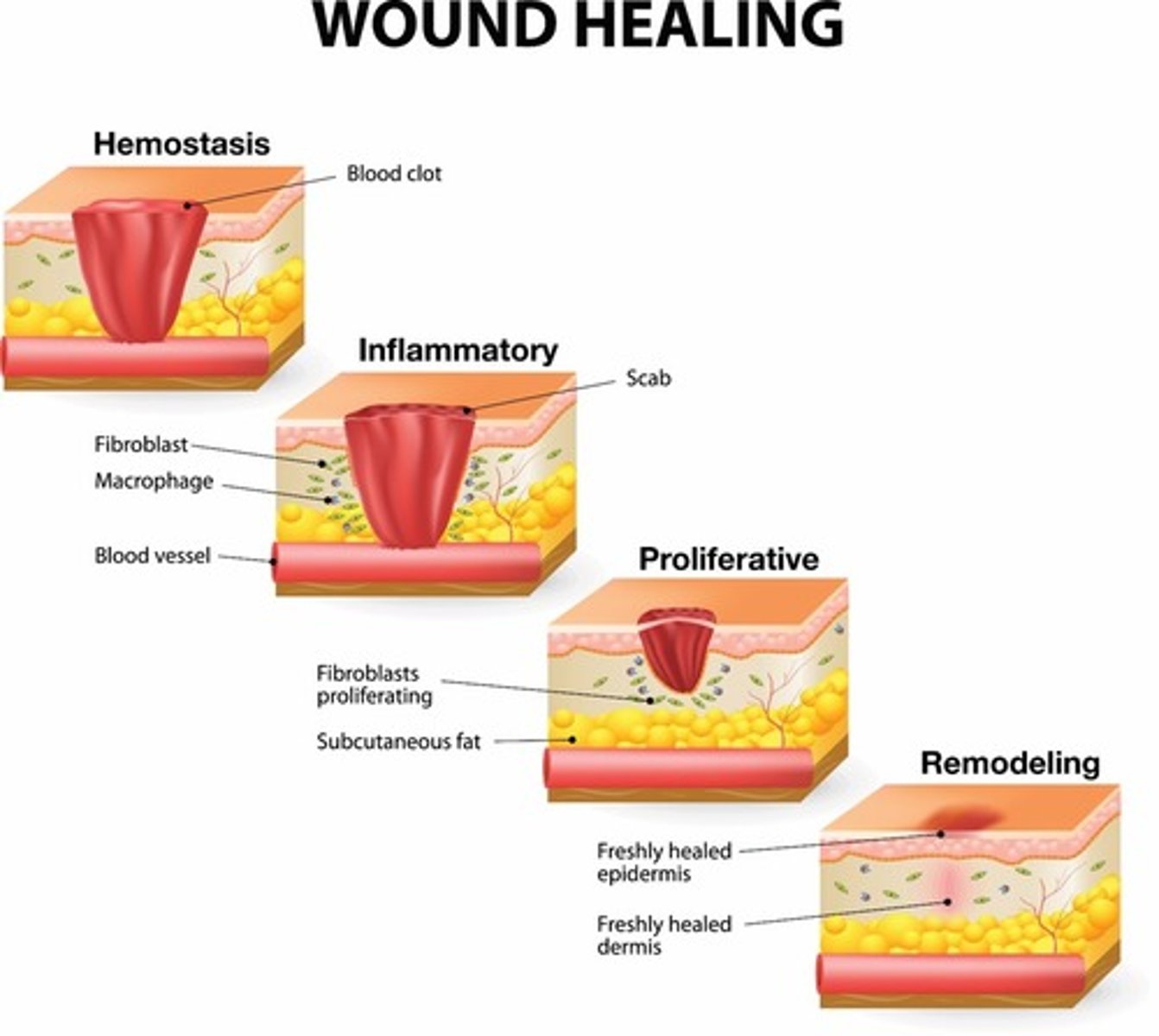
Which phase of wound healing has formation of granulation tissue & re-epithelialization, with increased fibroblasts + collagen synthesis
Proliferative (7-21)
-epithelial cells aid in angiogenesis
-tissue connectivity is re-established
Which phase of wound healing includes acellular collagen rich scar formation
Maturation/ Remodeling (21+)
Which type of wound closure leaves wound edges unopposed, & is MC seen with "dirty/contaminated" wounds
Secondary intention (closure)
closes by re-epithelializtion & wound contraction
Which type of wound closure is seen with a contaminated wound initially being treated with repeated debridement or ABX for several days before closure
Tertiary (delayed primary)
What IV anesthetic has increased secretions & risk of laryngospasm, with hallucinations & post-op disorientation?
