5. pigmented lesions part 4
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
59 Terms
endocrine abnormality and melanin disruption
The pituitary gland's melanocyte-stimulating hormone (MSH) is a key endocrine factor in melanin production, directly influencing skin and hair pigmentation. Other hormones like adrenocorticotropic hormone (ACTH) and estrogen can also affect melanin by influencing MSH levels or the activity of the tyrosinase enzyme, a key component in melanin synthesis. These hormones are linked to various pigmentation changes, from tanning to conditions like melasma and Addison's disease.
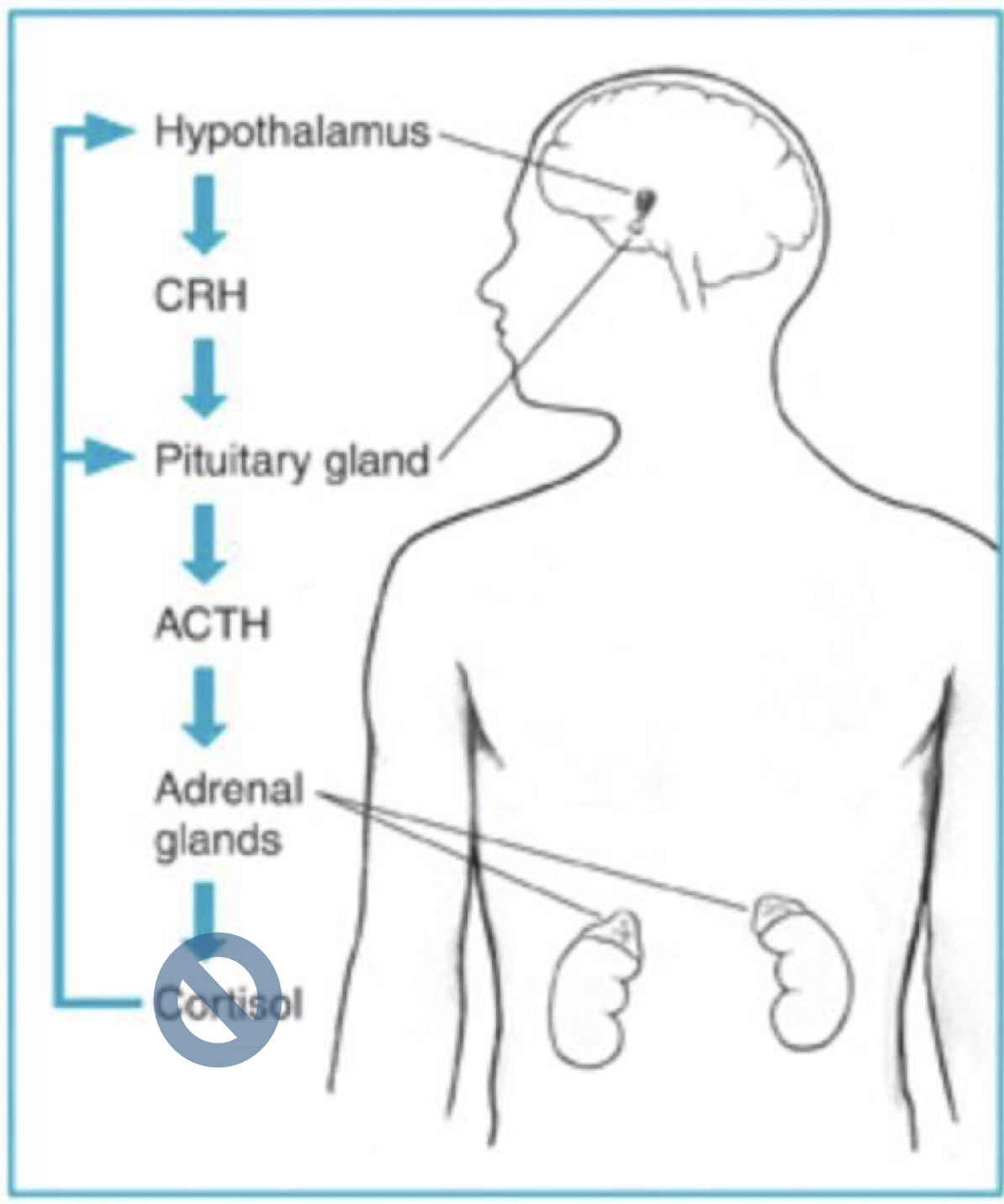
Addison’s disease
hypoadrenocorticism
insufficient production of adrenal corticosteroids
diffuse or patchy hyperpigmentation, especially of sun-exposed sin

what are some characteristics of Addison disease?
bronze pigmentation of skin
changes in distribution of body hair
GI disturbances
weakness
weight loss
postural hypotension
hypoglycemia
what are characteristics of adrenal crisis?
profound fatigue
dehydration
vascular collapse (↓bp)
renal shutdown
↓serum NA
↑serum K

which autoimmune melanin-associated pigmented lesion?
Addison’s
what are the types of metabolic/systemic melanin-associated pigmented lesions?
melasma, acanthosis nigricans, cushings
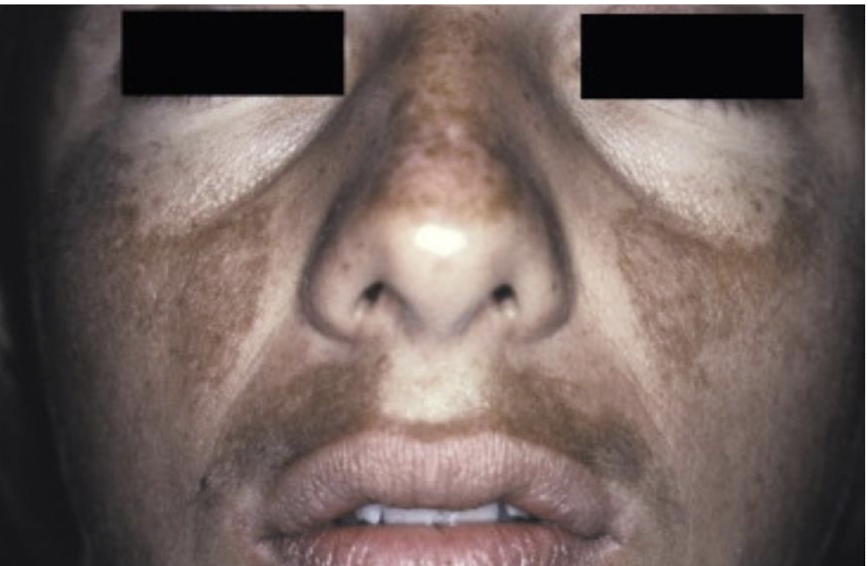
which type of metabolic/systemic melanin-associated pigmented lesions?
brown or gray-brown patches of hyperpigmentation on the face (sometimes a mylar pattern)
aka mask of pregnancy = chloasma
melasma
what are the types of neoplastic melanin-associated pigmented lesion?
melanotic neuroectodermal tumor of infancy (MNTI, rare but distinct)
oral melanotic nevus
which neoplastic melanin-associated pigmented lesion?
