PARASITOLOGY (PROTOZOAN)
1/13
Earn XP
Description and Tags
HAYS PLS PAPASARA KO
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
14 Terms

Entamoeba histolytica
Pseudopod-forming non flagellated protozoan
Most invasive
The only one causes ccolitis and liver abscessin humans, leading to amoebic dysentery.
Life cycle: INFECTIVE CYST and INVASIVE TROPHOZOITE
HUMAN is the only host
Quadrinucleated cyst is resistant to gastric acidity and desiccation and can survive in moist environment.
Infection occurs when cyst is ingested from fecal contaminated material.
MOT: FECAL ORAL ROUTE
Other MOT: VENEREAL TRANSMISSION & DIRECT COLONIC INOCULATION
TROPHOZOITE:
size: 12um-60um
karyosome: small and central “bulls eye”
cytoplamic inclusion: RBC
multiply via binary fission
has the ability to colonize/invade large bowels
CYST
size: 10um-20um
cytoplamic inclusion: chromatid bars (cigar-shape), glycogen mass (food reserve)
no. of nuclei: 1-4
DIAGNOSIS
Microscopic detection of trophozoite and cyst in stool.
3 stool specimen will be examined on different days
Fresh stool must be examined within 30 mins to detect trophozoite via DFS
METHYLENE BLUE to diffentiate with WBC
E.histolytica trophozoite with ingested RBC is diagnostic of AMEBIASIS.
Concentration method: FECT and MIFC are more sensitive than DFS (size of cyst, number of nuclei, location and appearance of the karyosome, the characteristic appearance of chromatoid bodies and presence of cytoplasmic structures like glycogen vacoule).
STOOL CULTURE: Robinson’s medium
TREATMENT
TREATMENT OF AMEBIASIS:
a.) cure invasive disease both intestinal and extraintestinal sites.
b.) eliminate the passage of cysts from intestinal lumen
METRONIDAZOLE - drug of choice for invasive amebiasis
DILOXANIDE FUROATE - for asymptomatic cyst passer
PERCUTANEOUS DRAINAGE - liver abscess.

Entamoeba moshkovskii
Free living organism
First found in sewege
Able to grow at room temperature (25-30C)
Osmotolerant (0-41C)
Morphologically indistinguishable with E.histolytica and E.dispar
Cyst size: 10um - 20um
No. of cyst nuclei: 1-4
Cytoplasmic inclusion of cyst: chromatid bars, glycogen mass
Trophozoite size: 12um-60um
Trophozoite karyosome: small, centrally located
Trophozoite cytoplamic inclusion: ingested bacteria, no RBC
MOT: Fecal-Oral
Host: Commensal organism
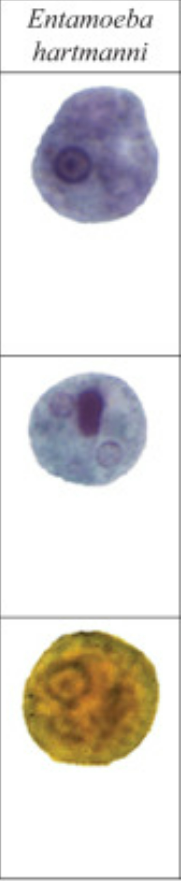
Entamoeba harmanni (trophozoite sa taas, ubos ang cyst)
similar to E.histolytica but smaller (3um-12um)
does not ingest RBC
Size of cyst: 4um-10um (mature)
No. of cyst nuclei: 1-4
Cytoplamic inclusions of cyst: Chromatoid bars (rod-shaped w/ rounded/square ends), diffuse glycogen mass
Size of trophozoite: 3um-12um
Trophozoite karyosome: small, centrally or eccentrically
Cytoplasmic inclusion of trophozoite: Ingested bacteria, no RBC
MOT: Fecal-Oral