Ketamine
used in low doses for painful bedside procedures
- bronchodilator properties
Which IV anesthetic would you AVOID in patient with increased ICP and low RR?
Ketamine
Which benzo is MC used for pre-procedure sedation & provides anxiolysis, sedation, & amnesia?
Midazolam (versed)
Which agent mimics effects of Ach, causes fasciculations, prolonged paralysis, and is often used in RSI?
Succinylcholine
Which injectable local anesthetic has a slow onset, but the longest duration of action and is ideal for post-op control?
Bupivicaine
risk for ventricular arrhythmias
Which laparoscopic device utilizes ultrasonic energy and minimizes the need for instrument exchange?
Harmonic scalpel
Which suture filament has less risk for harboring bacteria and easily passes through tissue, however has increased likelihood of knot slippage & suture breaks
Monofilament
Are synthetic or organic sutures more reactive, stimulating more of an inflammatory response?
Organic
Name the absorbable synthetic sutures that break down via hydrolysis
- Vicryl
- Monocryl
- PDS II
Which absorbable synthetic suture has superior monofilament pliability, with 60-70% tensile strength at 1 wk ?
Monocryl
strength lost at 28 days
What is the least reactive absorbable suture available?
PDS II (inflammable)
loses majority of strength at 6 wks
List the absorbable sutures from MOST to LEAST reactive
- Fast Gut
- Plain Gut
- Chromic Gut
- Vicryl
- Monocryl
- PDS II
List the non-absorbable sutures from MOST to LEAST reactive
- Silk
- Pronova
- Mersilene & Ethibond
- Ethilon & Nurolon
- Prolene
Which suture has a larger diameter: monocryl 5-0 or 4-0
4-0
the more 0's, the smaller the suture
What method of wound closure can only be used in low skin-tension areas?
steri-strips
How long should sutures be left in high tension eyelid wounds?
5-7 days
face/neck - 5
scalp - 7-10
trunk & UE - 7
LE - 8-14
joints - 14
palms/soles/digits - 10-14
Which type of fluid shifts from the intravascular space into the intracellular space?
Hypotonic (0.45% NS)
intravascular = part of ECF
Urine Na < 20
FeNa < 1%
Prerenal azotemia
Urine Na > 40
FeNa > 1%
Intrinsic dysfunction (ATN, AIN, GN)
Urine Na > 40%
FeNa > 4%
Postrenal (obstruction, bladder dysfunction, narcotics)
What does a Sentinel Node bx help patients avoid if their results are negative?
Axillary dissection
sentinel node - lowest draining node is bx
What complication is associated with an axillary dissection?
Long thoracic n injury (winged scapula)
Which type of mastectomy removes all of affected breast & part of the axillary lymphatics (Levels I & II), preserving underlying muscle
Modified Radical
Radical = ALL lymphatic drainage and removes muscle
25 y/o female presents with a U/L, firm, rubbery mass with regular borders on her right breast. She does not complain of any pain. What is your plan in managing the likely diagnosis?
Observe and reassure the patient
Fibroadenoma
Pt presents to the hospital after an MVA complaining of dysuria. On PE you note blood at the meatus and a palpable bladder. What are important treatment considerations?
Urethral Injury
Dx: Retrograde urethrogram
Tx: Cystoscopy with urethral repair
leave foley in for 1-3 mo until completely healed
65 y/o male presents with hesitancy, urgency, and nocturia. What is the gold standard surgery for the likely condition?
