Autonomic Nervous System
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
Visceral nervous system
The visceral nervous system functions to maintain homeostasis within the body by
controlling the functions of the internal organs, blood vessels, & certain structures in the
skin. It has both sensory and motor components
Viscerosensory neurons
carry sensory information from the internal organs and this
information is processed and used predominantly without reaching conscious awareness.
Sympathetic division of ANS
carries information from nociceptors located in heart, respiratory
structures, and gastrointestinal and urogenital tracts. This information is used to
mediate reflexes at the level of the spinal cord and it is conveyed to brain regions via
the ALS
parasympathetic division of ANS
carries information from physiological receptors that convey
innocuous stimuli and monitor the functions of visceral structures (mediation of
reflexes will be most important) and this information is carried on cranial nerves and
processed by the solitary nucleus or on pelvic nerves and processed at the level of the
spinal cord and conveyed to brain regions via the ALS.
referred pain
visceral pain is generally poorly localized and often referred to as somatic body part
Sympathetic viscerosensory neurons travel with spinal
nerves & upon entering the spinal cord they send
collaterals that synapse on posterior horn cells that
receive primarily somatosensory input; the cortex
interprets the pain as coming from the body surface
rather than the viscera.
referred pain examples
• Examples: pain associated with:
• heart disease = referred to the chest wall or
arm
• gallbladder disease = referred to the back or
between the scapulae
• pancreatic disease = referred to the back
True or false? The sympathetic division of the viscerosensory system conveys innocuous information from the viscera.
This statement is false: the sympathetic division of the viscerosensory system conveys pain information and the parasympathetic division conveys innocuous sensory information (e.g., stretch/tension in hollow organs contributing to the sense of fullness; blood composition).
True or false? Visceral pain is poorly localized and often referred to along a dermatome of the somatic nervous system secondary to "cross talk" between the visceral and somatic sensory systems.