Host: Commensal organism
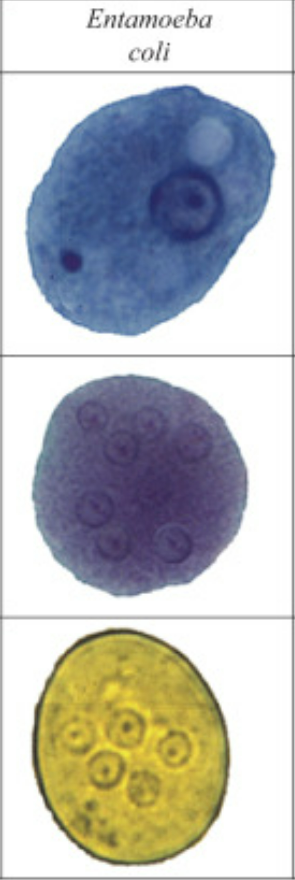
Entamoeba coli
More common than any other human amoebae
Motility of trophozoite is sluggish
Can be differentiated by E.histolytica by:
a.) more vacuolated or granular endoplasm w/bacteria and debris, no RBC
b.) narrower, less differentiated ectoplasm
c.) broader and blunter pseudopodia used more for feeding rather locomotion
d.) more sluggish, unidirected movements
Cyst size: 10um-35um
No. of cyst nuclei: 1-8
Cytoplasmic inclusion of cyst: thin chromatid bars (splintered/pointed ends)
Size of trophozoite: 15um-50um
Trophozoite karyosome: Large and irregular, eccentrically located
Cytoplamic inclusion of trophozoite: vacuoles w/bacteria
MOT: Fecal-Oral
Host: Human
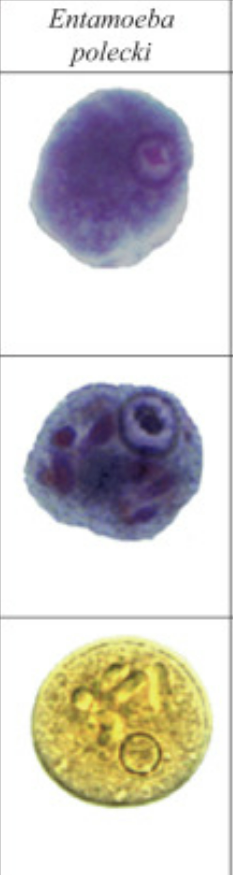
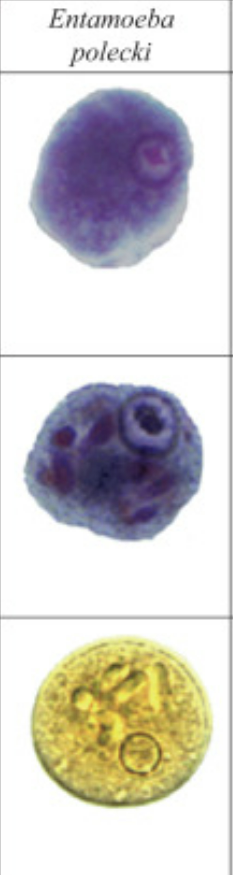
Entamoeba polecki
Found in the intestine of pigs and monkey
Rarely infects human
Motility of the trophozoite is sluggish
E.policki can be distinguishable from E.histolytica by its former cyst is consistently uninucleated, chromatoidal bars are frequently angular or pointed.
Cyst size: 9um-18um
No. of nuclei: 1
Cytoplasmic inclusion cyst: chromatoid bars (angular/pointed), glycogen mass, inclusion mass
Size of trophozoite: 10um-25um
Karyosome: small, centrally located
Cytoplasmic inclusion trophozoite: ingested bacteria and food particles
MOT: Fecal-Oral
Host: Monkey and pigs
Entamoeba chattoni
Found in apes and monkeys
Morphologically identical to E. polecki
Rare to infect humans (only 8 cases)
Identification of E.polecki is done via isoenzyme analysis
Cyst size: 8um-15um
No of nuclei: 1
Cytoplasmic inclusion cyst: similar to E.polecki
Trophozoite size: 10um-20um
Karyosome: similar to E.polecki
Trophozoite Cytoplasmic inclusion: similar to E.polecki
MOT: Fecal-Oral
Host: Apes and monkey

Entamoeba gingivalis
Found in the mouth (oral cavity, lives in the surface of gums and teeth, tonsillar crypts)
Moves quickly and has numerous of blunt pseudopodia
NO CYST STAGE
Abundant cases of oral disease
Size: 10um-20um
Karyosome: central and distinct
Cytoplasmic inclusions: food vacuoles, WBC
MOT: kissing, droplet spray, sharing of utensils
Host: humans

Endolimax nana
Occurs the same frequency as E. coli
Exhibit sluggish movement
Have blunt, hyaline pseudopodia, and nucleus has large, irregular karyosome
Smallest amoeba
Cyst size: 5um-12um
No. of nuclei: 1-4 “cross-eyed cyst”
Trophozoite cytoplasmic inclusion: chromatin granules, diffuse glycogen mass
Trophozoite size: 5um-12um
Karyosome: Centrallly located, large and irregular, blot-like appearance
Cytoplasmic inclusion trophozoite: bacteria
MOT: Fecal-Oral
Host: Humans
Iodamoeba butschilii
Large, vesicular nucleus with a large, central karyosome, surrounded by achromatic granules
No peripheral chromatin granules on the nuclear membrane.