BPH - TURP
72 y/o male has a nodular prostate on DRE and PSA levels > 10. What is the Gold standard diagnostic for the likely condition?
Prostate Ca - BX
What is removed in a radical prostatectomy?
Prostate & Seminal Vesicles
What is removed in a total vs radical hysterectomy?
Total - cervix & uterus
Radical = uterus, cervix, upper part of vagina, ovaries, fallopian tubes
How much CO2 is used to insufflate the abdomen and what is this process called?
4 L
Pneumoperitoneum for lap procedure
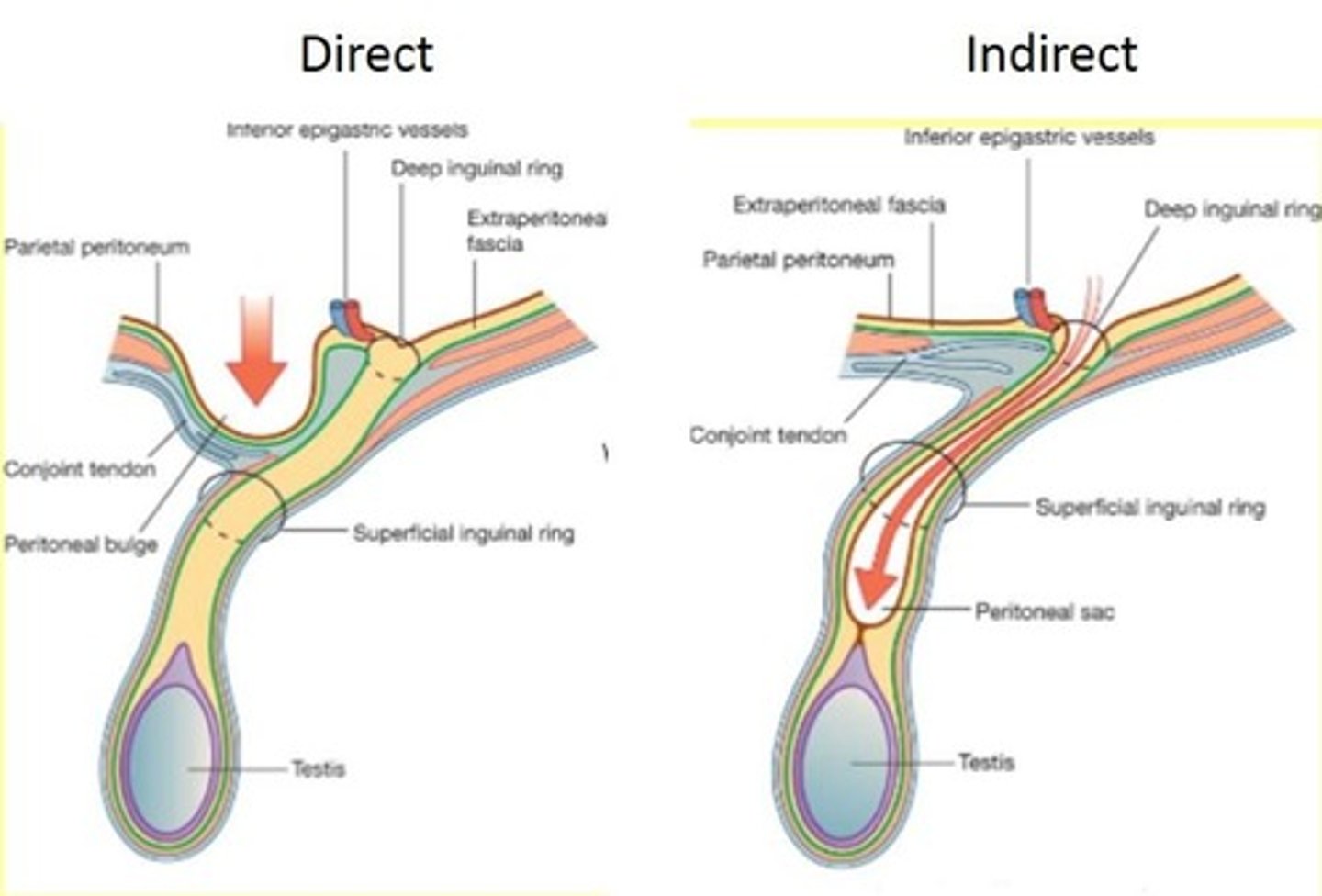
Hernia protruding through the internal inguinal ring
Indirect inguinal
