Asthma 1-4, Environmental Aspects of COPD and Asthma, Cystic Fibrosis, COPD 1-2
1/77
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
78 Terms
What is asthma?
A chronic lung disease, characterised by excessive variation in both:
Expiratory lung function
Respiratory symptoms
Cough
Wheeze
Chest tightness
Breathlessness (dyspnoea)
Asthma diagnosis investigations
Spirometry (and FeNO - not compulsory): pre- and post-bronchodilator FEV1
History-taking of clinical signs and symptoms
Asthma diagnosis thresholds
Post-bronchodilator FEV1 increase >= 200 mL and >=12% from baseline .
FeNO greater than or equal to 40 ppb.
The 8 management points for Asthma + COPD
Action plan + pharmacological therapies
Smoking cessation
Manage co-morbidities
Immunisation
Diet
Exercise (+ Pulmonary Rehab)
Education + Inhaler Technique
Monitoring
Poor asthma control
Three or more of the following:
reliever needed 3 or more times a week
symptoms experienced 3 or more times a week
morning or nighttime symptoms present
any limitations on daily activities
Partial asthma control
One or two of the following:
reliever needed 3 or more times a week
symptoms experienced 3 or more times a week
morning or nighttime symptoms present
any limitations on daily activities
Good asthma control
reliever needed <2 times a week
symptoms experienced <2 times a week
no morning or nighttime symptoms
no limitations on daily activities