This statement is true: visceral pain is poorly localized because of low receptor density and the large receptive fields of viscerosensory neurons, and because there is a small area of the cortex processing visceral sensory information (in comparison to somatosensory information). Sympathetic viscerosensory neurons travel in spinal nerves and often contact somatic dorsal horn cells. This "cross talk" results in visceral pain being interpreted as coming from the dermatome supplied by that spinal cord segment.
viseromotor neurons
control smooth muscle, cardiac muscle, and secretory glands, and these components are often referred to as the autonomic nervous system
innervation of structures of head and body
innervation of structures of the head and body require dual innervation from parasympathetic and sympathetic divisions
innervation of structures of the body wall and limbs
body wall and limbs (blood vessels supplying skeletal muscles and skin, sweat glands, and the arrestor pili muscles)
regulated but he sympathetic system
communication of the autonomic nervous system
communication involves two neurons
preganglionic neurons: has its cell body in either the brainstem or spinal cord; axons of these neurons will project to an autonomic ganglion
postganglionic neuron: has its cell body in the autonomic ganglion; axons of these neurons will project to visceral targets (e.g. smooth muscle cells, cardiac muscle cells)
sympathic division of the ANS
preganglionic cells: origina ein the intermediolateral cell column (T1-L2)
post-ganglionic neurons are located in the sympathetic chain of ganglia or pre vertebral ganglia (near abdonomial/pelvic arteries)
neurotransmitters: acetylcholine and norepinephrine (post-ganglionic)
parasympathetic division of the ANS
preganglionic neurons: cranial visceromotor nuclei (cranial outflow) and S2-S4 (sacral outflow) spinal segments
post-ganglionic neurons are located in ganglia in the head region and intramural ganglia (near organs)
neurotransmitters: acetylcholine
structural comparisons of sympathetic and parasympathetic divisions
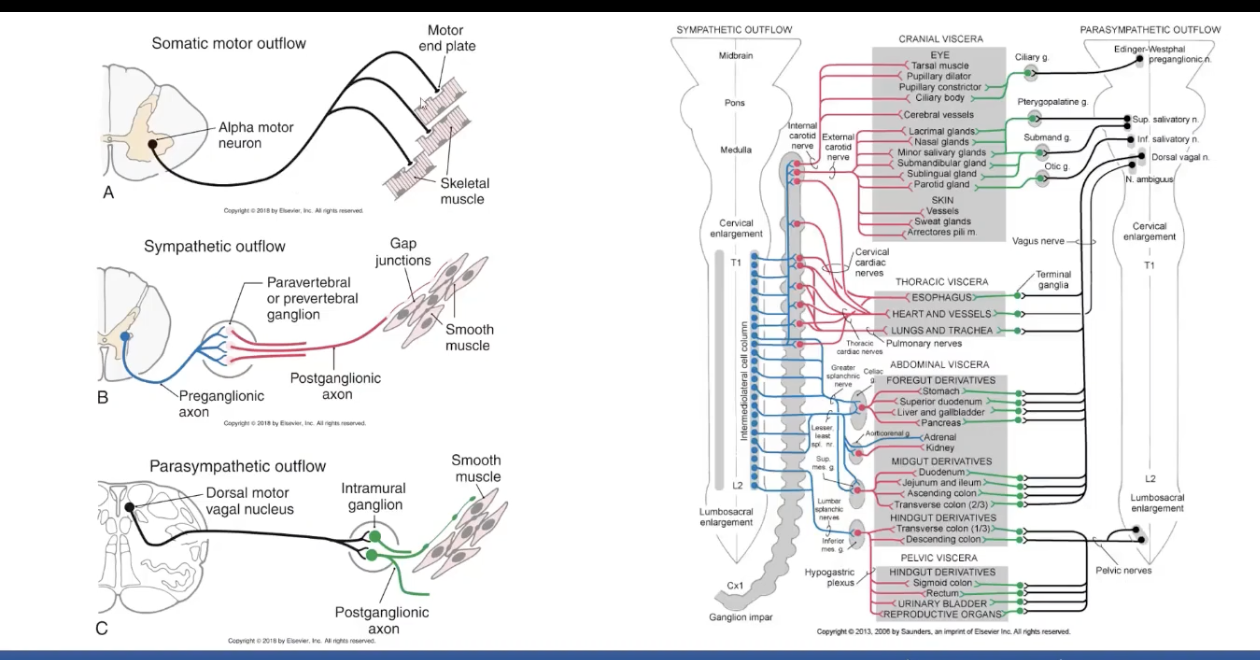
Functional Comparison of Divisions: sympathetic
increases heart rate, blood pressure, blood flow to skeletal muscle and blood glucose levels
decreases gut motility, digestive glandular secretion, and blood flow to the viscera and skin
pupil and bronchiole dilation, sweating, and piloerection
functional comparison of divisions: parasympathetic
decreases heart rate
increases digestive glandular secretion, blood flow to the gut and motility of the gut
pupil and bronchiole constriction and accommodation of the lens of the eye
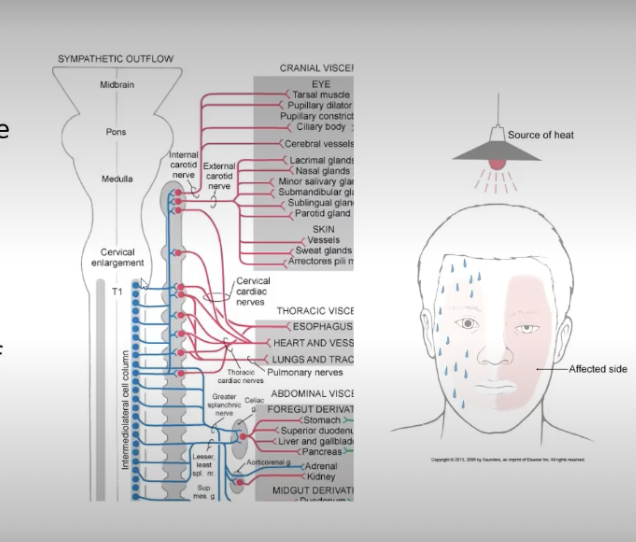
Horner Syndrome
interruption of the pathway through the superior cervical ganglion results in Horner syndrome
favor of sympathetic control?