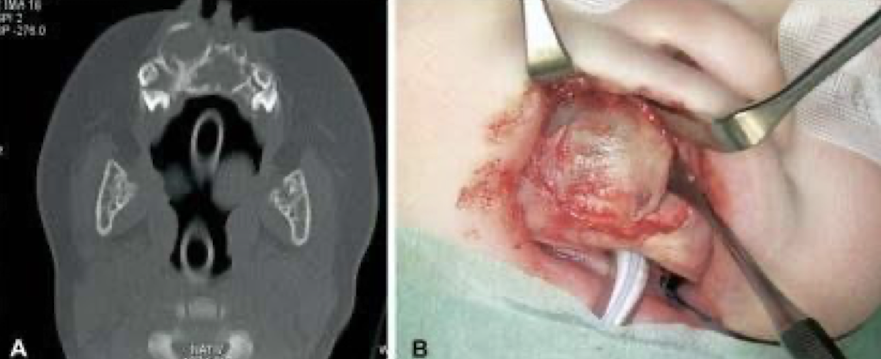
Krompecher in 1918 as a congenital "melanocarcinoma”
90% in head and neck and within the first 6 months of life
Male predilection (1.5:1), 60% on the palatal mucosa
Brownish-red mass of alveolar mucosa
High levels of vanillylmandelic acid in urine
BRAF V600E mutation identified in some cases (targeted therapies yay!)
surgically excised
MNTI
BRAF V600E
MNTI

MNTI
T or F: MNTI usually in maxilla
true
MNTI
what is the treatment for MNTI?
surgical resection (~20% recurrence rate; some intentionally left to be removed later)
radiation
chemotherapy
what is this: benign developmental malformation(s), variants can be acquired or congenital ex: melanocytic (blank)
