Peripheral Nervous System: Nerve Structure, Classification, and Cranial Nerves
1/105
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
106 Terms
Nerve
cordlike organ of PNS
Endoneurium
loose connective tissue that encloses axons and their myelin sheaths (Schwann cells)
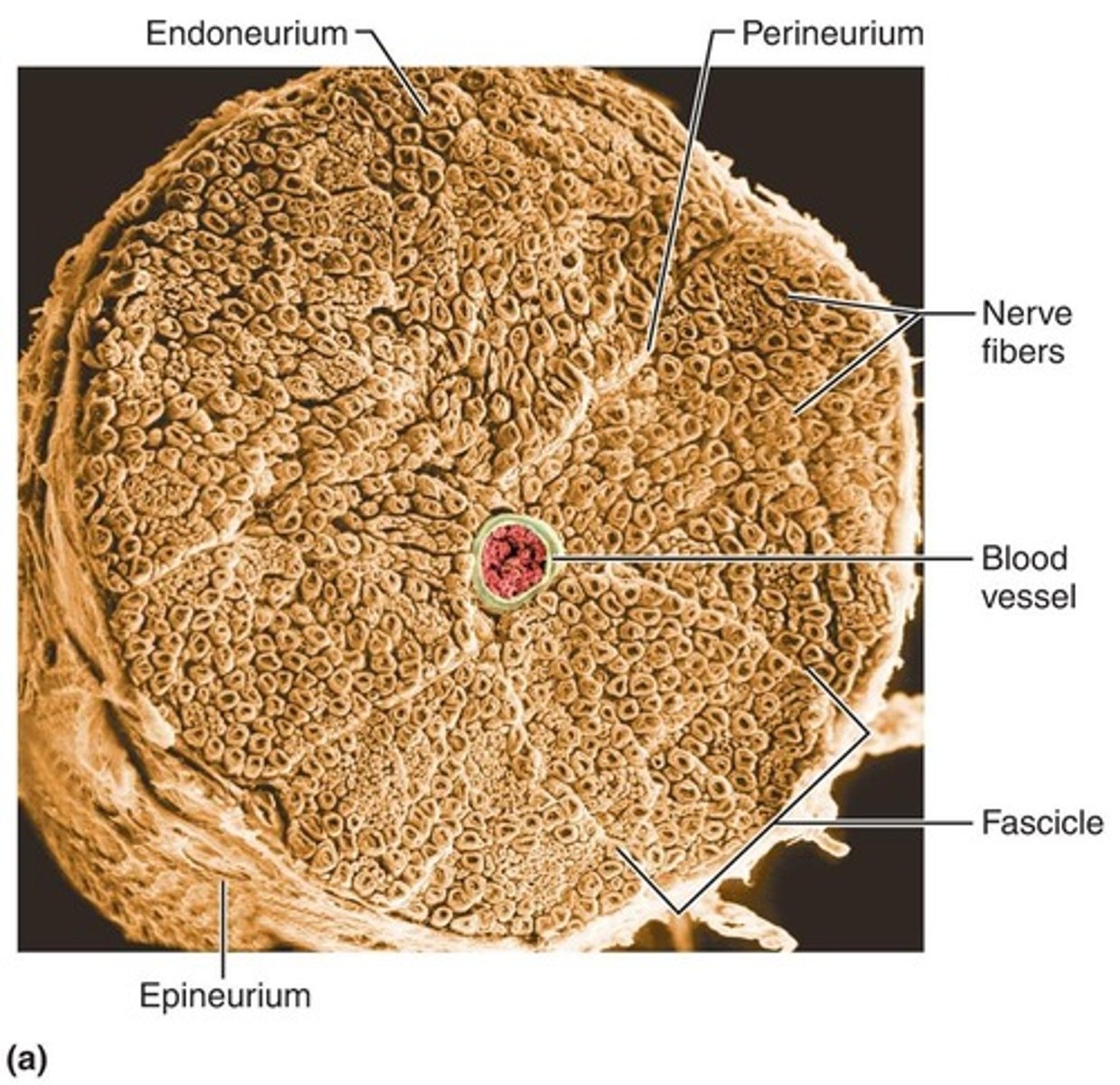
Perineurium
coarse connective tissue that bundles fibers into fascicles
Epineurium
tough fibrous sheath around all fascicles to form the nerve
Mixed nerves
contain both sensory and motor fibers; impulses travel both to and from CNS
Sensory (afferent) nerves
impulses only toward CNS
Motor (efferent) nerves
impulses only away from CNS
Somatic afferent
sensory from muscle to brain