Factors associated with increased risk of life-threatening asthma (admission history)
1 or more ICU admissions
2 or more hospital admissions in the past year
3 or more ED admissions in the past year
Hospital admission in the last month.
Factors associated with increased risk of life-threatening asthma
High SABA use
Cardiovascular disease
Sensitivity to an unavoidable allergen
No Action Plan
History of sudden acute flareups or delayed hospital presentation
Admission history (ICU, hospital, ED + recent hospitalisation)
Factors associated with an increased risk of flare-ups
Other respiratory conditions
Smoking
Eosinophilic T-helper Cell Type II inflammation
Poor asthma control
Flare-ups in the last year
Difficulty noticing reduced airflow
Socio-economic disadvantage
Mental illness
Asthma exacerbation risk factors
Triggering medications
Poor adherence
Infection
Thunderstorm
Allergen triggers
Occupational sensitisers
1st step on the Asthma treatment ladder (adults)
Low dose
AIR , or
ICS + SABA

2nd step on the Asthma treatment ladder (adults)
Low dose
MART, or
ICS/LABA + SABA
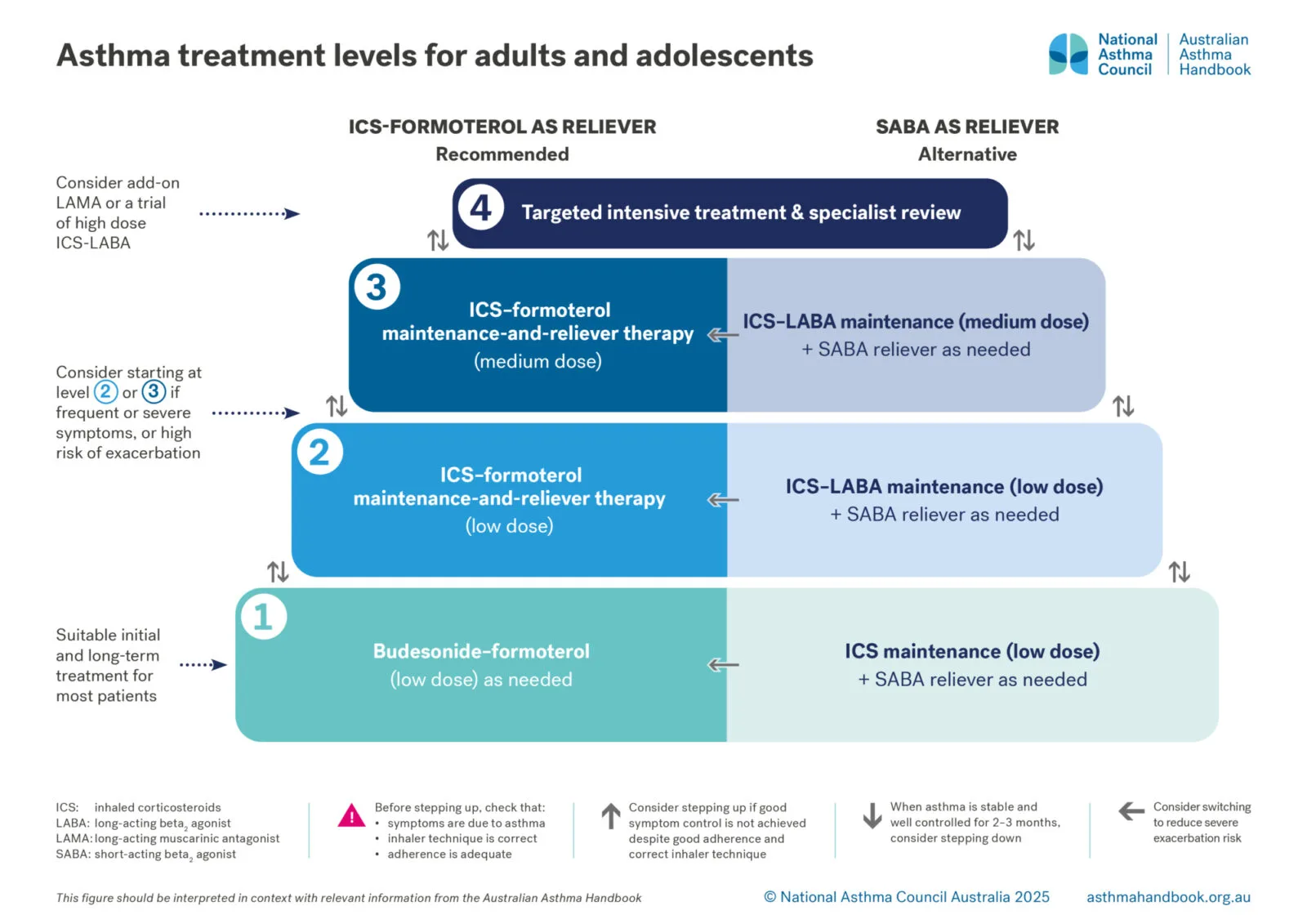
3rd step on the Asthma treatment ladder (adults)
Medium dose
MART, or
ICS/LABA + SABA
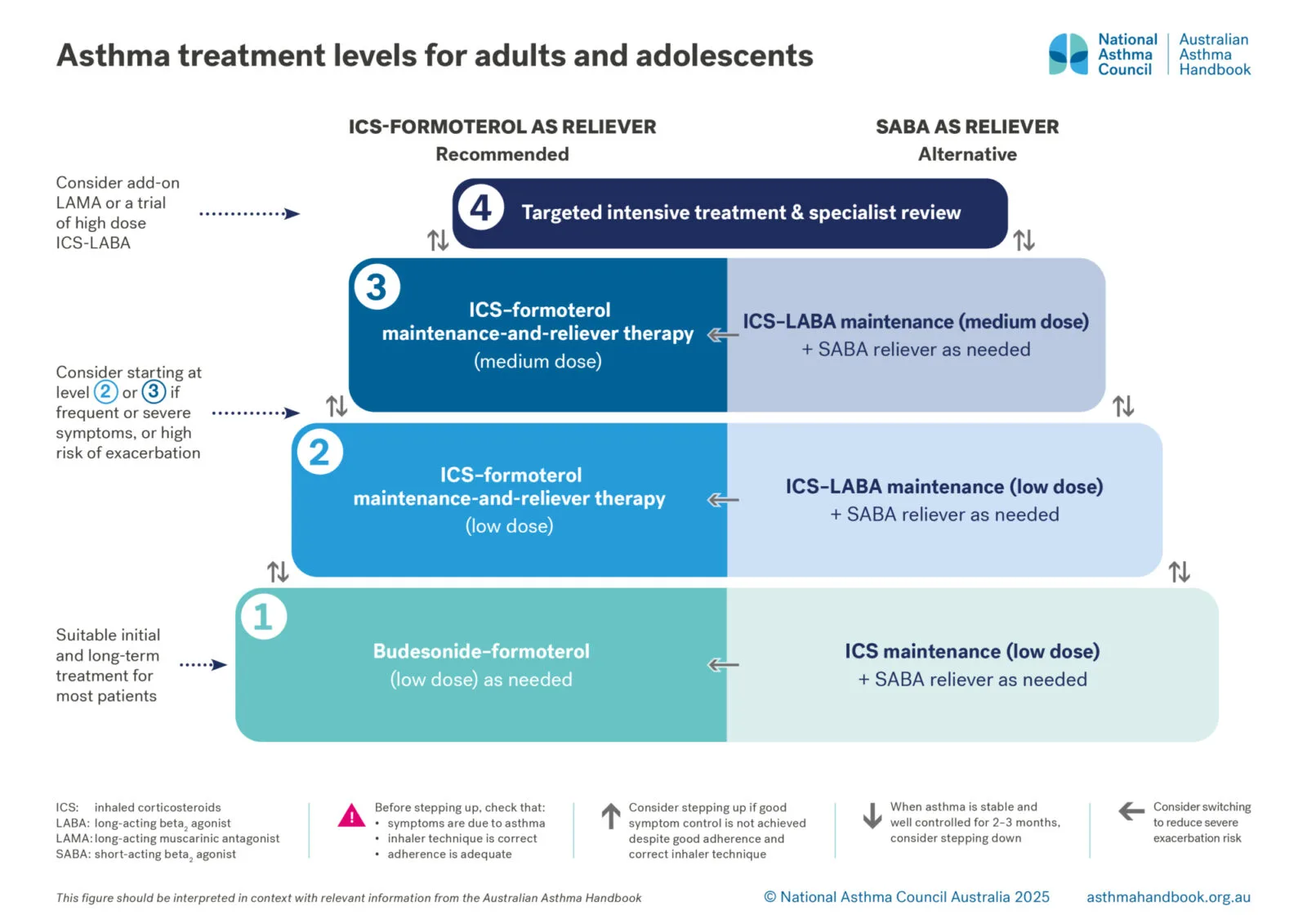
4th step on the Asthma treatment ladder (adults)
Specialist involvement with
High dose
ICS/LABA + SABA
LAMA add-on
Monoclonal antibody add-on