Can only be stained by iodine
Cyst size: 9um-10um
No. of cyst nuclei: 1
Cytoplasmic inclusions cyst: absence of chromatoid bars but has large glycogen body which stains dark brown with iodine
Trophozoite size: 9um-14um
Karyosome: eccentric, large & central
Cytoplasmic inclusions trophozoite: bacteria, yeast & other debris
MOT: Fecal-Oral
Host: humans
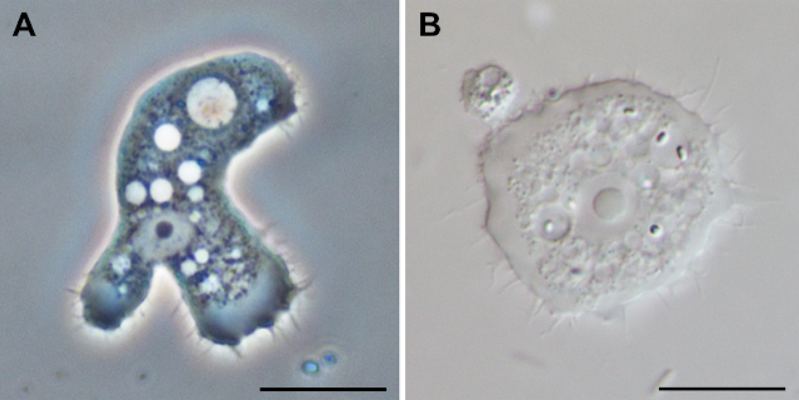
Acanthamoeba spp. (A. trophozoite, B. Cyst)
Found everywhere, free living amoeba
Aquatic organism
Etiologic agent of Acanthamoeba keratitis (AK) and Granulomatous Amebic Encephalitis (GAE).
Active trophozoite stage with characteristic prominent "thorn-like" appendages
Highly resilient cyst stage into which it transforms when environmental conditions are not favorable.
Motile trophozoites feed on gram-negative bacteria, blue-green algae, or yeasts and reproduce by binary fission, but can also adapt to feed on corneal epithelial cells and neurologic tissue through phagocytosis and secretion of lytic enzymes.
Acanthamoeba trophozoites exhibit a characteristic single large nucleus with a centrally located, densely staining nucleolus, a large endosome; finely granulated cytoplasm; and a large contractile vacuole
Acanthamoeba has only two stages, cysts and trophozoites