Somatic efferent
motor from brain to muscle
Visceral afferent
sensory from organs to brain
Visceral efferent
motor from brain to organs
Ganglia
contain neuron cell bodies associated with nerves in PNS
Dorsal root ganglia
ganglia associated with afferent nerve fibers that contain cell bodies of sensory neurons
Autonomic ganglia
ganglia associated with efferent nerve fibers that contain autonomic motor neurons
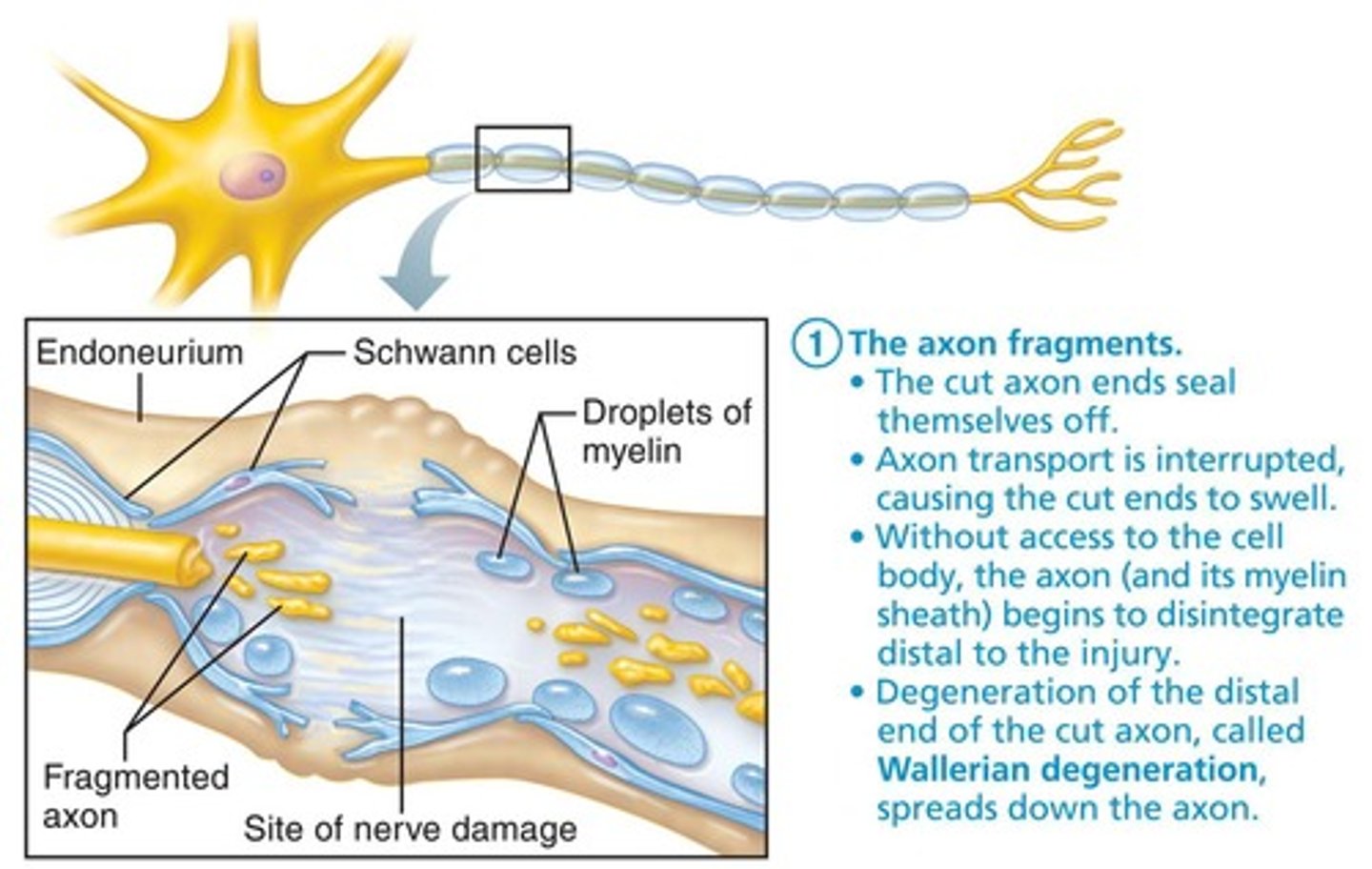
Wallerian degeneration
axon fragments and myelin sheaths distal to injury degenerate; degeneration spreads down axon
CNS axons
most CNS fibers never regenerate
CNS oligodendrocytes
bear growth-inhibiting proteins that prevent CNS fiber regeneration