Most potent to least potent ICS
Fluticasone furoate (20 mcg)
Ciclesonide (80 mcg)
Beclometasone, fluticasone propionate (100 mcg)
Budesonide (200 mcg)
(equivalent amount to 100 mcg fluticasone propionate)
Alarmins released during asthma in response to airway epithelium damage
IL-25
IL-33
TSLP (thymic stromal lymphopoietin)
Cytokines released during asthma by T helper Type 2 cells
IL-4
IL-5
IL-13
These cytokines released by TH2 cells recruit and activate eosinophils, driving the inflammatory response
The steps in asthma pathophysiology
Airway epithelium disrupted
Alarmins released
Dendritic cells become antigen presenting cells carrying the allergen
Antigen presenting cells present the allergen antigens to naive T helper cells
T helper cells differentiate into T Helper type II cells
IL-4, IL-5, IL-13 is released by the TH2 cells
Eosinophils are recruited and inflammation occurs
Epithelium undergoes growth-factor-driven remodelling
More blood vessels and mucous, hypertrophy, narrow lumen
Asthma treatment in children 6-11 years
1st level: SABA
2nd level (most children):
ICS (low dose) + SABA or,
Montelukast + SABA
3rd level (starting level for severe sx or high risk of exacerbation):
ICS/LABA (low dose) + SABA or,
ICS (medium dose) + SABA
4th level:
ICS/LABA (medium dose) + SABA
5th level: Specialist involvement
Montelukast can be an add-on treatment at any level from level 2.