miosis: constriction of the pupil
ptosis: drooping of the upper eye lid
flushing of the face
anhidrosis: diminished or absence of sweating
Central Control of ANS
visceromotor pathways operate locally at the level of the spinal cord and brainstem (aka reflexes) and are influenced by a variety of “higher centers” collectively called the Central Autonomic Network
spinal cord and brainstem (medulla plays key role) reflexes are important for short term regulation of the autonomic nervous system (e.g., regulation of heart rate and blood pressure during changes in body position)
higher centers are involved in regulation of more complex responses (e.g., elevated heart rate and blood pressure related to anxiety or anticipation of pain)
Central control of ANS: hypothalamus
nuclei of the hypothalamus: considered the highest integrator of autonomic and endocrine functions
reciprocal connections with limbic system
reciprocal connections with the solitary nucleus
project directly to preganglionic neurons in the dorsal motor vagal nucleus, to neurons in the anterolateral medulla, and the intermoediolateral cell column of the spinal cord
DMVN: parasympathetic outflow
IMLCC: sympathetic outflow
The blood vessels of the skin and skeletal muscles of the body wall and limbs are innervated by only the sympathetic division of the ANS.
This statement is true: Innervation of structures of the body wall and limbs (i.e., blood vessels supplying skeletal muscles and skin, sweat glands, and the arrector pili muscles) are regulated by the sympathetic system only; smooth muscle, cardiac muscles and glands of the head and body receive dual innervation from both divisions that produce opposing results.
Which of the following statements correctly describes the structural components of the parasympathetic division of the ANS? Select all that apply.
The preganglionic neurons of the parasympathetic division are found in the cranial visceromotor nuclei (cranial outflow) & S2 – S4 (sacral outflow) spinal segments. The post-ganglionic neurons are located in ganglia in the head region and intramural ganglia (near organs), an the neurotransmitter that allows communication to take place between the neurons and between the neuron and the target tissue is acetylcholine. The preganglionic neurons of the sympathetic division originate in the intermediolateral cell column (T1-L2) and the post-ganglionic neurons are located in the sympathetic chain of ganglia or prevertebral ganglia (near abdominal/pelvic arteries). Acetylcholine is the neurotransmitter that allows communication between the neurons and norepinephrine is the transmitter that allows communication between the post-ganglionic cell and the target tissue.
Your patient sustained a neck injury that damaged the right superior cervical ganglion. You anticipate seeing which of the following clinical signs. Select all that apply.
Damage to the right superior cervical ganglion reduces sympthateic outflow to the structures of the head/face: this will result in an ipsilateral Horner syndrome: right pupillary constriction (unopposed parasympathetic outflow), right ptosis (weak/paralyzed superior tarsal muscle); right facial flushing (loss of vascular tone); and absence of sweating on the right side (loss of innervation of sweat glands).