First described as an opportunistic ocular surface pathogen causing keratitis in 1974.
Documented as the causative agent of human GAE by Stamm in 1972.
TROPHOZOITE
15um – 45um
With shiny or filiform pseudopodia (acanthopodia)
“thorn-like” appendages
Infective stage
Replicate via mitosis
MOT: eye, the nasal passages to the lower respiratory tract, or ulcerated or broken skin
Diagnostic stage
CYST
10 um – 12um
Detectable in tissues
Double walled – outer wrinkled wall
Diagnostic stage
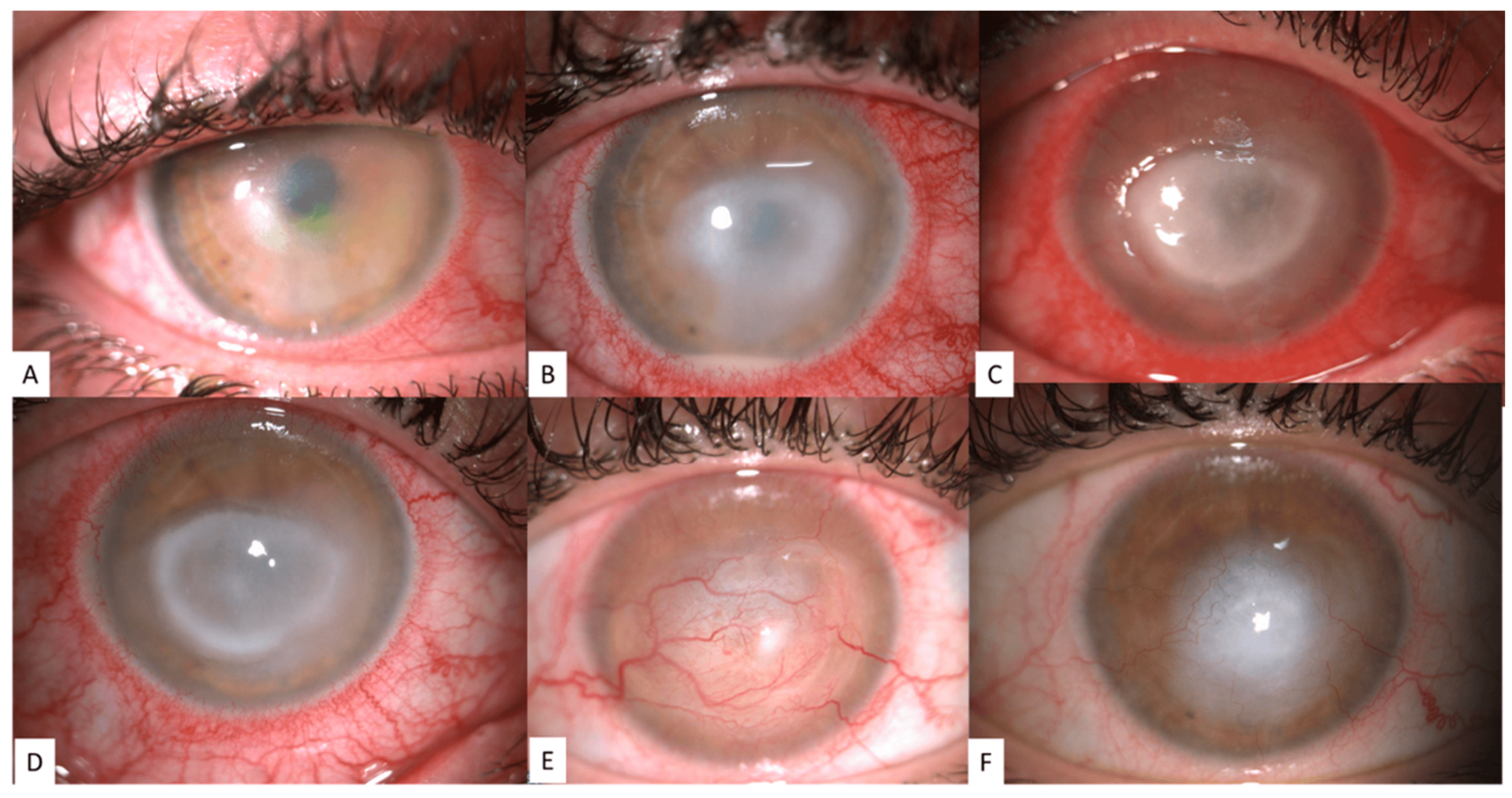
Acanthamoeba kerititis
Associated with the use of improperly disinfected soft contact lenses, particularly those which are rinsed with tap water or contaminated lens solution.
Immunocompromised state contributes to increased susceptibility to infection
Symptoms: ocular pain and blurring of vision, corneal ulceration with progressive corneal infiltration may occur.
Progression leads to scleritis and iritis leading to vision loss
Diagnosed by epithelial biopsy or corneal scrapings for recoverable amoeba
Amebae have also been isolated from the contact lens and lens solution of patients
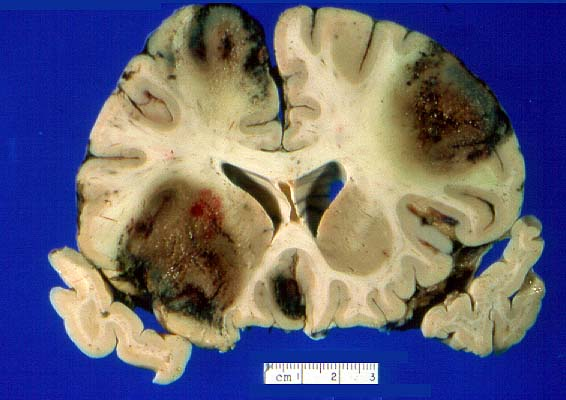
Granulomatous Amebic Encephalitis
Signs and symptoms: fever, malaise, anorexia
Neurologic symptoms: increased sleeping time, severe headaches, mental status changes, epilepsy, coma.