nevus
features of which neoplastic melanin-associated pigmented lesion?
2nnd-4th decade
locations:
hard palatal mucosa 44%
buccal mucosa 22%
vermillion border 18%
gingiva 12%
retromolar pad 4%
oral melanocytic nevus
describe most common types of oral melanocytic nevi
intramucosal nevus 64%
blue nevus 16.5%
compound nevus 16.5%
junctiona; 3%
combined
balloon cell
spitz
features of which neoplastic melanin-associated pigmented lesion?
Diagnosed and biopsied in the 2nd -4th decades, females (2:1)
Pigmented, raised (nodular/papular)
Hard palatal mucosa and buccal mucosa…. Lip mucosa, gingiva, vermilion
Intramucosal ➔ blue and compound ➔ others
BRAFV600E mutation and GNAQ209 (blue nevus)
BRAFV600E and GNAQ209 gene mutations
oral melanocytic nevus, blue nevus
4 types of oral melanocytic nevi and their macule, plaque, and nodule status
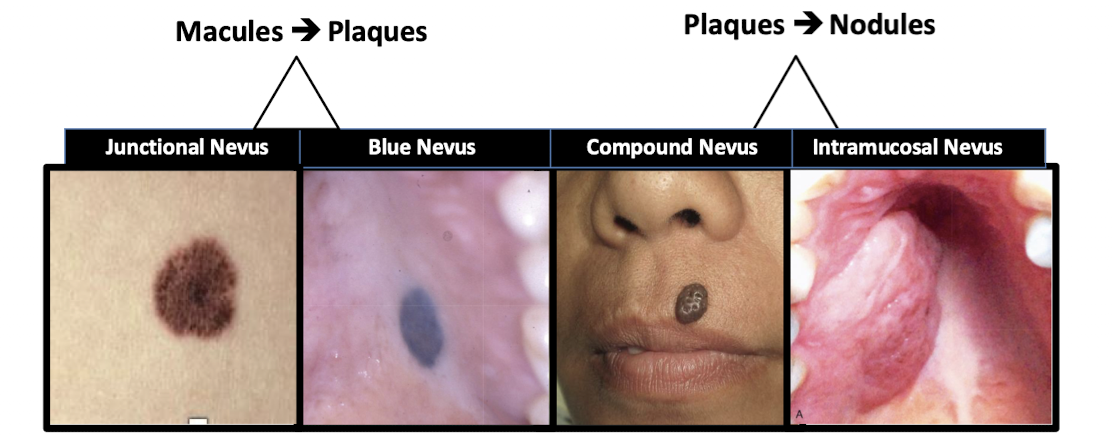
nevi vs macule
nevi = developmental, flat or raised VS macule = reactive, flat

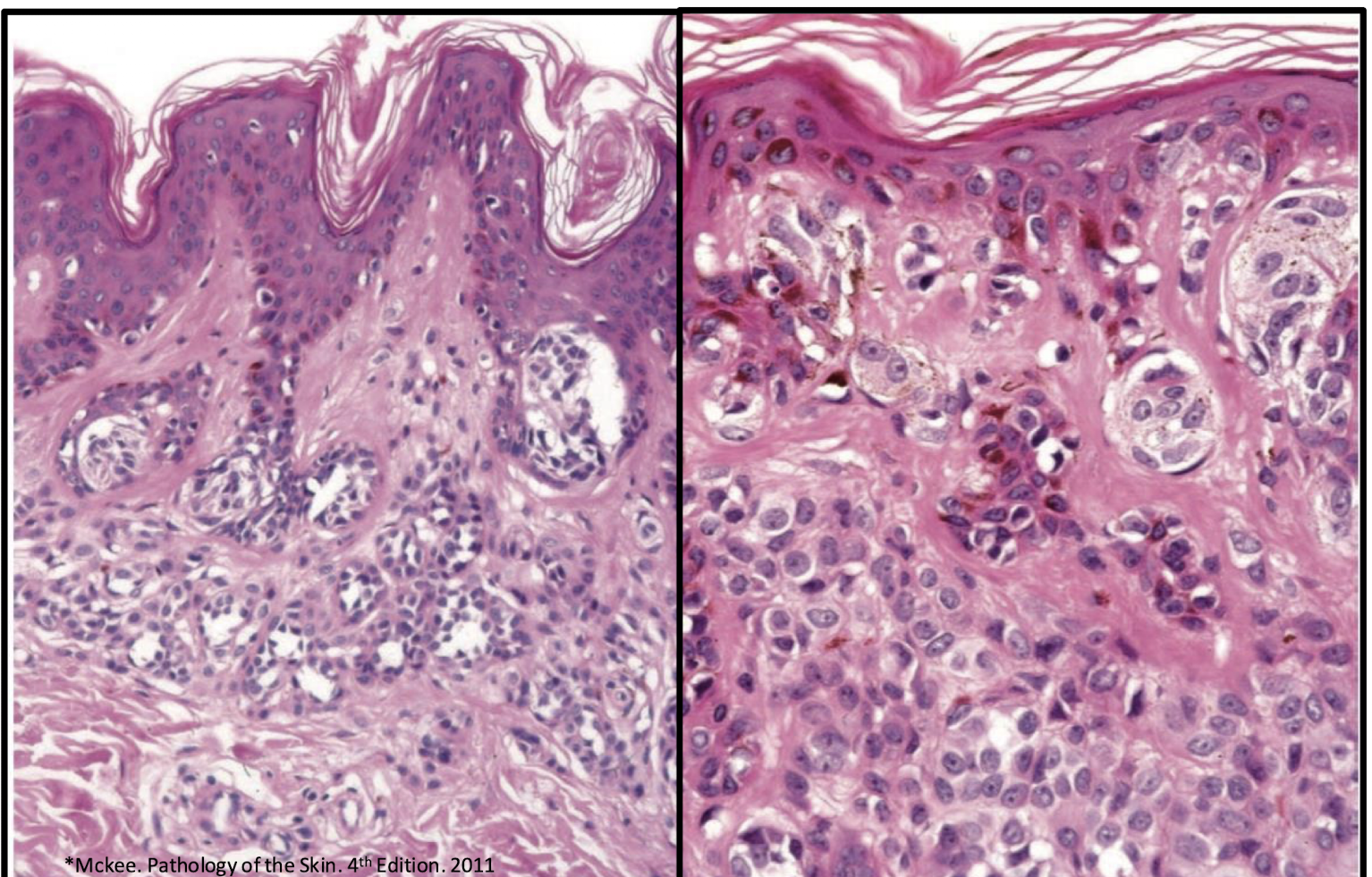
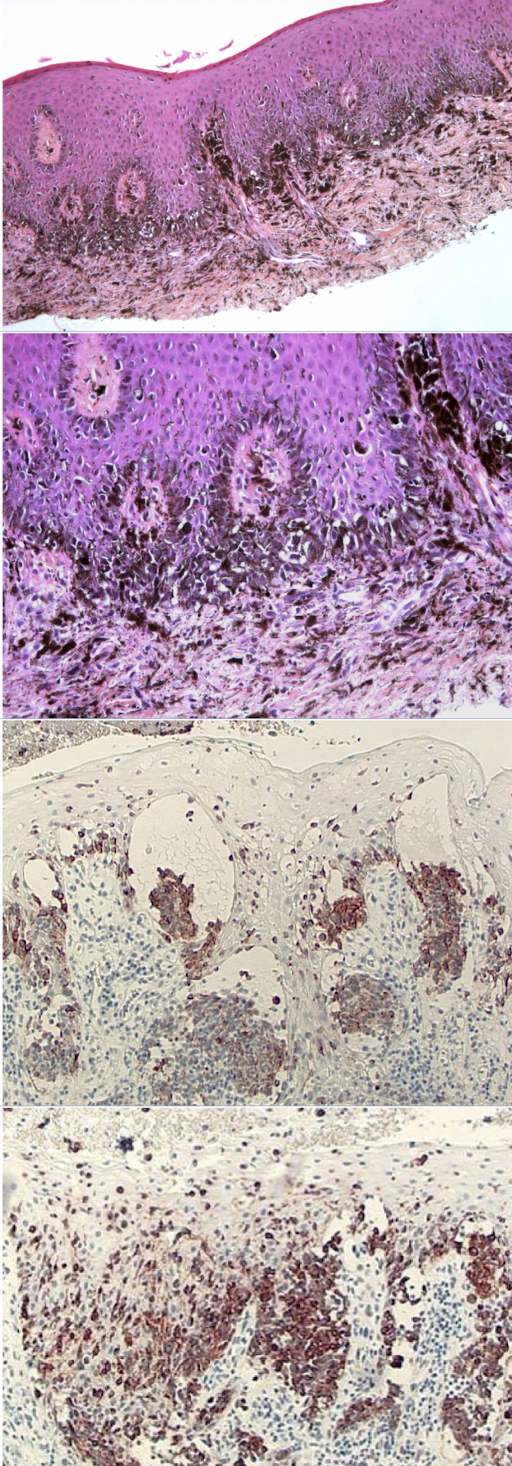
which melanocytic nevus histopathological features?
Unencapsulated proliferation of nevus cells, organized in theques
Lack dendritic processes of melanocytes
Migrate from junctional to compound to intradermal
acquired melanocytic nevus
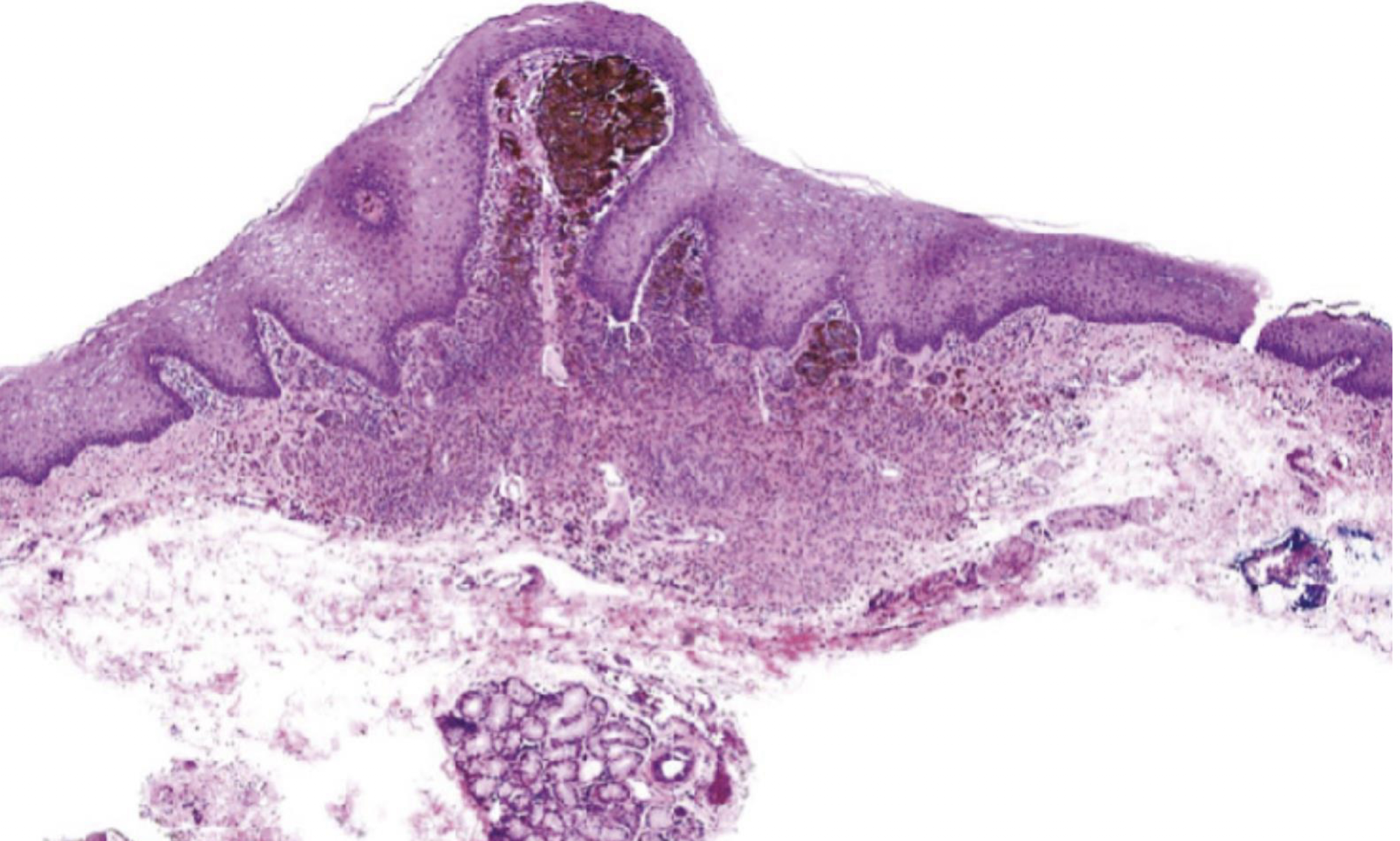
intramucosal nevus, (unique nevus cells)
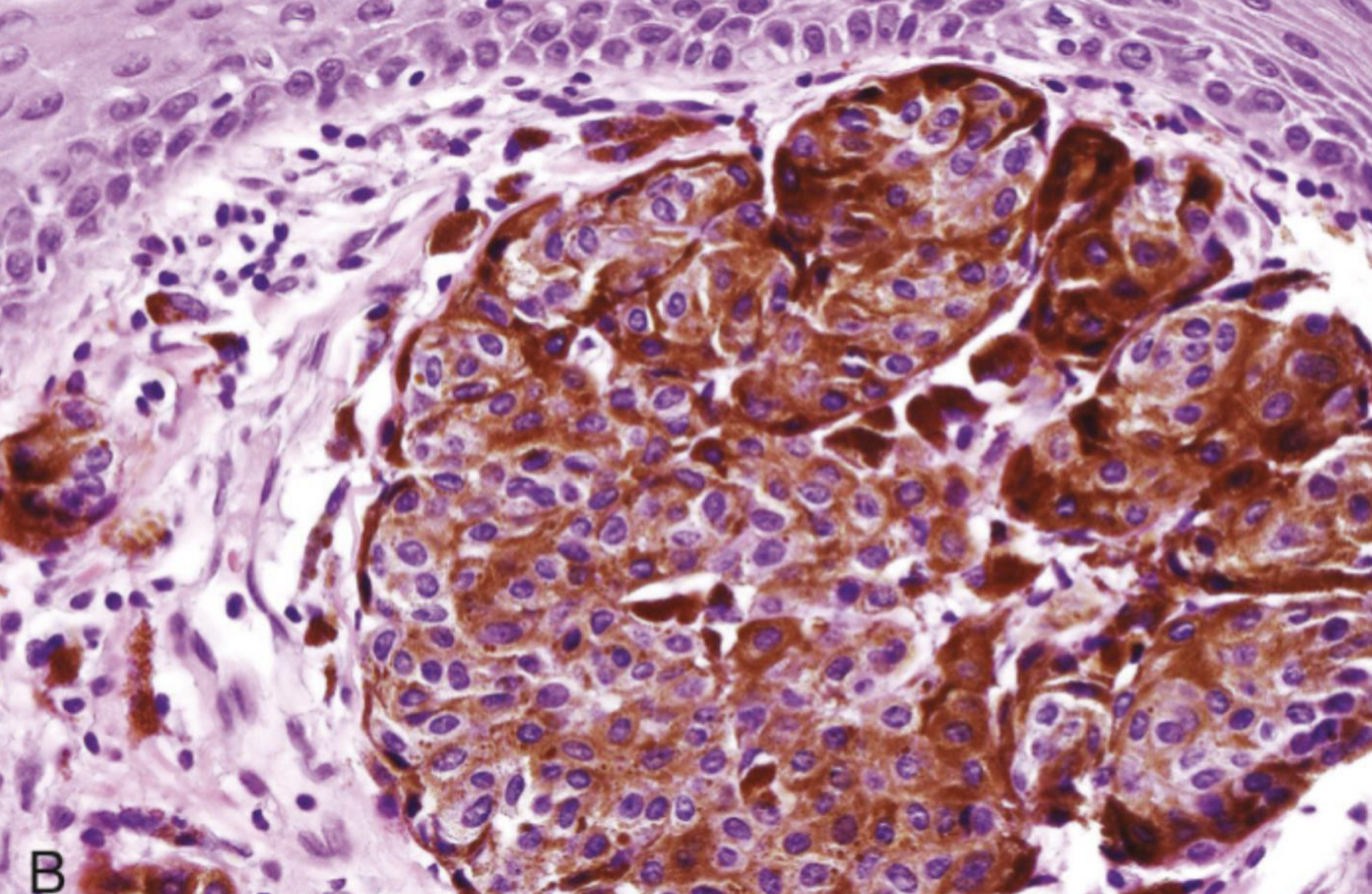