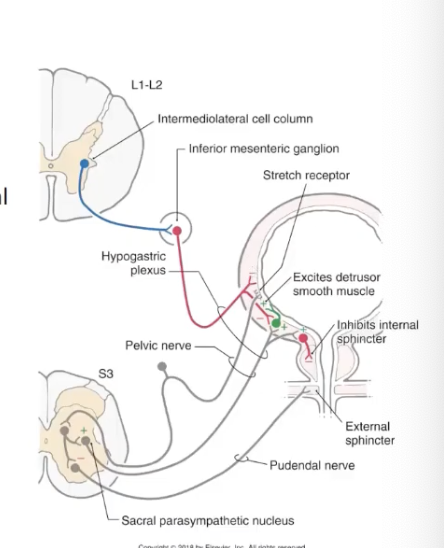
micturition reflex
urinary bladder emptying
contraction of smooth muscle of the bladder wall (detrusor muscle) - mediated by parasympathetic outflow
bladder was also has sympathetic innervation which is inhibitory to the detrusor muscles dn the post-ganglionic parasympathetic neurons in the bladder wall
relaxation of smooth muscle in the internal urethral sphincter - mediated by parasympathetic outflow
relaxation of the skeletal muscle of the external urethral sphincter - mediated by somatic motor system (S3-S4 - pudendal nerve)
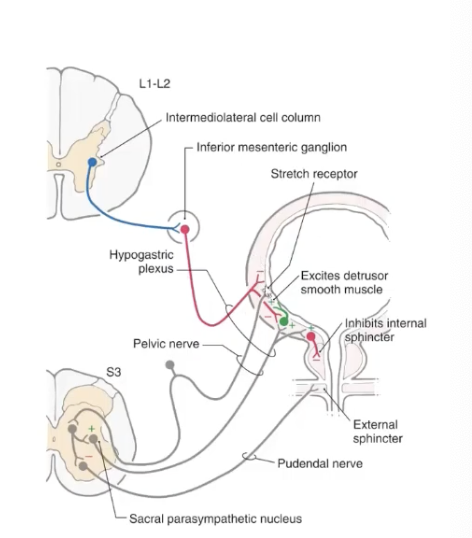
micturition reflex: neural control
during periods of urine storage there are low levels of activity in afferent neurons of the bladder wall resulting in
decreased parasympathetic outflow and tonic activity in sympathetic neurons causes relaxation of detrusor muscle and contraction of internal urethral sphincter
tonic activity of alpha motor neurons causes contraction of external urethral sphincter
as bladder fills, tension on bladder wall causes increased firing of afferents until they reach a threshold level (full bladder) inducing micturition via brainstem and spinal level reflexes that result in
decreased sympathetic outflow
increased parasympathetic outflow
inhibition of somatic motor neurons
main coordinating center is located in the pons and frontal lobes exert voluntary control
True or false? In order to empty the bladder there needs to be contraction of the smooth muscle of the bladder wall (detrusor muscle), relaxation of the internal urethral sphincter, and contraction of the external urethral sphincter.
This statement is false: While it is true that in order to empty the bladder contraction of the detrusor muscle and relaxation of the internal urethral sphincter are needed. The external sphincter must RELAX not CONTRACT.
Which of the following statements best describes the micturition reflex?
Decreased firing rate of the sensory afferents of the bladder wall results in increased parasympathetic outflow, increased sympathetic outflow, and inhibition of the somatic motor neurons resulting in bladder voiding.
Increased firing rate of the sensory afferents of the bladder wall results in increased parasympathetic outflow, decreased sympathetic outflow, and inhibiton of the somatic motor neurons resulting in bladder voiding.check
Increased firing rate of the sensory afferents of the bladder wall results in decreased parasympathetic outflow, increased sympathetic outflow and inhibition of the somatic motor neurons resulting in bladder voiding.
Decreased firing rate of the sensory afferents of the bladder wall results in decreased parasympathetic outflow, decreased sympathetic outflow and excitation of the somatic motor neurons resulting in bladder voiding.
b. When tension on the bladder wall reaches a threshold (full bladder), the sensory afferents increase their firing rate resulting in increased parasympathetic outflow and decreased sympathetic outflow resulting in the contraction of the detrusor muscle and relaxation of the internal sphincter. The sensory afferents also inhibit the somatic motor neurons that are mediating contraction of the external sphincter (results in relaxation of the skeletal muscle and opening of the sphincter).