Diagnosis of GAE is usually made post-mortem in most cases.
Post-mortem gross examinations reveals edematous and soft cerebral hemispheres with areas of hemorrhage and focal abscesses.
Most common affected areas are posterior fossa structures, thalamus, and brainstem
Incubation period from initial inoculation is 10 days
Usually made postmortem in most cases due to the rarity of the disease and its unfamiliarity.
Recovery of ameba in the CS is exceedingly rare, imaging results are nonspecific
Naegleria spp.
Free-living protozoan
Two vegetative forms: an ameba(trophozoite form), and a flagellate (swimming
form).
Thermophilic organisms which thrive best in hot springs and other warm aquatic environment
A dormant cyst form is produced when conditions are not favorable.
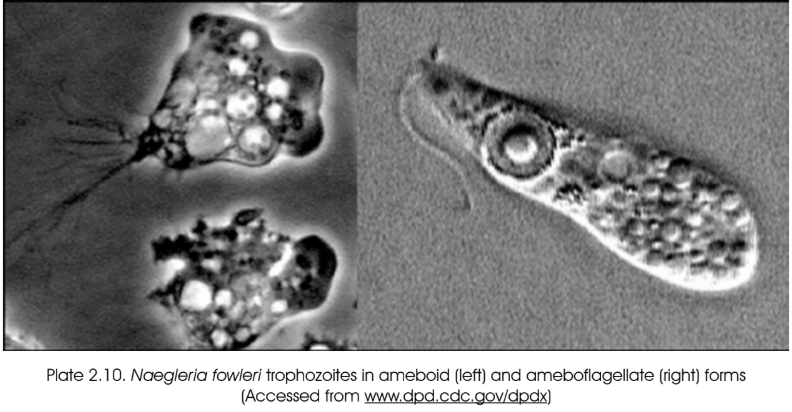
Two forms of trophozoites of Naegleria fowleri: ameboid and ameboflagellate
Only Naegleria fowleri has been reported to consistently cause disease in humans, although some non-fowleri species may cause opportunistic infections.
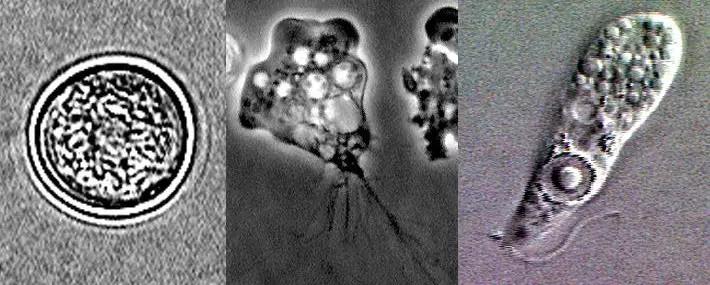
Naegleria fowleri (A. Cyst, B. Ameboid, C. Ameboflagellate)
Has three stages: Cyst, trophozoite, and flagellated form
Causitive agent of rare Primary Amebic Meningoencephalitis (PAM).
PAM usually occurs in previously healthy adults with a history of swimming.
The route of entry is through invasion of organisms through the olfactory bulb after accidental inhalation of water containing the organisms.
PAM presents as fever, nausea, vomiting, headache, nuchal rigidity, and mental status changes, with rapid progression to coma and death
Post-mortem examination of infected brain shows hemorrhagic necrosis, particularly of the olfactory bulbs, congestion and edema of neural tissue
Death usually occurs as a result of cerebral or cerebellar herniation as a result of increased intracranial pressure.
Most persons infected with Naegleria die prior to institution of effective treatment.
Symptoms of PAM are indistinguishable from bacterial meningitis.
Amphotericin B in combination with clotrimazole is synergistic, and has been successfully used to treat PAM.
TROPHOZOITE
Trophozoite replicate via promitosis
Trophozoites infect humans or animals by penetrating the nasal mucosa and migrating to the brain via the olfactory nerves.
Trophozoite are found in cerebrospinal fluid and Tissue
Measures 10um – 35um
Rapidly motile
Two forms:
a.) Amoeboid – lobate pseudopodia
b.) Amoeboflagellate – flagella
Infective stage of N. fowleri
Diagnostic stage of N. fowleri
CYST
7um-15um
Not detectable in clinical specimens
Double walled-outer smooth wall
Not seen in brain tissue