Chapter 14 Review Sheets - Antimicrobial Drugs
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
36 Terms
Who produces Antibiotics?
Bacteria
Why do antibiotics exist in nature?
Because of natural competition between microbes (provide competitive advantages)
What was the contribution of paul Ehrlich to antimicrobial therapy?
Would this be considered an antibiotic?
Discovered Compound 606, an antimicrobial agent that proved to be an effective treatment for Syphilis
Yes, it is considered the first modern antibiotic
What is Prontosil?
Is this an antibiotic?
What is the actual active ingredient of Prontosil?
Dye discovered to have antimicrobial activities
Active ingredient was Sulfanilamide
Yes, it was the first commercially available antibiotic
Who is Alexander Fleming?
How did he contribute to modern medicine?
First to discover a naturally produced Antimicrobial, Penicillin, in 1928
Penicillin was antibacterial against many different causative agents of diseases
What type of organism produces Penicillin?
Mold (Penicillium notatum)
Which group of bacteria are responsible for the majority of antibiotics in prodiction today?
Actinobacteria
Explain the difference between Broad Spectrum and Narrow Spectrum antibiotics.
Broad Spectrum — drug that targets many types of microbes
Narrow Spectrum — drug that targets on a specific subset of microbes
What are the potential consequences of choosing a broad spectrum antibiotic over a narrow spectrum antibiotic?
Broad spectrum antibiotic will also target a broad spectrum of the normal microbiota
Can cause a superinfection because the antibacterial intended for the preexisting infection kills the protective microbiota
Why might one choose to use a broad spectrum antibiotic?
Can be used when a narrow spectrum drug fails because of development of drug resistance by target pathogen
What is a Superinfection?
Why does it occur?
Secondary infection that may develop as a result of long-term, broad spectrum antimicrobial use
What are some potential routes of administration for an antibiotic?
Why are these different routes preferred?
Just any way you take meds, basically
Different ones preferred over others based on:
Bactericidal vs. Bacteriostatic
Spectrum of Activity
Dosage
Side Effects
Potential Interactions
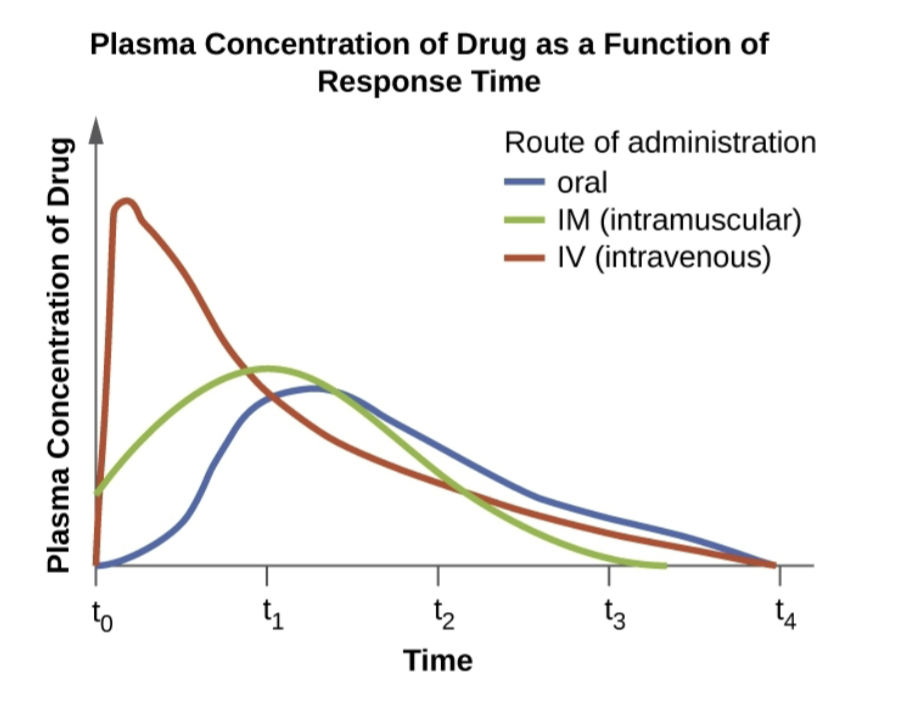
How does the route of administration affect the amount of the antibiotic present in the patients plasma?