Astrocytes
at injury site form scar tissue
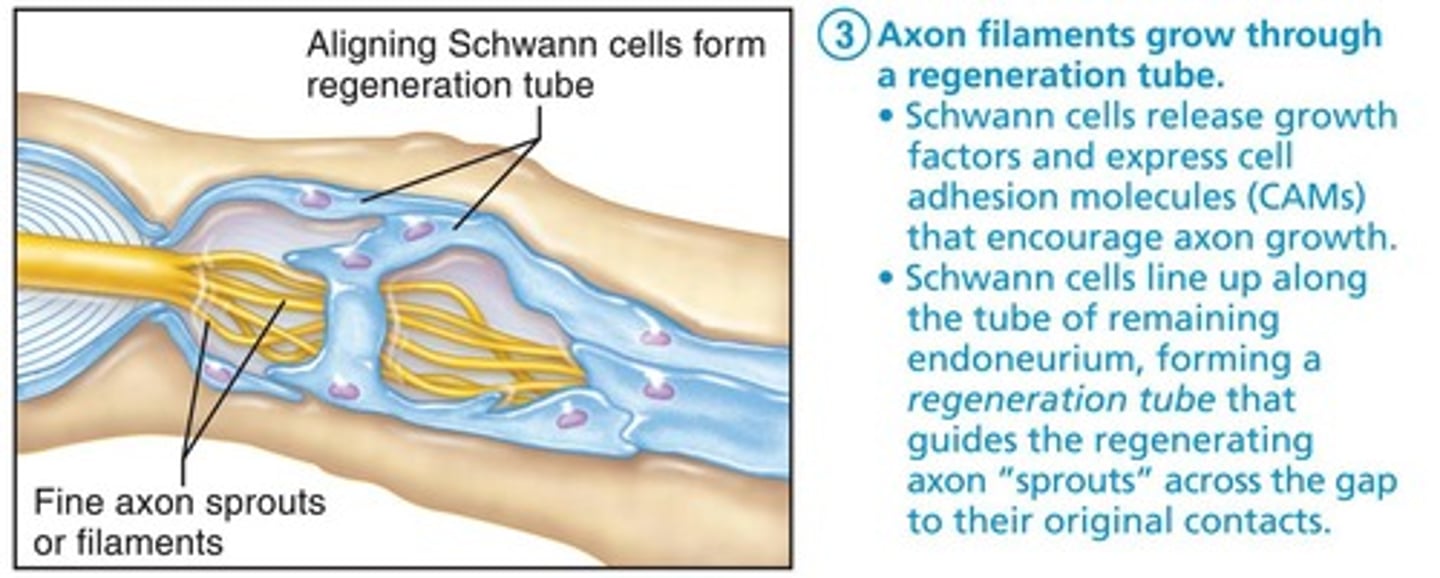
PNS axons
can regenerate if damage is not severe
Regeneration tube
axon filaments grow through this structure during regeneration
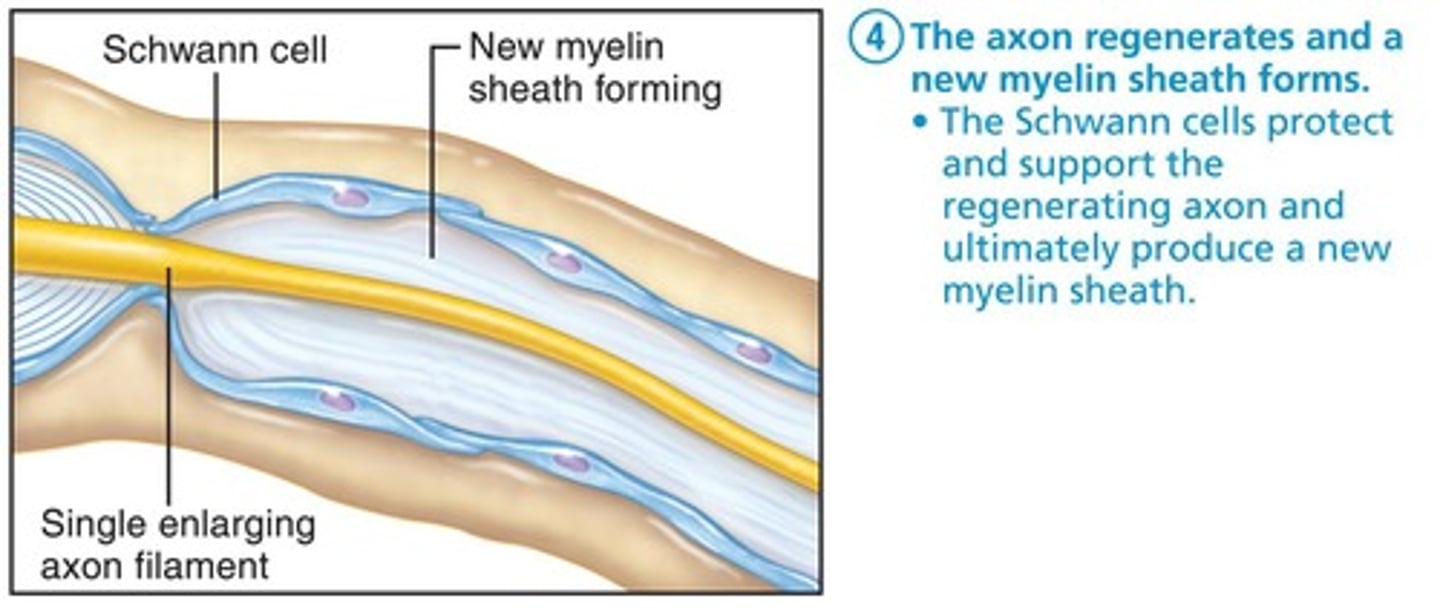
New myelin sheath
forms after axon regenerates
Cranial Nerves
12 pairs of cranial nerves are associated with brain
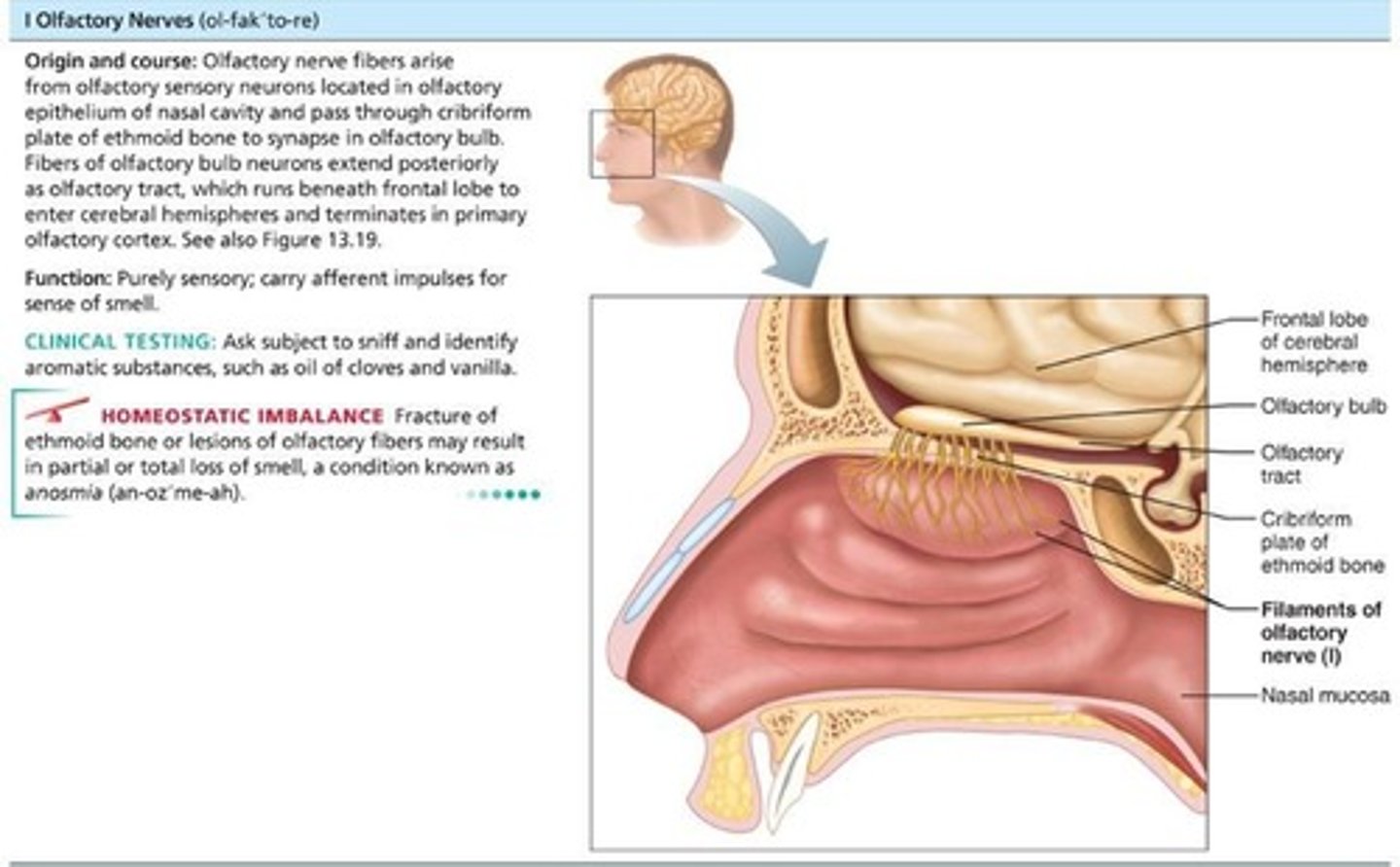
Olfactory Nerves (I)
Sensory nerves of smell; run from nasal mucosa to olfactory bulbs; pass through cribriform plate of ethmoid bone; fibers synapse in olfactory bulbs; pathway terminates in primary olfactory cortex; purely sensory (olfactory) function.
