Ch. 9 Cardiac Muscle
1/43
Earn XP
Description and Tags
Flashcards covering the key concepts of cardiac muscle, the cardiac cycle, and heart regulation.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
44 Terms
What are the two separate pumps of the heart?
The right heart (pulmonary circulation) Chamber:
responsible for venous return
distributes blood to lungs to create oxygenated blood
Left heart (peripheral circulation)
related to process of cardiac output
distributes blood to entire body system
Each side has two chambers, the atrium is the primer pump and the ventricles are the Main pump
What are the three types of cardiac muscle?
Atrial muscle
Ventricular muscle
Excitatory and conductive muscle
How does atrial and ventricular cardiac muscle contract compared to skeletal muscle?
Like skeletal muscle except the duration of contraction is longer in cardiac muscle due to the slow closing of voltage-gated calcium channels prolonging depolarization.
Both uses Calcium for muscle contraction however, cardiac muscle uses calcium from the ECF because there is not enough calcium in the SR
What unique property do excitatory cardiac muscles exhibit?
Automatic rhythmical electrical discharge (action potential or conduction).
Describe the anatomy of the cardiac muscle
Fibers form a latticework of fibers of dividing, recombining, and spreading again
Have actin and myosin filaments like skeletal muscle
Unique Features:
longer contraction duration
Intercalated discs
Functional syncytium: atrial and ventricular
What are intercalated discs?
make the cardiac tissue one that connects cardiac muscle cells, allowing for synchronized contraction and communication between cells.
joined with gap junctions for cell-to-cell communication and ion diffusion
Why do cardiac cells have the ability to spread action potential easily?
Because they have specialized intercalated discs and gap junctions that facilitate rapid electrical communication between cells.
lack of intercalated discs would slow the contraction rate and due to slow signal conduction
What are the two syncytium in the heart?
Why are they separated?
*syncytium is a group of cells that function as a single unit because they are electrically and mechanically connected.
Atrial syncytium and ventricular syncytium.
Separated by the fibrous tissue - Atrioventricular Valve (a non-conductive tissue) because the atria and ventricles do not contract together, but the ventricles are delayed to ensure proper blood pumping of the heart
How do action potentials travel within the heart?
By way of a specialized conductive system (A-V bundle).
What is the resting membrane potential (RMP) of cardiac muscle?
What about action potential?
-85 mV
+20 mV during an action potential
After the spike, the membrane remains depolarized for 0.2 seconds (plateau) followed by rapid repolarization
Why does ventricular contraction last 15 times as long in cardiac muscle than skeletal muscle?
Due to the depolarization plateau
influx of Na+ (fast channel) and Ca+ (slow channel)
The slow channels open longer causing more Ca+ to enter the cell for contraction
What happens to K+ permeability at the onset of action potential in cardiac muscle?
It decreases about 5-fold, preventing early return of RMP.
What is the difference between absolute and relative refractory?
absolute - when a cell can’t respond to any stimulus regardless of how strong
Relative - when a second action potential can be generated but only with a stronger than usual stimulus; occurs after absolute
T/F: Ventricles have a shorter refractory period?
False - atrias do
Atria need to be ready to contract more frequently to accommodate the rapid filling and pushing cycles to the ventricles
Atria have thinner walls and work with lower pressure than ventricles so they don’t have stronger contractions than ventricles = shorter action potential = shorter refractory period
What is E-C coupling?
The mechanism by which an action potential causes myofibrils of muscle to contract.
Action potential will travel down the T-Tubles and large number of calcium ions enter from the T-tubles
the SR in cardiac muscle is less developed so they are unable to store the volume of calcium needed for contraction
Calcium will come from ECF
How many calcium pumps are present in the cardiac cycle?
Two
first is at the SR as Calcium is pumped into the SR
second is at the cell membrane, pumping Ca out into the ECF and Na in with counter-transport (secondary active transport) to establish a membrane potential
What is the cardiac cycle?
Cardiac events from the beginning of one heartbeat to the beginning of the next and stimulated by action potential of the sinus node
Action potential travels through the atria, to the AV node, to the ventricles and causes the ventricles to contract
Where is the sinus node located?
In the superior lateral wall of the right atrium.
Describe the Atria as Primer Pumps
80% of the blood flow from the great veins flow (passively) into the right atria and to the right ventricles
Atrial contraction is responsible for the additional 20% filling of ventricles with pumping - important for exercise
T/F: atrial pumping is not necessary and will become useful with exercise
true
example of seeing function of full heart function and atria function is applying a stress-test to patient
What are the three atrial pressure waves?