What is the difference between a Synergistic and an Antagonistic drug interaction?
Synergistic —> combined effect of a combination of drugs is LARGER than the additive effect of each individual drug
Antagonistic —> combined effect of a combination of drugs is SMALLER than the additive effect of each individual drug
Understand that not all antibiotics persist for the same length of time in the system.
How does the length of a half-life affect the frequency of when you take the antimicrobial?
Longer half-life means you take the antimicrobial less frequently and vice versa (inverse relationship between half-life and taking of dose)
What does it mean if an antimicrobial compound is selectively toxic?
It selectively kills or inhibits the growth of microbial targets while causing minimal or no harm to the host
What are the major targets of antimicrobial compounds?
Cell Wall
Plasma Membrane
DNA and RNA Synthesis
Ribosomes
Metabolic Pathways
What is the common characteristic between Penicillins, Cephalosporins, Monobactams, and Carbapenems?
Contain a Beta-Lactam ring
What do the Beta-Lactam Antibiotics inhibit?
Cell wall synthesis
What are the benefits of chemically modifying antimicrobial compounds, such as Penicillin, to create variations of that compound (e.g. Methicillin)?
Can change the spectrum of action, improve absorption, and make it resistant to enzymes
What is the difference between Natural, Semisynthetic, and Synthetic antimicrobial compounds?
Natural —> produced naturally by microorganisms in nature
Semisynthetic —> chemically modified derivative of a natural antibiotic
Synthetic —> developed from a chemical not found in nature
What is the function of Aminoglycosides?
What is an example of an Aminoglycoside antibiotic?
Bind to the 30S subunit and interfere with the ribosome’s proofreading ability, leading to the generation of faulty proteins that insert into and disrupt the bacterial cytoplasmic membrane
Streptomycin
What is the function of Tetracyclines?
Binds to the 30S subunit, blocking the association of tRNAs with the ribosome during Translation
What is the function of Chloramphenicols?
Binds to the 50S subunit, inhibiting peptide bond formation
What is the function of Polymyxins?
Targets the lipopolysaccharide component of Gram-Negative bacteria and ultimately disrupt the integrity of their outer and inner membranes
Why might general toxicity be an issue with Polymyxins?
Can just be toxic in general and kill cells that it shouldn’t
Why would nucleic acid synthesis be an appropriate target for antibiotic compounds if Eukaryotes also synthesize nucleic acids?
Because the RNA Polymerase enzymes in bacteria are structurally different from those in Eukaryotes, allowing for selective toxicity against bacterial cells
What are the targets of Rifamycin and Fluoroquinolones like Ciprofloxacin?
Bacteria and their nucleic acid synthesis
How do Sulfanilamide and Trimethoprim inhibit bacterial cell growth?
Why does this affect bacteria but not Eukaryotes?
Interfere in the bacteria synthesis of folic acid by blocking Purine and Pyrimidine biosynthesis (inhibiting bacterial growth)
Does not affect Eukaryotes because they do not create folic acid (obtain it through nutrition sources instead)
Isoniazid inhibit Mycolic Acid synthesis. Which group of organisms would be targeted by this treatment?
Mycobacteria — prevents the synthesis of Mycolic Acid, which is essential for Mycobacterial cell walls
What is the challenge associated with treating diseases caused by Eukaryotic organisms?
Eukaryotes have cells very similar to human cells, making it more difficult to develop drugs with selective toxicity
What are the cellular targets that provide specificity to the treatment of fungal infections?
Chitin, Ergosterol, microtubules, etc.
Acyclovir is an analog of Guanosine.
How does this work to combat viral infections?
It is activated by the herpes simplex viral enzyme Thymidine Kinase and, when added to a growing DNA strand during replication, causes chain termination
What are the main areas used to target viral infections?
Nucleic acid and protein synthesis
What Polymerase is unique to RNA viruses, such as HIV, that is a target of some anti-viral medications?
RNA-Dependent RNA Polymerase (RdRp)
How does inhibiting Neuraminidase help to treat viral infections?
The specifically target influenza viruses by blocking the activity of the influenza virus Neuraminidase, preventing the release of the virus from infected cells