nest of melanocytes, unique
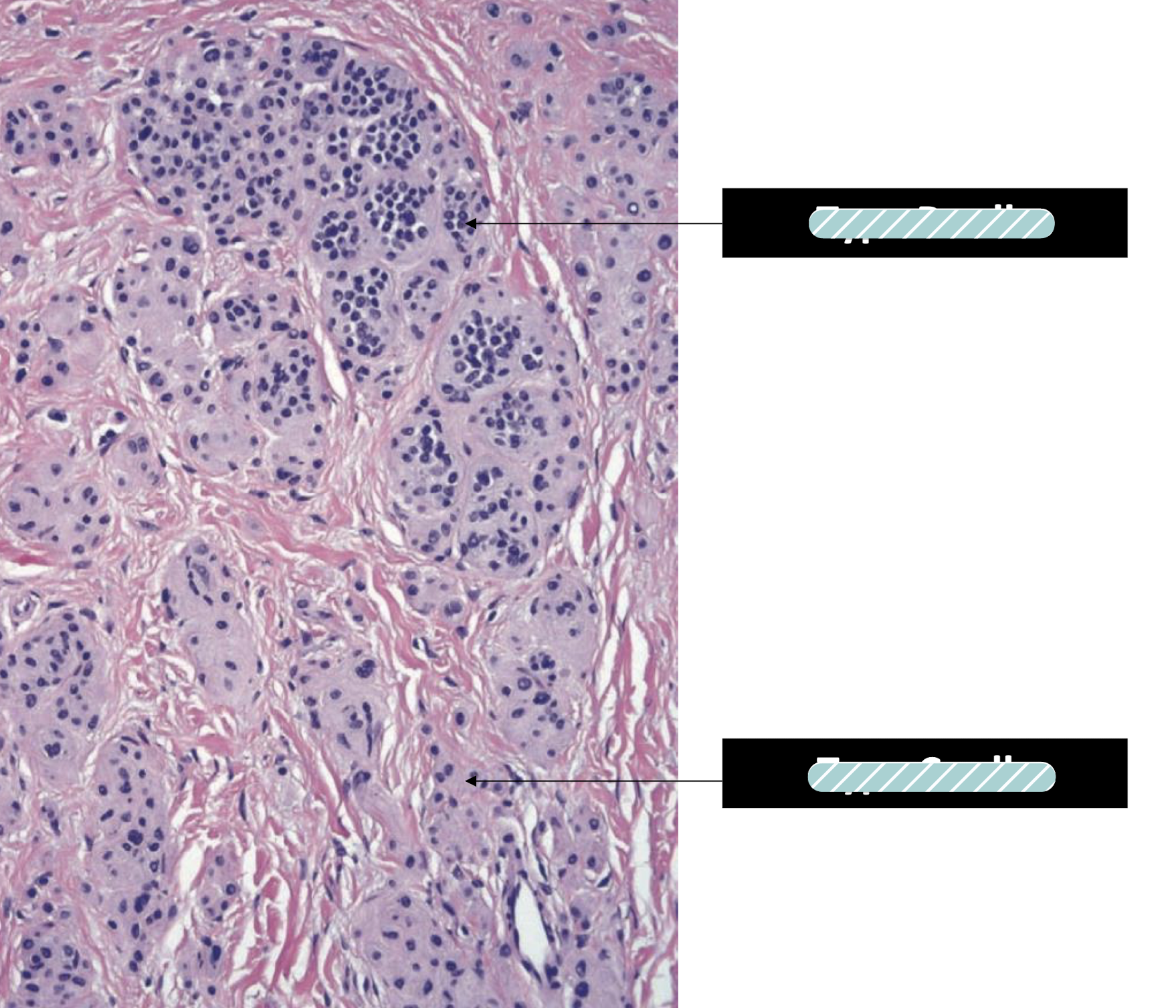
Type B to Type C morphology is a key characteristic of benign nevi and a sign of normal cell maturation, which helps pathologists distinguish them from melanoma, where this organized maturation process is typically lost
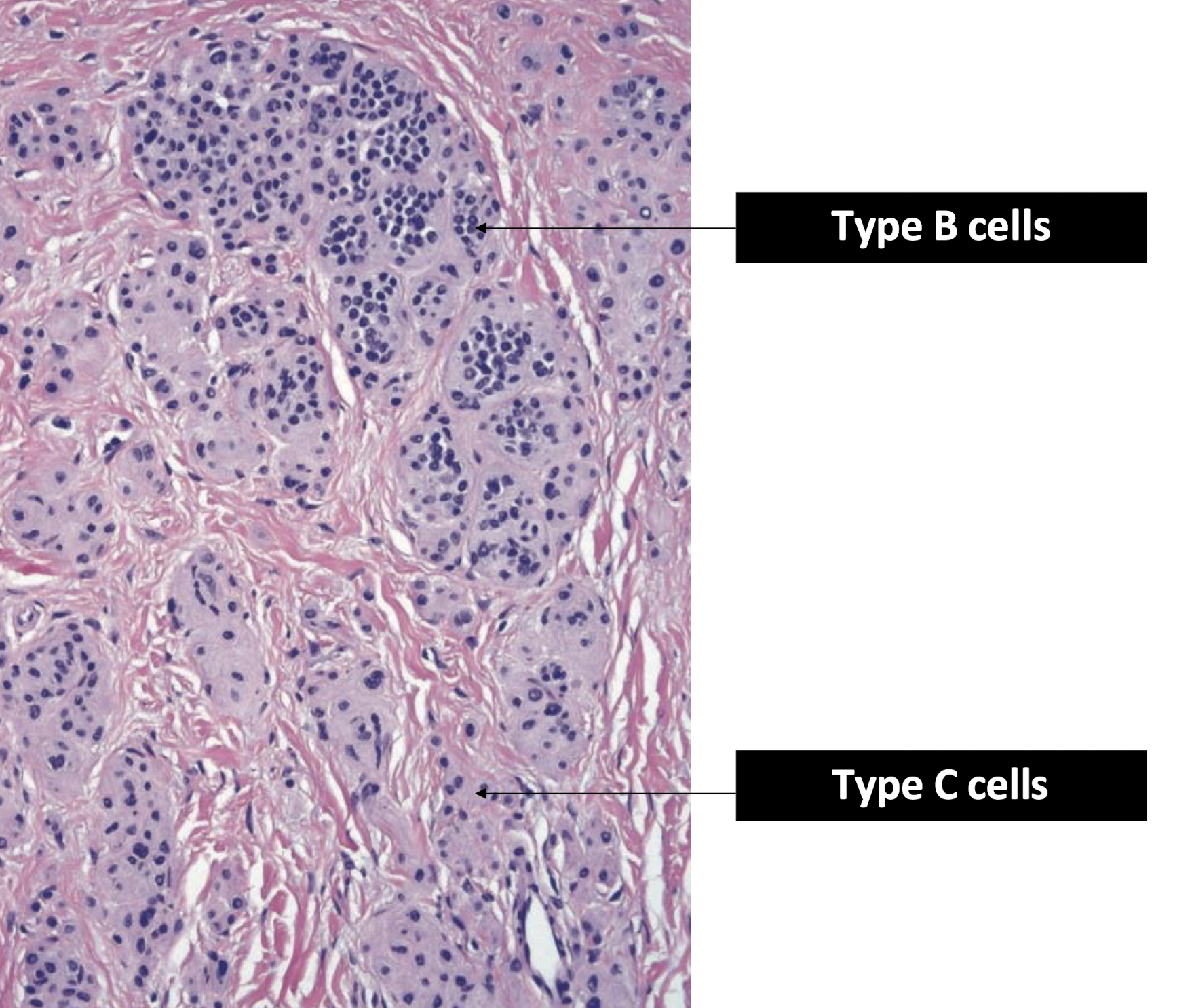

blue nevus, 1:subtle 2: not subtle
common blue nevus
compound nevus
combined nevus
what is the differential diagnosis for a pigmented lesion (nevus)?
amalgam tattoo
medication-induced pigmentation
melanoma (hopefully not)
treatment for pigmented lesion (nevus)
excision