A wave - for atrial contraction
The right atrium increases by 4-8 mm Hg in pressure which will lead to an increase in the ventricles as well
left atrium increases pressure to 7-8 mmHg
left atrium will always have a greater pressure than the right atrium.
C wave - begins at ventricular contraction and is caused by backflow of blood of blood into the atria by bulging of the AV valve as the pressure in the ventricle increases. Bulging will occur in atria.
V Wave - at the end of ventricular contraction and occurs at atrial filling while AV valve is closed.
V wave will disappear when the A-V valve opens
source of 80% of venous return
Describe the relationship between Atrial pressure and Ventricular volume
Prior to atrial contraction, ventricular volume increases due to passive blood flow
Atrial contraction will occur when atrial pressure is greater than ventricular pressure
Between the cessation of atrial contraction and the c-wave is the occurance of isovolumic contraction = same volume of blood in the ventricles
C-wave occurs due to bulging of AV valve BUT valve is not open
At the C wave, there will be a decrease in ventricular volume due to decrease in ventricular volume and will cause atrial pressure to decrease too
the V-wave is the end of ventriular contraction and blood flows into the atria, and AV valve is now open
Repeat cycle
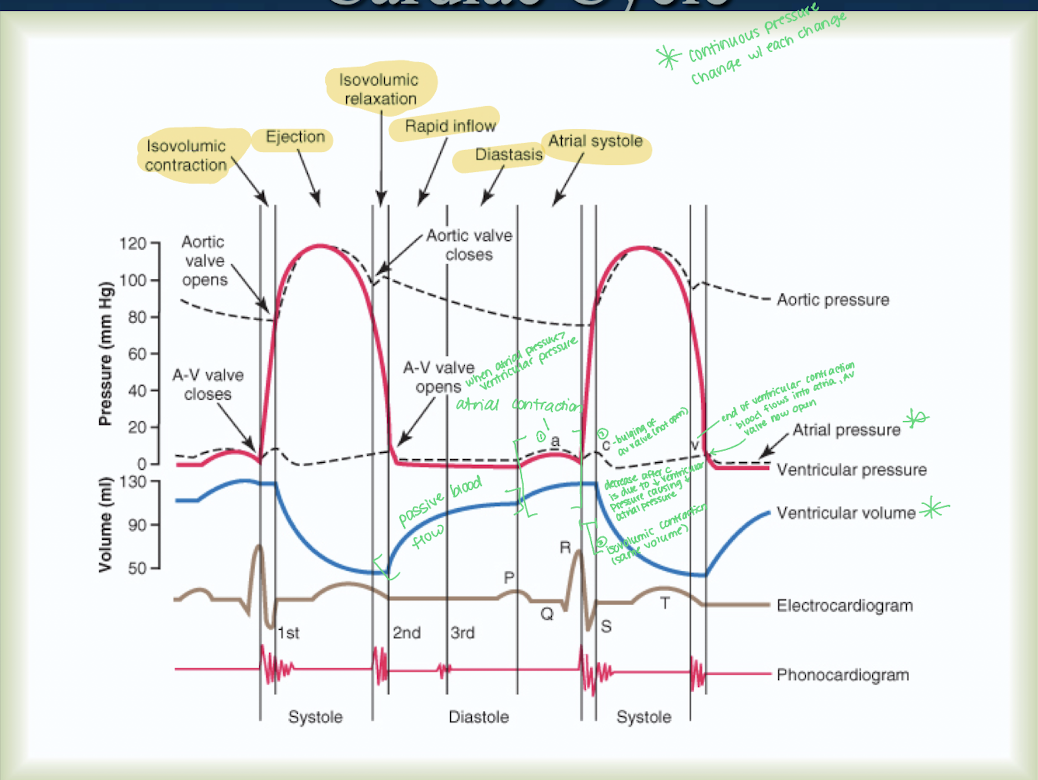
What occurs during isovolumic contraction during the emptying of the ventricles?
Contraction of ventricles increasing pressure to the point of opening the aortic and pulmonary valves without emptying.
What is the approximate pressure when the left ventricle valve opens?
Approximately 80 mm Hg.
Describe how the Ventricles work as pumps.
Undergo a Rapid filling phase
Atria will collect blood during ventricular systole.