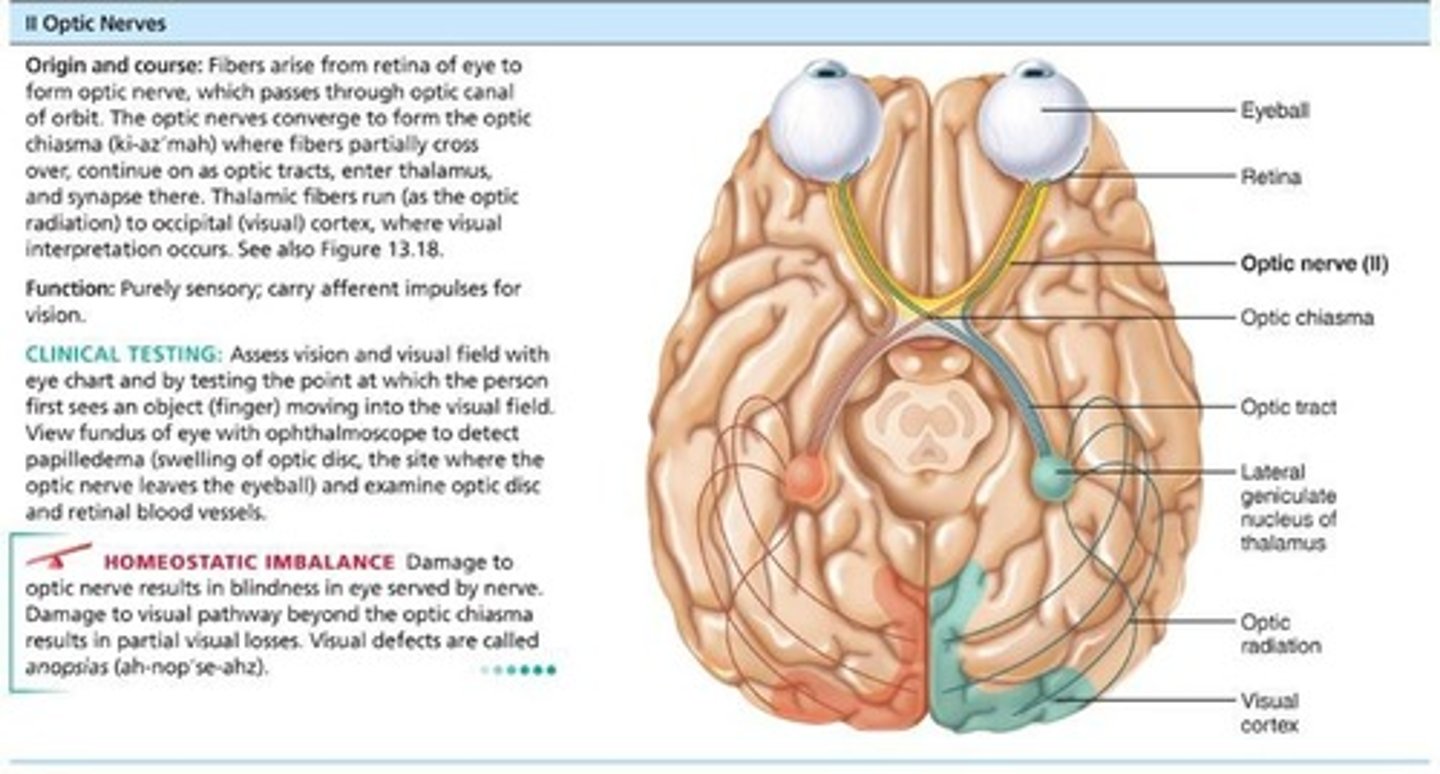
Optic Nerves (II)
Arise from retinas; really a brain tract; pass through optic canals, converge, and partially cross over at optic chiasma; optic tracts continue to thalamus, where they synapse; optic radiation fibers run to occipital (visual) cortex; purely sensory (visual) function.
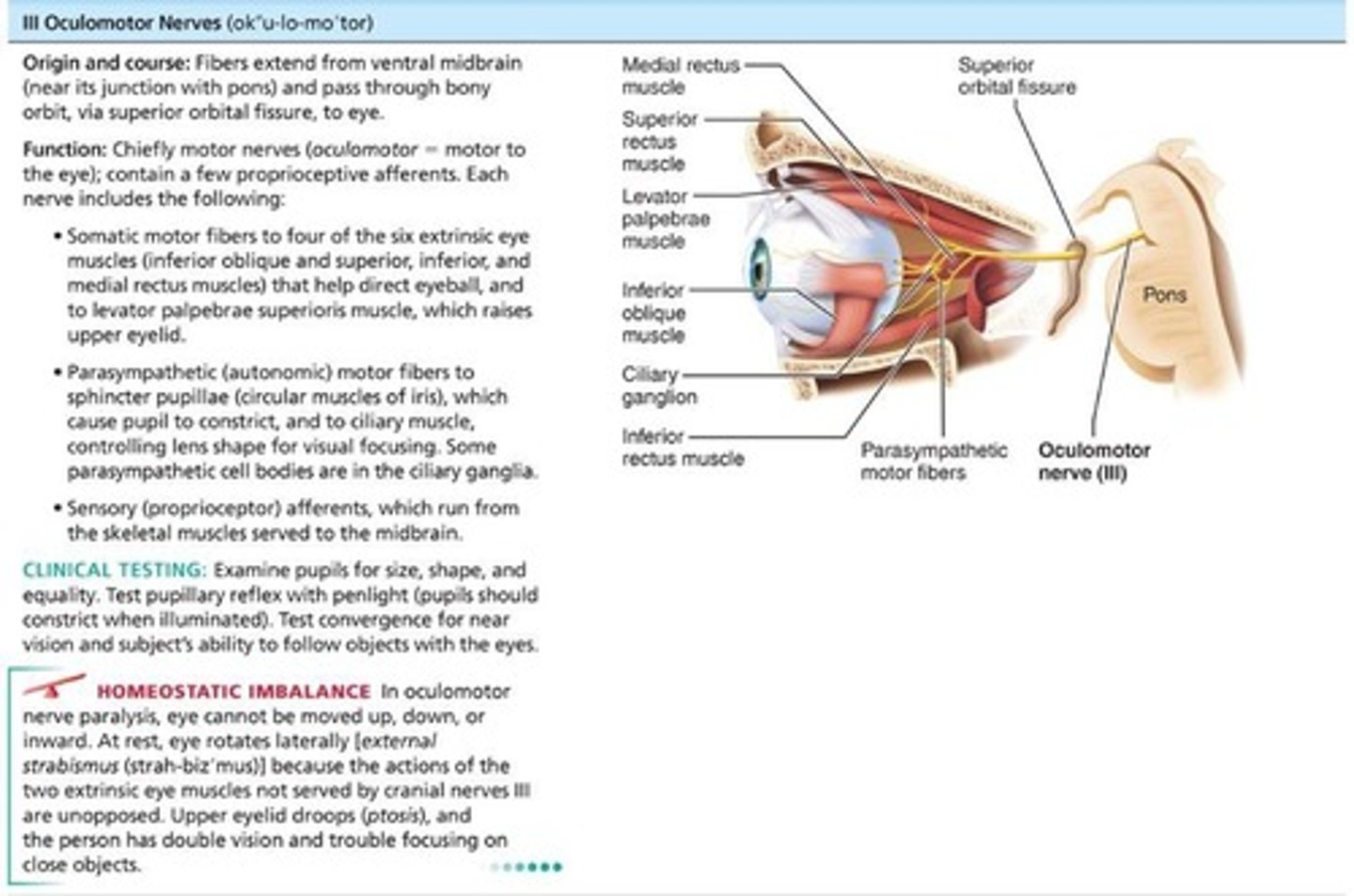
Oculomotor Nerves (III)
Fibers extend from ventral midbrain through superior orbital fissures to four of six extrinsic eye muscles; function in raising eyelid, directing eyeball, constricting iris (parasympathetic), and controlling lens shape.