Melanomas are a type of cancer that occurs in both the skin and oral mucosa. It however occurs far less commonly intraorally and the palate and gingiva are high risk sites.
A. both statements are true
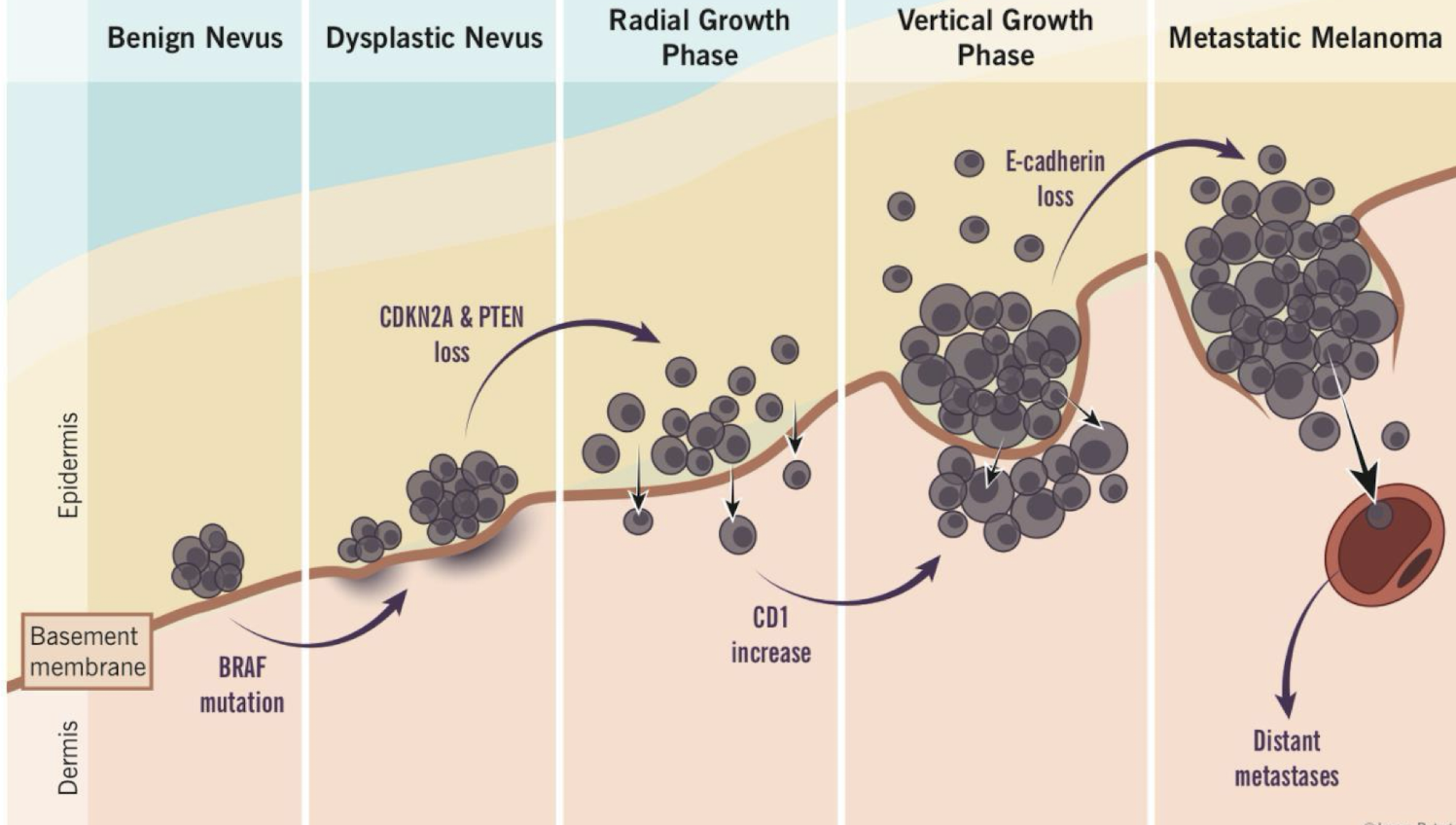
describe the evolution of a melanoma (hint)
nevi vs melanoma (ABCDE)
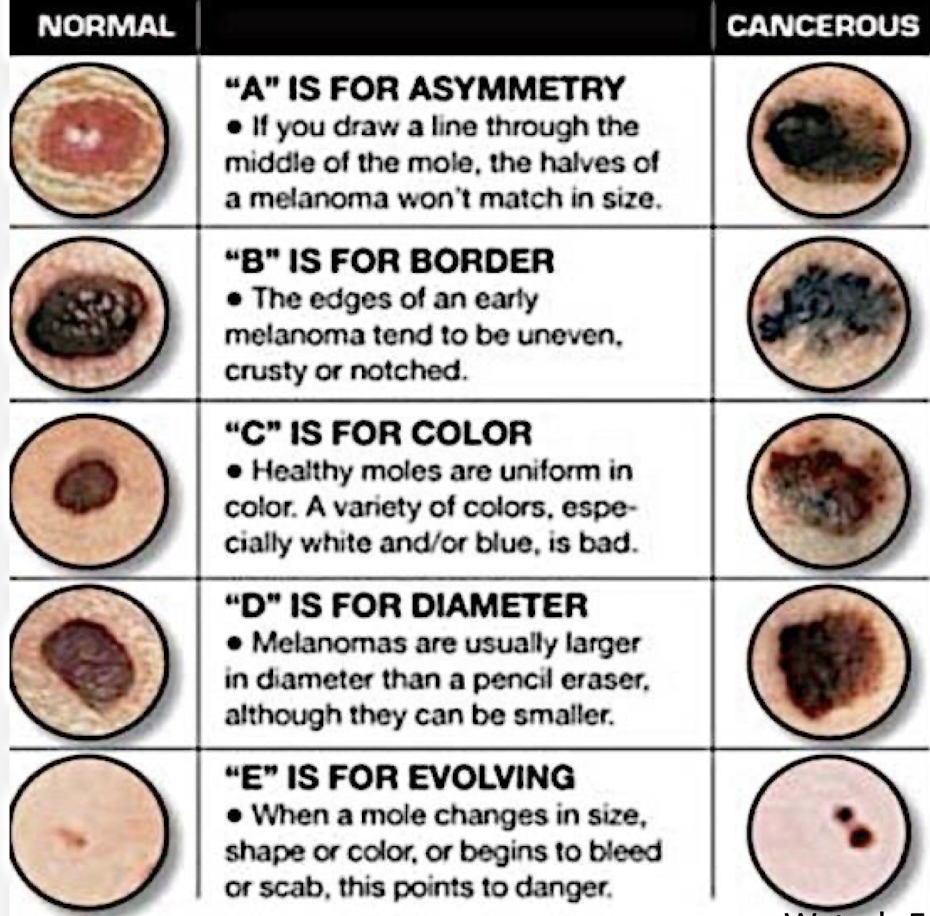
melanoma rates
87,100 cases, 5.2% of all new cancer cases
9,730 deaths, 1,6% of all cancer deaths
97.1% survival (death stable over the years)
what are some melanoma risk factors?
use of immunosuppressants
large number of freckles
presence of red hair
skin that burns easy
exposure to sunlight
presence of atypical moles
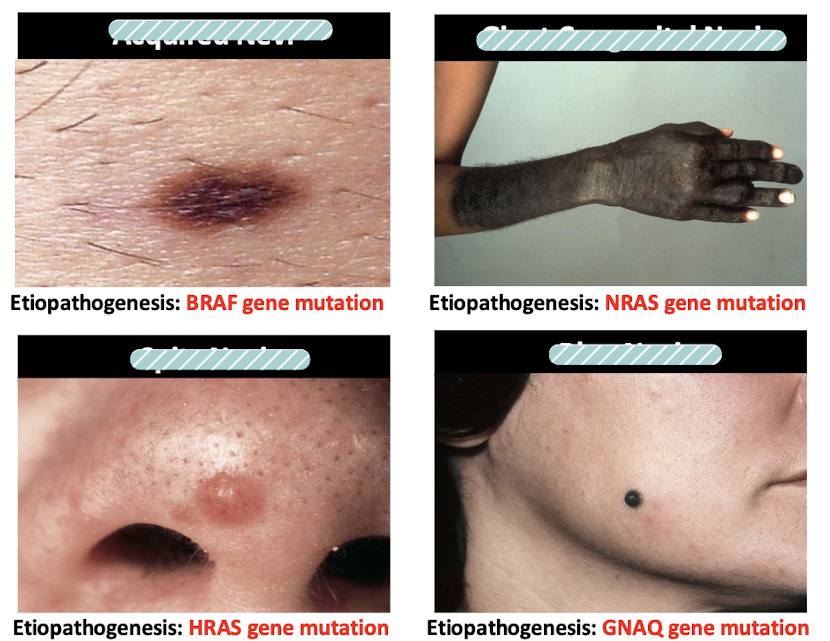
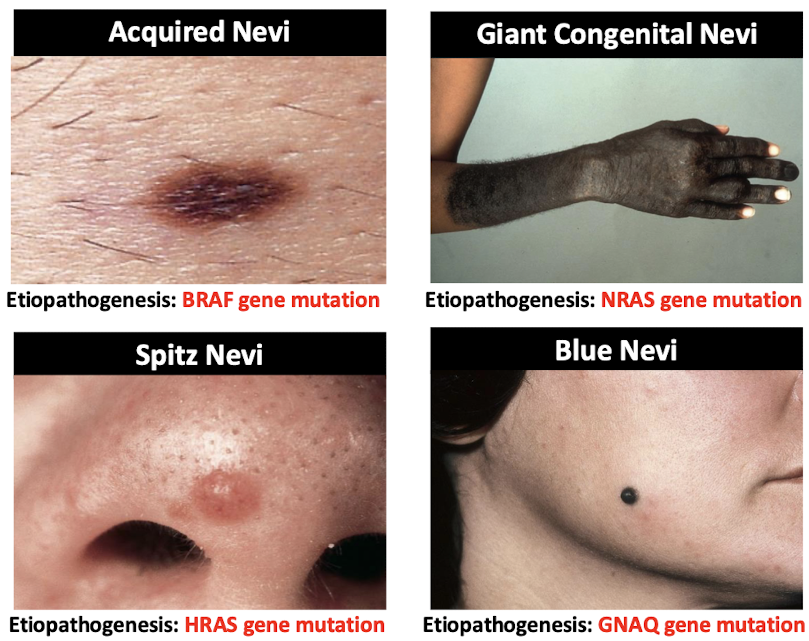
which gene mutation BRAF?