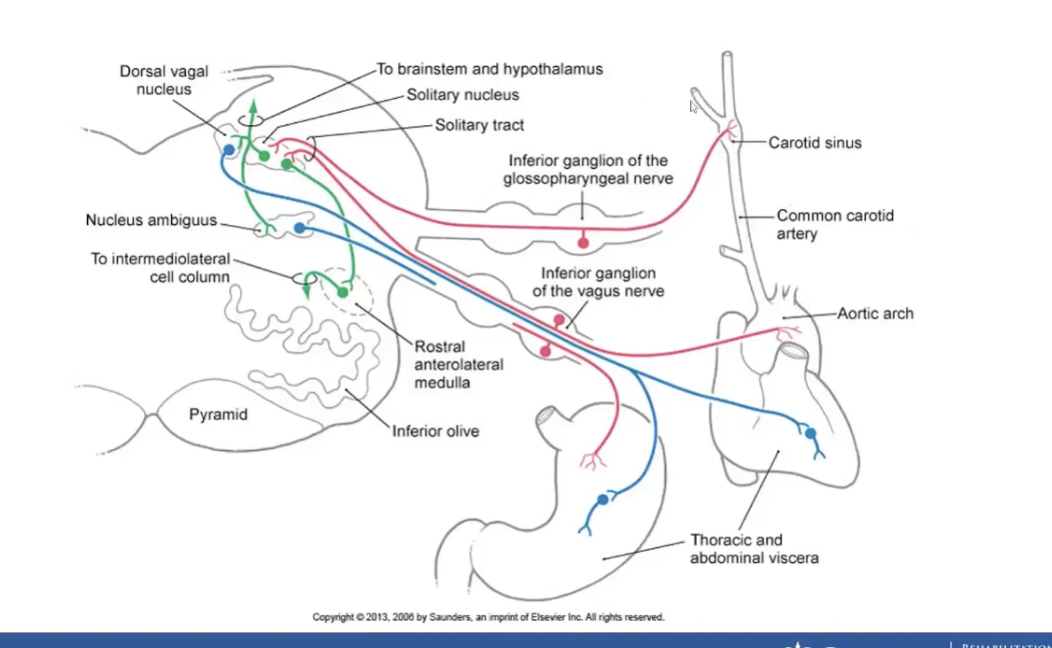
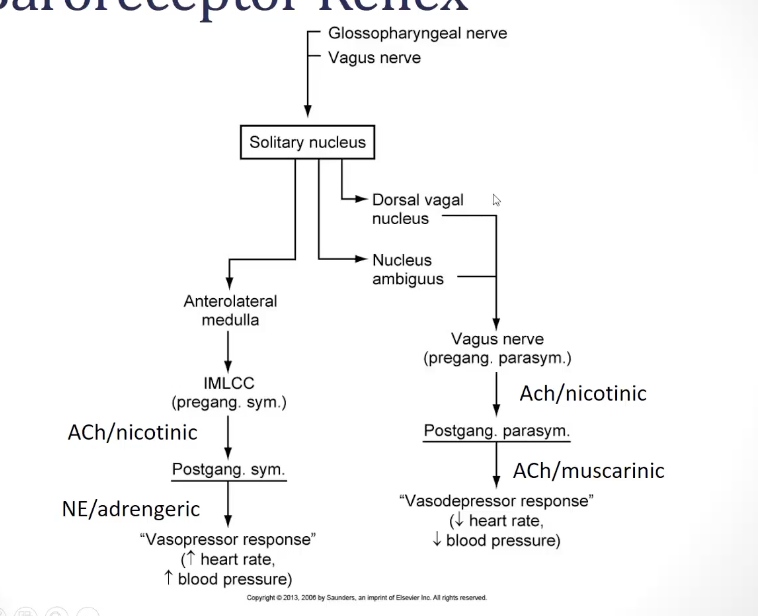
Baroreceptor reflex
baroreceptors located in the carotid sinus and aortic arch will detect changes in the tension of corresponding vessels
increased tension of these vessels will increase the firing rate of the baroreceptors: this is caused by an increase in blood pressure
decreased tension of these vessels will decrease the firing rate of the baroreceptors: this is caused by a decrease in blood pressure
afferent input from the carotid and aortic baroreceptors enters the medulla on CN IX and X
these afferents terminate on 2nd order neurons in the solitary nucleus which project to:
dorsal motor vagal nucleus: parasympathetic - vasodepressor cells
anterolateral medulla: sympathetic - vasopressor cells
output of the solitary nucleus
inhibitory to the vasopressor cells of the anterolateral medulla causing a decrease in sympathetic outflow
excitatory to the vasodepressor cells of the dorsal motor vagal nucleus causing an increase in parasympathetic outflow
output of the solitary nucleus
inhibitory to the vasopressor cells of the anterolateral medulla causing a decrease in sympathetic outflow
excitatory to the vasodepressor cells of the dorsal motor vagal nucleus causing an increase in parasympathetic outflow
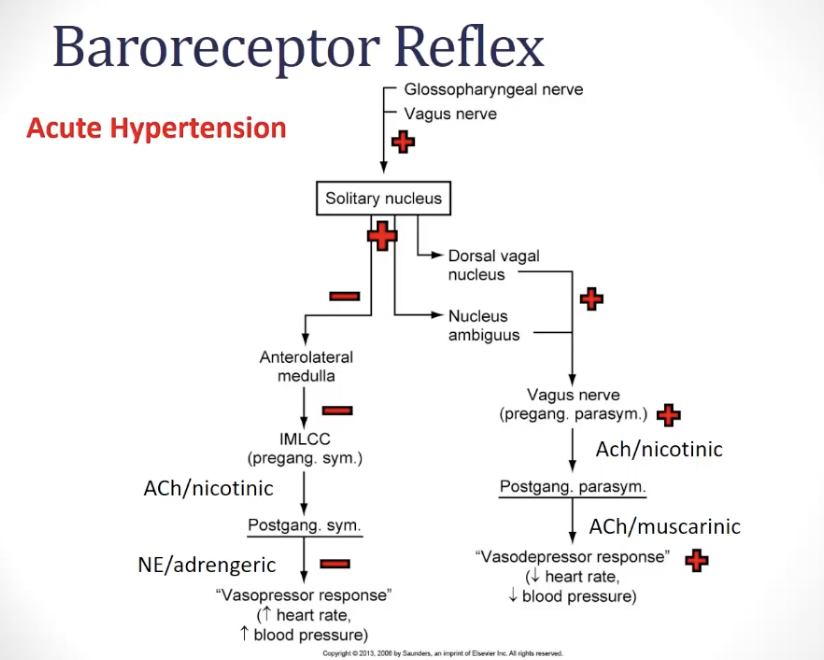
baroreceptor reflex: acute hypertension
baroreceptors increase firing rate
solitary nucleus increases output
excitatory to DMVN = increases parasympathetic outflow
inhibitory to rostral anterolateral medulla = decreases sympathetic outflow
end result: vasodepressor response = decreased heart rate and blood pressurea