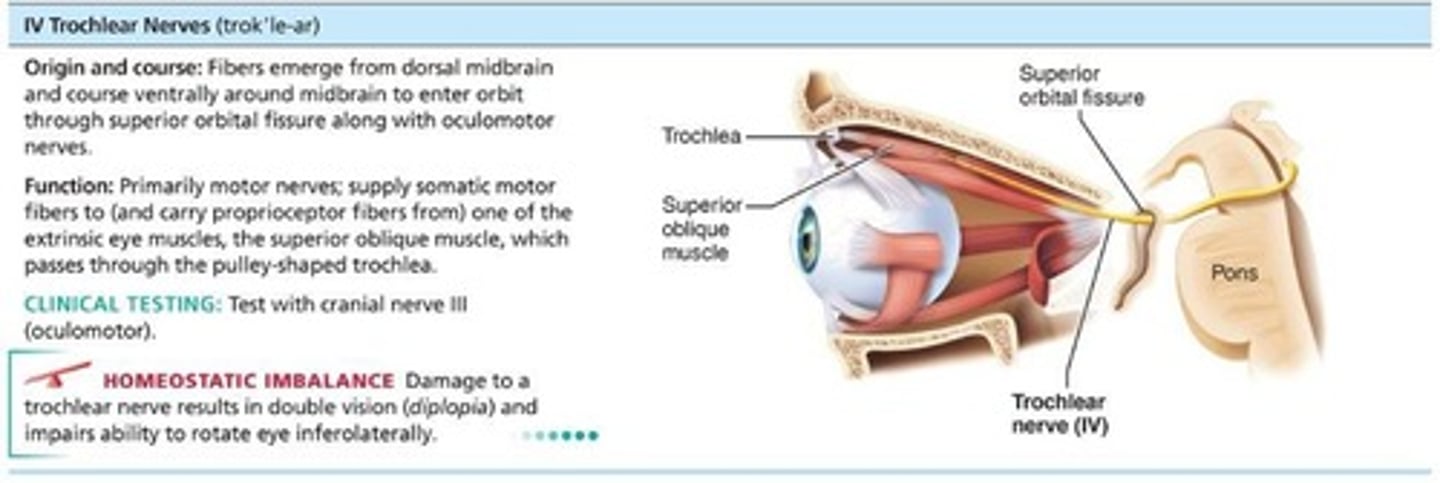
Trochlear Nerves (IV)
Fibers from dorsal midbrain enter orbits via superior orbital fissures to innervate superior oblique muscle; primarily motor nerve that directs eyeball.
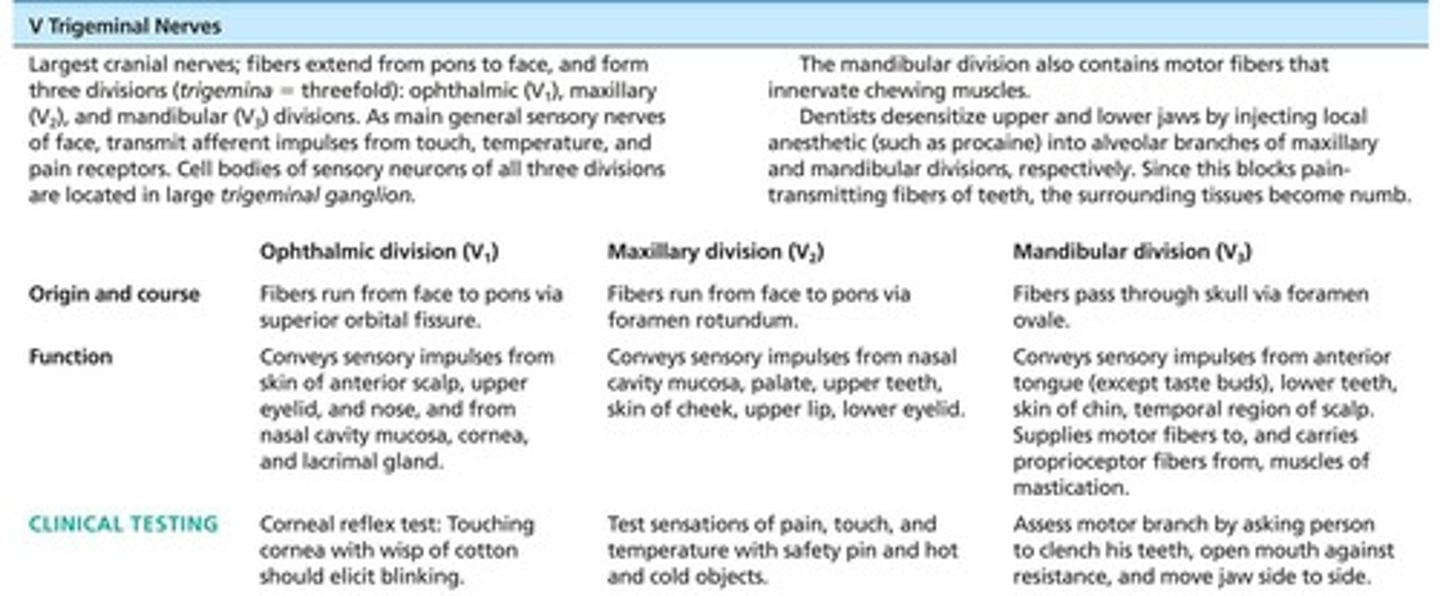
Trigeminal Nerves (V)
Largest cranial nerves; fibers extend from pons to face; three divisions: Ophthalmic (V1) passes through superior orbital fissure, Maxillary (V2) passes through foramen rotundum, Mandibular (V3) passes through the foramen ovale; convey sensory impulses from various areas of face (V1 and V2); supply motor fibers (V3) for mastication.