acquired nevi and cutaneous melanoma (BRAF V600E MNTI)
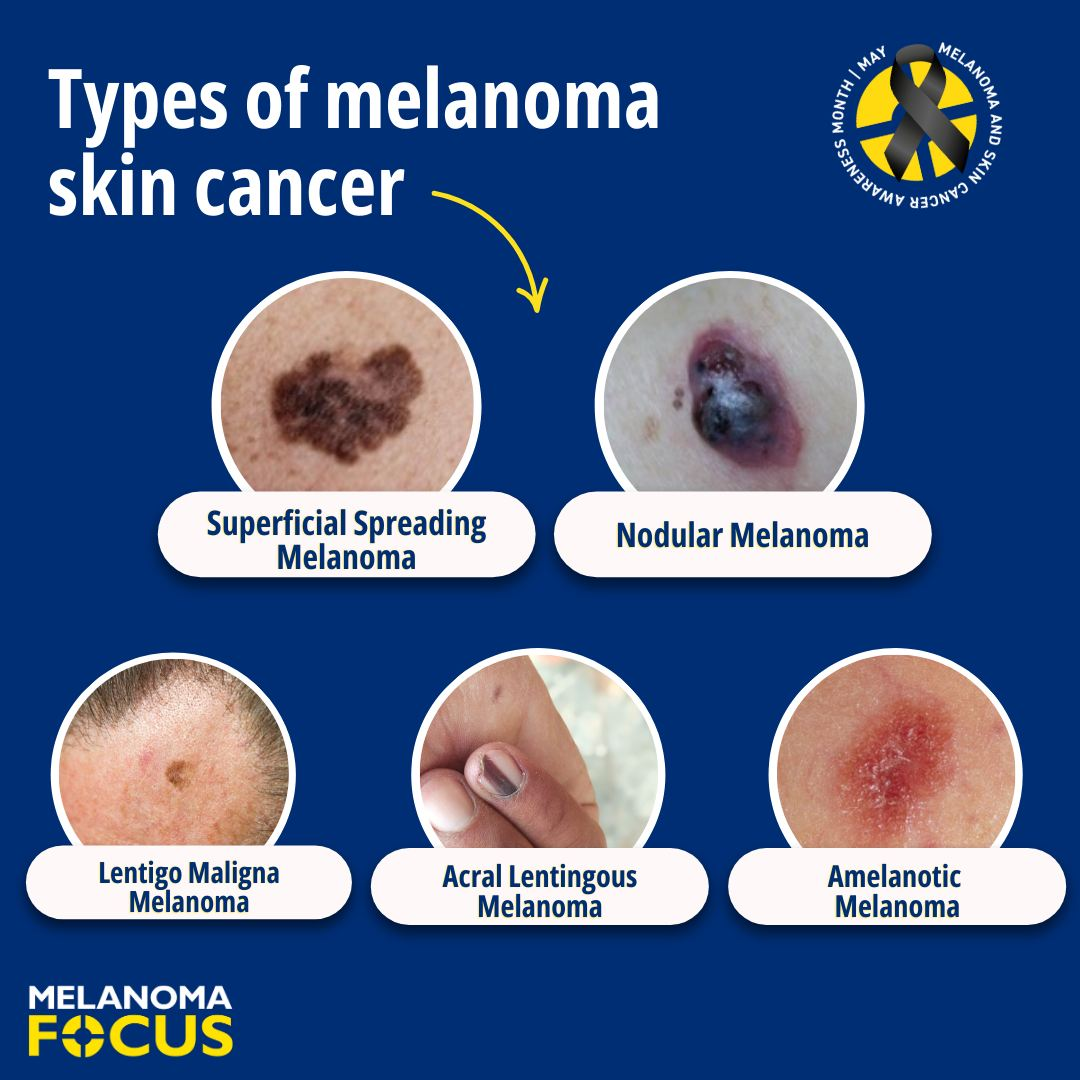
what are the major clinicopathological types of cutaneous melanoma?
superficial spreading melanoma
lentigo maligna melanoma
acral lentiginous melanoma
nodular melanoma
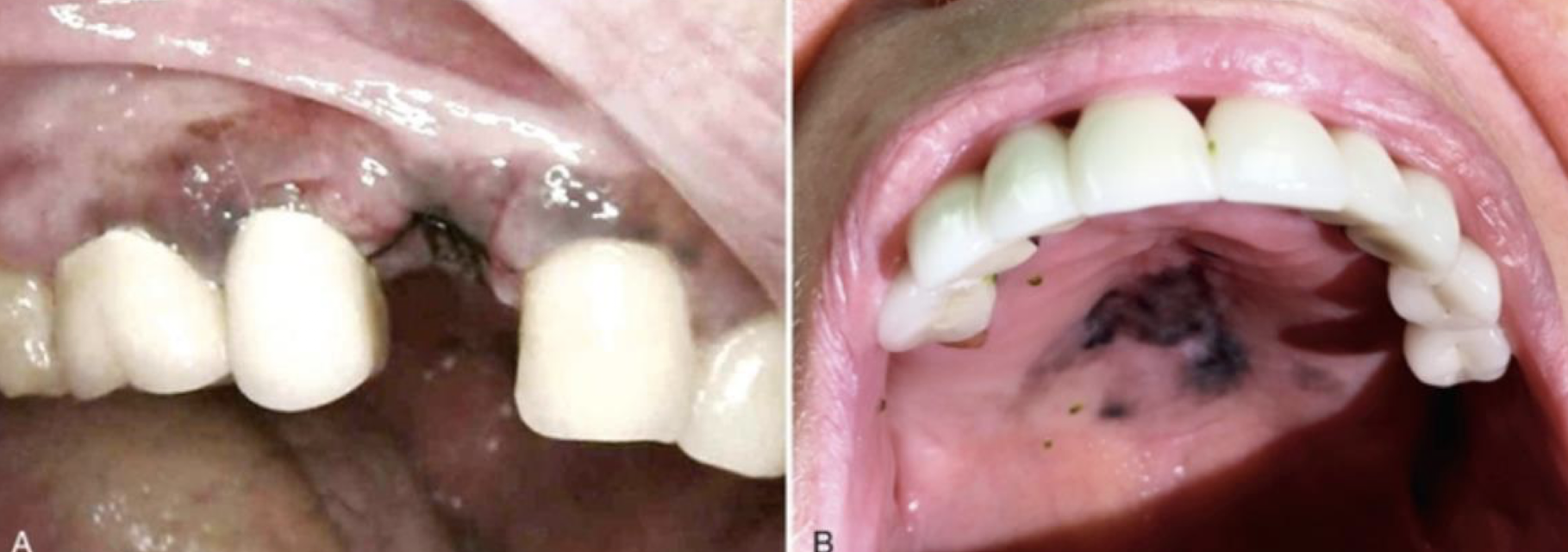
which premalignant/malignant melanin-associated pigmented lesion?