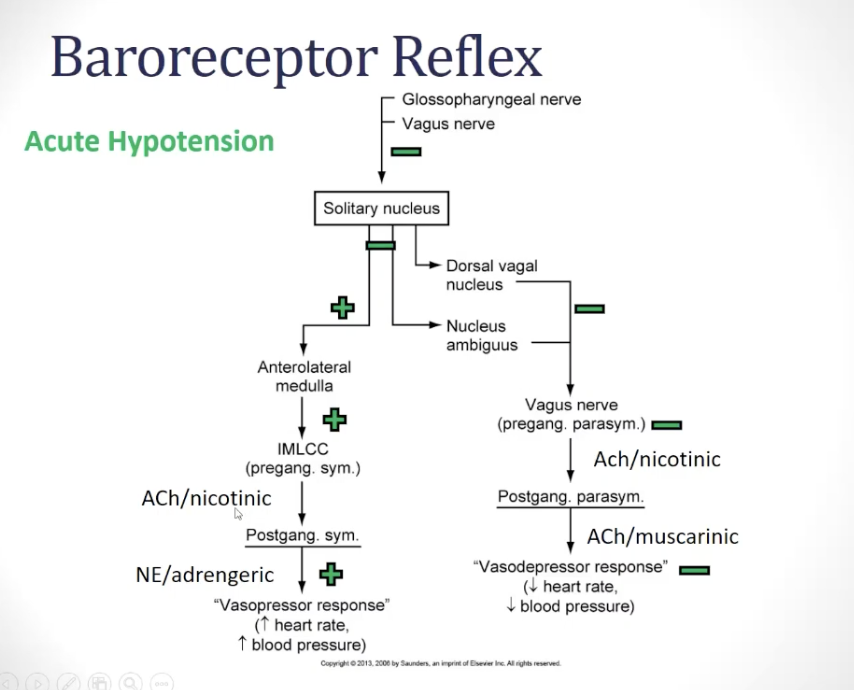
baroreceptor reflex: acute hypotension
baroreceptors decrease their firing rate
solitary nucleus decreases its output
reduction in excitation of DMVN = decreases parasympathetic outlfow
disinhibits rostral anterolateral medulla = increases symmpathetic outflow
end result = vasopressor response = increased heart rate and blood pressure
orthostatic hypotension
during a sudden change in posture if the baroreceptor reflex is not working properly, the result will be a severe drop in blood pressure
baroreceptor reflex
T/F? Baroreceptors are located in the carotid sinus and the arotic arch and increased tension in the walls of these arteries causes a reduction in the firing rate of these receptors.
This statement is false: While baroreceptors are located in the carotid sinus and aortic arch, increased tension in these vessels will INCREASE not DECREASE their firing rate.
Which of the following statements correctly describes what will happen during an acute episode of hypertension?
Baroreceptors will decrease their firing rate resulting in an increase in parasympathetic outflow and a decrease in sympathetic outflow producing the vasodepressor response.close
Baroreceptors will increase their firing rate resulting in an increase in parasympathetic outflow and a decrease in sympathetic outflow producing the vasodepressor response.check
Baroreceptors will decrease their firing rate resulting in an decrease in parasympathetic outflow and an increase in sympathetic outflow producing the vasopressor response.
Baroreceptors will increase their firing rate resulting in an decrease in parasympathetic outflow and a increase in sympathetic outflow producing the vasopressor response.