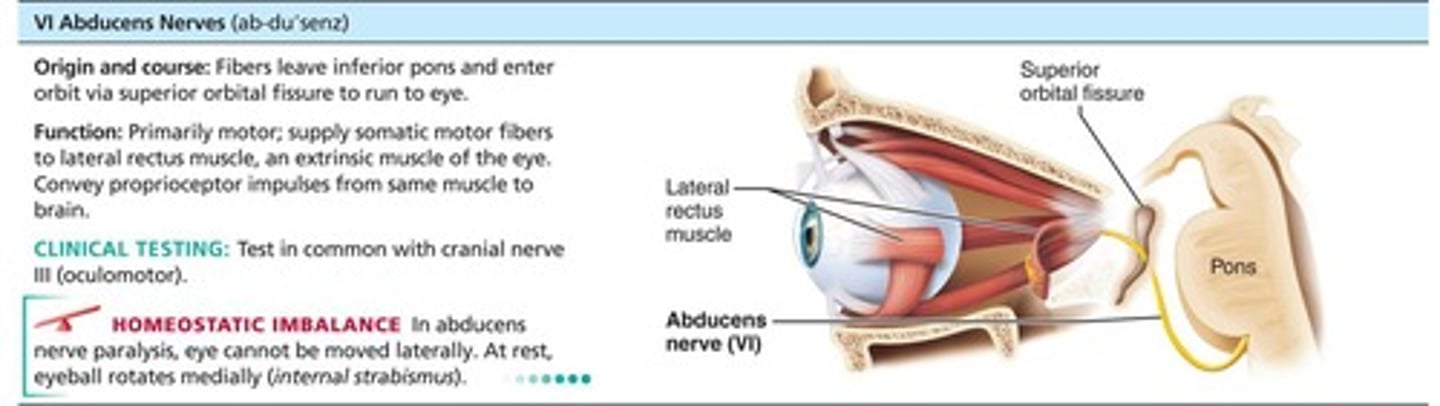
VI: Abducens nerves
Fibers from inferior pons enter orbits via superior orbital fissures. Primarily a motor, innervating lateral rectus muscle.
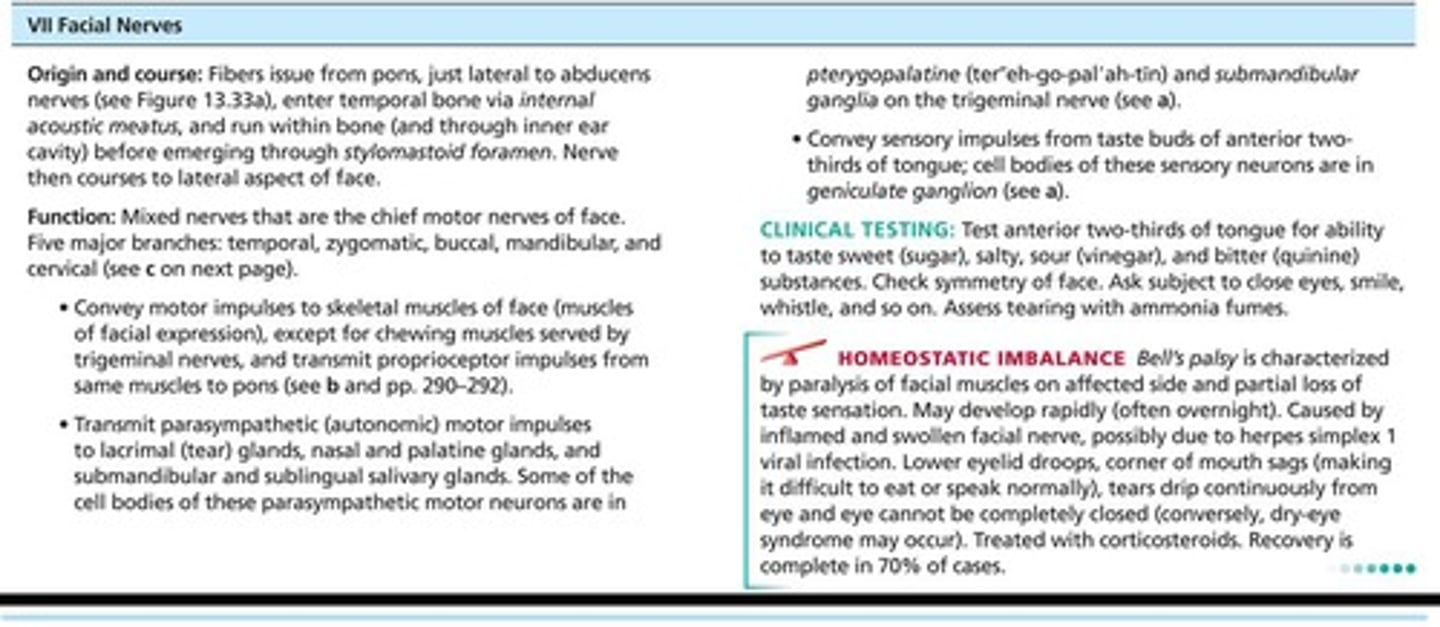
VII: Facial nerves
Fibers from pons travel through internal acoustic meatuses and emerge through stylomastoid foramina to lateral aspect of face. Chief motor nerves of face with five major branches. Motor functions include facial expression, parasympathetic impulses to lacrimal, and salivary glands. Sensory function (taste) from anterior two-thirds of tongue.
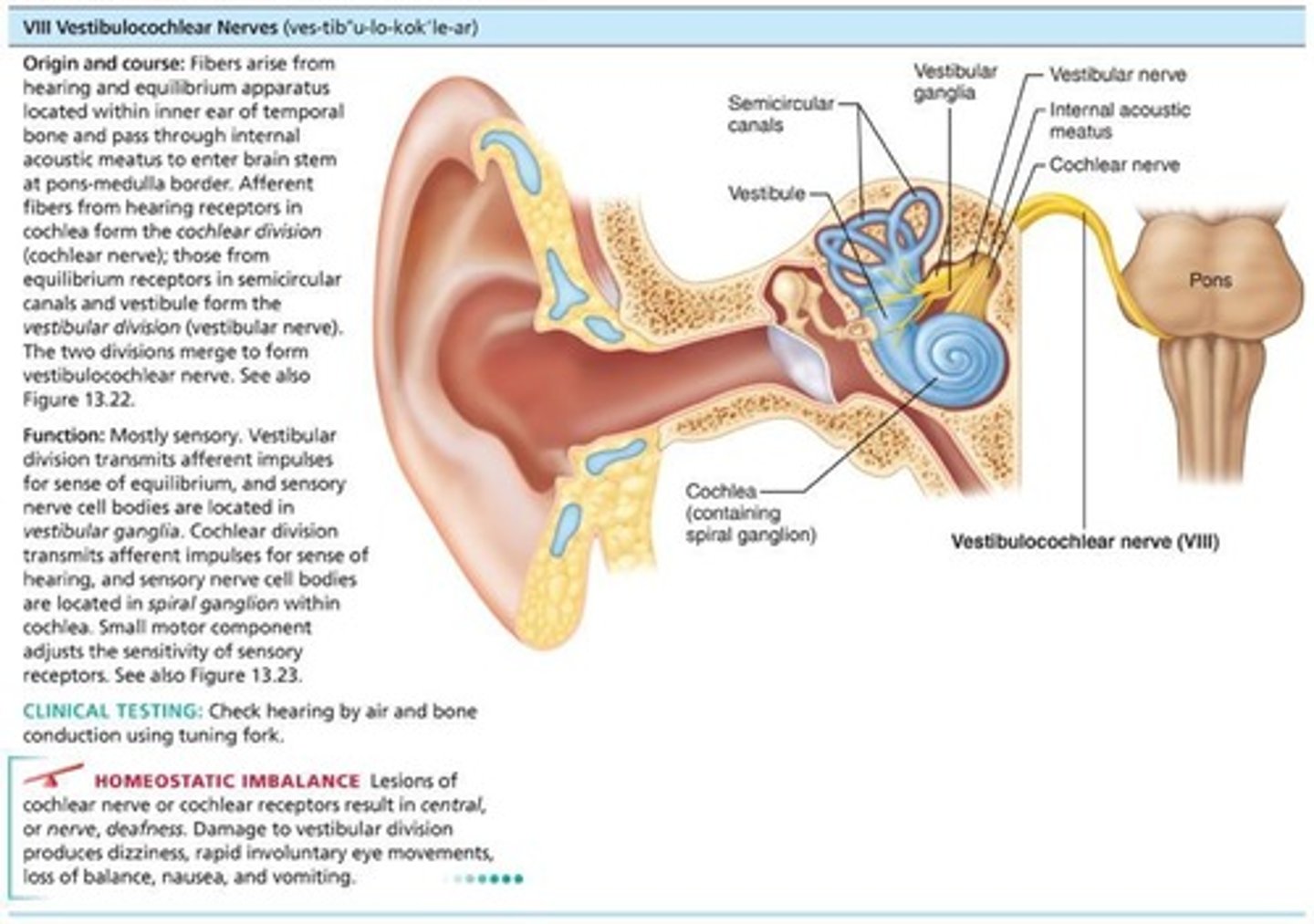
VIII: Vestibulocochlear nerves
Afferent fibers from hearing receptors (cochlear division) and equilibrium receptors (vestibular division) pass from inner ear through internal acoustic meatuses and enter brain stem at pons-medulla border. Mostly sensory function; small motor component for adjustment of sensitivity of receptors. Formerly auditory nerve.
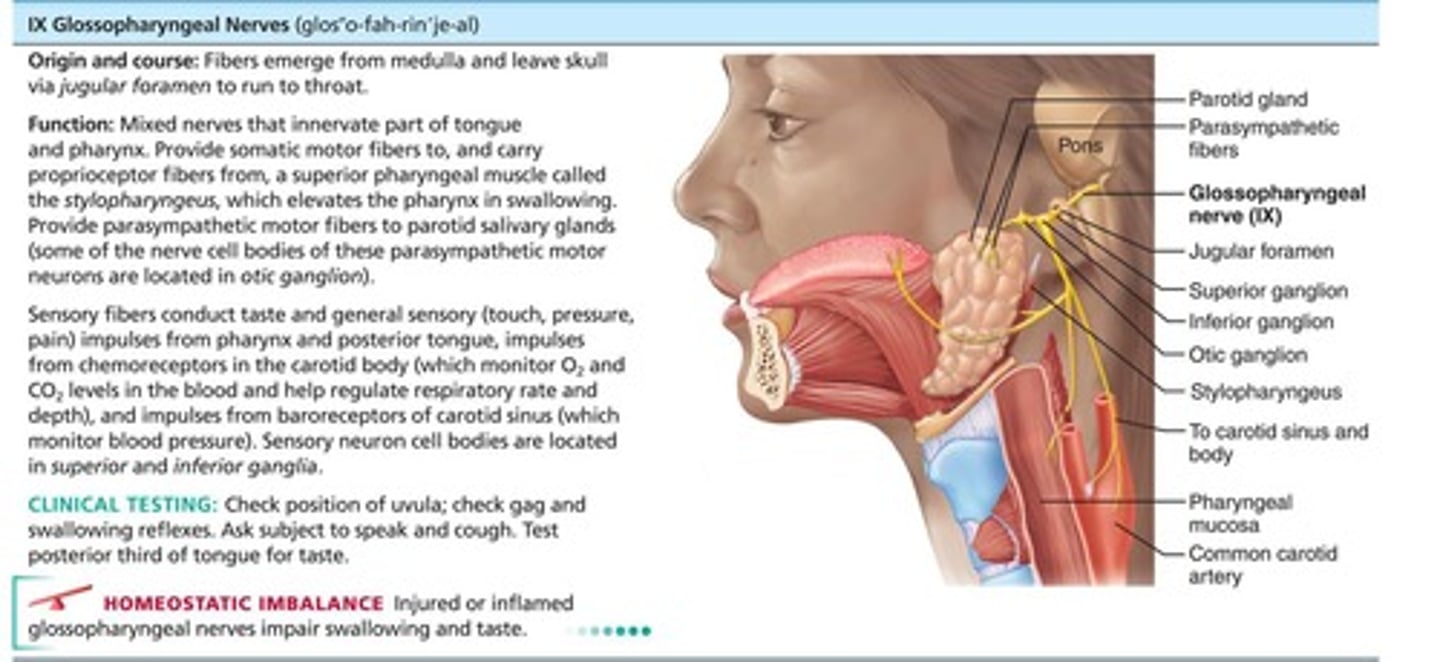
IX: Glossopharyngeal nerves
Fibers from medulla leave skull via jugular foramen and run to throat. Motor functions: innervate part of tongue and pharynx for swallowing and provide parasympathetic fibers to parotid salivary glands. Sensory functions: fibers conduct taste and general sensory impulses from pharynx and posterior tongue, and impulses from carotid chemoreceptors and baroreceptors.
X: Vagus nerves
Only cranial nerves that extend beyond head and neck region. Fibers from medulla exit skull via jugular foramen. Most motor fibers are parasympathetic fibers that help regulate activities of heart, lungs, and abdominal viscera. Sensory fibers carry impulses from thoracic and abdominal viscera, baroreceptors, chemoreceptors, and taste buds of posterior tongue and pharynx.
XI: Accessory nerves
Formed from ventral rootlets from C1 to C5 region of spinal cord (not brain). Rootlets pass into cranium via each foramen magnum. Accessory nerves exit skull via jugular foramina to innervate trapezius and sternocleidomastoid muscles. Formerly spinal accessory nerve.
XII: Hypoglossal nerves
Fibers from medulla exit skull via hypoglossal canal. Innervate extrinsic and intrinsic muscles of tongue that contribute to swallowing and speech.
Olfactory and optic nerves
Neuron cell bodies located within special sense organs.
Other nerves with sensory information
Neuron cell bodies located in cranial sensory ganglia.
Motor neuron cell bodies
Most motor neuron cell bodies are in ventral gray matter of the brain stem.
Autonomic motor neurons
Some autonomic motor neurons are located in ganglia.