Once ventricles relax, the atrial pressure will excede ventricular pressure and the AV valve will open
phase lasts for a 1/3 of distally = very fast
Emptying of Ventricles
Ventricles will undergo isovolumic contraction - contraction of ventricles increasing pressure to point of opening the aortic and pulmonary valves without emptying
Ejection of blood from ventricles with 70% with rapid ejection and 30% slowly
Isovolumic Relaxation - ventricles relax but there is no change in volume because the AV valve is closed (intraventricular pressure decreases with no change in volume)
What are the four phases of the Pressure-Volume curve/Ventricular pumping?
Period of Filling, Period of Isovolumic Contraction, Period of Ejection, Period of Isovolumic Relaxation.
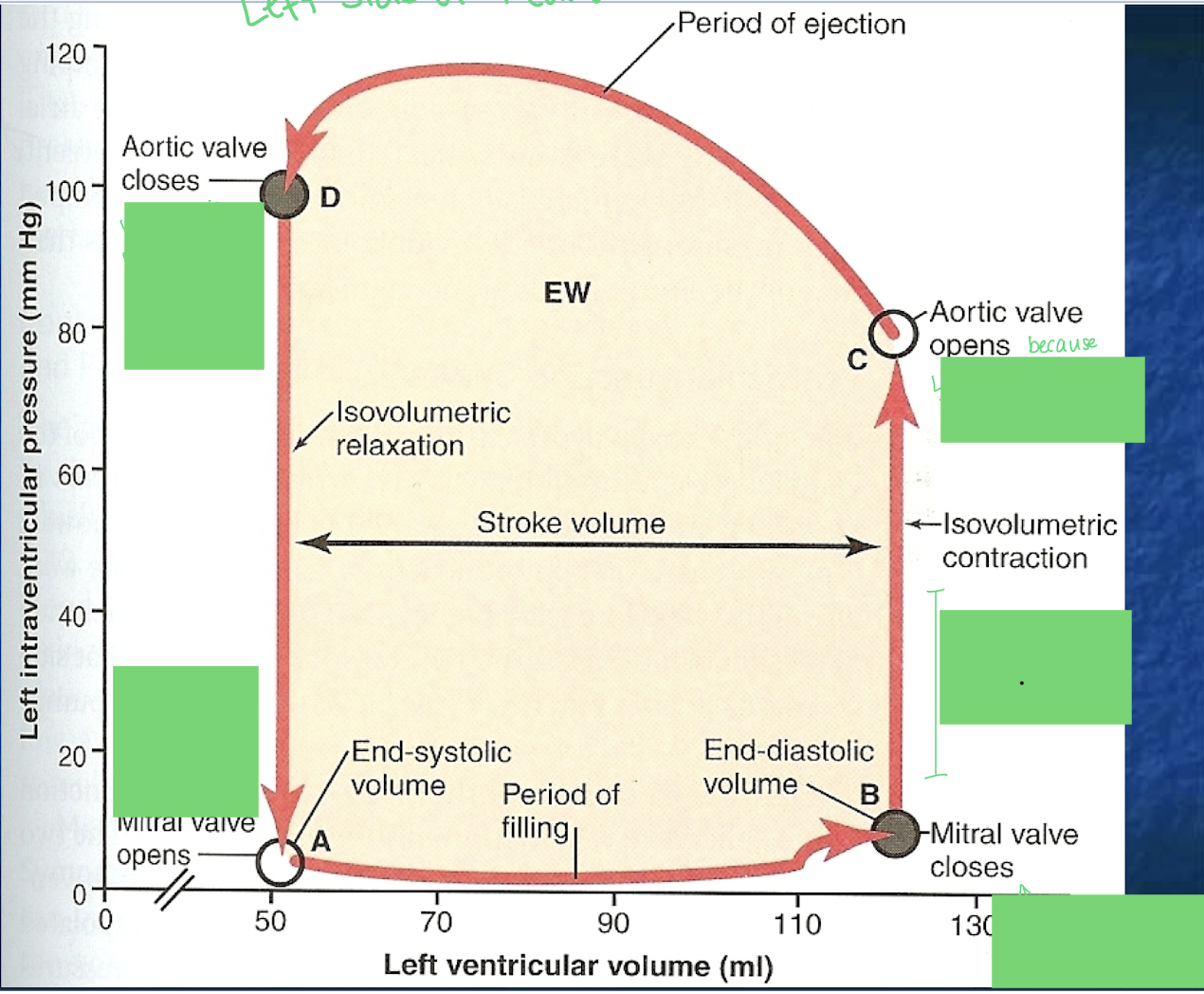
Describe each part of the Pressure Volume curve
*shows cardiac output in the left side of the heart
Mitral Valve Closed = End diastolic volume
Mitral valve (between L atria and L ventricle) is closed because ventricular pressure > atrial pressure
Max volume in LV
LVentricle contracts (systole) increasing Ventricular pressure
both mitral and aortic valve are closed to the volume remains the constant = isovolumetric contraction
Aortic Valve will open when ventricular pressure > Aortic pressure
Ejection phase as blood flows from LVentricle to Aorta
Aortic Valve closes because Aortic pressure > ventricular pressure due to ventricular volume decrease = decrease in pressure
end of Systole
Isovolumetric relaxation - constant volume
Mitral Valve open
Atrial pressure > ventricular pressure
blood flows from atria to ventricle
Ventricle fills with blood till ventricular pressure > atrial pressure
REPEAT
What is preload vs afterload
Preload is End diastolic pressure (increased blood volume, increased pressure, and vise versa)
Afterload is pressure in the artery leaving ventricles (resistance)
pressure in the aorta
Has a greater resistance to stroke volume
How is the volume pumped by the heart regulated?