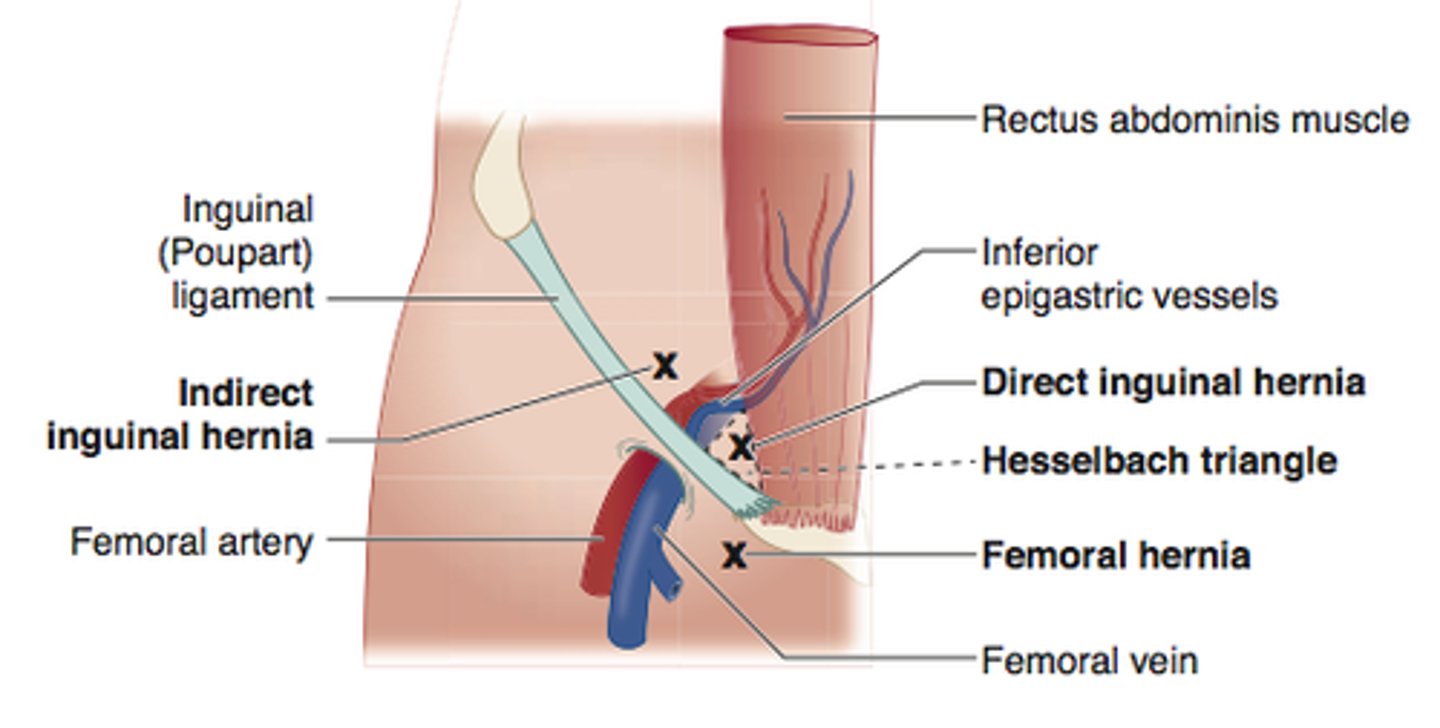
Hernia protruding through the transversalis fascia and Hesselbach's triangle
Direct Inguinal
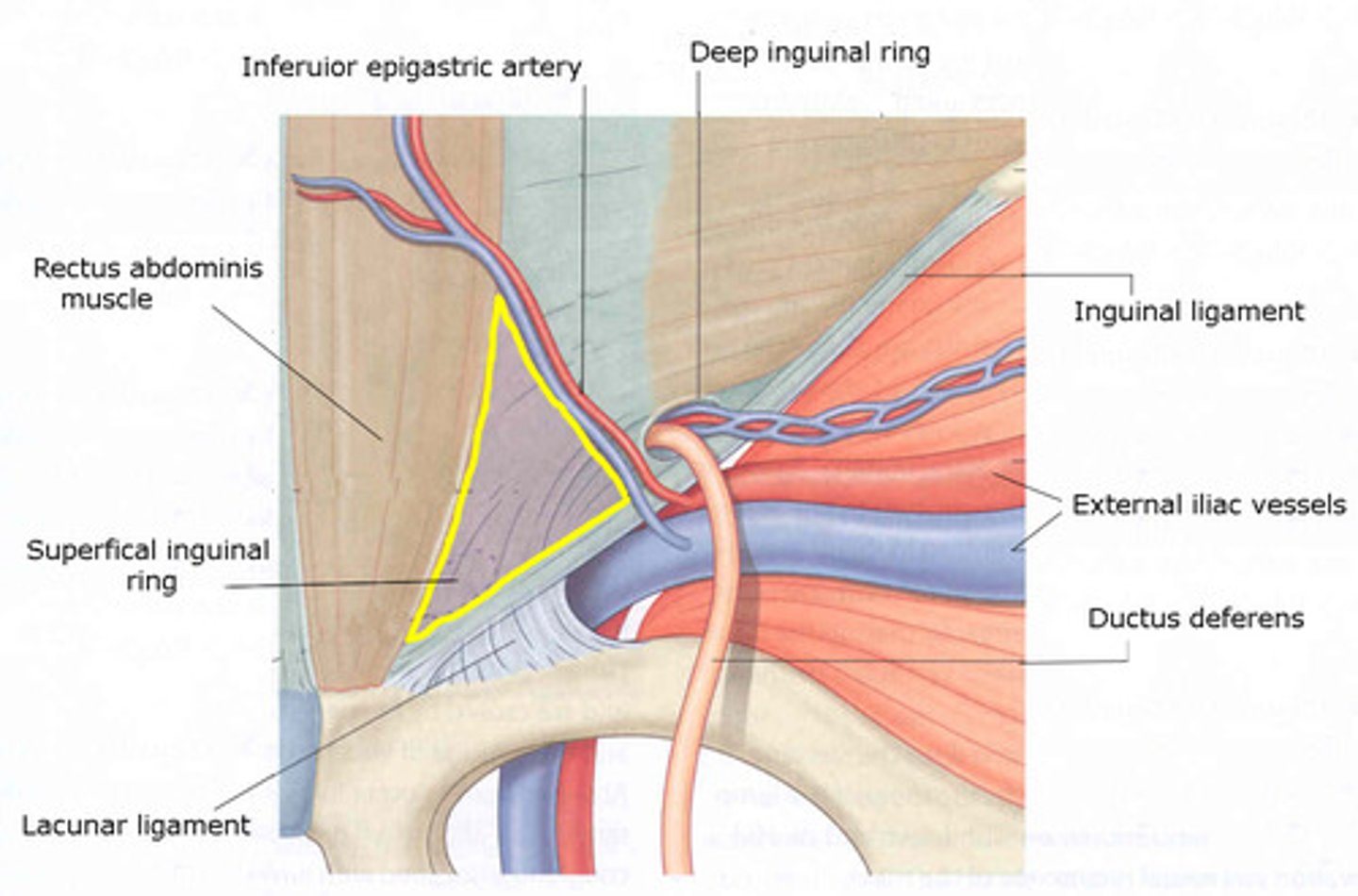
Borders of Hesselbachs Triangle
Inf: Inguinal ligament
Lat: inf epigastric vessels
Med: Rectus abdominis
What structure lies in the female inguinal canal?