b. During an episode of acute hypertension, baroreceptors will increase their firing rate resulting in an increase in parasympathetic outflow and a decrease in sympathetic outflow producing the vasodepressor response (lowering of heart rate and blood pressure). During an episode of acute hypotension, baroreceptors will decrease their firing rate resulting in a decrease in parasympathetic outflow and an increase in sympathetic outflow producing the vasopressor response (increase in heart rate and blood pressure).
autonomic dysreflexia
life-threatening medical emergency that can develop in individuals with SCI at or above T6 level ; acute, uncontrolled hypertension
caused by an imbalance between parasympathetic and sympathetic outflow in control of blood pressure
typically, a noxious stimuli below the level o injury will initiate a peripheral sympathetic response through spinal reflexes (vasopressor response - causing vasoconstriction below the level of injury), resulting in peripheral arterial hypertension
baroreceptors detect this rise in BP and they increase firing rate the solitary nucleus; sends inhibitory input to the anterolateral medulla and excitatory input to the dorsal motor vaga l nucleus
parasympathetic response causes reduction in HR (bradycardia) but inhibitory impulse being sent to cord cant reach target below the level of the injury, resulting in parasympathetic response above the injury and a sympathetic response below the injury
imbalance results in uncontrolled hypertension removal of noxious stimuli is key to restoring balance