When to step down asthma treatment?
If patient is stable after 2-3 months and at low risk of exacerbation.
Before stepping up asthma treatment, check:
Adherence
Inhaler technique
Symptoms are due to asthma and not something else
When to step up asthma treatment?
If good symptom control is not achieved despite adherence and correct inhaler technique
Montelukast dosage
15 years-adult: 10 mg once a day
6-15 years: 5 mg once a day
<6 years: 4 mg once a day
Asthma treatment levels for children 1-5 years
1st level (when symptoms are mild or infrequent): SABA
2nd level (frequent or troublesome symptoms, or history of oral corticosteroid to treat an episode in the past):
ICS (low dose) + SABA or,
Montelukast + SABA
3rd level:
ICS (medium dose) + SABA
4th level: Specialist involvement
Montelukast can be an add-on treatment at any level from level 2.
No LABA for children under 5 years.
Salbutamol and terbutaline (SABA) adverse effects
tachycardia
headache
palpitations
tremor
hypokalaemia, hyperglycemia (high doses)
Which LAMA-only formulation is approved in asthma (and what are the requirements)?
Spiriva Respimat Tiotropium 2.5 mcg
severe asthma not controlled with optimised treatment, inhaler technique and adherence.
at least one severe exacerbation requiring oral corticosteroids in the last 12 months
must be used in combination with an ICS/LABA treatment (unless LABA is contraindicated)
Which triple therapy formulations are approved in asthma (and what are the requirements)?
Trelegy (fluticasone furoate/vilanterol/umeclidinium)
Trimbow (beclometasone/formoterol/glycopyrronium)
Enerzair (mometasone/indacaterol/glycopyrronium)
Requirements for asthma:
18 year old+ (adults only)
severe asthma not controlled with optimised treatment, inhaler technique and adherence.
at least one severe exacerbation requiring oral corticosteroids in the last 12 months
LAMA adverse effects
Dry mouth
Throat irritation
Blurred vision
Dizziness
Urinary retention
Rarely: constipation, acute angle-closure crisis, palpitations, anaphylaxis/allergy
Which triple therapy is only indicated in COPD (and not asthma)?
Breztri (budesonide/glycopyrronium/formoterol)
Inhaled corticosteroid (ICS) side effects
Pneumonia in COPD patients
Dysphonia (hoarseness)
Oral thrush
Low bone mineral density (osteoporosis)
Cataracts or Glaucoma (high doses)
Skin thinning and bruising (high doses, elderly)
Diabetes
In children:
Adrenal insufficiency in high doses with dual use of intranasal and inhaled corticosteroids
Growth suppression by 1.2 cm
How to step down asthma ICS therapy?
Small, gradual dose adjustments by 25-50% at 2-3 month intervals
Oral corticosteroid dosage for acute/emergency asthma flare-up
Prednisone or Prednisolone 0.5-1 mg/kg for 3-5 days or shortest time possible
Montelukast (Leukotriene receptor antagonist) side effects
Headache
Abdominal pain
Diarrhoea
Mood changes, sleeping issues
Eosinophilic granulomatosis with polyangiitis (EGPA) (Churg Strauss syndrome)
When can macrolides be used in asthma?
Low dose azithromycin can be used in severe asthma under specialist supervision for neutrophilic phenotypes.