More prevalent in African Americans and Japanese
Arise de novo
7th decade, slight male predilection
Palatal mucosa, maxillary gingiva (>70%)
Breslow and Clark criteria (skin criteria) do not correlate with clinical behavior/prognosis
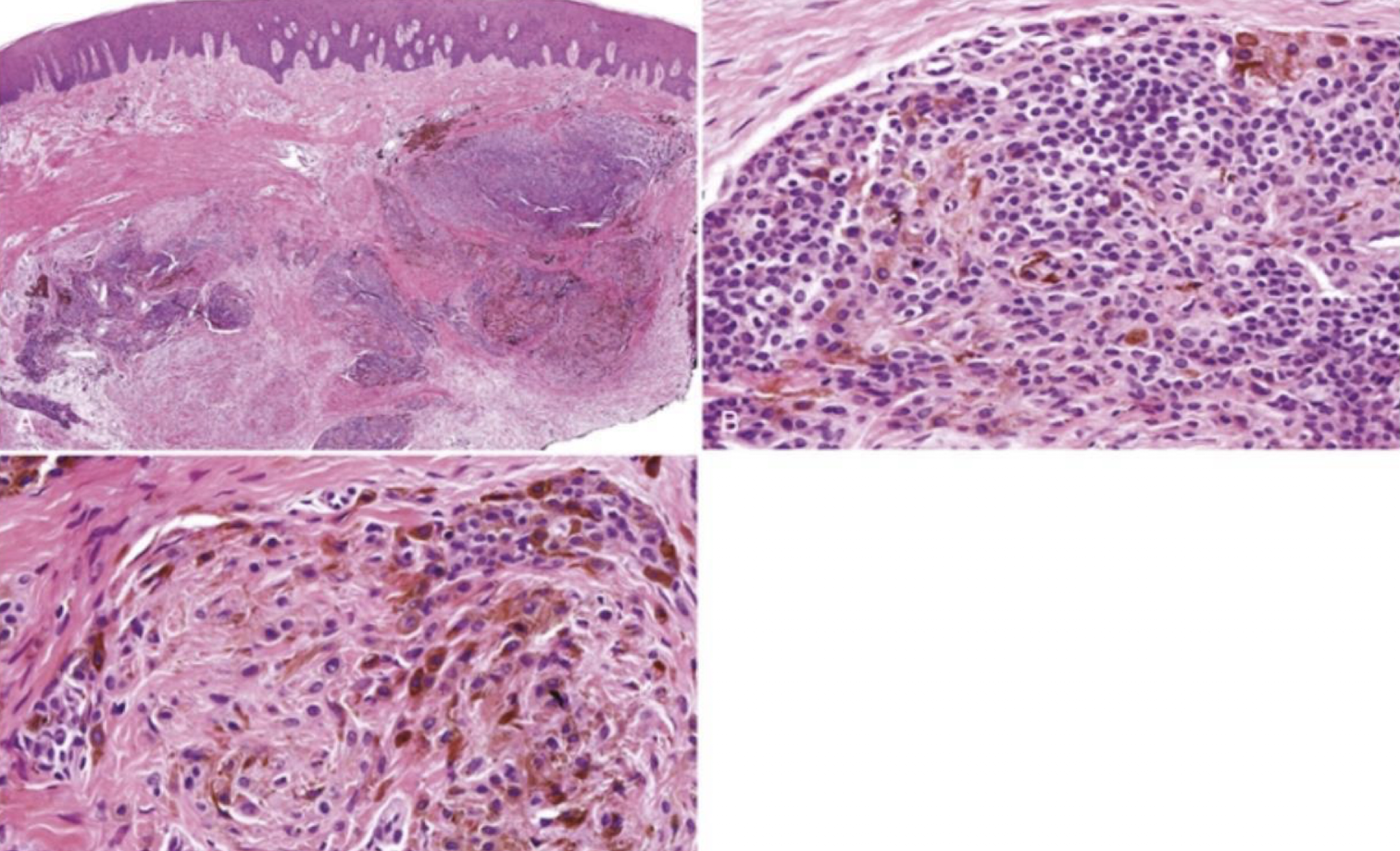
can be heterogenous or homogenous
oral melanomas
primary oral melanomas are less than (blank)% of all melanomas
1%
oral mucosal melanoma
KIT gene mutation
oral mucosal melanoma

heterogenous oral melanoma

oral melanoma
describe site distribution in primary head and neck mucosal melanoma
nasal cavity (47.5%), hard palate and gingiva (15%), alveolus (11.5%), sinonasal cavity (10%)
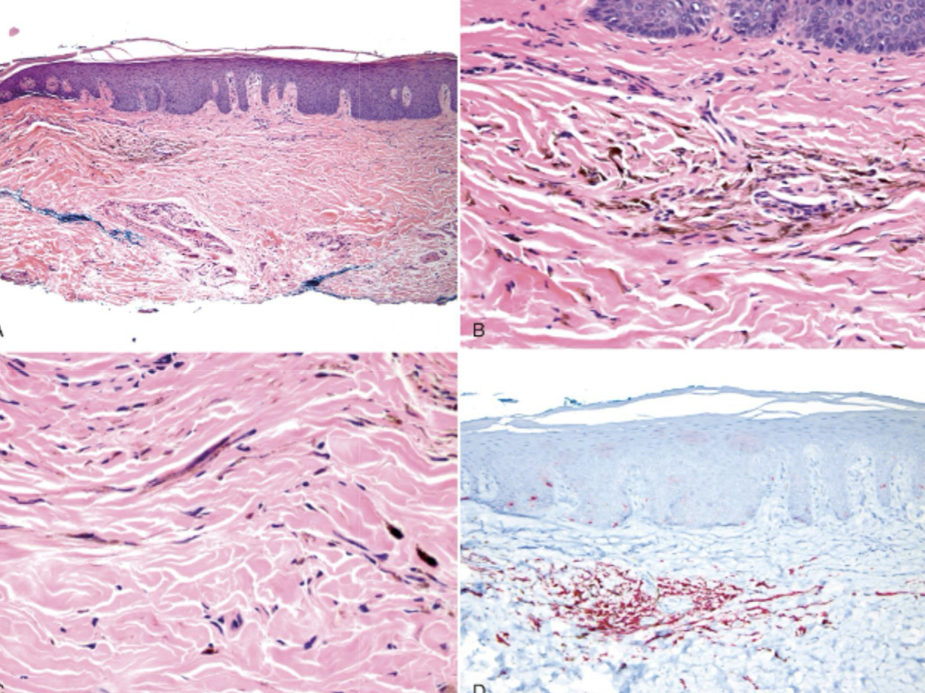
what are the five levels in Clark tumor invasion?
level I: in situ melanoma
level II: invasion of the papillary dermis by single cells or small nests
level III: invasive tumor usually as expansile nodule abutting on reticular dermal interface
level IV: invasion of reticular dermis
level V: invasion of subcutaneous fat
describe microstaging of primary head and neck mucosal melanoma
level I: pure in situ melanoma w/o evidence of invasion or in situ w microinvasion
level II: invasion up to lamina propria
level III: deep tissue invasion into skeletal muscle, bone, or cartilage
how is microinvasion defined in the context of primary head and neck mucosal melanoma ?
invasive or individual or clusters of < 10 atypical melanocytes near the epithelial-subepithelial junction
oral melanoma
what is the management for oral melanoma management?
Primary rx – excision with clear margins or radiation
50% recurrence
Nodal and distant mets in upto 65%
5 year survival is 10-20% (from mets)
oral pigmented lesions are considered ?
melanoma until proven otherwise
high risk sites of oral pigmented lesions include
maxillary gingiva and hard palate
multifocal lesions may suggest
systemic conditions
describe flow of finding a pigmented lesion: differential diagnosis, history, etc

what are some endogenous and exogenous reasons for pigmented lesions?
foreign material
melanin
vascular
saliva/mucin
cystic fluid
Which of the following cutaneous melanoma is found more commonly in the oral cavity?
a) Superficial Spreading Melanoma
b) Acral Lentiginous Melanoma
c) Nodular Melanoma
d) Metastatic Melanoma
e) Lentigo Maligna Melanoma
b) Acral Lentiginous Melanoma
describe the differences between:
appearance, growth pattern, and location
Superficial Spreading Melanoma is the most common type, growing horizontally before invading deeper
Nodular Melanoma grows vertically from the start and is more aggressive
Acral Lentiginous Melanoma is found on the palms, soles, and under nails, and is not strongly linked to sun exposure
Lentigo Maligna Melanoma typically affects older people on sun-damaged skin like the face, and has a prolonged horizontal growth phase before becoming invasive
Metastatic Melanoma is a later stage where the cancer has spread to other parts of the body.