Primary functions of cranial nerves
Remembered by the phrase: 'Some say marry money, but my brother believes (it's) bad business (to) marry money.'
Spinal nerves
31 pairs of spinal nerves that are all mixed nerves named for point of issue from spinal cord.
Cervical nerves
8 pairs of cervical nerves (C1-C8).
Thoracic nerves
12 pairs of thoracic nerves (T1-T12).
Lumbar nerves
5 pairs of lumbar nerves (L1-L5).
Sacral nerves
5 pairs of sacral nerves (S1-S5).
Coccygeal nerves
1 pair of tiny coccygeal nerves (C0).
Cervical spinal nerves exit
Each of the first 7 pairs (C1 to C7) exits the vertebral canal superior to the vertebra for which it is named.
Last spinal nerve (C8)
Exits canal inferior to C7.
Spinal nerve connections
Each spinal nerve is connected to the spinal cord via two roots: ventral roots and dorsal roots.
Ventral roots
Contain motor (efferent) fibers from ventral horn motor neurons that innervate skeletal muscles.
Dorsal roots
Contain sensory (afferent) fibers from sensory neurons in dorsal root ganglia that conduct impulses from peripheral receptors.
Spinal nerves emergence
Spinal nerves emerge from the vertebral column via their respective intervertebral foramina.
Spinal roots length
Spinal roots become progressively longer superiorly to inferiorly down the cord.
Cauda equina
Lumbar and sacral roots are very long and extend through the lower vertebral canal as cauda equina.
Spinal nerves length
Spinal nerves are quite short (~1-2 centimeters).
Branches of spinal nerves
Almost immediately after exiting foramen, spinal nerves divide into three branches: dorsal ramus, ventral ramus, and meningeal branch.
Rami communicantes
Contain autonomic nerve fibers that join ventral rami in the thoracic region.
Dorsal rami
Supply posterior body trunk.
Ventral rami
Supply the rest of the trunk and limbs.
Roots
Lie medial to and form spinal nerves; each root is purely sensory or motor.
Rami
Lie distal to and are lateral branches of spinal nerves; can carry both sensory and motor.
Nerve plexuses
Interlacing nerve networks formed by all ventral rami except T2-T12.
Cervical plexus
Formed by the first four ventral rami (C1-C4); most branches form cutaneous nerves.
Phrenic nerve
Major motor and sensory nerve of diaphragm, receives fibers from C3 to C5.
Irritation of the phrenic nerve
Causes spasms of the diaphragm, also called hiccups.
Severed phrenic nerves
If both are severed or if C3-C5 region of spinal cord is destroyed, diaphragm becomes paralyzed.
Respiratory arrest
Occurs when diaphragm is paralyzed; victim requires mechanical respirators to stay alive.
Brachial plexus
Formed by ventral rami of C5-C8 and T1 (and often C4 and/or T2); gives rise to nerves that innervate upper limb.
Roots of brachial plexus
Five ventral rami (C5-T1) unite to form trunks.
Trunks of brachial plexus
Upper, middle, and lower trunks unite to form divisions.
Divisions of brachial plexus
Anterior and posterior divisions unite to form cords.
Cords of brachial plexus
Lateral, medial, and posterior cords give rise to nerves of the upper limb.
Axillary nerve
Innervates deltoid, teres minor, and skin and joint capsule of shoulder.
Musculocutaneous nerve
Innervates biceps brachii, brachialis, coracobrachialis, and skin of lateral forearm.
Median nerve
Innervates skin, most flexors, forearm pronators, wrist and finger flexors, thumb opposition muscles.
Ulnar nerve
Supplies flexor carpi ulnaris, part of flexor digitorum profundus, most intrinsic hand muscles, skin of medial aspect of hand, wrist/finger flexion.
Radial nerve
Innervates essentially all extensor muscles, supinators, and posterior skin of limb.
Brachial plexus injury
Common injuries that can weaken or paralyze the entire upper limb, often occurring when the upper limb is pulled too hard.
Median nerve injury
Makes it difficult to use pincer grasp (opposed thumb and index finger) to pick up small objects, often seen in carpal tunnel syndrome.
Ulnar nerve vulnerability
Very vulnerable to injury; severe or chronic damage can lead to sensory loss, paralysis, and muscle atrophy.
Claw hand
Condition where little and ring fingers become hyperextended at the knuckles and flexed at distal interphalangeal joints due to ulnar nerve damage.
Funny bone
The spot where the ulnar nerve rests against the medial epicondyle, can cause tingling in the little finger when struck.
Radial nerve trauma
Results in wrist drop, an inability to extend the hand at the wrist.
Saturday night paralysis
Occurs when an intoxicated person falls asleep with an arm draped over a chair or sofa edge, cutting off blood supply to the radial nerve.
Lumbosacral plexus
Serves mostly the lower limb but also sends some branches to the abdomen, pelvis, and buttocks.
Lumbar plexus
Arises from L1 to L4; innervates thigh, abdominal wall, and psoas muscle.
Femoral nerve
Innervates quadriceps and skin of anterior thigh and medial surface of leg.
Obturator nerve
Passes through obturator foramen to innervate adductor muscles.
Sacral plexus
Arises from L4 to S4 and serves the buttock, lower limb, pelvic structures, and perineum.
Sciatic nerve
Longest and thickest nerve of body; innervates hamstring muscles, adductor magnus, and most muscles in leg and foot; composed of two nerves: tibial and common fibular.
Tibial nerve
Gives rise to sural nerve that serves parts of leg; at ankle, tibial nerve divides into medial and lateral planar nerves that serve the foot.
Common fibular nerve
Also known as common peroneal nerve; innervates knee joint, areas of skin of leg, and muscles of leg.
Superior gluteal nerve
Innervates buttocks and tensor fascia lata muscle.
Inferior gluteal nerve
Innervates buttocks and tensor fascia lata muscle.
Pudendal nerve
Innervates muscle and skin of perineum.
Sciatica
A common problem characterized by stabbing pain radiating over course of the sciatic nerve; injury could be caused by a fall, disc herniation, or badly placed injection into the buttock.
Footdrop
Condition where foot drops into plantar flexion due to inability to move foot and ankle.
Dermatome
Area of skin innervated by cutaneous branches of single spinal nerve; all spinal nerves except C1 participate in dermatomes.
Hilton's law
Any nerve serving a muscle that produces movement at a joint also innervates that joint and skin over that joint.
Anterolateral thorax and abdominal wall
Ventral rami of T12-T12 are intercostal nerves that supply muscles of ribs, anterolateral thorax, and abdominal wall.
Back innervation
Back is innervated by dorsal rami via several branches; each branch innervates a strip of muscle and skin in line with where it emerges from spinal cord.