Medications that exacerbate asthma
NSAIDs and Aspirin
Beta-blockers (“-lol”)
Opioids
Asthma flare-up triggers
Medications
Viral or bacterial infection
Allergen exposure
Occupational sensitisers
Stress
Poor adherence
Thunderstorms (for those with allergic rhinitis sensitised to rye grass)
Severity levels of an asthma flare up and hospital management
Mild/Moderate: Can walk and speak whole sentences in one breath. 4-12 puffs salbutamol with spacer
Severe: Accessory muscle use, can’t speak full sentences, oxygen saturation 90-94%. 12 puffs salbutamol with spacer. Ipratropium 8 puffs with spacer. Start oxygen if required.
Life-threatening: Drowsiness or collapse, exhaustion, cyanosis, oxygen saturation <90%, poor respiratory effort. Salbutamol + ipratropium continuous nebulisation, start oxygen, ventilate if required.
If poor response (for any level of severity), add IV Magnesium Sulfate.
Within the first hour, start systemic corticosteroids
Asthma first aid
Salbutamol 4 puffs every 4 minutes, 4 breaths per puff
Worse or no better: call 000 and continue first aid.
Struggling still? Give 4 more puffs. Still struggling? Then call 000 and first aid.
Repeat doses every 20 minutes (or sooner if needed) for the first hour: 3 doses in an hour
Magnesium sulfate in acute asthma contraindications
Heart-block,
Myasthenia gravis
Elderly using nifedipine
Existing hypermagnesaemia
What is exercise induced bronchoconstriction?
Acute airway narrowing that can occur as a result of exercise. Can occur in individuals with and without asthma.
Exercise-induced bronchoconstriction management
Warm ups and cool downs
avoiding exercise in an at-risk air environment (cold, dry, pollutants or allergens present)
Asthma medications in competitive sport
All beta-2 agonists are prohibited (Therapeutic Use Exemption (TUE) required) with exceptions for some inhaled formulations (salbutamol, salmeterol, formoterol, vilanterol) within limits
Salbutamol limits in competitive sport
Up to:
16 puffs (1600 mcg) in 24 hours
6 puffs in 8 hours
Salmeterol limit in sport
Up to 200 mcg in 24 hours
Formoterol limit in sports
Up to 54 mcg in 24 hours
Vilanterol limit in sport
Up to 25 mcg in 24 hours
Corticosteroid use in sports
Inhaled corticosteroids (asthma) allowed
Intranasal corticosteroids (allergic rhinitis) allowed
Oral or IV corticosteroids prohibited during competition
Main reasons for the impact of climate change on respiratory health
Particulate matter below 2.5 microns (PM2.5) diameter
Ozone O3 increasing from greenhouse gas emissions
Aeroallergen and pollen counts increasing with El nino activity and climate changes
These are resulting in more emergency admissions
Natural phenomena that impact asthma/COPD exacerbations
Bushfires (increase fine particle matter PM2.5)
Heatwaves (hyperventilation + bronchoconstriction + inflammation)
Thunderstorms (increase fine particle matter PM2.5)
Flood (increase fine particle matter PM2.5)
Earthquake (increase fine particle matter PM2.5)
How heatwaves affect asthma
Hyperventilation
Increase allergens and moulds
Heat shock proteins
Pulmonary C-type nerve fibres TRPs activity and cholinergic reflex (bronchoconstriction) and cytokine production
Greenhouse gases
Carbon dioxide
Methane
Nitrous oxide
Fluorinated gases (F-gases)
CO2 gas equivalent and GWP
The Global Warming Potential of a greenhouse gas, expressed in tonnes of CO2 that it is equivalent to (tCO2 -e)
Most common inhaler propellant in pMDIs
Hydrofluorocarbon (HFC)
Top 5 common detected pharmaceuticals in aquatic life in Australia
Memantine
Codeine
Fluconazole
Clotrimazole
Mianserin
Healthcare contribution to the climate footprint
20% (one-fifth)
The role of pharmacists in sustainable healthcare
Reduce carbon emissions
Green chemistry examples
CFC-containing inhalers deteriorate ozone
PFAS chemicals can cause exacerbations
Aspirin induced asthma flare ups mechanism
Inhibiting COX results in upregulation of LOX, which leads to synthesis of leukotrienes that are associated with bronchoconstriction and airway inflammation.