Intrinsic regulation determined by volume, and heart rate and strength of contraction by the ANS.
What are the two equations to find cardiac output?
CO = HR x SV
CO = Arterial Pressure / TPR
What is baseline cardiac output in males and females about?
5 L/min
If person A has a baseline cardiac output of 5 L/min and their heart rate is 70 compared to person B has a heart rate of 40. What can you say about how their heart is working?
Person A will make more work for their heart
Person B will have a higher SV (CO=HR x SV) but less work for the heart and better contractility
What is the Frank-Starling mechanism?
Intrinsic ability of heart to adapt to increasing volumes of venous return. The greater the heart is stretched (preload), the greater the force of contraction. Which will create optimal amount of overlap of filaments. Stretch of the right atrium (increases firing of SA node) increases heart rate, increasing CO.
venous return determines the amount of blood pumped by the heart
peripheral tissues control and regulate own local blood flow
How does the sympathetic nervous system affect the heart?
Increases heart rate and increases force of heart contraction.
How does the parasympathetic (Vagal) nervous system affect the heart?
Decreases heart rate and decreases force of muscle contraction; distributed mainly to atria.
What is the effect of sympathetic stimulation on cardiac pumping?
It can increase rate from rest (70 to 200 bpm)
increase contractility which will increase volume of blood pumped (increase SV)
sympathetic stimulation can’t reduce cardiac pumping below 30% normal
What is the effect of strong Vagal stimulation on the heart?
Strong stimulation can stop the heartbeat for a few seconds, but then the heart “escapes”.
It can decrease strength of heart muscle.
The rate is impacted greater than the strength
What is normal right atrial pressure value?
0 mmHg
What effect does excess K+ have on the heart?
Causes the heart to become dilated, flaccid, and slows heart rate.
It can also block conduction from atria to ventricles leading to stopping HR
Decreases RMP and intensity of AP = inability to move blood beyond aortic pressure
What could cause blood to not move beyond aortic pressure?
High K+ levels
What effect does excess Ca2+ have on the heart? How about deficiency?
Should we be concerned?
Causes the heart to go toward spastic contraction.
Deficiency causes flaccidity, similar to high K+
No, calcium is regulated tightly
How does increased temperature affect heart rate? How about decreased?
It causes increased heart rate due to increased permeability of ions.
Decreased temp decreases heart rate
During exercise, why does atrial contraction become more important?
A. It increases the C wave
B. It helps maintain preload
C. It lengthens diastole
D. It reduces venous return
B. It helps maintain preload
preload refers to the volume of blood in the ventricles at the end of diastole — it's directly related to how stretched the heart muscle is before it contracts.
During exercise, heart rate increases, which shortens diastole (the relaxation/filling time).
With less time to fill passively, atrial contraction becomes more important to push additional blood into the ventricles, helping to maintain adequate preload and stroke volume.
Which scenario best illustrates the Frank-Starling mechanism?
A. Increased sympathetic tone causes a faster HR
B. Increased venous return leads to stronger contraction and higher SV
C. Decreased Ca²⁺ influx reduces contractility
D. Vagal stimulation reduces ventricular ejection
B. Increased venous return leads to stronger contraction and higher SV
*Frank Starling is related to venous return
The greater the stretch of the cardiac muscle fibers (from increased venous return), the stronger the contraction.”
This means that if more blood returns to the heart (higher preload), the ventricles stretch more, and contract more forcefully, increasing stroke volume (SV