Round ligament of the uterus
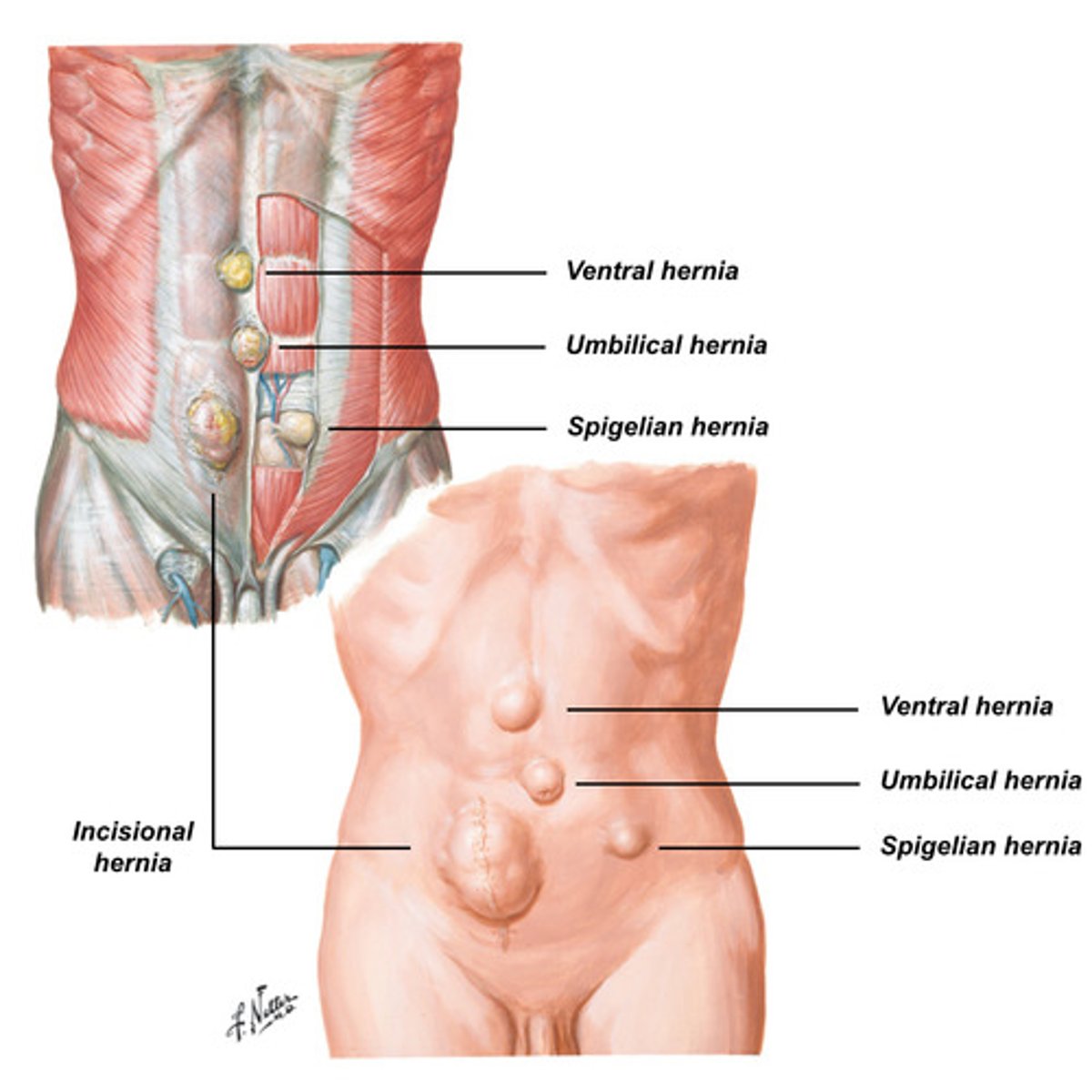
Which type of hernia is at the lateral edge of the rectus muscle @ the semilunar line?
Spigelian
Which hernia repair is tension free, using mesh rather than sutures
Lichtenstein