What is cystic fibrosis?
The autosomal recessive disorder caused by mutations in the Cystic Fibrosis Transmembrane conductance Receptor (CFTR), which is an ABC transporter protein for chloride ions.
Less chloride ions are secreted, so less water is drawn into the extracellular space, so extracellular space is filled with thick, viscous, clogging mucous.
What is the most common CFTR gene mutation that causes cystic fibrosis?
DELTA 508
Folding of the CFTR is delayed, and so the cell treats it as defective and sends it to the proteasome for degradation: so a much smaller proportion of CFTR survives to be functional.
The other mutation that is common: G551D, where there is a gating defect so ATP won’t open the receptor.
Cystic fibrosis treatments
CFTR modulators
Antibiotics for infections
Inhaled Corticosteroids for lung function
Inhaled Mucolytics (dornase alpha, saline, mannitol)
CFTR modulators in cystic fibrosis
Ivacaftor (allosteric modulator “potentiator” that keeps CFTR open even without ATP)
Deutivacaftor
Lumacaftor
Tezacaftor
Elexacaftor
Vanzacaftor
Once daily dosing Cystic Fibrosis triple therapy
Deutivacaftor + Tezacaftor + Vanzacaftor
Current triple therapy available for Cystic Fibrosis
Ivacaftor + Tezacaftor + Elexacaftor
Ivacaftor keeps receptor open
Tezacaftor stabilises TMD1 binding site
Elexacaftor enhances the effect of Tezacaftor
What is COPD?
Chronic, lung disease where air flow limitation is not fully reversible with bronchodilators
Post-bronchodilator FEV1/FVC less than 0.7
COPD diagnosis investigations
Spirometry: pre- and post-bronchodilator FEV1
History-taking of clinical signs and symptoms
Levels in COPD management
SABA or SAMA prn
Add LAMA or LABA or both
Add ICS
Consider triple therapy LAMA/LABA/ICS only if LABA/LAMA or ICS/LABA isn’t working, and in the past 12 months:
Hospitalisation(s) for exacerbations, or
At least 2 moderate exacerbations
What is COPD triple therapy
LAMA/LABA/ICS
What is COPD triple therapy requirement?
When LABA/LAMA or ICS/LABA isn’t working, and in the past 12 months:
Hospitalisation(s) for exacerbations, or
At least 2 moderate exacerbations
COPD lung pathology
Emphysema
Obstructive bronchiolitis
Mucous hypersecretion
COPD Severity Scales - Mild COPD
Few symptoms, cough and sputum
Breathless on moderate exertion
Predicted 60-80% FEV1
COPD Severity Scales - Moderate COPD
Breathless while walking
Limitation on activities
Chest infections
Exacerbations require antibiotics or oral corticosteroids
Predicted 40-59% FEV1
COPD Severity Scales - Severe COPD
LESS THAN 40% predicted FEV1
Which COPD medication is most common for daily control?
LAMAs
Tiotropium
Glycopyrronium
Umeclidinium
Aclidinium
They have a better effect on exacerbation frequency and reduced side effects compared to LABAs in COPD.
However, dual LAMA/LABA is superior to either alone.
What can indacaterol + glycopyrronium + mometasone triple therapy be used for?
Severe asthma only.
Not approved for COPD.
When to review COPD
Every 6 weeks
Mucolytics for COPD
N-acetylcysteine (NAC)
ambroxol
sobrerol
carbocysteine
letocteine
cithiolone
iodinated glycerol
N-isobutyrylcysteine (NIC)
myrtol
erdosteine